Table of Contents
Definition / general | Essential features | Terminology | Clinical applications | Advantages of telecytology (ROSE) | Disadvantages of telecytology (ROSE) | Implementation | Validation of telecytology (ROSE) | Other uses of telecytology | Diagrams / tables | Digital cytology education material | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Baskota SU, Lajara S, Landau M. Telecytology. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/informaticstelecytology.html. Accessed May 5th, 2024.
Definition / general
- Telecytology has been implemented for rapid off site evaluation of cytology specimens, which improves efficiency by saving time spent in evaluation and subsequent triage of specimens for appropriate investigations and management by pathologist
Essential features
- Telecytology has been integrated into the clinical practice of cytopathology for rapid off site evaluation of cytology specimens
- Other use cases of telecytology include primary diagnosis, teleconsultation and education / research
- To reproduce 3 dimensional (3D) structure of cytology specimen, digital cytology requires advanced scanning modes (Z stacking or extended focus) or video microscopy
Terminology
- Rapid on site evaluation (ROSE): refers to immediate microscopic evaluation of fine needle aspiration material, traditionally performed on site, to assess for adequacy and to triage the obtained material for ancillary studies (Cytopathology 2014;25:322)
- Static image transmission: 1 person (e.g. cytotechnologist or house staff) on site takes representative photomicrographs of the slide and sends them electronically to the pathologist
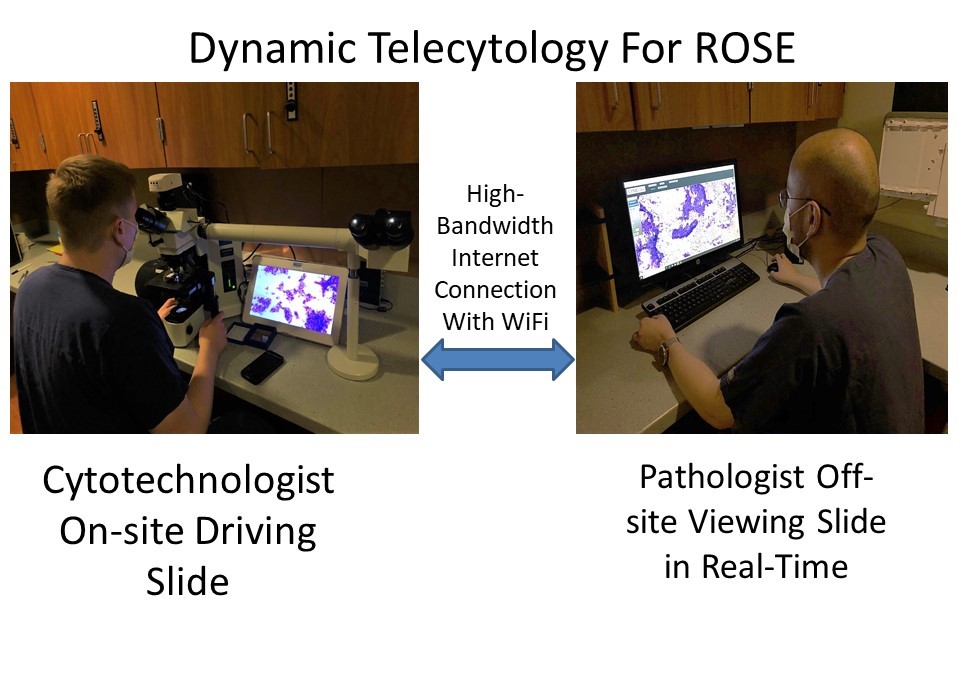
- Dynamic microscopy: 1 person on site controls the microscope (position, magnification and focus) with a camera that streams the field of view to a remote computer, which a pathologist uses to view the slide in real time
- Whole slide imaging: digitization of glass slide images by scanning them at different planes and magnifications;
digital cytology requires advanced scanning mode to correctly reproduce 3D structure of cytology specimen (J Pathol Inform 2010;1:15)
- Z stacking: images captured from multiple planes along the z axis above / below the optimal focal plane are used to create a 3D structure (Z stack) image
- Extended focus mode (also known as EDF, extended depth of field): multiplane scanning with integration of the best focused image at each tile into a final single plane file
Clinical applications
- Rapid on site evaluation: telecytology is being used increasingly for rapid on site evaluation (J Am Soc Cytopathol 2018;7:1)
- Intraoperative consultation of neuropathology specimens with smears and touch imprints preparations (J Pathol Inform 2020;11:13)
Advantages of telecytology (ROSE)
- No time wasted by pathologist to travel to site
- No delay for clinical team while waiting for pathologist to arrive
