Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Mallikarjunappa SS, Gonzalez RS. Pseudomembranous colitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/colonAAcolitis.html. Accessed April 26th, 2024.
Definition / general
- Nonspecific pattern of injury occurring as a result of decreased oxygenation, disrupted blood flow and endothelial injury (Cleve Clin J Med 2016;83:361)
- Often occurs following use of broad spectrum antibiotics
Essential features
- Formation of a pseudomembrane resulting from multiple disease states and overlying colonic mucosa
- Most commonly caused by Clostridioides difficile (formerly Clostridium difficile)
- Often treated with antibiotics but may rarely require surgery
Terminology
- Also termed antibiotic associated colitis
- Pseudomembrane is a layer of fibropurulent exudate made of mucus and acute inflammatory cells originating from inflamed and erupting crypts
ICD coding
- ICD-10: A04.7 - enterocolitis due to Clostridium difficile
Epidemiology
- C. difficile is the most common cause of pseudomembranous colitis and is the most common cause of nosocomial infectious diarrhea in the U.S. (Gastroenterology 2019;157:1492)
- Overall incidence has been increasing (Gastroenterology 2019;157:1492)
Sites
- Colon
Pathophysiology
- For cases caused by C. difficile
- Usage of other antibiotics disrupts normal gut flora, allowing C. difficile to establish a presence
- After colonization, the bacteria produce 2 large exoproteins, toxins A and B
- Following release in the colon, the toxins bind to cell surface receptors and are internalized into the cell
- Glycosylation of small proteins occurs inside the cells involved in signaling and regulating pathways
- Leads to cytoskeleton disruption, causing morphologic cell changes, cytoskeleton activation and cell death
- Infiltration of neutrophils and inflammatory cell reaction occurs due to tight junctions getting affected
- Pseudomembranous formation occurs by toxin activation of the native immune system and by activation of macrophages and monocytes, leading to release of proinflammatory cytokines like interleukin 1, interleukin 8, tumor necrosis factor and leukotriene B4 (Dis Mon 2015;61:181)
Etiology
