Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Steele J, Hecht JL. Maternal vascular malperfusion. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/placentauteroplacentalinsuff.html. Accessed May 13th, 2024.
Definition / general
- Conditions in which the functional capacity of the placenta is impaired due to altered maternal blood flow to the intervillous space
- Clinical presentation ranges from fetal growth restriction to preeclampsia
- References: Arch Pathol Lab Med 2016;140:698, Pediatr Dev Pathol 2004;7:237
Essential features
- Conditions in which the functional capacity of the placenta is impaired due to altered maternal blood flow to the intervillous space
- 2 patterns: global (small placenta with villous malformation: accelerated villous maturation or distal villous hypoplasia) and segmental (villous infarcts from occluded spiral arteries)
- Gross features: infarction, infarction hematoma
- Microscopic features: accelerated villous maturation, distal villous hypoplasia, syncytiotrophoblastic knots, decidual arteriopathy or acute atherosis
Terminology
- Uteroplacental insufficiency
- Maternal vascular underperfusion
- References: Arch Pathol Lab Med 2016;140:698, Pediatr Dev Pathol 2004;7:237
ICD coding
- ICD-10: O36.5190 - maternal care for known or suspected placental insufficiency, unspecified trimester, not applicable or unspecified
Epidemiology
- Reported incidence range is broad: 8% of low risk nulliparous women to 32.8% of term placentas in an unselected cohort (Obstet Gynecol 2017;130:1112, Am J Obstet Gynecol 2017;216:411.e1)
- Higher incidence with:
- Preterm birth: 47.7 - 50.6% (Placenta 2016;48:56, Am J Obstet Gynecol 2017;216:411.e1)
- Small for gestational age (SGA) and preeclampsia: 47% (Obstet Gynecol 2017;130:1112)
- Black women: odds ratio = 1.14 - 1.58 (Placenta 2018;69:102
- Gestational diabetes: 30.5% (Placenta 2017;49:10)
Sites
- Placenta
Pathophysiology
- Global maternal vascular malperfusion:
- Begins early in pregnancy with a high recurrence in subsequent pregnancy
- Due to abnormal implantation with inadequate spiral artery remodeling, leading to erratic and heterogeneous blood flow (areas of underperfusion and areas of high velocity flow)
- Severity determines the spectrum of disease from growth restriction to preeclampsia (see also: preeclampsia)
