Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Redding-Ochoa J, Morris M. Dementia with Lewy bodies. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/cnsnontumorlewybody.html. Accessed May 13th, 2024.
Definition / general
- Dementia is defined as a progressive cognitive decline of sufficient magnitude to interfere with normal social or occupational functions or usual daily activities (Neurology 2017;89:88)
- Lewy body dementia indicates dementia attributed to Lewy body pathology in the neocortex and limbic regions
- Cognitive changes should occur before or simultaneously with Parkinsonian motor symptoms (see 1 year rule below)
- Lewy body dementia and Parkinson disease with dementia are distinguished based on clinical criteria; pathologically the 2 conditions cannot be distinguished
Essential features
- Lewy body dementia (or dementia with Lewy bodies [DLB]) is a clinicopathological term that encompasses a clinical dementia phenotype that precedes or coincides with Parkinsonism within a year of onset and the presence of Lewy bodies in supratentorial distribution (i.e., limbic and neocortical Lewy body pathology subtypes)
- Misfolded aggregated alpha synuclein is the main constituent of Lewy bodies
- Alzheimer disease neuropathologic changes frequently co-occur with Lewy body dementia and the relative burden of the 2 pathologies is thought to influence the clinical presentation
Terminology
- Diffuse / neocortical Lewy body disease (neuropathologic term; recommended)
- Dementia with Lewy Bodies
- Lewy body variant of Alzheimer disease (historical term; not recommended)
- Senile dementia of Lewy body type (historical term; not recommended)
ICD coding
Epidemiology
- Prevalence in the general population up to 5% (Age Ageing 2005;34:561)
- Accounts for up to 30% of all dementia cases (Age Ageing 2005;34:561)
- Annual incidence was estimated at 3.8% (range: 3.2 - 4.5%) in a systematic literature review (Psychol Med 2014;44:673)
Sites
- Lewy body pathology primarily affects the nervous system (i.e., central, peripheral and autonomic)