- Most common cause is C. difficile
- Other causes include infectious agents, ischemia, medications and inflammatory mucosal diseases (see table below) (Dis Mon 2015;61:181, Cleve Clin J Med 2016;83:361)
| Drugs | Medications | Infections | Inflammatory conditions |
| Cocaine Glutaraldehyde | Cisplatin Cyclosporine A Docetaxel 5-Fluorouracil Nonsteroidal anti-inflammatory drugs | Thomasclavelia ramosum Cytomegalovirus Entamoeba histolytica Escherichia coli O157:H7 Klebsiella oxytoca Plesiomonas shigelloides Salmonella species Schistosoma mansoni Shigella species Staphylococcus aureus Strongyloides stercoralis | Behçet disease Collagenous colitis Inflammatory bowel disease Ischemic colitis |
Clinical features
- Most common symptom is diarrhea
- Acute symptoms like abdominal pain and cramping
- Fever and leukocytosis indicate severe disease
- Rarely, perforation, toxic megacolon, colonic ischemia and septic shock (hypotension) can occur (Crit Care Clin 2013;29:827)
Diagnosis
- Clinical clues such as history of hospitalization and utilization of antibiotics are important
- Lab investigations are used to confirm C. difficile associated disease (see Laboratory)
- In more fulminant disease cases, endoscopy and radiology are useful
- Endoscopic visualization of the colonic mucosa shows pseudomembrane formation
- Computerized tomography (CT) scan of the abdomen / pelvis is the most common imaging modality used for pseudomembranous colitis (Crit Care Clin 2013;29:827)
Laboratory
Radiology description
- CT scan of abdomen / pelvis shows pericolonic fat stranding, accordion sign (high attenuation oral contrast in the colonic lumen alternating with low attenuating inflamed mucosa) and target sign (varying degrees of attenuation of the IV contrast material in the mucosa) (Crit Care Clin 2013;29:827)
- In some cases, pneumatosis or perforation can also be seen (Crit Care Clin 2013;29:827)
Radiology images
Prognostic factors
- Risk factors for recurrent disease include older age, female sex, additional courses of antibiotics / chemotherapy, use of gastrointestinal (GI) medications or procedures, prolonged hospital stays and prior episodes of recurrent pseudomembranous colitis (Dis Mon 2015;61:181)
Case reports
