Table of Contents
Definition / general | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Differential diagnosisCite this page: Nagarajan P, Peters SB. HPV independent squamous cell carcinoma-vulva. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/vulvaverrucous.html. Accessed April 23rd, 2024.
Definition / general
- Not a common tumor
- Verrucous carcinoma was first described in 1948 in the oral cavity (Surgery 1948;23:670)
- Though verrucous carcinoma has traditionally been considered to be in the spectrum of giant condylomas histologically, recent studies have suggested that verrucous carcinomas are distinct entities with a non human papillomavirus (HPV) etiology (Am J Surg Pathol 2004;28:638, Int J Gynecol Cancer 2003;13:317)
Epidemiology
- Most common in elderly, postmenopausal women
- Almost all lesions in younger women with similar features are giant condyloma or warty carcinoma / basaloid carcinoma
Sites
- Most commonly affected sites are labium majora > labia minora > posterior commissure
Etiology
- Though initially considered human papillomavirus (HPV) associated (Eur J Gynaecol Oncol 1998;19:319), recent studies show no HPV nucleic acids detected
Clinical features
- Slow growing firm mass, usually accompanied by pruritus and occasionally pain and discharge (especially if large, ulcerated or infected)
Diagnosis
- Histologic examination alone can be misleading due to superficial sampling or lack of an obvious invasive component
- Therefore, clinical history indicating exophytic tumor in an elderly woman is often helpful
Radiology description
- May be useful to assess extent of tumor and exclude metastases (Pan Afr Med J 2014;17:303)
Prognostic factors
- Most important prognostic factors are depth of invasion and surgical margin status
- Local recurrence is common (30 - 50%), especially after resection with inadequate margins (Br J Dermatol 2000;142:1195)
Case reports
- 41 year old woman with Turner syndrome (Gynecol Oncol 2004;92:380)
- 72 and 78 year old women (Eur J Gynaecol Oncol 2011;32:680, Case Rep Obstet Gynecol 2013;2013:932712)