- Extracerebral Lewy body pathology has been documented in the gastrointestinal tract, skin, adrenal gland, salivary glands, heart and genitourinary tract in postmortem studies (Mov Disord 2014;29:1010, Acta Neuropathol 2010;119:689, J Mov Disord 2020;13:1)
Pathophysiology
- Alpha synuclein aggregates in neuronal cell bodies and neurites in brainstem, limbic and neocortical structures (Neurology 2005;65:1863)
- Synuclein aggregates in limbic and neocortical areas are associated with cognitive and neuropsychiatric symptoms of dementia with Lewy bodies
- Synuclein aggregates in brainstem areas are associated with Parkinsonian symptoms
- While alpha synuclein aggregates are thought to progress in an ascending fashion in Parkinson disease (with or without dementia), whether this is true for Lewy body dementia remains unclear (Neurobiol Aging 2003;24:197, Mol Neurodegener 2019;14:5)
- Alpha synuclein aggregates are thought to form in a 2 step process (Biochemistry 2008;47:2413, Mol Neurodegener 2019;14:5)
- Nucleation phase: association of soluble monomers into intermediate oligomers or protofibrils
- Elongation phase: protofibrils are incorporated into insoluble, β sheet rich fibrils
- Fragments of the intermediate fibrils (i.e., seeds) may be capable of templating conformational conversion of the native protein, which could explain the spread of pathology across cells in the brain
- This seeding capability is the basis for studies of synuclein RT-QuIC assays for biomarkers of synuclein pathology (Mol Neurodegener 2019;14:5)
Etiology
- Lewy body dementia is a sporadic disease in the majority of cases
- Estimated genetic heritability ranges from 31 - 60% (Neurobiol Dis 2019;127:492)
- Genes associated with higher risk of dementia with Lewy bodies (e.g., APOE, SNCA, GBA) overlap with other neurodegenerative disorders (i.e., Alzheimer disease, Parkinson disease) (Lancet Neurol 2018;17:64, Handb Clin Neurol 2018;148:431)
- Familial Alzheimer disease mutations can also cause diffuse Lewy body pathology (Arch Neurol 2006;63:370, Neurology 2008;71:1925)