- Segmental maternal vascular malperfusion:
- Represents acute / intermittent events, associated with thrombophilia or abruption
- Reference: Placenta 2009;30:473
Etiology
- Maternal vascular disease
- Diabetes
- Chronic hypertension
- Thrombophilia
- Smoking
- Drug abuse (especially cocaine, heroin and methamphetamine)
- Prior history of pregnancy with intrauterine growth retardation
- References: Arch Pathol Lab Med 2016;140:698, Pediatr Dev Pathol 2004;7:237
Clinical features
- Fetal growth restriction
- Preeclampsia
- Prematurity
- Stillbirth
- References: Arch Pathol Lab Med 2016;140:698, Pediatr Dev Pathol 2004;7:237
Diagnosis
- Second and third trimester ultrasound for placental size of the placenta, uterine artery Dopplers or fetal growth delay
- Maternal alpha fetoprotein levels (a fetal liver function test)
- Fetal nonstress test
- References: Arch Pathol Lab Med 2016;140:698, Pediatr Dev Pathol 2004;7:237
Laboratory
- Elevation of maternal serum alpha fetoprotein levels (a test of fetal liver function) (Prenat Diagn 1997;17:305)
- Elevation of maternal serum sFLT1/PlGF ratio (Ultrasound Obstet Gynecol 2018;52:631)