- Verrucous carcinoma of vulva (J Indian Med Assoc 1996;94:456)
Treatment
- Usually excision by partial, simple or radical vulvectomy, with or without inguinal or femoral lymphadenectomy
- Local radiotherapy may be used as an adjuvant but has been associated with development of higher grade squamous cell carcinoma
- Systemic acitretin treatment (dose: 25 mg/day, for 4 - 6 weeks) is effective, with tumor regression in most patients (Br J Dermatol 2000;142:1195)
- Chemotherapy (cisplatin, bleomycin, methotrexate and leucovorin) (Eur J Gynaecol Oncol 2011;32:680)
Gross description
- Large, hyperkeratotic papillary or exophytic lesion, usually slow growing
- Rarely multiple lesions (Br J Dermatol 2000;142:1195, Am J Surg Pathol 2004;28:638)
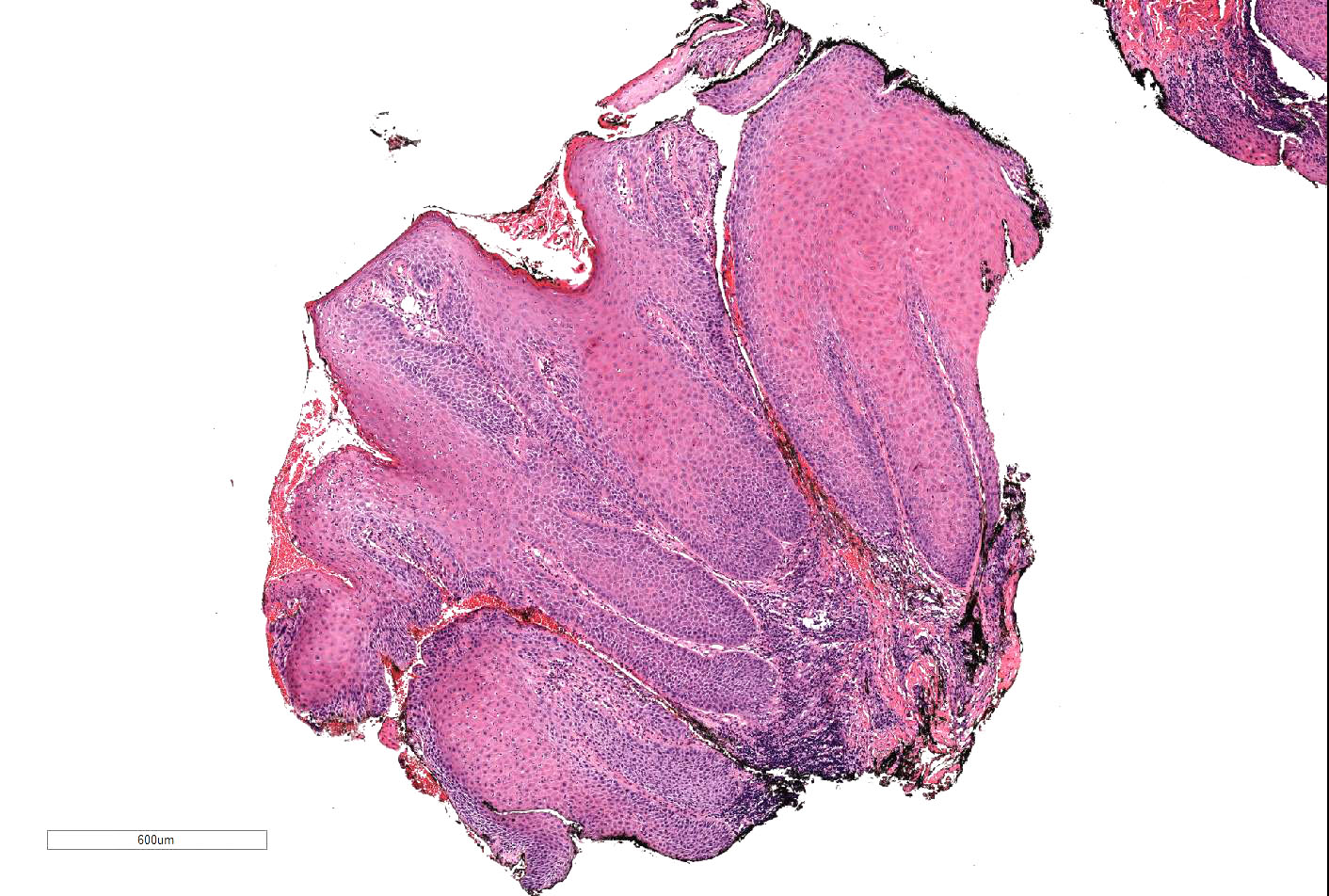
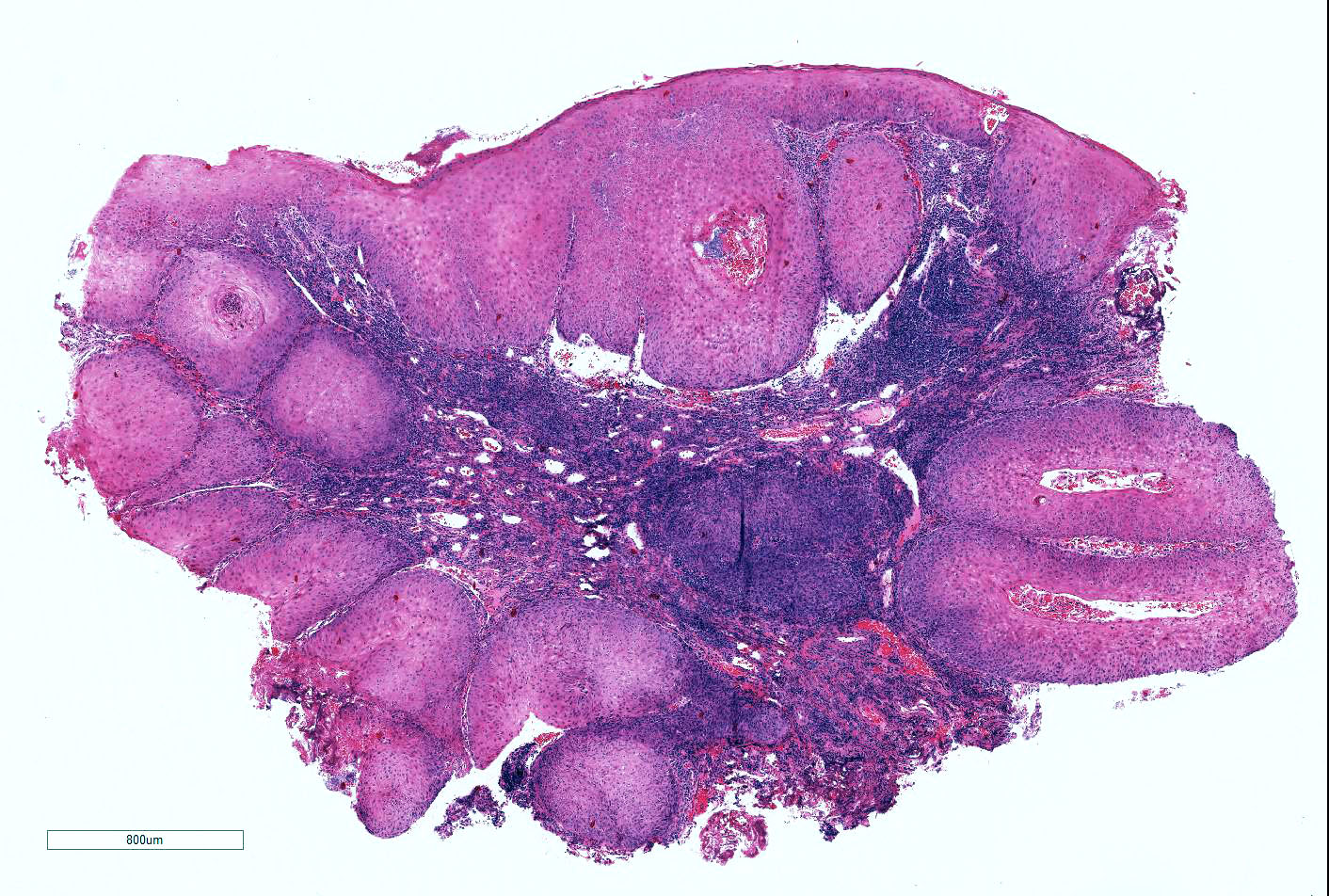
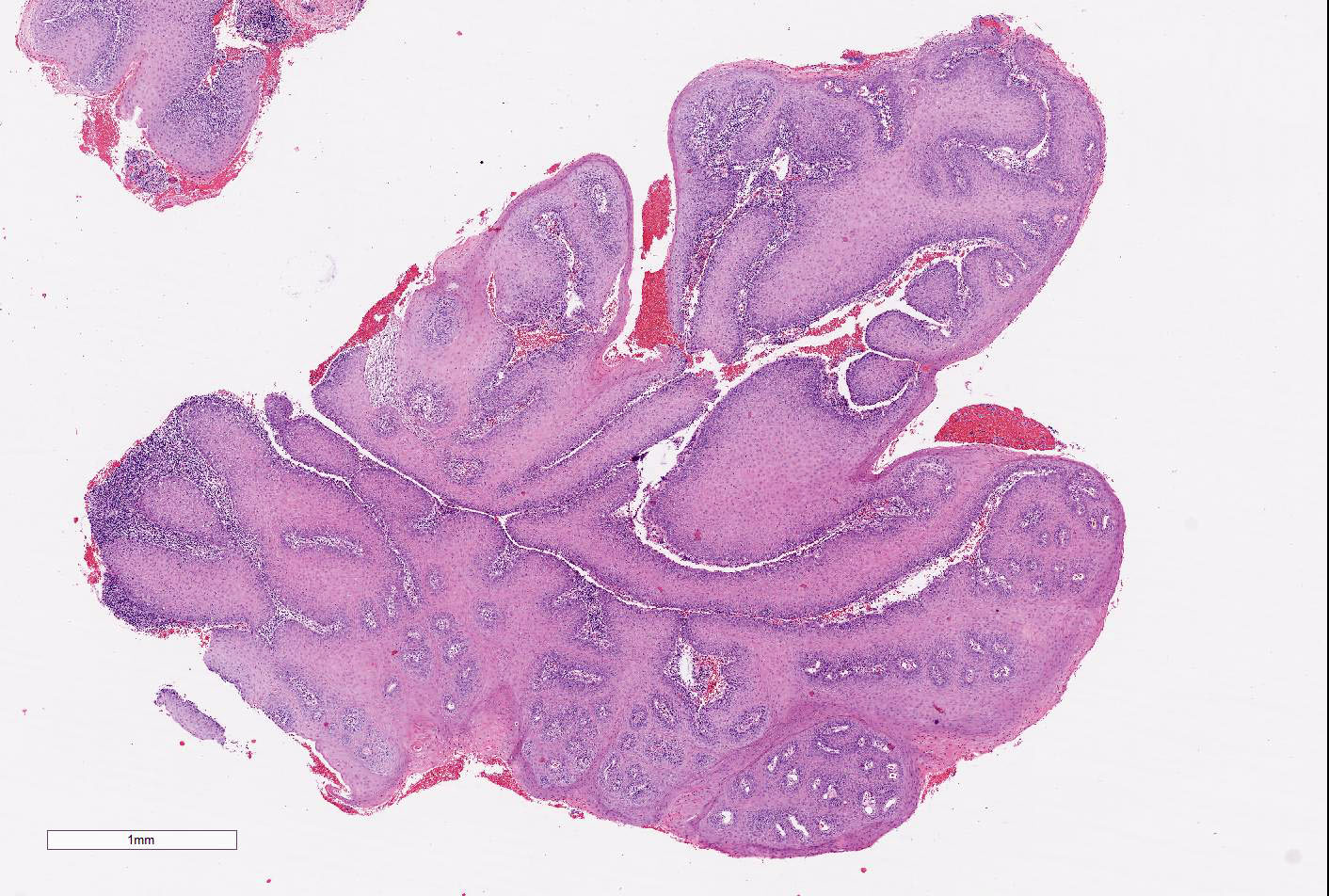
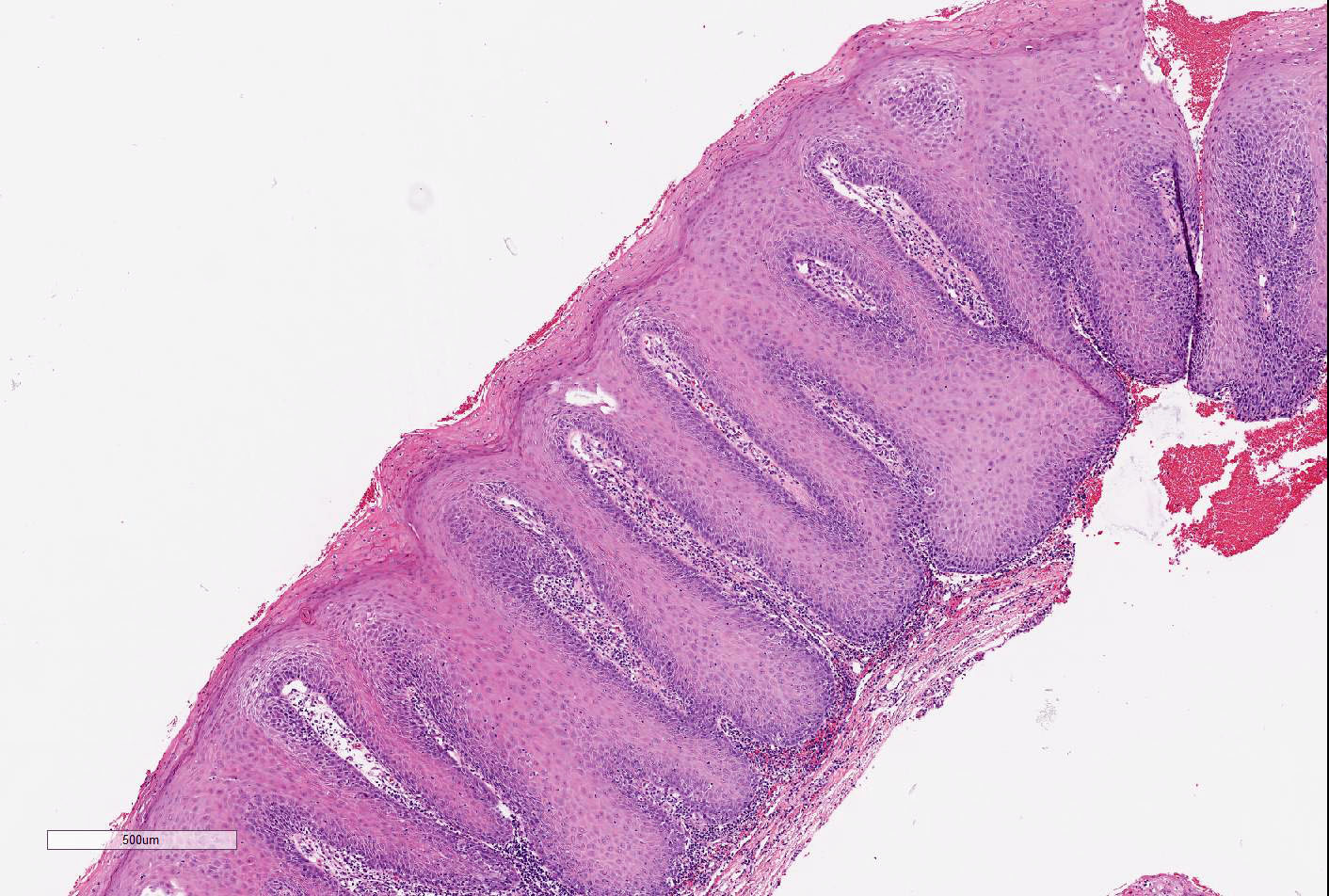
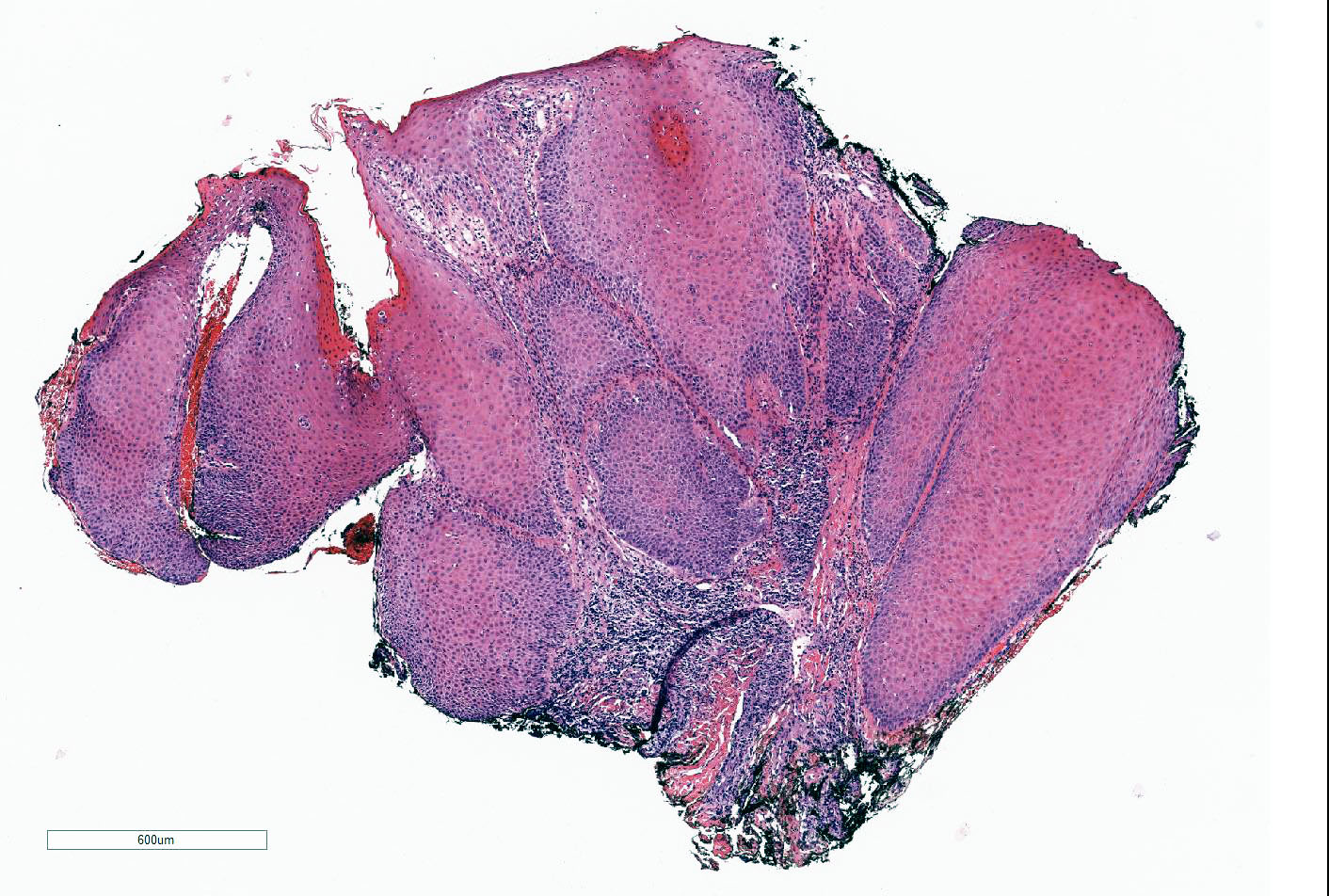
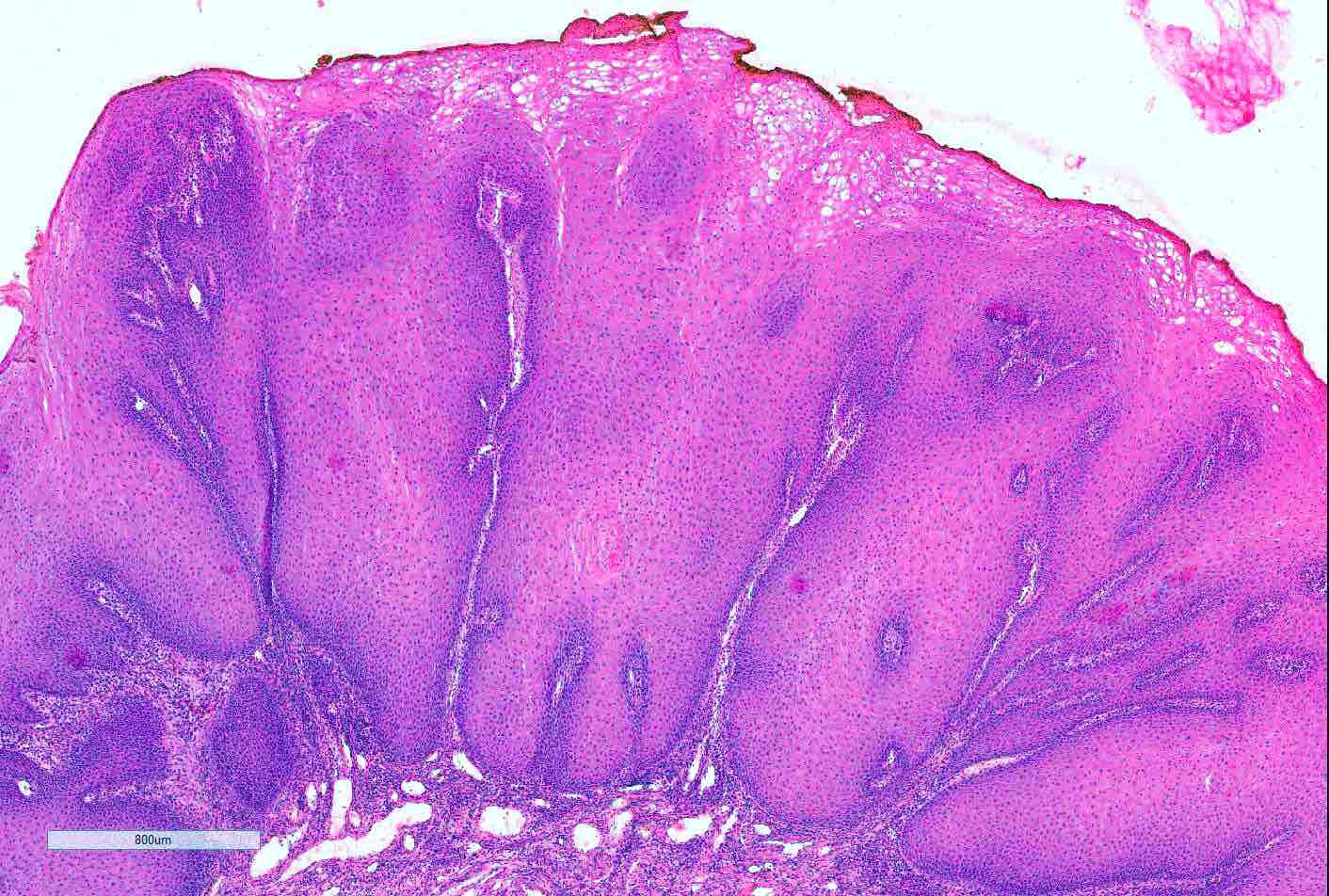
Microscopic (histologic) description
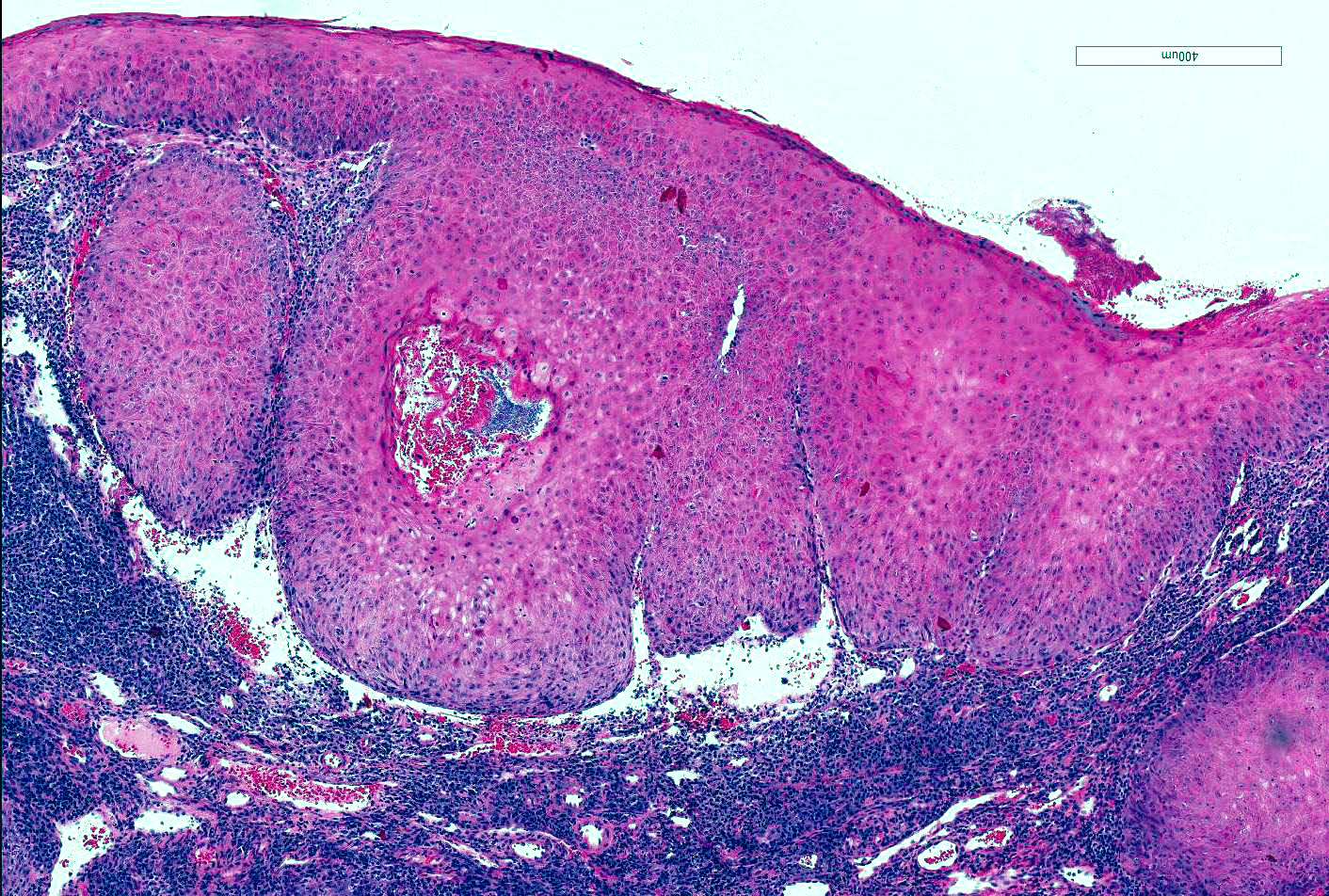
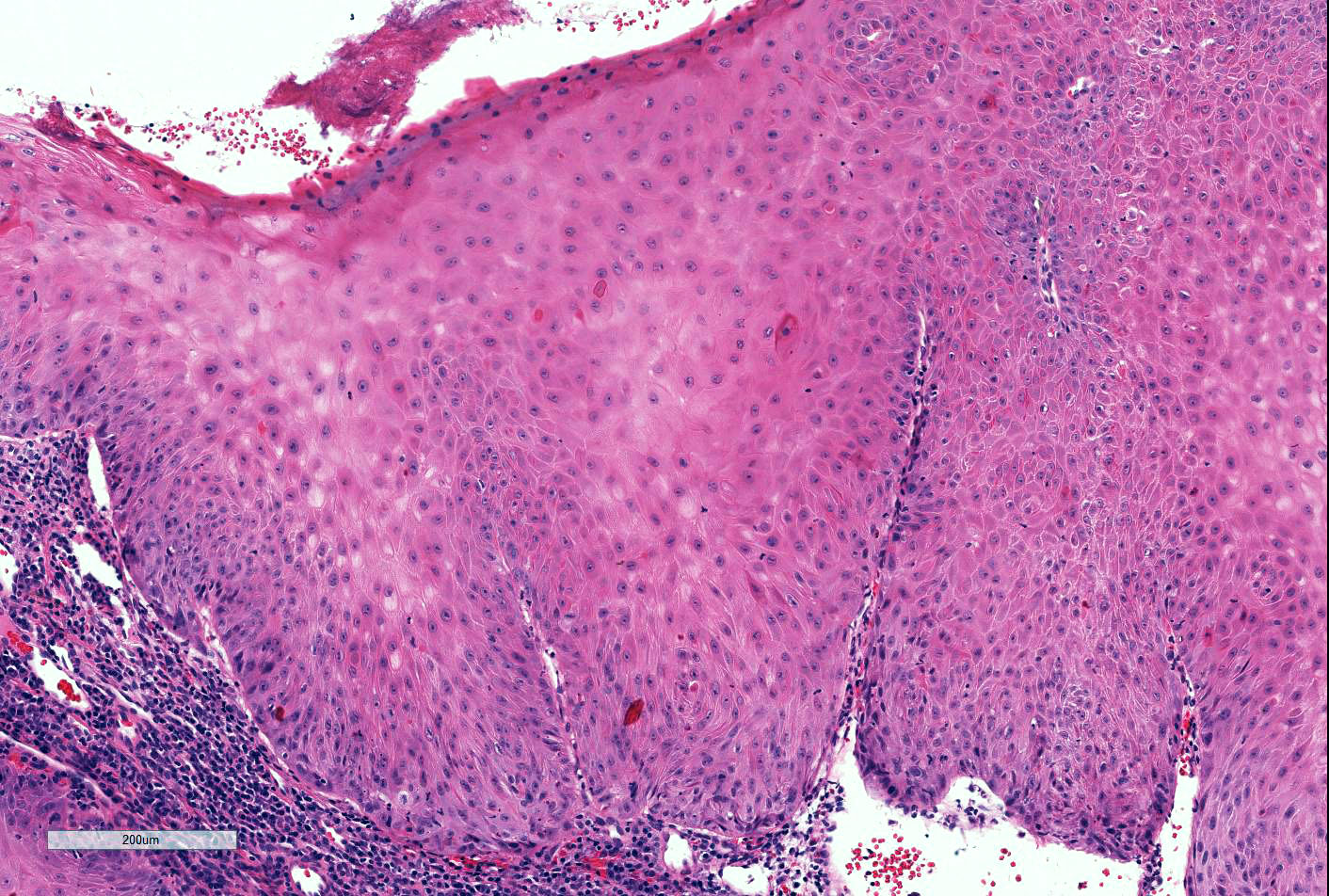
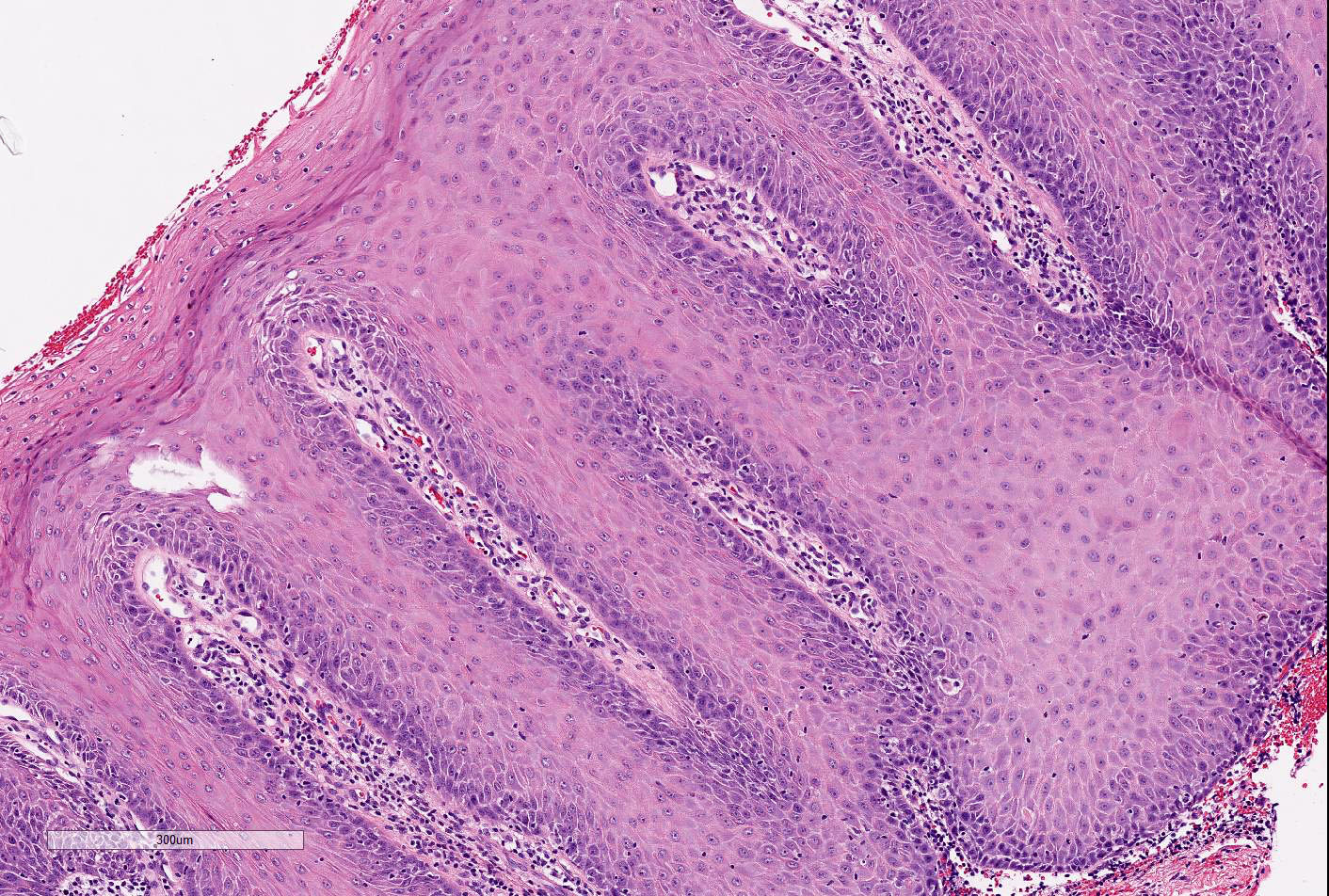
- Exo-endophytic, well circumscribed tumor composed of closely packed papillary structures lined by well differentiated stratified squamous epithelium, with minimal cellular atypia
- By definition, no invasion by clusters or single tumors cells should be present