- Mutations and multiplications in SCNA have been described in families with variable phenotypes of Parkinson disease and dementia with Lewy bodies (Curr Neurol Neurosci Rep 2018;18:67)
- Discordant incidence between monozygotic twins suggests environmental or epigenetic influences (J Neurol Neurosurg Psychiatry 2009;80:562)
Diagrams / tables
Clinical features
- Unlike Alzheimer disease, dementia with Lewy bodies tends to affect attention, executive function and visuospatial function early in disease progression (J Neuropsychiatry Clin Neurosci 2000;12:425)
- Besides dementia, DLB patients must present with ≥ 2 core clinical features (Neurology 2017;89:88)
- Cognitive fluctuations
- Visual hallucinations: early clinical sign; useful clinical feature in the differential diagnosis of dementia with Lewy bodies versus Alzheimer dementia (Brain 2006;129:729)
- Rapid eye movement (REM) sleep behavior disorder
- Parkinsonism: present in 70 - 85% (J Neuropsychiatry Clin Neurosci 2001;13:374, Neurology 2017;89:88)
- 1 year rule: DLB patients show Parkinsonian motor symptoms within 1 year of the dementia diagnosis; Parkinson disease with dementia is diagnosed when the cognitive symptoms occur in longstanding (i.e., > 1 year) Parkinsonism
- Supportive clinical features
- Marked sensitivity to antipsychotic agents
- Postural instability
- Repeated falls
- Syncope or other episodes of unresponsiveness
- Severe autonomic dysfunction (e.g., urinary incontinence)
- Hypersomnia
- Polysomnographic evidence of REM sleep without atonia is an indicative biomarker (Neurology 2017;89:88)
- Hyposmia
- Hallucinations in other modalities
- Systematized delusions
- Apathy, anxiety and depression
Diagnosis
- Brain autopsy is the gold standard for Lewy body pathology diagnosis (see Microscopic (histologic) features)
- Correlation of Lewy body pathology distribution and dementia is the cornerstone of the integrated clinicopathologic diagnosis (Neurology 2005;65:1863)