Radiology description
- Ultrasound may show fetal growth restriction and reversal of end diastolic flow on umbilical arterial Doppler (Clin Genet 2006;69:97)
- MRI is not routine but may show restricted diffusion (Radiology 2010;257:810)
Prognostic factors
- Risk of recurrence for severe global maternal malperfusion: 10 - 25%
Case reports
- 20 year old woman with placental infarct, preeclampsia and fetal intrauterine demise (Fetal Diagn Ther 2014;36:154)
- 33 year old woman with early intrauterine growth restriction at 22 weeks gestation and severe preeclampsia (Pulm Circ 2020;10:2045894020970056)
Treatment
- Close surveillance in subsequent pregnancy due to risk of recurrence (10 - 25%)
- Consider acetylsalicylic acid (ASA) therapy and early third trimester placental ultrasound
- Early delivery for growth restriction or poor uterine artery flow (J Obstet Gynaecol Can 2012;34:17)
- Consider screening mother for diabetes, thrombophilia, metabolic syndrome
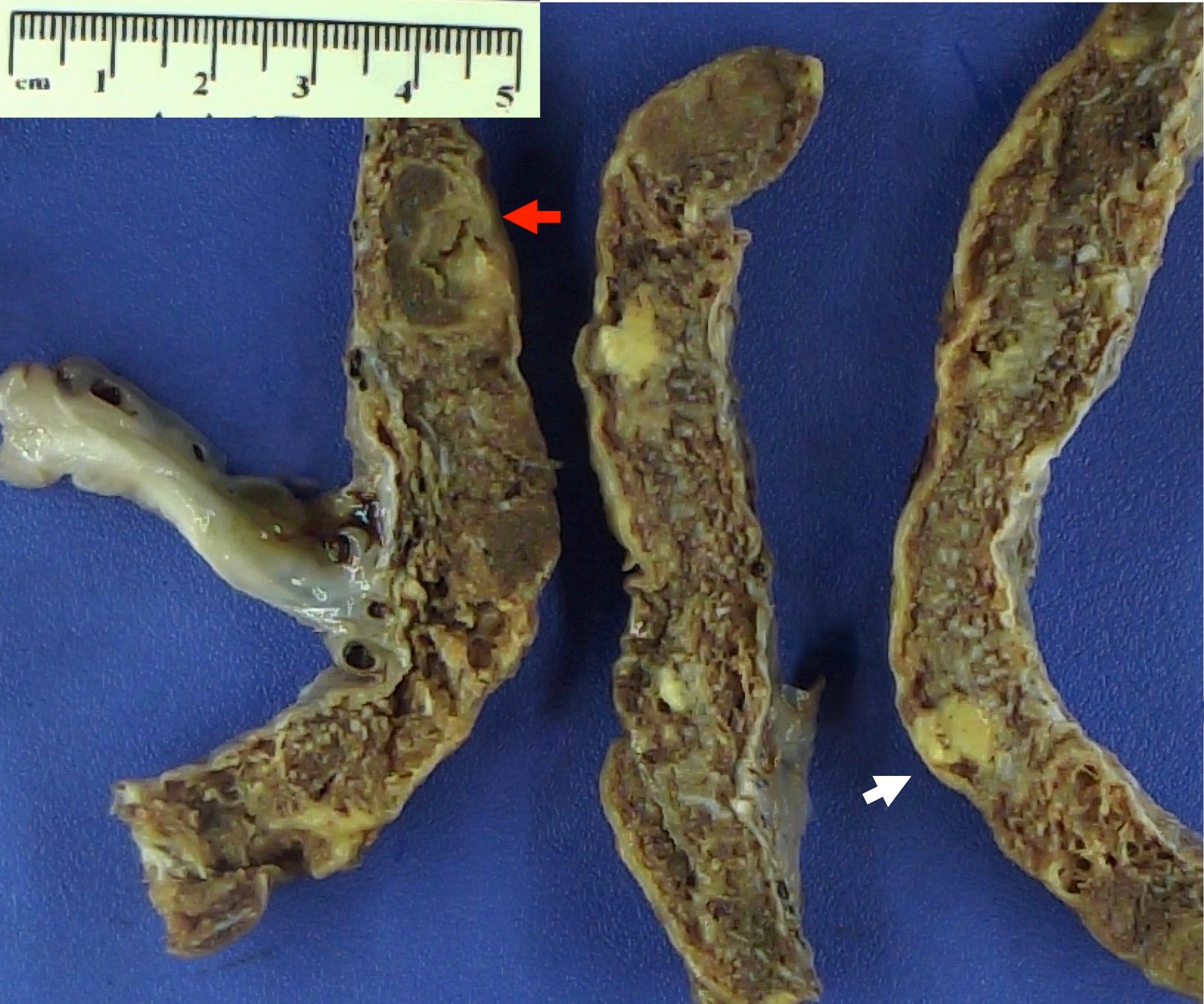
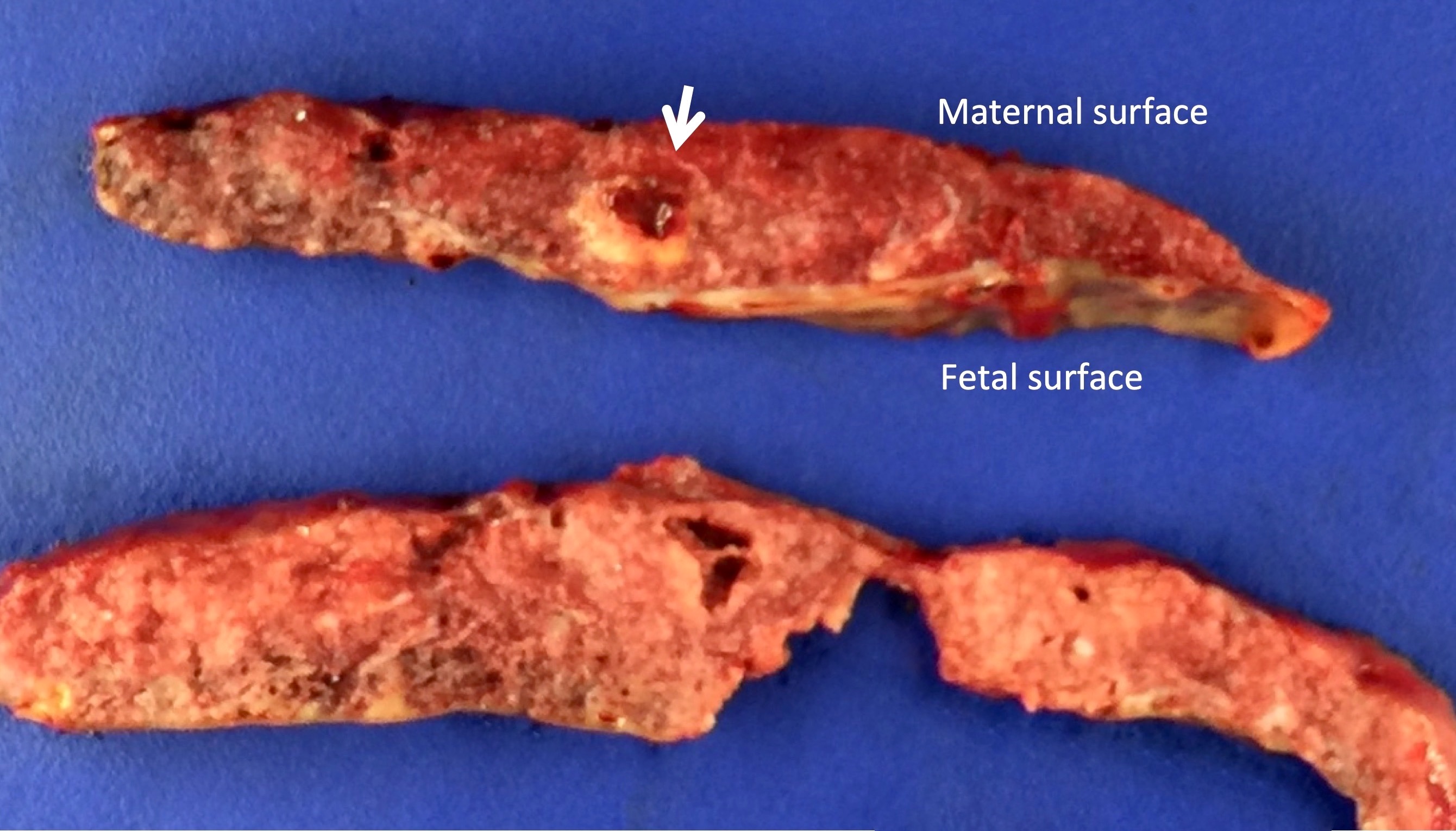
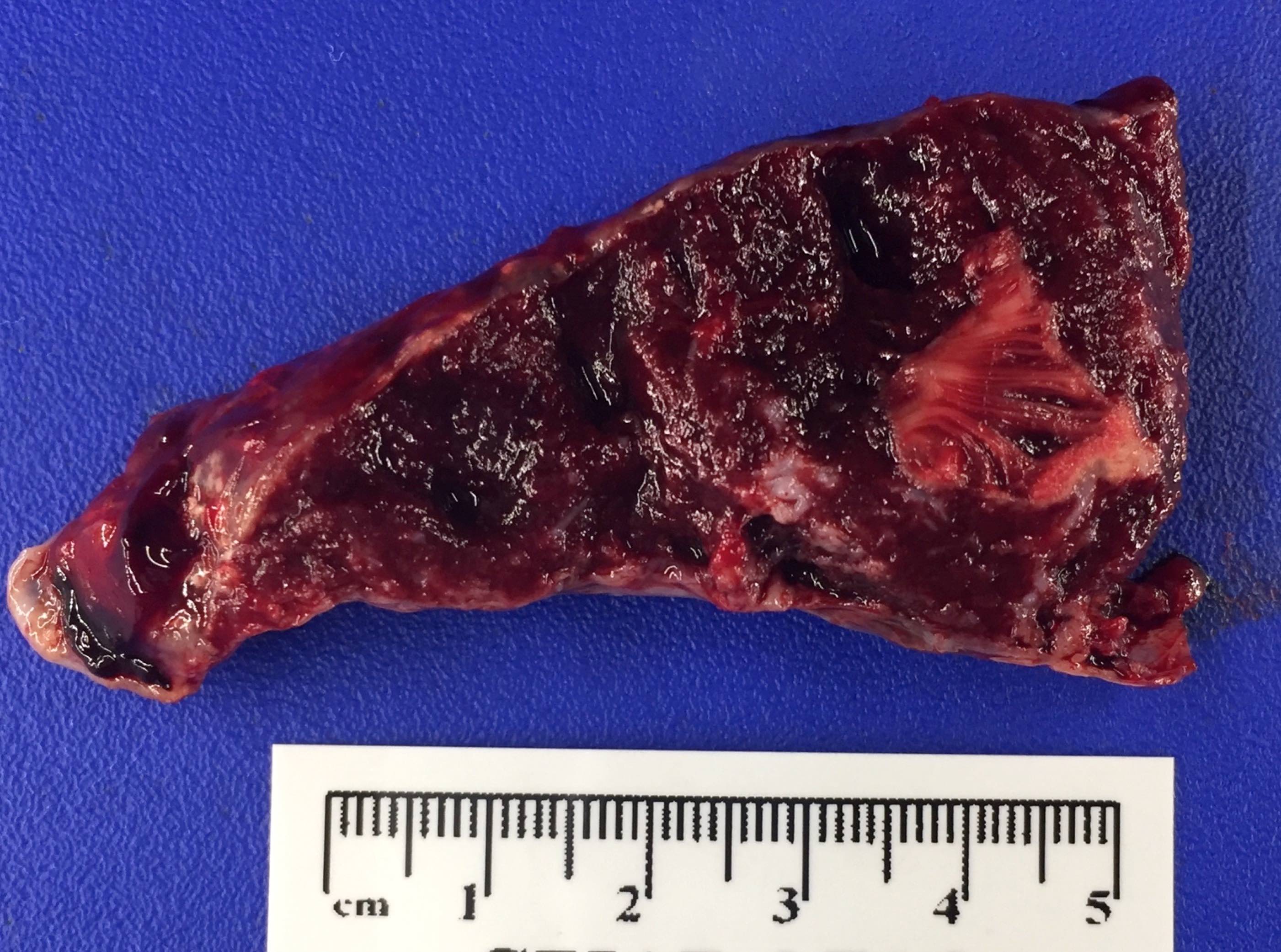