- 20 year old man with a history of psoriasis presented with a 3 week history of nonbloody diarrhea (BMJ Case Rep 2021;14:e240890)
- 30 year old woman with clindamycin use and acute onset of watery, nonbloody diarrhea (Gastroenterology 2019;156:883)
- 61 year old man with a history of stage IIIa adenocarcinoma of the lung presented with diarrhea (Gastroenterology 2019;157:1492)
- 72 year old woman presented with sudden onset watery diarrhea (Acad Pathol 2023;10:100076)
- 77 year old man with abdominal pain and watery diarrhea (Medicine (Baltimore) 2019;98:e15004)
Treatment
- Supportive care and antimicrobial therapy in most cases
- Supportive care includes fluid resuscitation
- Metronidazole and vancomycin are the main antibiotics used
- Small number of fulminant cases need surgical management (Crit Care Clin 2013;29:827)
Gross description
- White to yellow plaques and nodules on the colonic mucosa, which can coalesce
Gross images
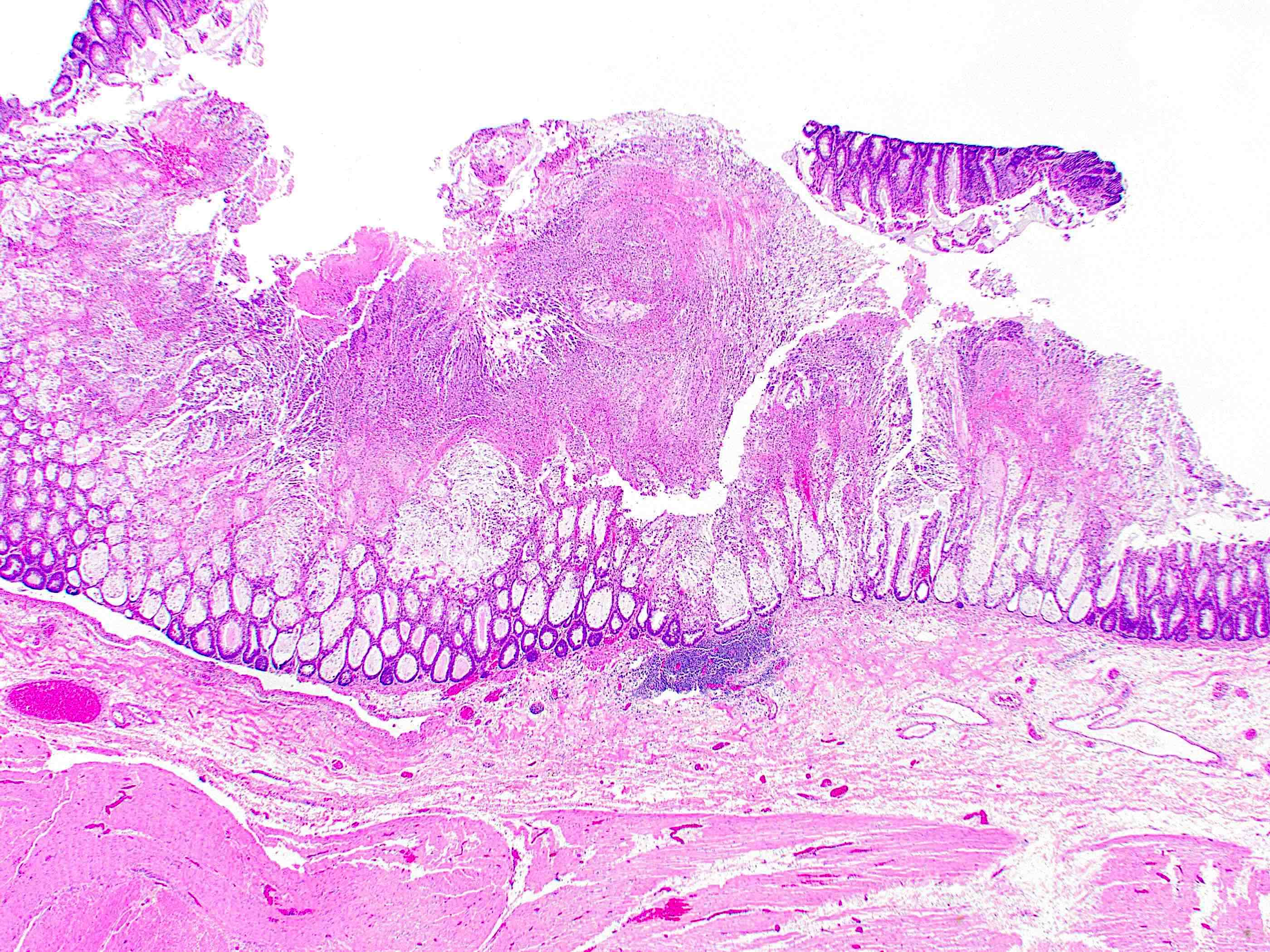
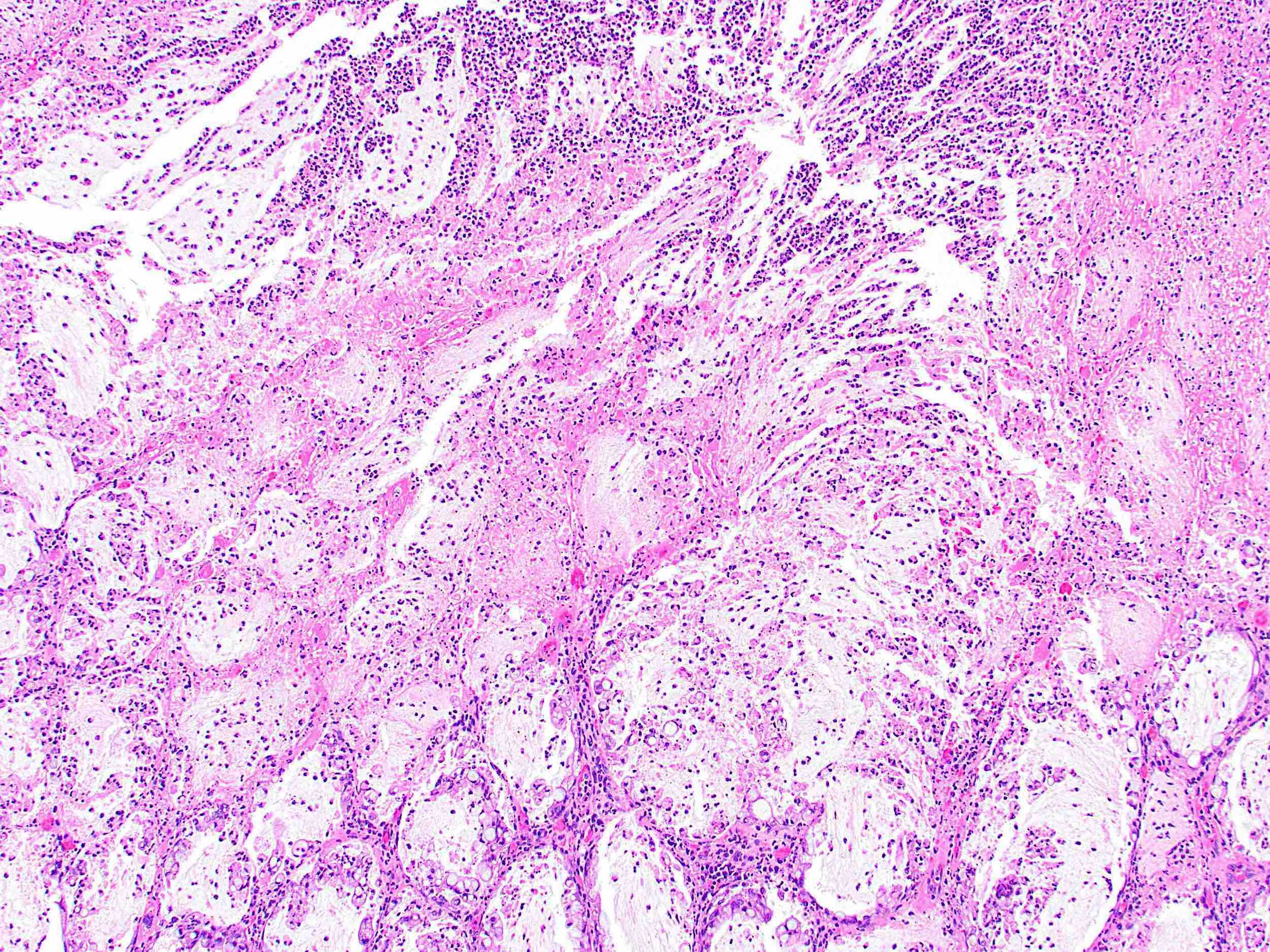
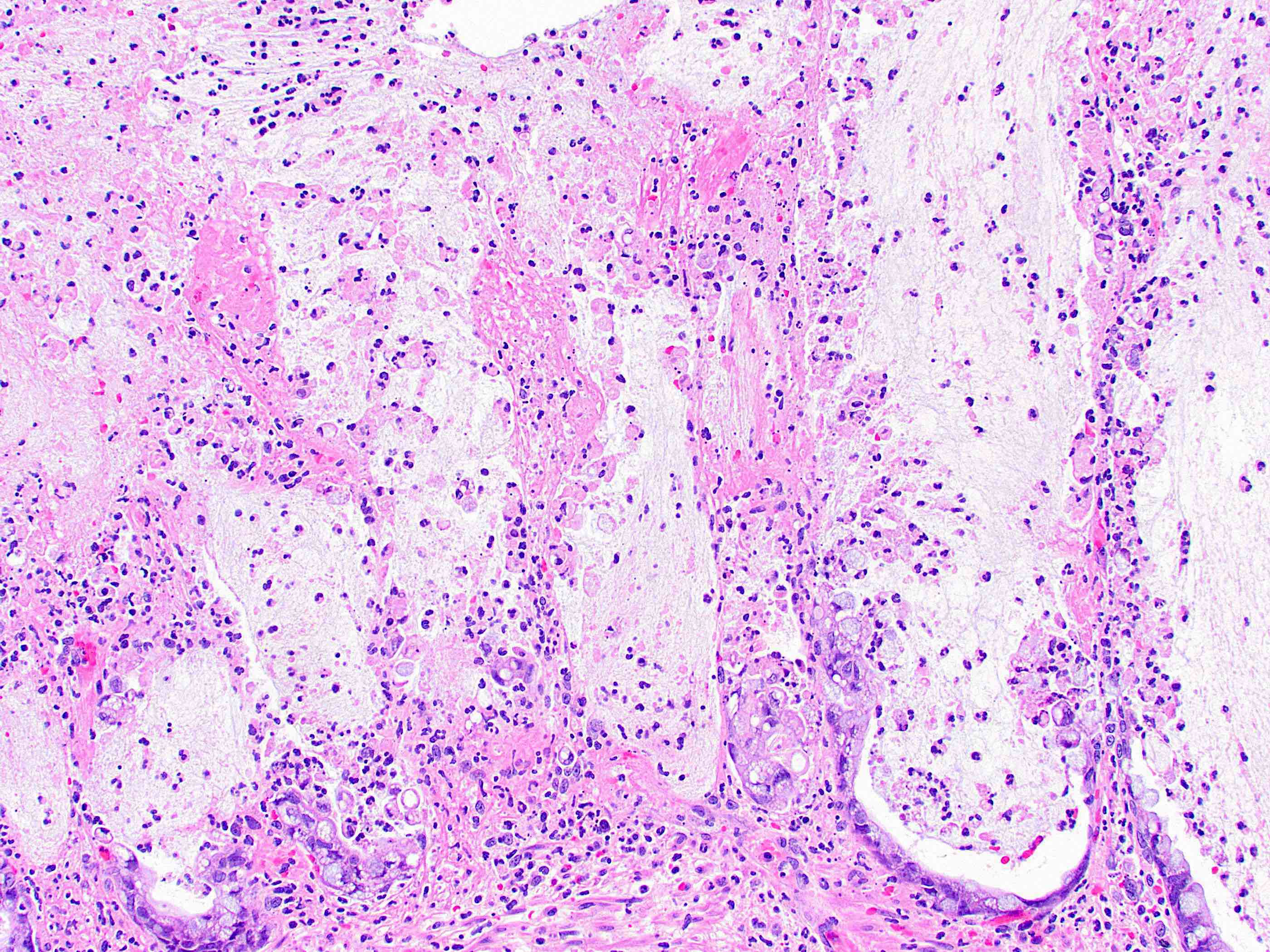
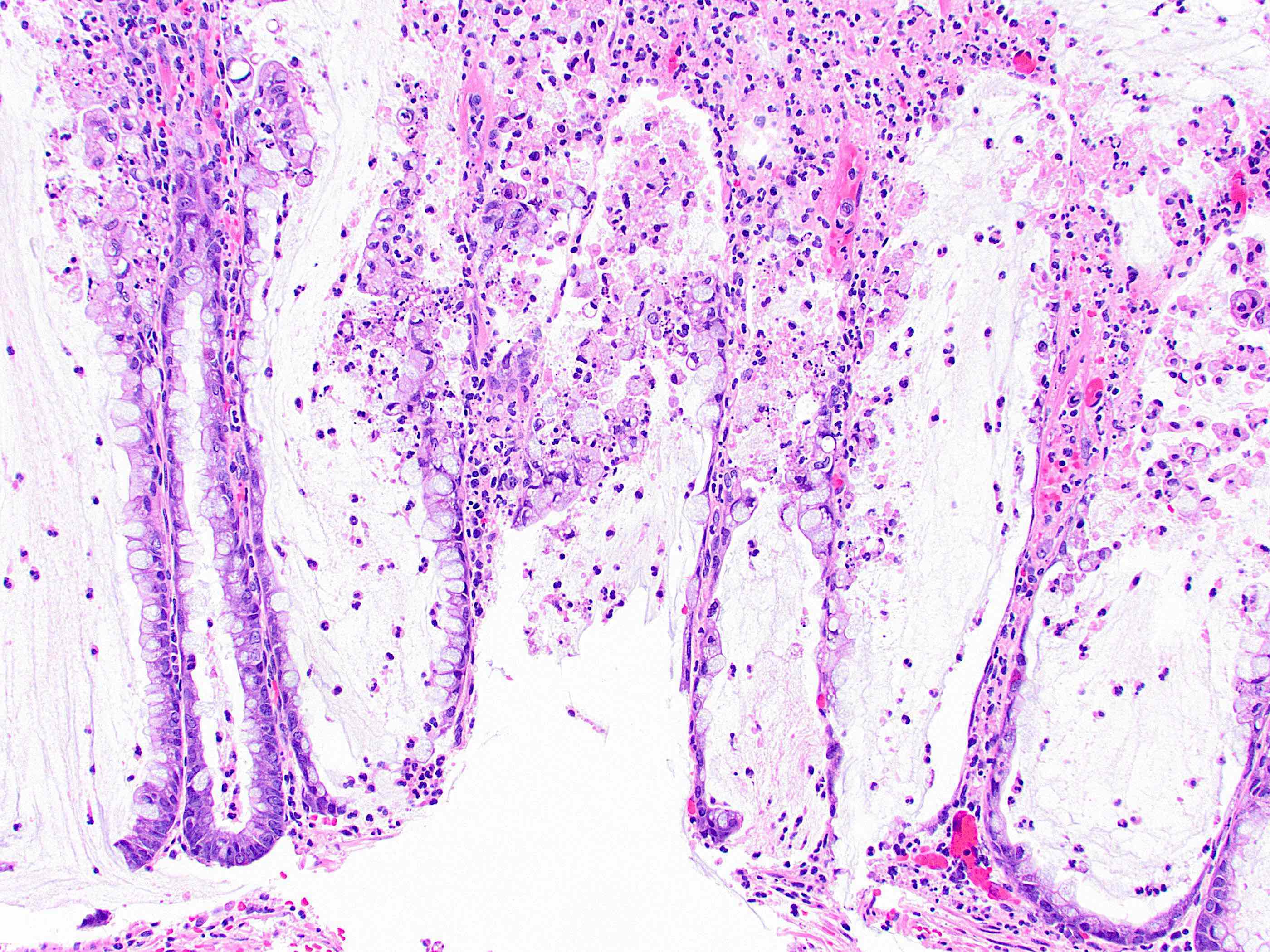