- In the presence of both Alzheimer disease neuropathologic changes (ADNC) and Lewy body pathology, the National Institute on Aging (NIA) Reagan score or Braak score is weighed against the Lewy body pathology to establish a probabilistic statement on the individual pathology contribution to the dementia presentation
- Dementia is an essential feature (see Definition / general)
- Current clinical criteria are formulated according to clinical features and biomarkers (Neurology 2017;89:88)
- Clinically probable dementia with Lewy bodies
- A) 2 or more core clinical features (see Clinical features)
- B) 1 core clinical feature and ≥ 1 indicative biomarker determined by single photon emission computed tomography (SPECT), PET, iodine meta iodobenzylguanidine (MIBG) myocardial scintigraphy, electroencephalography (EEG) / polysomnography
- Clinically possible dementia with Lewy bodies
- A) 1 core clinical feature is present, without biomarker evidence
- B) 1 or more biomarkers are present but no core clinical features are present
Laboratory
- Fluid and tissue biomarkers for Lewy body pathology is an area of active research (Front Neurol 2022;12:805135)
Radiology description
- Nonspecific generalized atrophy may be present
- An MRI based volumetric study found greater atrophy in the putamen in LBD patients compared to controls and Alzheimer disease dementia patients (Neurology 2003;61:1191)
- SPECT and FDG / PET scans demonstrate diminished general perfusion and hypometabolism, predominating in the occipital cortex (Prog Neuropsychopharmacol Biol Psychiatry 2001;25:447, Neurology 2001;56:643)
- Reduced dopamine transporter uptake in basal ganglia by SPECT or PET (Neurology 2017;89:88)
- Low uptake 123iodine MIBG myocardial scintigraphy is a biomarker (Neurology 2017;89:88)
Radiology images
Prognostic factors
- In a systematic review, dementia with Lewy bodies (1.9 - 6.3 years) showed a shorter survival compared to Alzheimer disease (3.2 - 6.6 years) (Lancet Neurol 2017;16:390)
- Cognitive decline rate appears to be greater in dementia with Lewy bodies compared to Alzheimer disease in a large multicenter, international cohort (J Alzheimers Dis 2017;57:787)