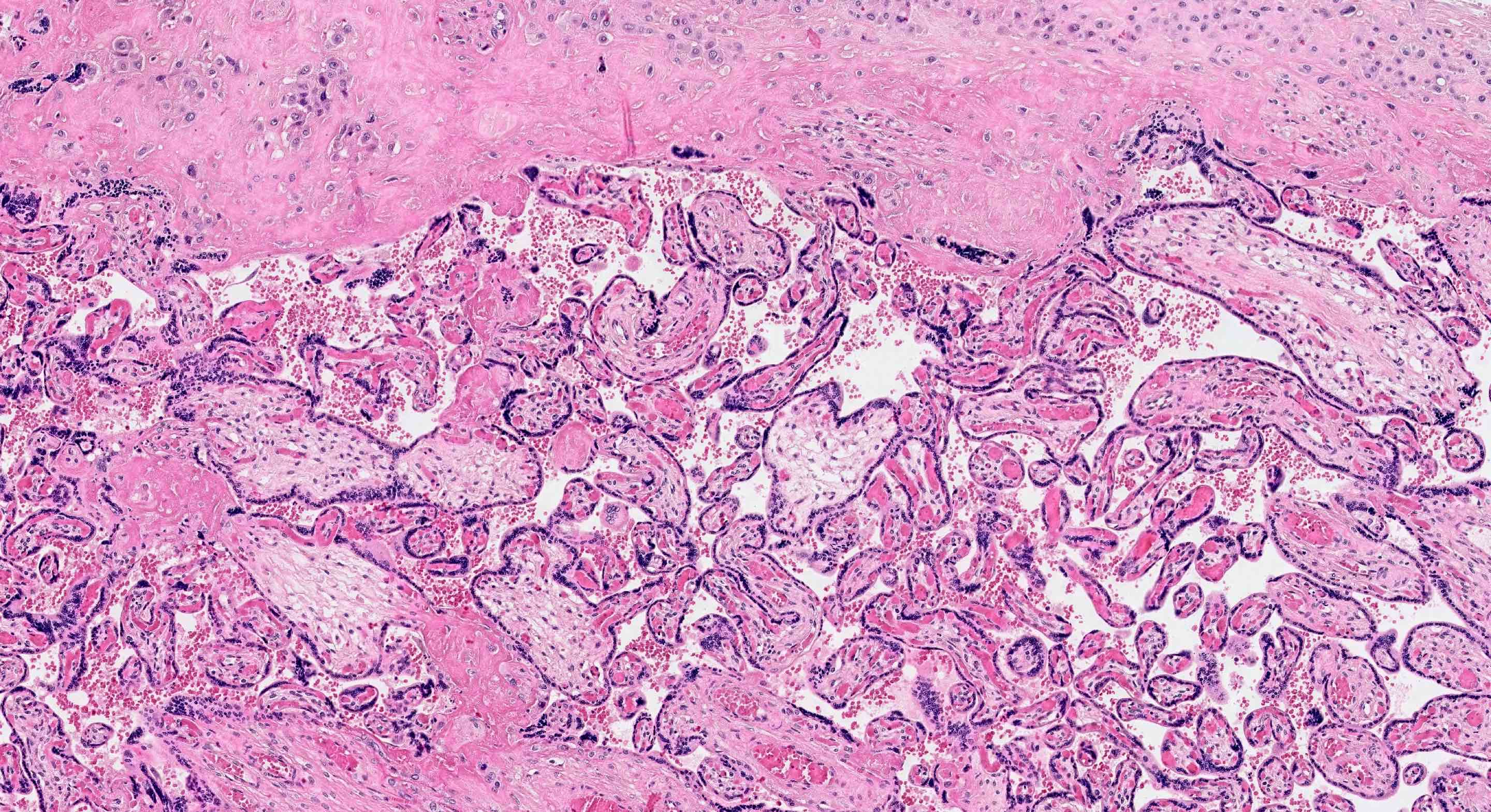
Gross description
- Placenta that is small for gestational age (< tenth percentile of weight)
- Infarction or infarction hematoma, located away from periphery of the disc and of significant size (any infarction in preterm or > 5% of the disc at term)
- Thin umbilical cord (< 8 mm diameter near term), correlating with small disc
- Reference: Placenta 2014;35:696
Gross images
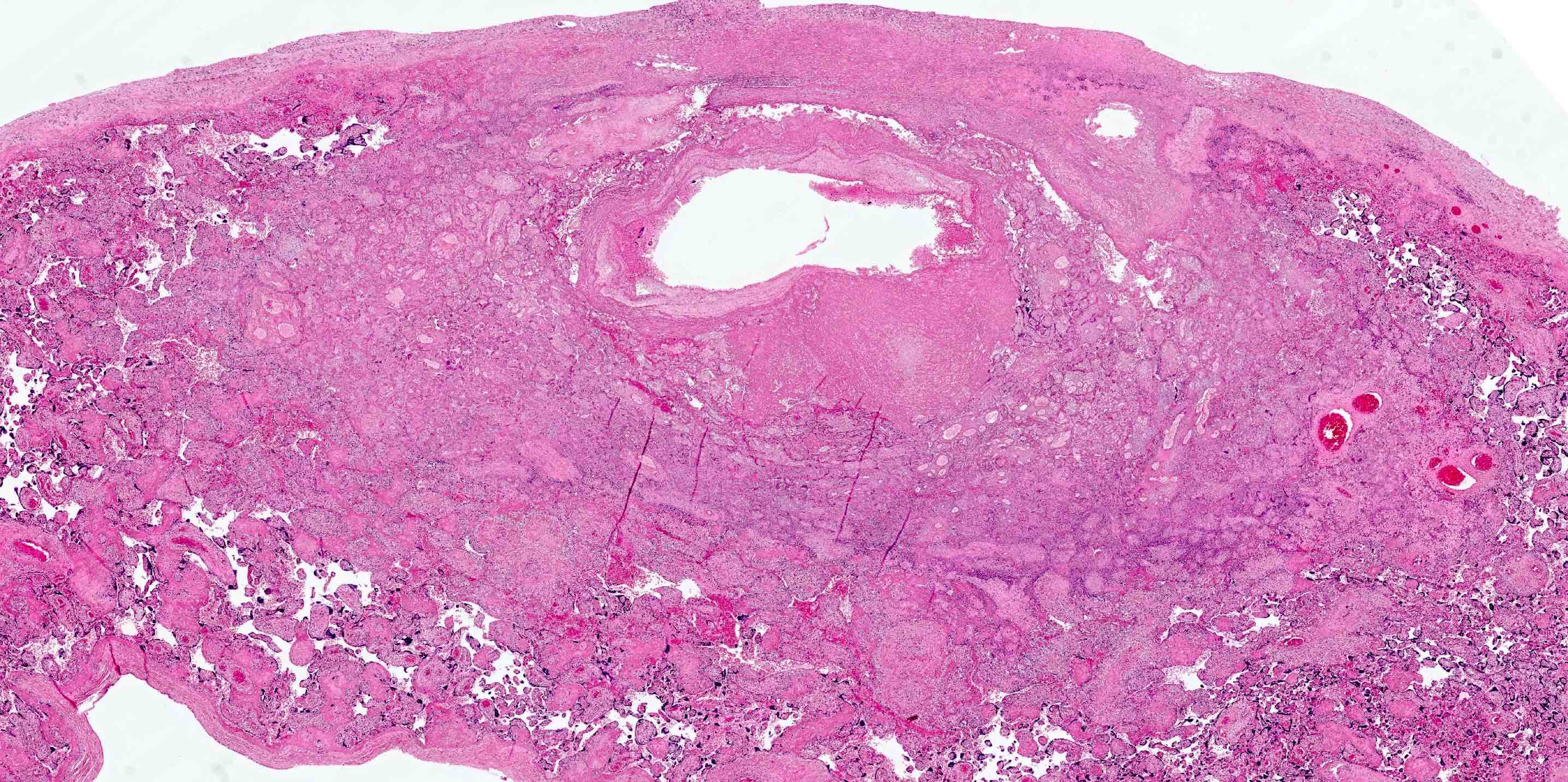
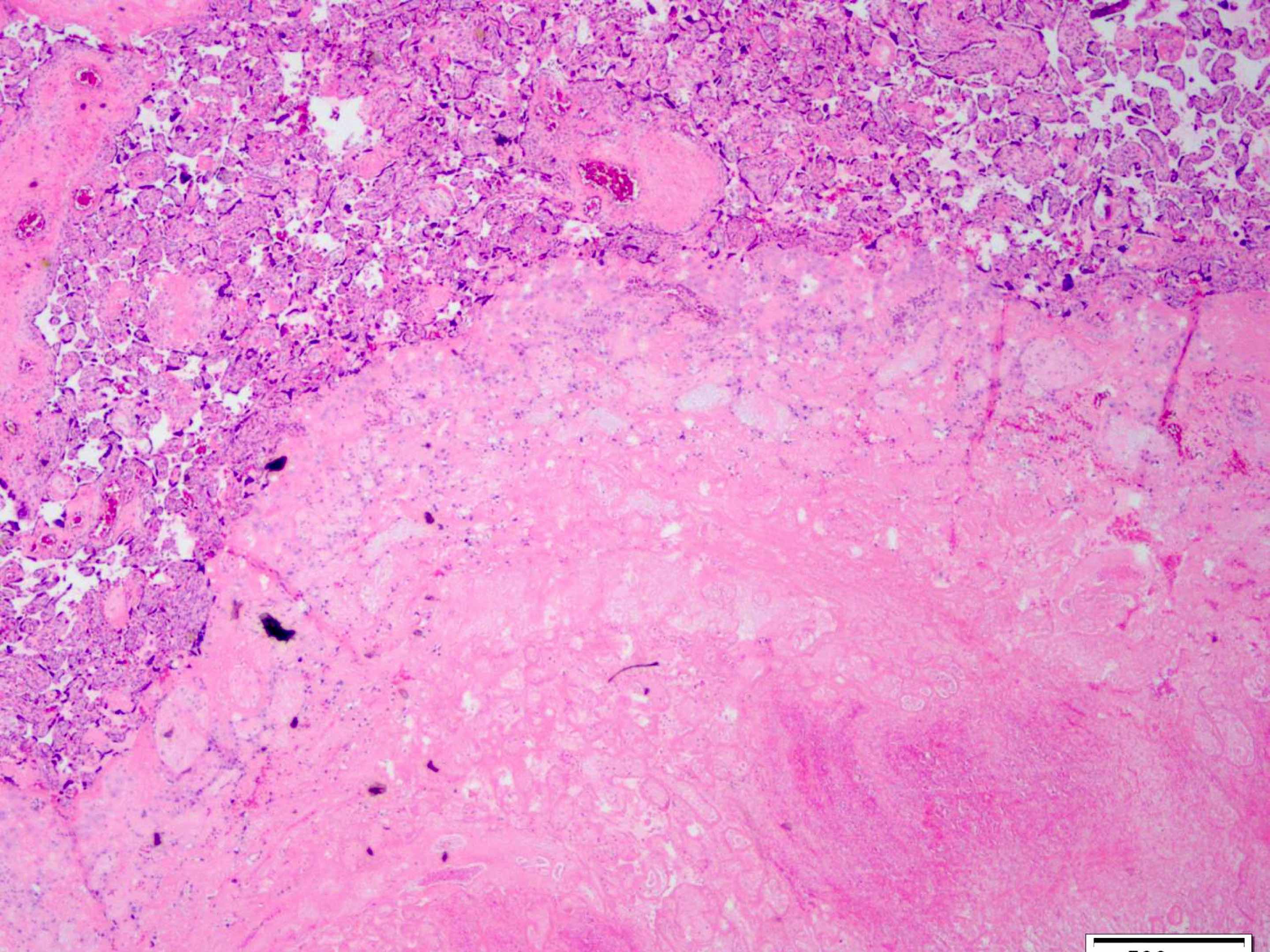
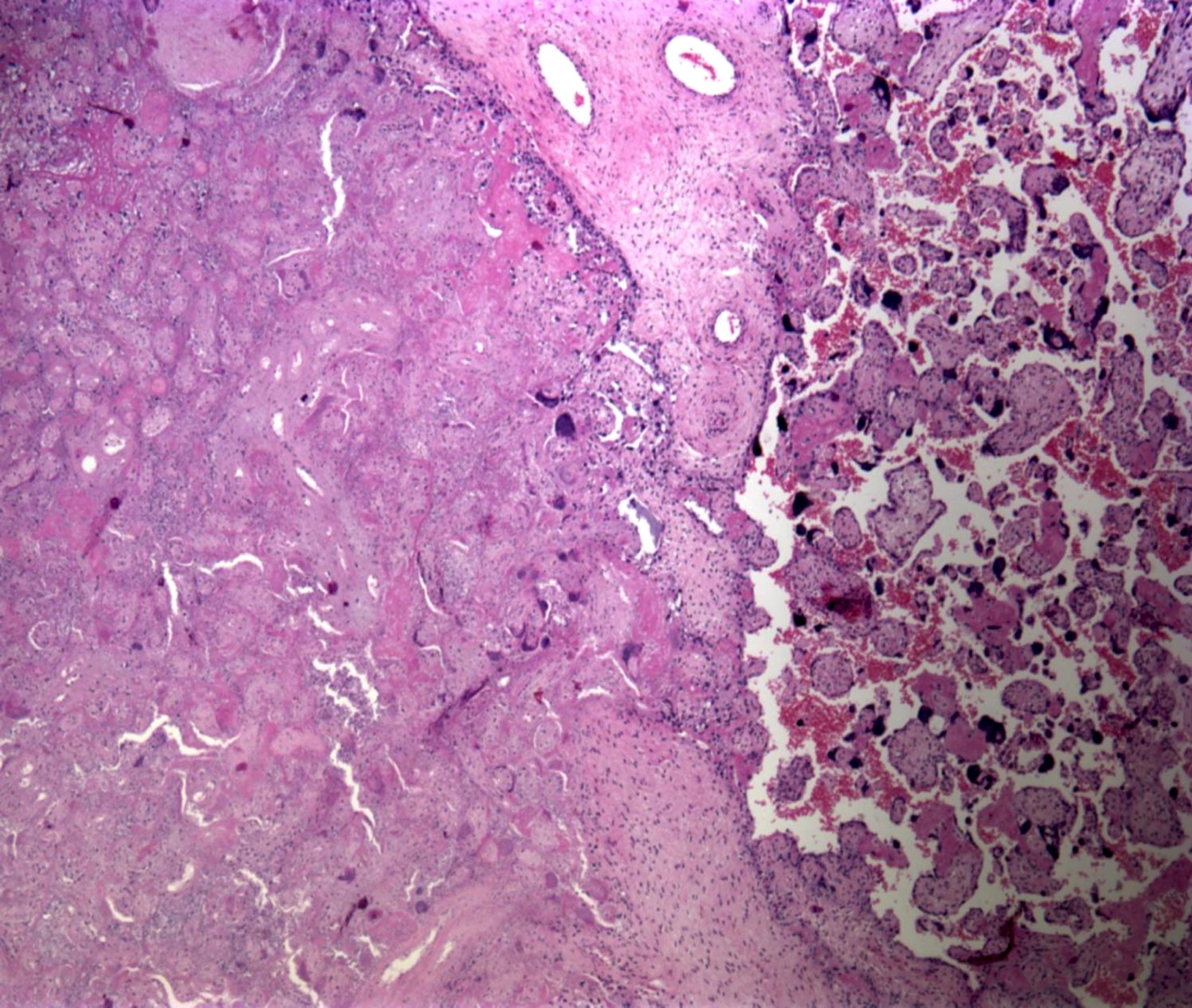
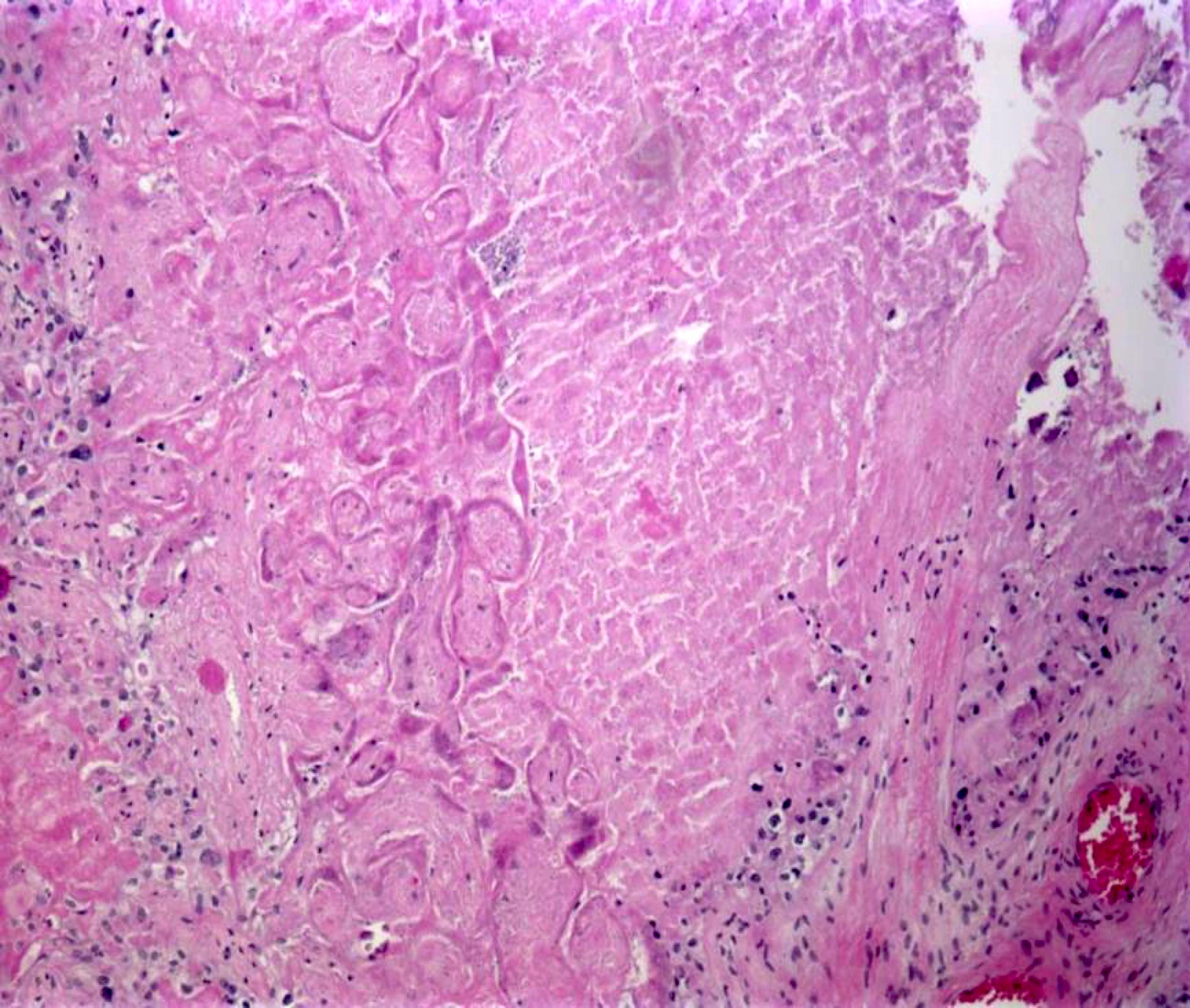
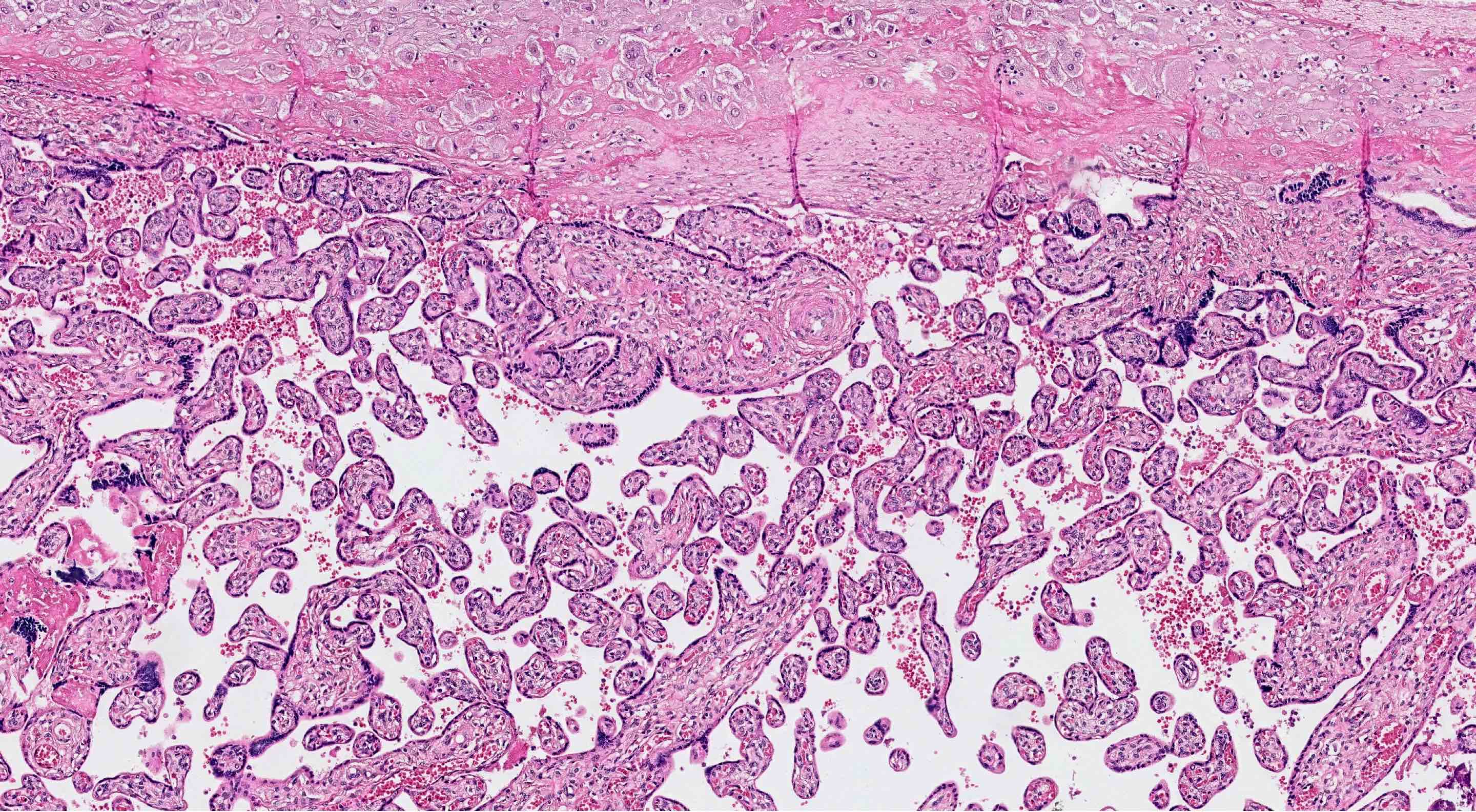
Microscopic (histologic) description
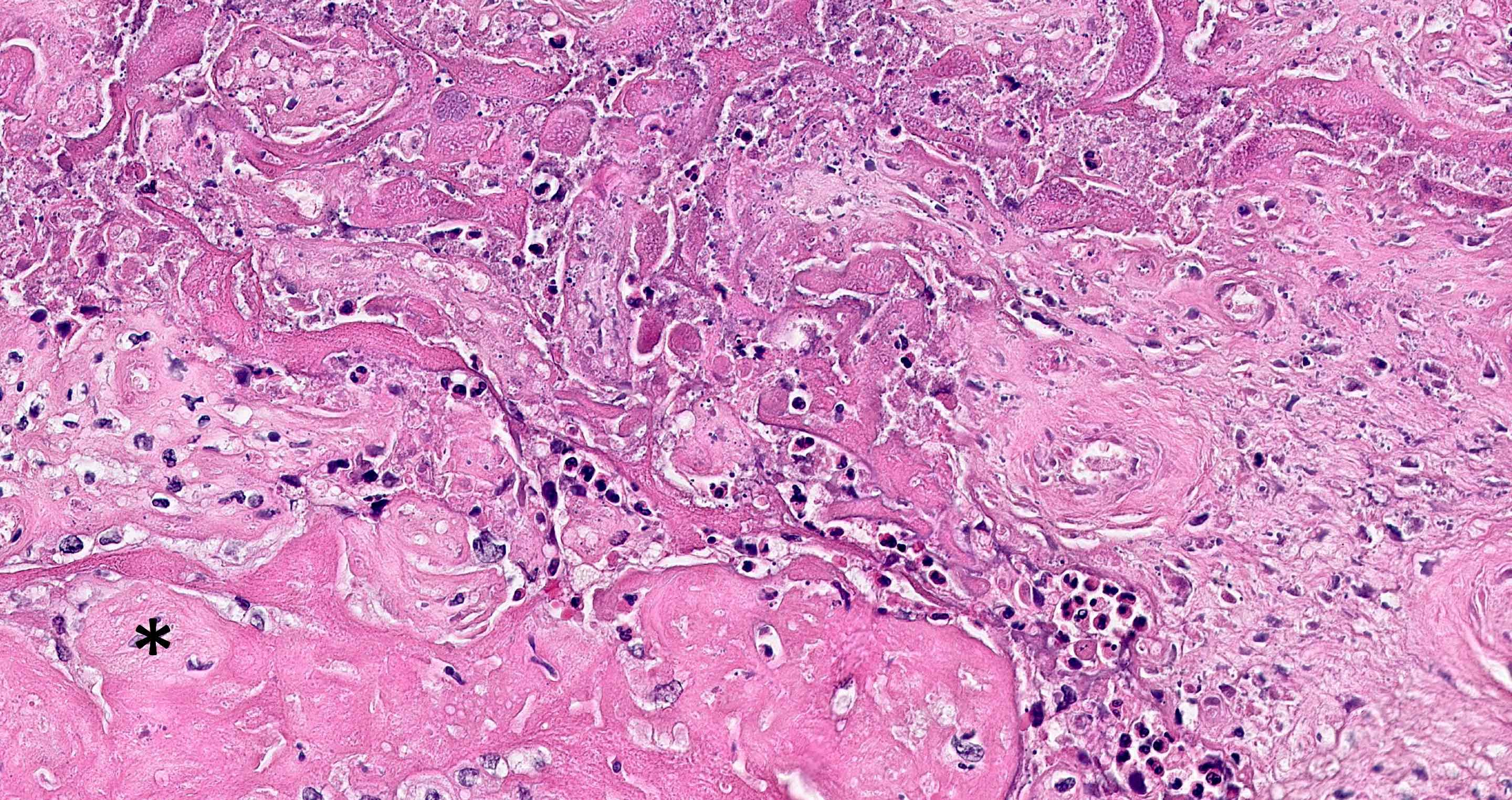
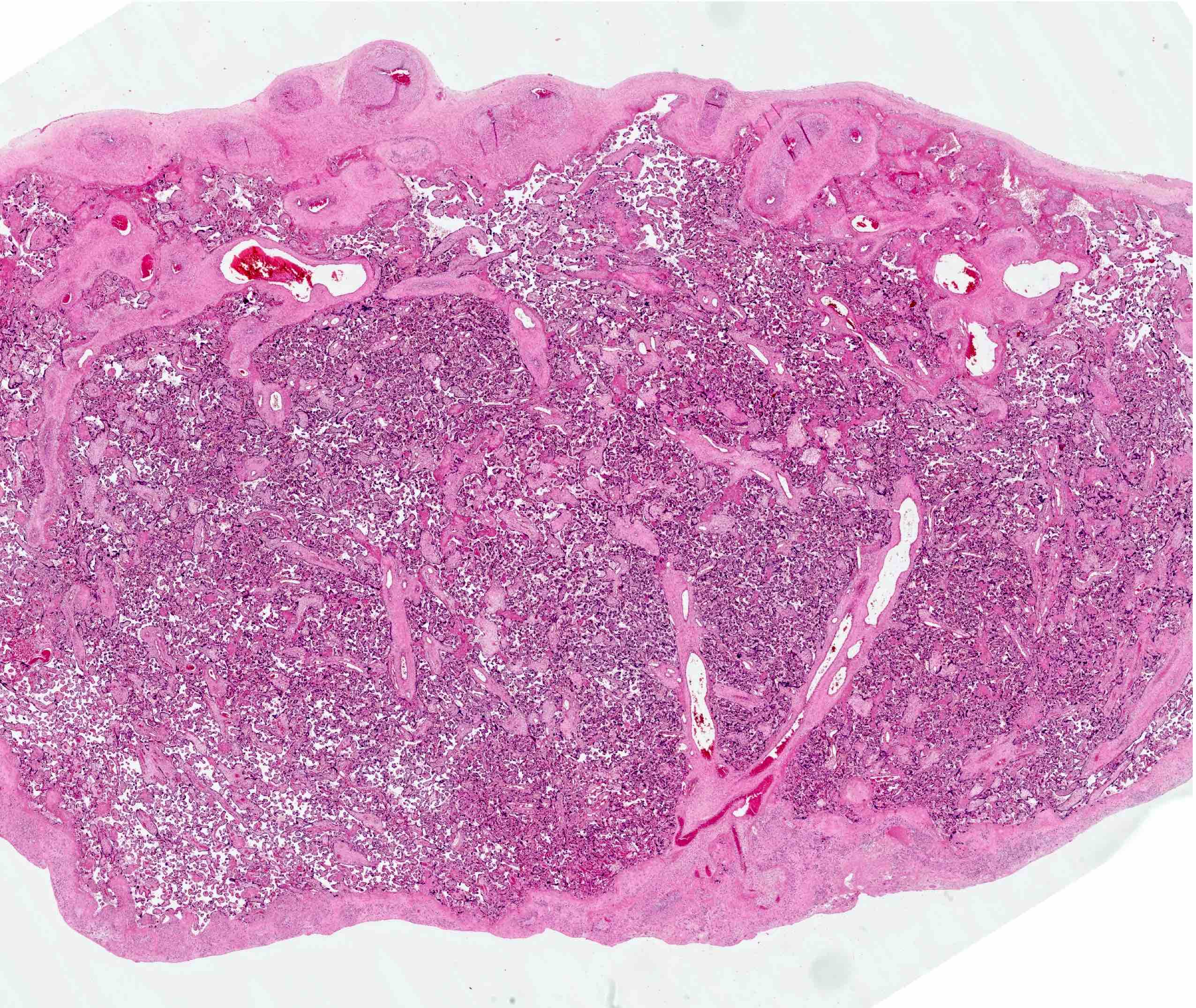
- Altered villous morphology (accelerated villous maturation):
- Villi are small, thin and elongated with increased syncytial knots
- Accelerated maturation should only be diagnosed based on examination of the villi adjacent to the maternal surface
- Appearance of accelerated maturation is identical to the normal appearance of the placental region under the fetal surface; this subchorionic zone serves as a good internal control