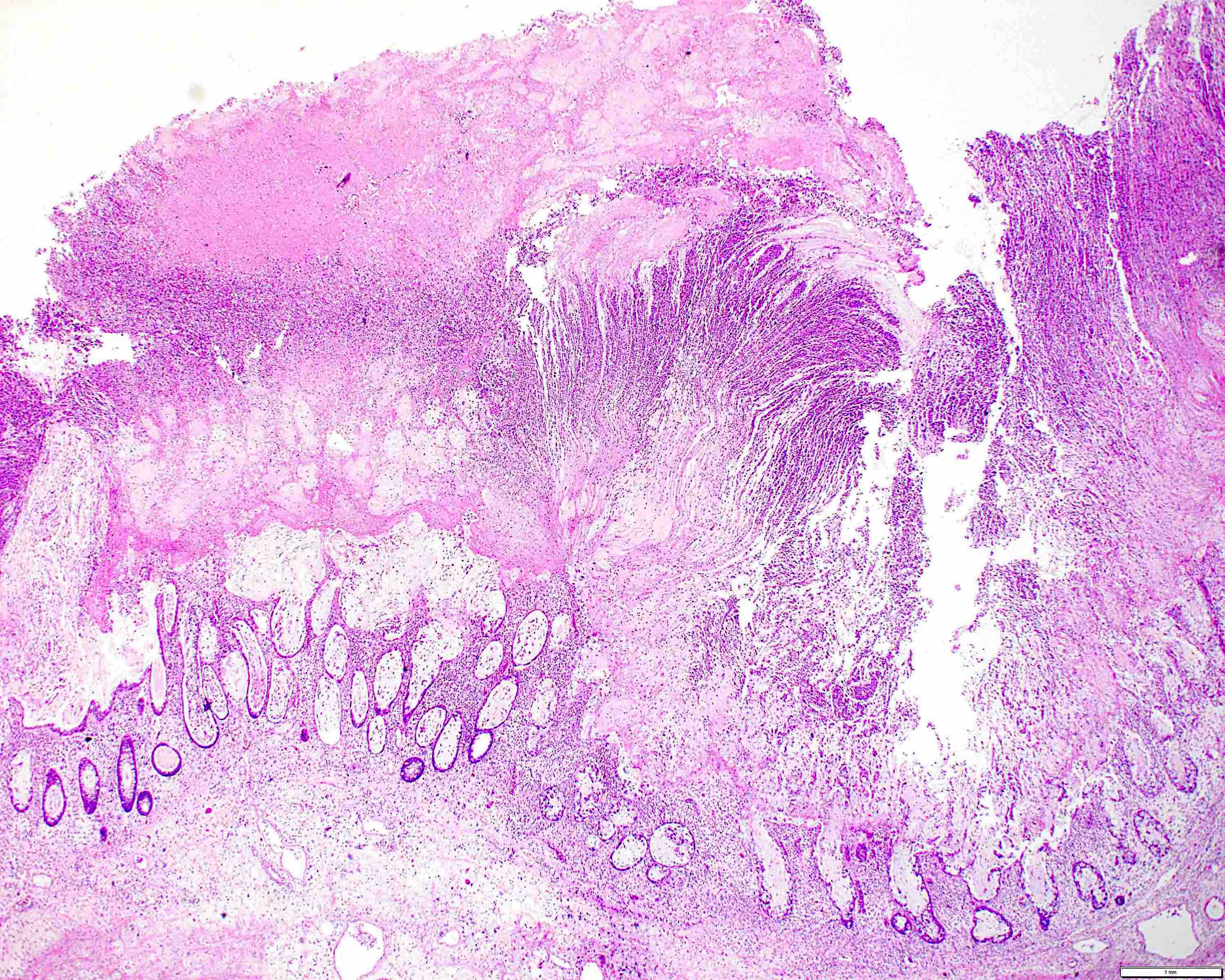
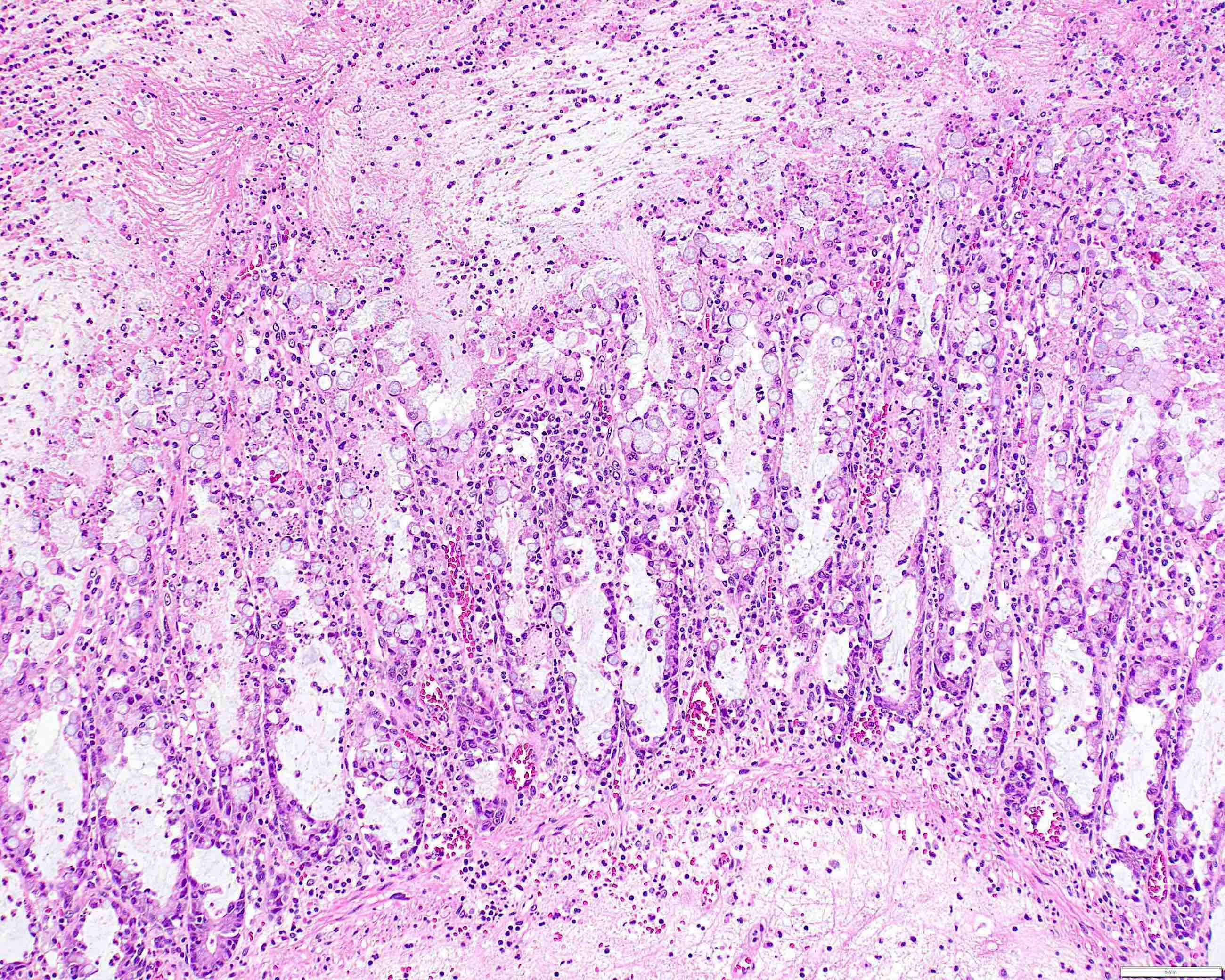
Microscopic (histologic) description
- Mix of inflammatory and ischemic features
- Volcano or mushroom-like eruption of fibrin, mucin and inflammatory cells, mainly neutrophils, forming a pseudomembrane overlying the injured mucosa
- Epithelium shows ischemic appearance with attenuated / withered crypts
- Enterocytes may rarely show signet ring change, somewhat mimicking signet ring cell carcinoma (Am J Surg Pathol 2004;28:1111)
- Superficial lamina propria contains dense neutrophils and some capillary fibrin thrombi
- Adjacent epithelium may show active colitis or hemorrhage (Pathologe 2022;43:16)
Microscopic (histologic) images
Sample pathology report
- Colon, biopsy:
- Colonic mucosa with sloughed epithelium, neutrophils, mucin, fibrin deposition on the surface and crypts (see comment)
- Comment: Given the reported history of recent antibiotic use and the appearance of a pseudomembrane on colonoscopy, the findings are most consistent with pseudomembranous / antibiotic associated colitis.
Differential diagnosis