Case reports
- 59 year old woman with a novel SNCA E83Q mutation associated with dementia with Lewy bodies and severe frontotemporal atrophy (Neuropathology 2020;40:620)
- 65 year old man with incidental neocortical Lewy body pathology without involvement of olfactory bulb and brainstem (J Korean Med Sci 2022;37:e195)
- 75 year old woman with dementia with Lewy bodies and Fahr disease copathology at autopsy (Clin Neuropathol 2020;39:227)
Treatment
- Involves a multidisciplinary team including providers from neurology, neuropsychology, psychiatry, social work and palliative medicine
- No pharmacologic approach modifies the disease progression
- Cholinesterase inhibitors (e.g., donepezil, rivastigmine) are used for the management of cognitive and behavioral symptoms (Am J Psychiatry 2015;172:731)
- Antipsychotic drugs are used only in severe and refractory behavioral cases
- Levodopa or carbidopa levodopa for cases with Parkinsonian symptoms
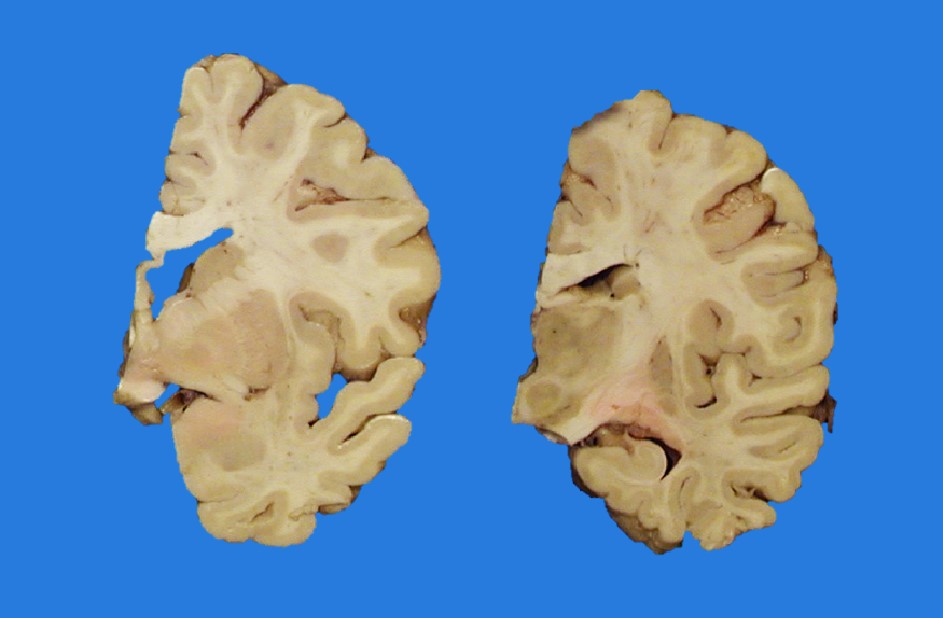
Gross description
- Brain weight is frequently within normal limits or slightly decreased
- Pallor of substantia nigra and locus coeruleus is common (Mol Neurodegener 2019;14:5)
- Cortical atrophy can be present, especially with co-occurring Alzheimer disease neuropathologic changes
- Hippocampal atrophy is not a gross feature of pure Lewy body pathology
Microscopic (histologic) description
- Frequent loss of dopaminergic neurons and gliosis in the substantia nigra
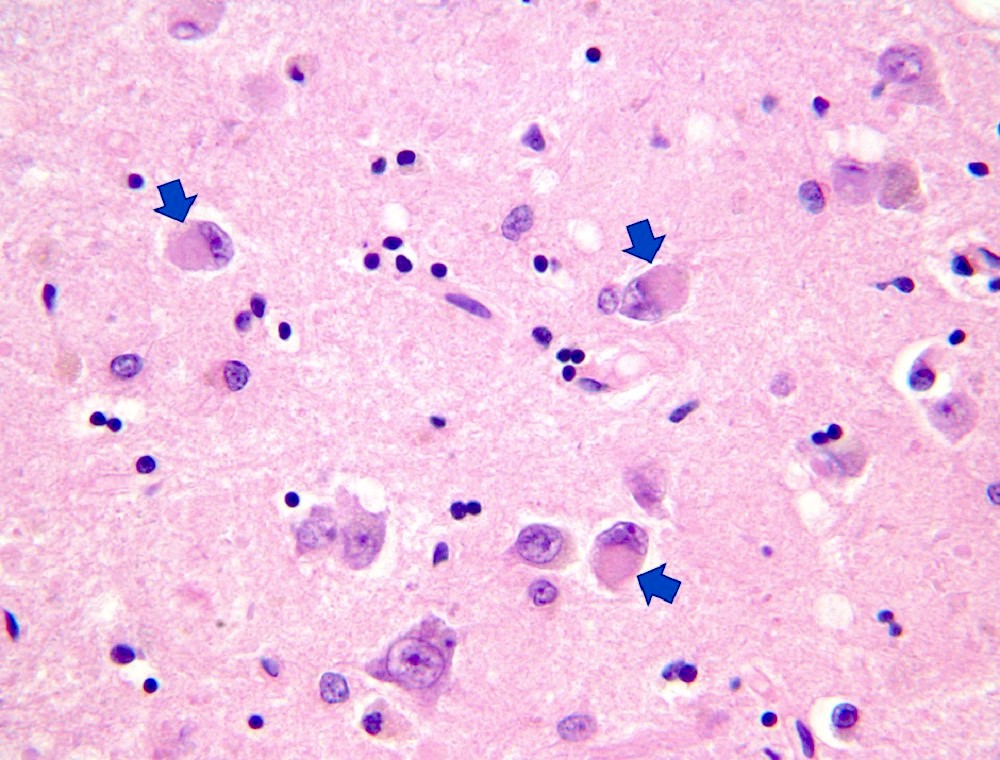
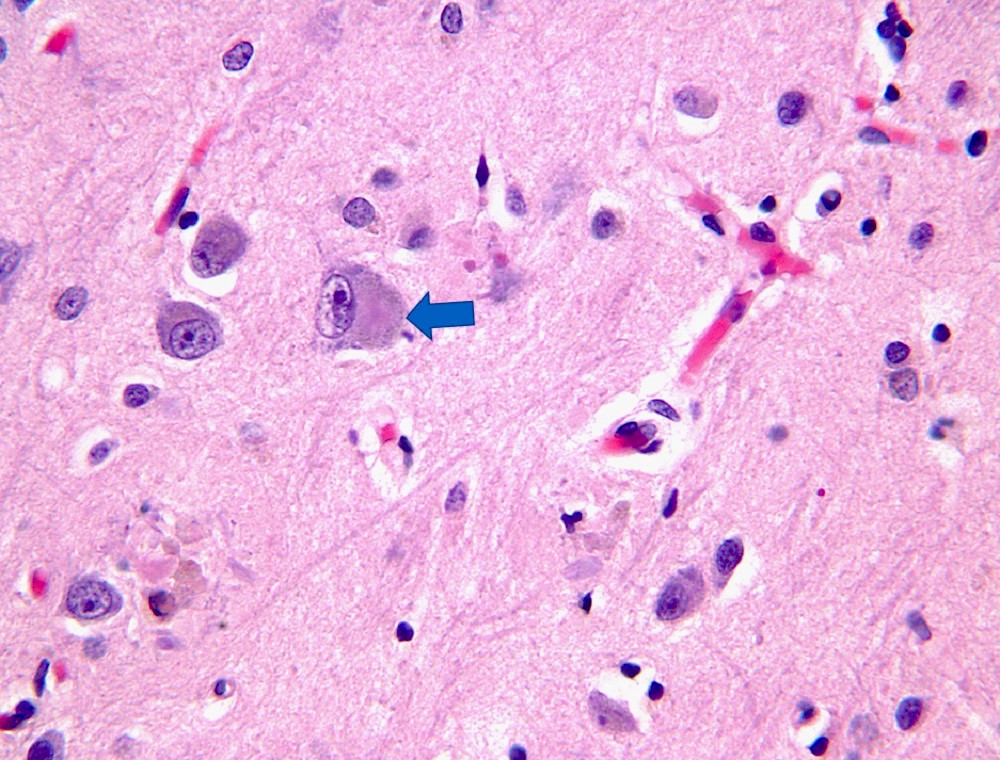
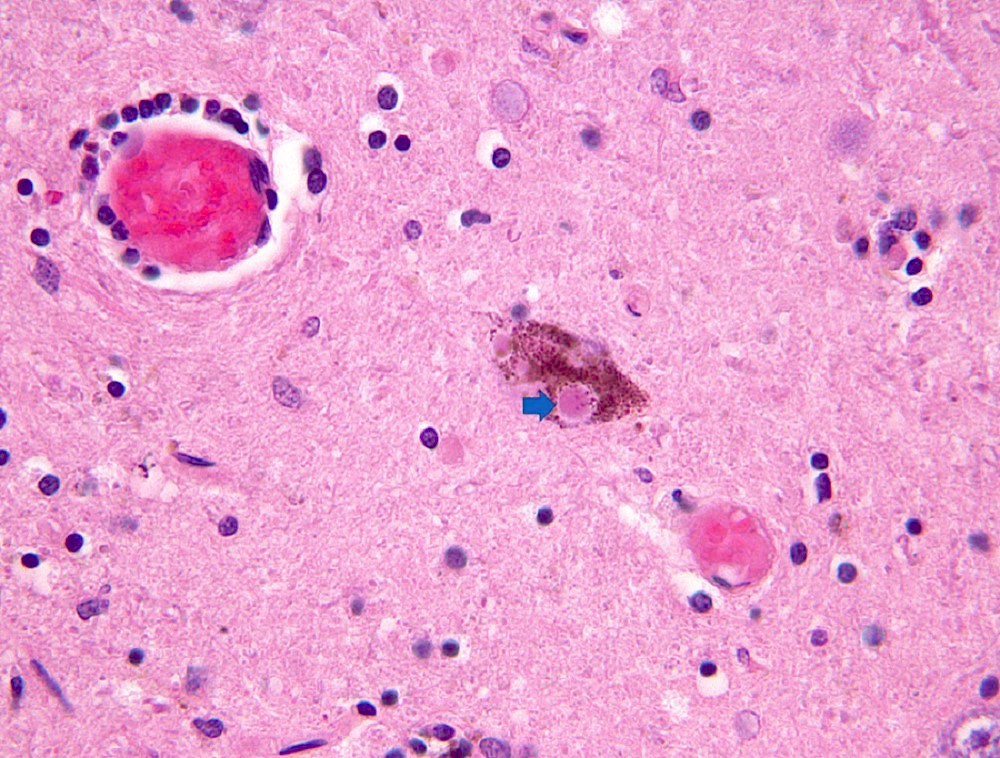
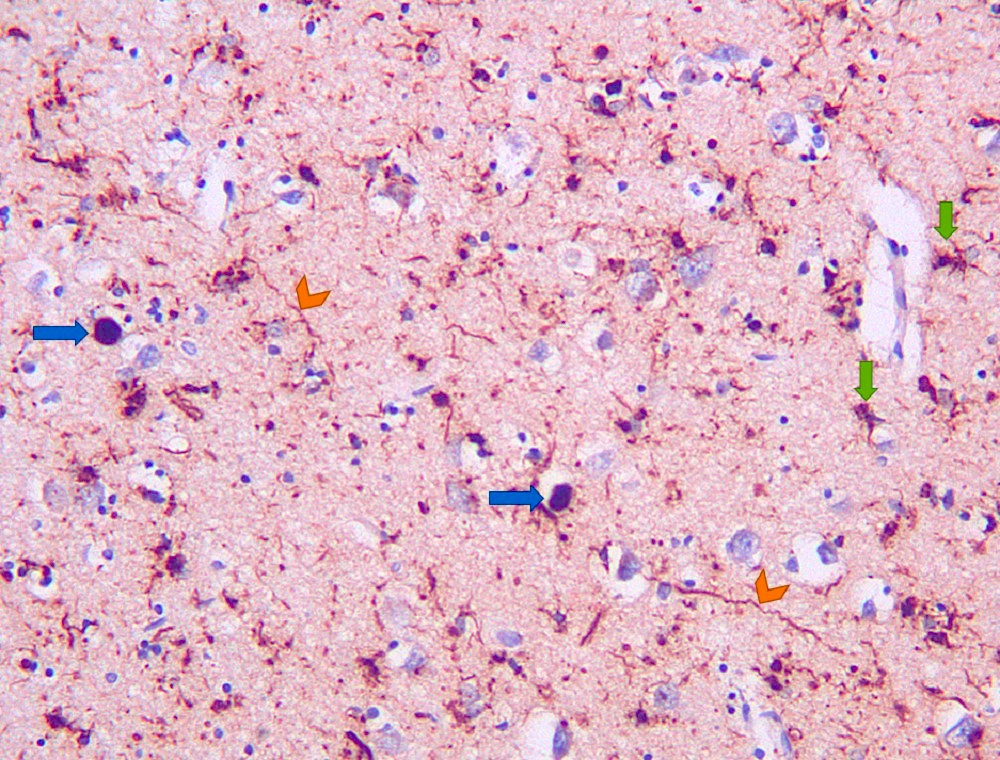
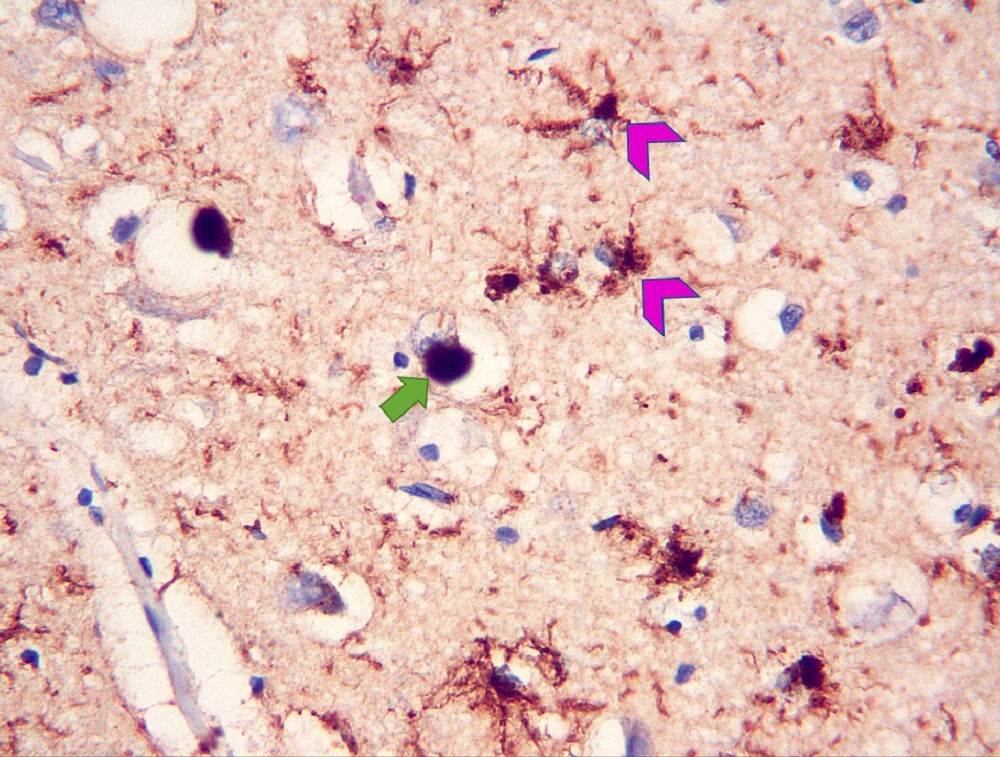
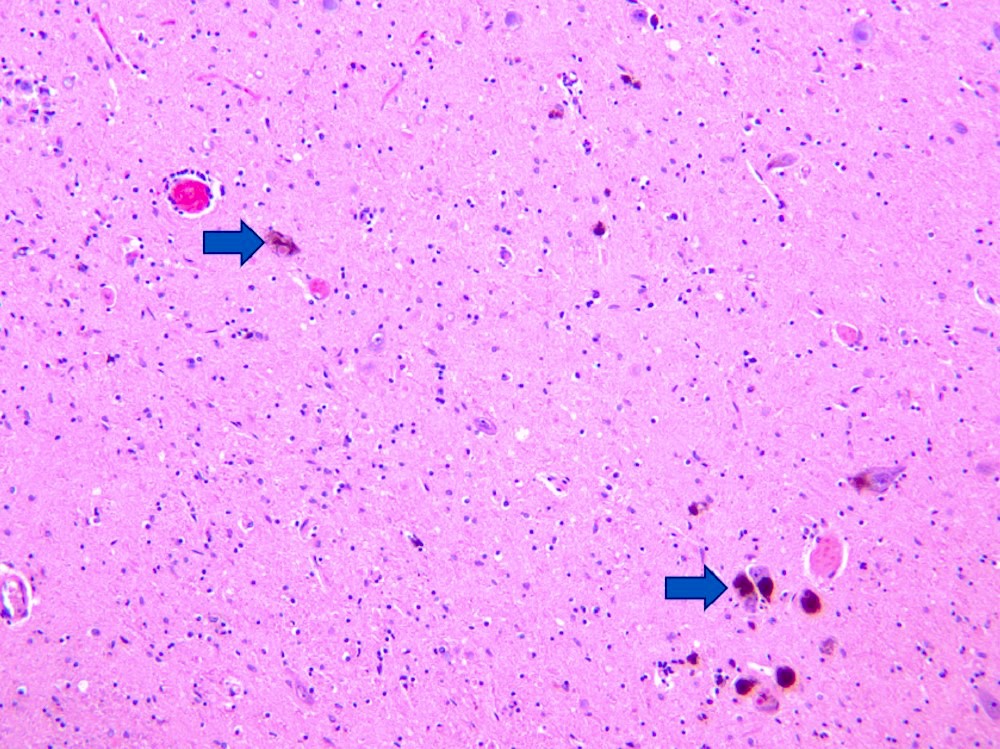
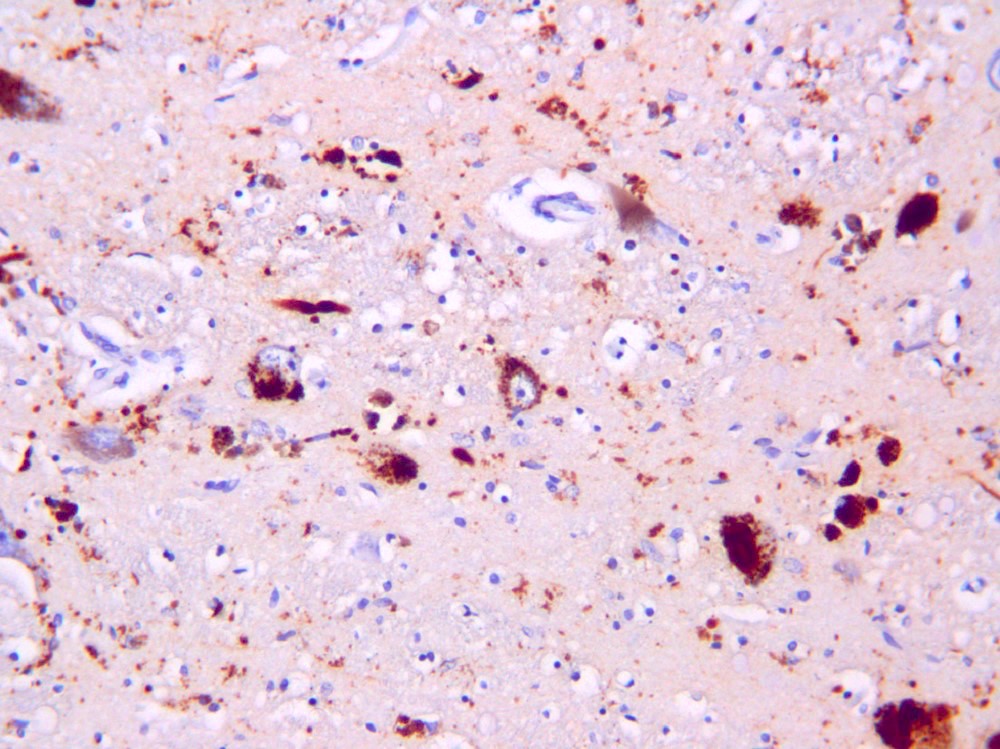
- Lewy bodies vary in morphology according to the brain region involved (Mol Neurodegener 2019;14:5)
- Cortical and limbic associated Lewy bodies are often poorly demarcated, round or reniform, hyaline, amphophilic and have neuronal perikaryal inclusions
