Table of Contents
Definition / general | Epidemiology | Clinical features | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Additional referencesCite this page: Roychowdhury M. Eosinophilic cystitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bladdereosinophilic.html. Accessed May 6th, 2024.
Definition / general
- Inflammatory condition of the urinary bladder, with recurrent episodes of urinary frequency, dysuria, gross hematuria and suprapubic pain during micturition
- Not related to Langerhans cell granulomatosis
Epidemiology
- Rare (about 200 reported cases)
- Women or children with allergic disorders and peripheral eosinophilia, older men with prostate / bladder disorders or parasitic infestation
Clinical features
- Reported at all ages with striking predominance in females
- 20% occur in children; symptoms tend to disappear spontaneously (Arch Dis Child 2001;84:344)
- Clinical and imaging findings are nonspecific; cystoscopic findings include ulcers, exudates, edematous bullae or polyps (which may simuate malignancy)
Case reports
- Case series in males (Arch Pathol Lab Med 2009;133:289)
- Eosinophilic cystitis associated with eosinophilic enterocolitis (Br J Radiol 2010;83:e122)
Treatment
- Treatments are typically not curative
- Withdrawal of any identifiable precipitating factor
- Nonsteroidal antiinflammatory agents and antihistamines are favored first line agents followed by corticosteroids or cyclosporine
- Transurethral resection is used in refractory cases (J Urol 2001;165:805)
- Longterm followup is recommended for all patients (Int J Clin Pract 2005;59:356)
Gross description
- Edematous and erythematous mucosa with polypoid growths resembling allergic polyps of nasal septum
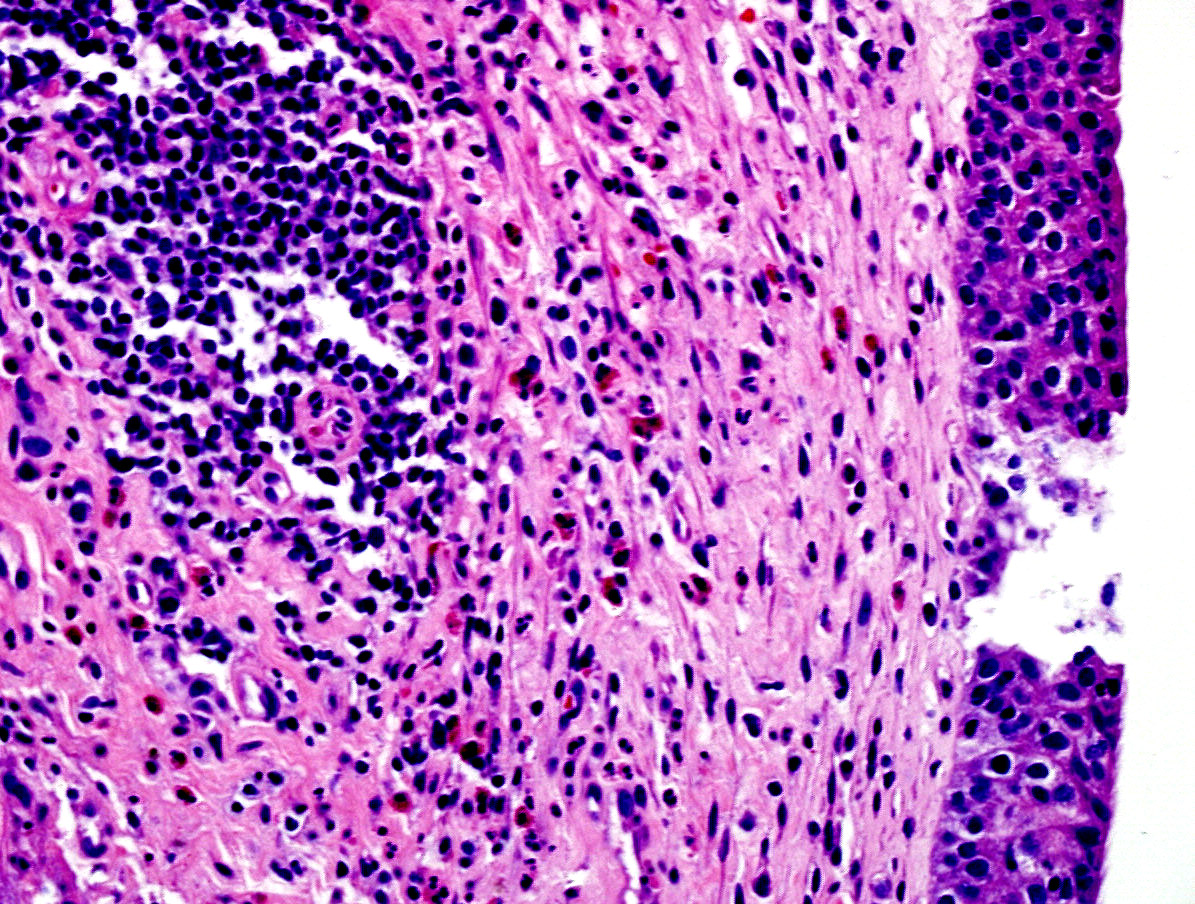
Microscopic (histologic) description
- Hispathological findgings can be divided in "acute" and "chronic" phase:
- Acute phase: prominent eosinophilic infiltrate (Yamada and Taguchi criteria are 20 or more eosinophils per five 20x fields) with edema and occasional muscle necrosis; Charcot-Leyden crystals may be present (Arch Pathol Lab Med 2009;133:289)
- Chronic phase: fewer eosinophils but more prominent mast cells, plasma cells and muscle fibrosis
Microscopic (histologic) images
Additional references