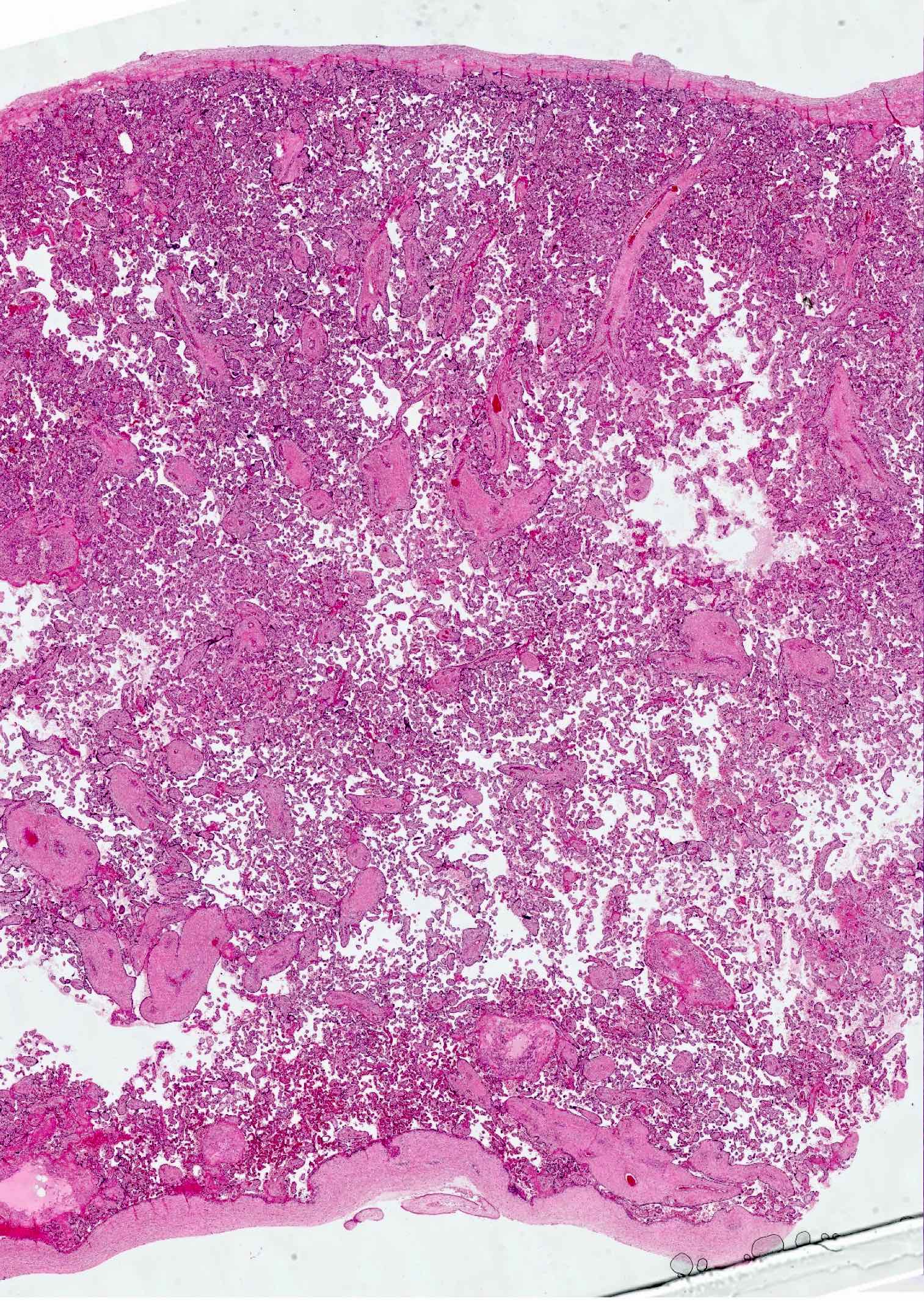
- Altered villous architecture (distal villous hypoplasia):
- More easily recognized before 32 weeks of gestation as a paucity of villi in relation to the surrounding stem villi (increased space around the villi)
- At lower power, this results in a prominence of large stem vessels all the way to the maternal surface
- In second trimester, there is a loss of the normal gradient of larger immature villi to small mature villi as one scans from mid placenta to maternal surface
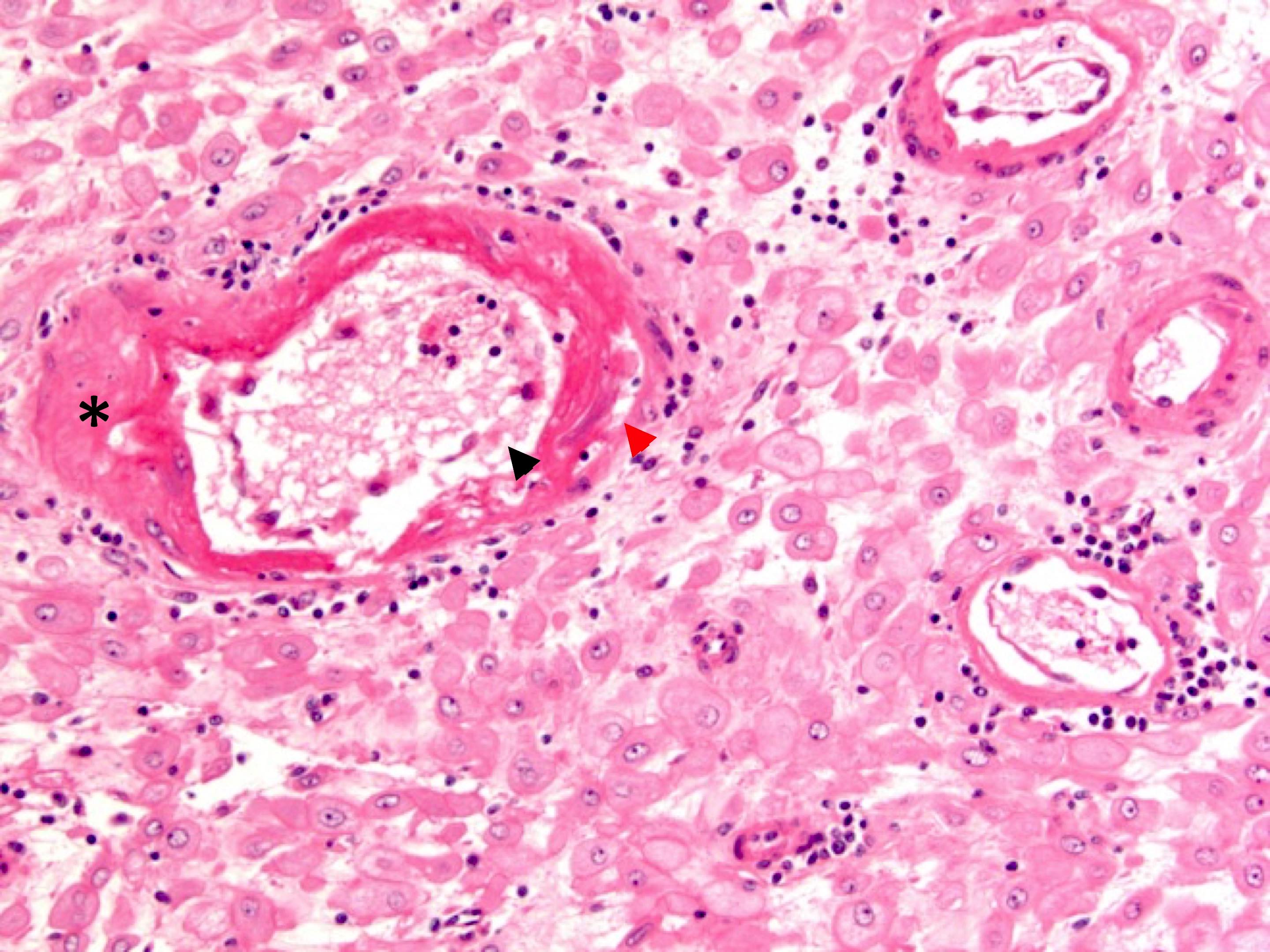
- Syncytiotrophoblastic knots (aka Tenney-Parker change):
- Increase in nuclear clumping and basophilia of the multinucleated cells on the terminal villi
- Knots should generally only be reported if they are present in every 40x field (30% of the villi) or when prominent in a gestation under 36 weeks
- Reference tables for syncytial knots are available (Pediatr Dev Pathol 2010;13:305)
- Decidual arteriopathy
- Acute atherosis: collection of intimal foam cells; best seen in the arteries in placental bed biopsies but may extend into the decidual arteries