- Most commonly found in deep cortical layers
- May not be appreciable on standard H&E staining
- Brainstem Lewy bodies show a central eosinophilic core, surrounded by a clear halo in pigmented neurons (J Geriatr Psychiatry Neurol 2002;15:210)
- Pale bodies are faintly stained neuronal cytoplasmic inclusions without a halo, which are composed of alpha synuclein and proposed as a possible precursor to Lewy bodies (Neuropathology 2020;40:30)
- Glial cells commonly show synuclein pathology in dementia with Lewy bodies, particularly in cortical and limbic areas (Acta Neuropathol 2003;105:163)
- Alzheimer disease neuropathologic changes (i.e., amyloid plaques and neurofibrillary tangles) occur frequently in dementia with Lewy bodies
- Lewy body pathology is scored in semiquantitative method in multiple brain regions (Neurology 2005;65:1863)
- Lewy body (LB) pathology is scored at low power field (10x) in each region from 0 - 4
- 0 = none
- Stage 1 = sparse LBs or Lewy neurites (i.e., 1 LB)
- Stage 2 = moderate (> 1 LBs and sparse neurites)
- Stage 3 = severe (≥ 4 LBs and scattered neurites)
- Stage 4 = very severe (numerous LBs and numerous neurites)
- Scored regions: cranial nerve nuclei IX / X, locus coeruleus, substantia nigra, nucleus basalis of Meynert, amygdala, transentorhinal cortex, cingulate cortex, temporal cortex, frontal cortex and parietal cortex
- Scores are used to categorize into brainstem predominant, limbic or neocortical Lewy body disease
- Higher Lewy body pathology burden in cortical (temporal, frontal and parietal cortices) and limbic (nucleus basalis of Meynert, amygdala, transentorhinal cortex, cingulate cortex) areas are related to a clinical presentation consistent with dementia with Lewy bodies
- Higher Alzheimer disease pathology scores are thought to inversely correlate with the likelihood of clinical presentation consistent with dementia with Lewy bodies (Neurobiol Aging 1997;18:S1, Neurology 2005;65:1863)
- Lewy body (LB) pathology is scored at low power field (10x) in each region from 0 - 4