- Epithelium demonstrates prominent acanthosis with (bulbous) expansion of rete ridges that push into the dermis / submucosa with rounded borders or a broad front
- In tangentially cut sections, the tumor is composed of large, back to back nests of well differentiated squamous epithelium
- Massive hyperkeratosis and parakeratosis is present
- Cells have abundant pale, eosinophilic cytoplasm with low nuclear to cytoplasmic ratio, no / mild nuclear pleomorphism, basally located mitotic figures
- Mild to moderate chronic inflammation in stroma is common
- If infection / ulceration, neutrophils may be prominent
- Lymphovascular and perineural invasion are extremely rare
- Coexisting non human papillomavirus (HPV) associated carcinomas of higher grade or precursors are not uncommon and should therefore be ruled out (Am J Surg Pathol 2004;28:638)
- Background lichen simplex chronicus with diffuse verrucous features or lichen sclerosus may be seen; VIN is not usually present
Microscopic (histologic) images
Cytology description
- Anucleate squamous cells (Acta Cytol 1993;37:871)
Positive stains
- Ki67 proliferation index is variably increased but in 70 - 80% of cases, Ki67 expression is localized to basal layer of squamous epithelium
Negative stains
- HPV in situ hybridization is negative (Int J Gynecol Cancer 2003;13:317)
- p53 is not overexpressed
Molecular / cytogenetics description
- Human papillomavirus (HPV) in situ hybridization is negative (Int J Gynecol Cancer 2003;13:317)
Differential diagnosis
- Giant condyloma acuminatum:
- Predominantly exophytic
- Human papillomavirus (HPV) associated cytopathic effects of koilocytes (wrinkled or raisinoid nuclei, perinuclear halo, multinucleation, suprabasal mitoses) are easily identified
- HPV nucleic acids demonstrated by in situ hybridization (Arch Gynecol Obstet 2013;287:1047)
- Other keratinizing squamous cell carcinomas:
- Demonstrate at least focal stromal invasion by single cells or small clusters of tumors cells
- Cellular atypia may be prominent
- Variable differentiation
- Rare metastases to regional lymph nodes