- Features often cited but not reproducible: islands of fibrin with extravillous trophoblasts; extensive increase in intervillous fibrin, chorion laeve pseudocyst; decidual necrosis
- Reference: Placenta 2014;35:696
Microscopic (histologic) images
Positive stains
- sFLT1 expression increased in hypoxic villi (those with accelerated maturation and syncytial knots)
Videos
General approach to diagnostic reporting
Clinical relationship to neonatal encephalopathy
Sample pathology report
- Singleton placenta at _ weeks gestational age; _ g (_ percentile):
- Small placenta with features of maternal vascular malperfusion
- Infarction, infarction-hematoma comprising _% of the disc
- Thin umbilical cord
- Accelerated villous maturation
- Distal villous hypoplasia
- Increased syncytiotrophoblastic knots
- Membranes with decidual arteriopathy
Differential diagnosis
- Incidental infarction:
- Any infarction at the disc edge or infarction comprising < 5% of the disc at term
- Features mimicking accelerated maturation:
- Small, widely spaced, elongated villi with increased syncytial knots (normally seen under the fetal plate and in a patchy distribution near the maternal surface in the region of venous drainage)
Additional references
Board review style question #1
A 34 year old woman who is pregnant with her third child and has 2 kids (G3P2002), with a history of gestational hypertension and diabetes, presents for delivery. Her placenta is sent for pathology. Gross examination reveals a placenta that is small for gestational age, with a 2.1 cm infarction within the central placenta (15% of placenta disc). What feature would be most expected on histopathologic examination?
- Chronic intervillositis
- Decreased syncytial knots
- Increased syncytial knots (Tenney-Parker changes)
- Maternal floor infarction
- Normal placenta
Board review style answer #1
C. Increased syncytial knots (Tenney-Parker changes)
Comment Here
Reference: Maternal vascular malperfusion
Comment Here
Reference: Maternal vascular malperfusion
Board review style question #2
Accelerated maturation is a feature of maternal vascular malperfusion. What histologic feature is associated with it?
- Decidual arteriopathy
- Decreased syncytial knots
- High placental weight
- Villlous sclerosis
Board review style answer #2