- Ischemic colitis:
- Most often involves the watershed areas like splenic flexure and rectosigmoid
- Lamina propria hyalinization and atrophic microcrypts are more common in ischemic colitis (Am J Surg Pathol 1997;21:706)
- Infectious colitis by pathogens other than C. difficile:
- Cannot be determined by histology alone
- Identification of the responsible pathogens by lab investigations like stool assay, PCR or culture
- Signet ring cell carcinoma:
- Should show destructive invasion into the colonic mucosa or wall, not just signet ring shaped epithelial cells lining the native crypt spaces (Am J Surg Pathol 2004;28:1111)
Board review style question #1
Which of the following is a histologic feature of pseudomembranous colitis?
- Apoptosis in crypts
- Crypt branching
- Fibrin, mucin and inflammatory cells on the surface with ischemic epithelial changes
- Hyalinization of lamina propria
- Signet ring cells in the lamina propria
Board review style answer #1
C. Fibrin, mucin and inflammatory cells on the surface with ischemic epithelial changes. Fibrin, mucin and neutrophils in the epithelium forming a mushroom shape are classic features of pseudomembranous colitis. Answer A is incorrect because apoptosis of crypts is seen in medication induced colitis and graft versus host disease. Answer B is incorrect because crypt branching is a feature of chronic colitides such as inflammatory bowel disease. Answer D is incorrect because hyalinization of lamina propria is seen in ischemic colitis. Answer E is incorrect because invasive signet ring cells are found in adenocarcinoma.
Comment Here
Reference: Pseudomembranous colitis
Comment Here
Reference: Pseudomembranous colitis
Board review style question #2
Board review style answer #2
D. Use of broad spectrum antibiotics. Broad spectrum antibiotic use leads to colonization of C. difficile, causing pseudomembranous colitis. Answer E is incorrect because it is seen more commonly in older individuals. Answers A, B and C are incorrect because autoimmune conditions, TP53 mutation and HLA DQ2 presence are not associated with pseudomembranous colitis.
Comment Here
Reference: Pseudomembranous colitis
Comment Here
Reference: Pseudomembranous colitis