- Pathologists can do other activities during wait time between needle passes, increasing their efficiency
- A single pathologist can provide consultation for multiple concurrent ROSE procedures occurring at different sites
- Multiple users can login at the same time for a single case review; helpful in trainee education and second opinion
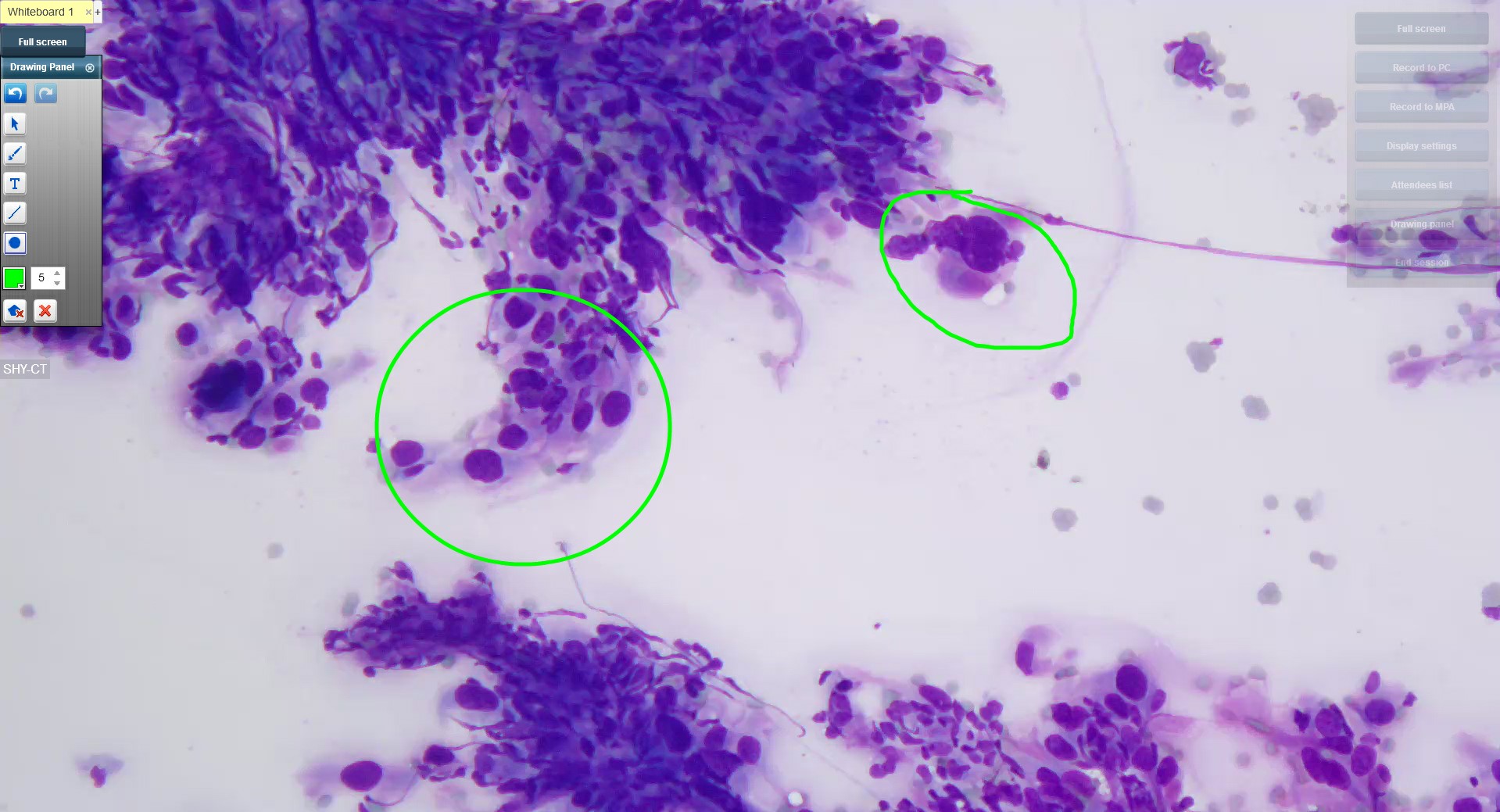
- Different users can annotate images at the same time to facilitate consultation (see Images section, image 1)
Disadvantages of telecytology (ROSE)
- Requires competent cytotechnologists or house staff to accurately identify areas of interest to present to pathologist (locator skills)
- Can slow the procedure if only 1 cytotechnologist or house staff is present for the procedure, since a single person cannot stain slides and screen slides at the same time
- Requires purchase of specialized software and hardware
Implementation
- Implementation of telecytology for ROSE is cost effective and time saving (J Am Soc Cytopathol 2018;7:1)
- Telecytology can be done by:
- Static telecytology: images of preselected microscopic fields are transferred as digital images to the pathologist
- This is the simplest telecytology set up and requires a microscope fitted with a digital camera connected to the computer and an internet network
- Static telecytology is useful in resource limited settings
- However, it limits the pathologist's ability to examine the entire slide
- Time consuming: the staff on site has to screen the slide, take photomicrographs and then send them electronically; turnaround time may not be appropriate for ROSE
- Two dimensionality: inability to adjust the plane of focus to fully examine 3 dimensional cell clusters
- Cost effective
- Dynamic telecytology: requires similar hardware to static microscopy, a microscope, high definition (HD) digital microscopy camera, computer with HD digital live streaming software, secure internet network with sufficient bandwidth and connectivity (see Images section, image 2)
- With a skilled cytotechnologist on site, a pathologist in his / her office can review selected areas of the slide or even the entire slide much more quickly than static images
- Time efficient: since the cytotechnologist and pathologist review the slide together in real time, the method is faster than static images; there is also less delay in the transmission of images compared to whole slide imaging
- Requires technical expertise: familiarity with the operational software and initial training for smooth operation
- Dependent on locator skills of on site cytotechnologist
- Cost effective and users can be easily trained
- Robotic microscopy: robotic microscopes allow full remote control of the slides including position, magnification and focus; in the absence of on site cytotechnologists, the slides can be prepared by pathology assistants or laboratory technicians (J Pathol Inform 2020;11:13)
- Requires high speed internet