Microscopic (histologic) images
Positive stains
- Alpha synuclein: stains Lewy bodies and Lewy neurites in neurons
- Total or phosphorylated alpha synuclein antibodies can be used
- Alpha synuclein is the major component of Lewy bodies and Lewy neurites (Nature 1997;388:839)
- Glial cells commonly harbor synuclein inclusions in diffuse type Lewy body pathology (Acta Neuropathol 2003;105:163)
- p62, ubiquitin: nonspecific marker of many protein aggregates in neurodegeneration (J Neuropathol Exp Neurol 2003;62:1241)
Negative stains
- Amyloid beta: may label coexisting Alzheimer pathology, negative in Lewy bodies
- Phospho-tau: may label coexisting tau pathology, can coaggregate in a minority of Lewy bodies (J Neuropathol Exp Neurol 2003;62:389)
- TDP-43: may label coexisting pathology, negative in Lewy bodies
Electron microscopy description
- Electron microscopy assessment is not used for diagnosis of Lewy body pathology
- Correlative light and electron microscopy (CLEM) assessment of Lewy bodies and neurites demonstrated disrupted lipid membranes, distorted organelles (e.g., mitochondria) and vesicles (Nat Neurosci 2019;22:1099)
Sample pathology report
- Brain, autopsy:
- Lewy body disease, diffuse (neocortical) type (see comment)
- Alzheimer disease neuropathologic changes, intermediate level (A2, B2, C2)
- Gross description:
- The fresh brain weight is 1,400 g. External examination of the brain is remarkable for mild atrophy. The base of the brain is remarkable for mild multifocal nonocclusive atherosclerosis. The cranial nerves I - XII are normal and the brainstem and cerebellum are externally unremarkable.
- On coronal sections, the cortical thickness is normal and subjacent white matter is well demarcated. The ventricular system is patent and shows moderate expansion of the lateral ventricles. The basal ganglia, thalamus and hypothalamus are normal in color, shape and size. The amygdalae and hippocampi are unremarkable. In the brainstem, the locus coeruleus and substantia nigra show marked pallor.