- Can be useful in low volume settings
- Whole slide imaging: rarely used for ROSE
- Time consuming due to need for z stacking (high resolution scanning in multiple focal planes) to adequately image 3 dimensional cell clusters
- Requires tremendous bandwidth
- Requires on site personnel to prepare and stain direct smears
- Might not be the most cost effective option (J Am Soc Cytopathol 2018;7:1)
- Static telecytology: images of preselected microscopic fields are transferred as digital images to the pathologist
Validation of telecytology (ROSE)
- College of American Pathologists requires validation to be done for clinical practice in the United States, regardless of the telecytology platform
- Recommends validation to be performed by the pathologists, who will be using the telecytology system
- Should be performed in a setup similar to the usual work environment
- A minimum of 60 cases, including positive and negative cases that reflect the spectrum and complexity of routine cases per application should be used; the digital and glass slides should be reviewed at least 2 weeks apart and the diagnostic concordance is evaluated
- Whenever there is a significant change to the system that may potentially impact the interpretation of digital slides (e.g., new scanner is used, major hardware / software upgrade), the validation process should be repeated using a smaller set of cases (20 cases) (Arch Pathol Lab Med 2013;137:1710)
- Center for Medicare and Medicaid Services (CMMS) considers ROSE as a clinical test, hence a Clinical Laboratory Improvement Amendments (CLIA) number and a New York State clinical laboratory permit (in New York sites) are necessary
Other uses of telecytology
- Primary diagnosis:
- Whole slide imaging (WSI) for primary diagnosis in cytology is currently not FDA approved
- Some WSI scanners do not allow for z stacking or EDF to address the issues associated with imaging cytology specimens
- However, some authors have investigated the utility of WSI for primary diagnosis and they have shown good concordance with review of glass slides (Acta Cytol 2020;64:323)
- Consultation:
- Telecytology using static images or WSI is being used for remote telepathology consultation
- Implementation of the two systems depends on the availability of resources (e.g. hardware, network speeds, manpower) (Diagn Cytopathol 2019;47:28)
- Education:
- Telecytology, combined with remote conferencing and learning management platforms, has been received positively by cytology program students (J Am Soc Cytopathol 2020;9:579)
Diagrams / tables
Digital cytology education material
- Cytoatlas
Board review style question #1
Digital cytology images as whole slide imaging requires which technique to enable the assessment of 3 dimensional cell clusters in multiple planes?
- Image flattening
- Smoothening
- Two dimensionality
- Z stacking
Board review style answer #1
Board review style question #2
Board review style answer #2