- Microscopic description:
- H&E stained sections of the brainstem are remarkable for Lewy bodies with severe loss of pigmented neurons in the substantia nigra and locus coeruleus and associated gliosis. In the limbic regions, the amygdala and cingulate cortex show neurons with poorly demarcated spherical eosinophilic cytoplasmic inclusions. Neocortical sections show sparse neurons with perikaryal expansion and eosinophilic inclusions. Additionally, sparse extracellular amyloid plaques are noted in the cortical gray matter.
- Immunostains for alpha synuclein show Lewy bodies and Lewy neurites with a score of 3 in the substantia nigra, locus coeruleus, cranial nerve nuclei IX / X, nucleus basalis of Meynert, transentorhinal cortex and cingulate cortex. Lewy body and Lewy neurite pathology are present with a score of 4 in the amygdala and with a score of 2 in the temporal and frontal cortex. Lewy body and neurite pathology is present with a score of 1 in the parietal cortex.
- Silver stains demonstrate moderate numbers of neurofibrillary tangles in the entorhinal cortex, amygdala and hippocampus, with sparse neurofibrillary tangles in the temporal cortex (B2). Moderate neuritic plaques are noted in the frontal, temporal and parietal cortices (C2). Immunostaining for beta amyloid is positive in the thalamus but negative in the midbrain and cerebellum (A2).
- Comment: This corresponds to a diffuse / neocortical type Lewy body disease. The likelihood that the pathologic findings are associated with a dementia with Lewy bodies clinical syndrome based on the degree of Lewy body and Alzheimer neuropathologic changes is high (Neurology 2005;65:1863).
Differential diagnosis
- Parkinson disease with dementia:
- Neuropathologically indistinguishable
- Clinically, Parkinsonism precedes cognitive changes by more than 1 year
- Alzheimer disease:
- Neurofibrillary tangles and amyloid beta plaques
- Mixed pathology (i.e., Alzheimer neuropathologic changes and Lewy body pathology) is very frequent (J Geriatr Psychiatry Neurol 2002;15:210)
- Multiple system atrophy:
- Glial cytoplasmic inclusions of alpha synuclein predominate
- Neuronal synuclein pathology is not characteristic, although it can be encountered
- Progressive supranuclear palsy:
- Glial and neuronal phospho-tau pathology predominantly in perirolandic cortex, putamen, pallidum, subthalamic nuclei, brainstem and cerebellar dentate nucleus
- Synuclein pathology is not a feature
- Neurodegeneration with brain iron accumulation (NBIA):
- Some subtypes show Lewy bodies (e.g., neuroaxonal dystrophy due to PLA2G6 mutations)
- Age of onset in childhood or early adulthood
- Iron accumulation in globus pallidus and substantia nigra with spheroids are a major component
- Postencephalitic Parkinsonism:
- Tauopathy with severe loss of neurons in the substantia nigra postencephalitis
- Synuclein pathology is not a feature
Board review style question #1
What feature is essential for a diagnosis of dementia with Lewy bodies?
- Dementia
- Lewy bodies in the brainstem
- Lewy bodies in the hippocampus
- Parkinsonism
Board review style answer #1
A. Dementia. Dementia with Lewy bodies is a clinicopathological term that should include a clinical diagnosis of dementia and distribution of Lewy body pathology that explains the neuropsychiatric manifestations (i.e., neocortical and limbic structures) (Neurology 2005;65:1863). Answers B and C are incorrect because Lewy body pathology alone is insufficient for a diagnosis of dementia with Lewy bodies. Answer D is incorrect because Parkinsonism, while a clinical feature of dementia with Lewy bodies, is not essential for the diagnosis.
Comment Here
Reference: Dementia with Lewy bodies
Comment Here
Reference: Dementia with Lewy bodies
Board review style question #2
Board review style answer #2
A. Alpha synuclein. Lewy bodies contain a multitude of components, however, their main constituent is misfolded alpha synuclein (Nature 1997;388:839). Answers C and D are incorrect because although neurofilaments and synaptophysin have been detected in Lewy bodies, these proteins show either weak IHC expression (i.e., synaptophysin) or haven’t been shown to be implicated as the main structural constituent or as a pathogenic driver (Mol Neurobiol 2013;47:495, J Comp Neurol 1991;309:150, Brain Res 1994;634:339). Answer B is incorrect because although lipid structures such as disrupted organelles are abundant in Lewy bodies, other lipid structures are also involved such as general vesicles and other membrane fragments (e.g., autophagosomes) (Nat Neurosci 2019;22:1099). The proportional contributions of these lipid structures are not clear and their pathogenic role in protein seeding, oligomerization or Lewy body maturation is not elucidated.
Comment Here
Reference: Dementia with Lewy bodies
Comment Here
Reference: Dementia with Lewy bodies