Table of Contents
Definition / general | Essential features | Terminology | Diagrams / tables | Treatment | Cytology description | Cytology images | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Hang JF. Neoplasm-salivary gland neoplasm of uncertain malignant potential (SUMP). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/salivaryglandsmilanSUMP.html. Accessed May 14th, 2024.
Definition / general
- Fine needle aspiration (FNA) result with cytomorphologic features diagnostic of a neoplasm but because a specific entity cannot be ascertained, a malignant neoplasm cannot be excluded
- 7.2% of all salivary gland FNA (Cancer Cytopathol 2022;130:800)
- Estimated risk of malignancy (ROM) by the Milan system: 35%
- Real world ROM: 42.1% (FNA with surgical follow up), 29.8% (overall) (Cancer Cytopathol 2022;130:511)
- Risk of neoplasm (RON): 96% (Cancer Cytopathol 2022;130:511)
Essential features
- Cellular benign neoplasm (e.g., cellular pleomorphic adenoma [PA])
- Neoplasm with atypical features
- Cellular neoplasm with basaloid features (e.g., pleomorphic adenoma, basal cell adenoma / adenocarcinoma, adenoid cystic carcinoma, epithelial myoepithelial carcinoma, polymorphous adenocarcinoma)
- Cellular neoplasm with oncocytic / oncocytoid features (e.g., Warthin tumor, oncocytoma, mucoepidermoid carcinoma, acinic cell carcinoma, secretory carcinoma)
- Cellular neoplasm with clear cell features (e.g., myoepithelioma, epithelial myoepithelial carcinoma, acinic cell carcinoma, secretory carcinoma, mucoepidermoid carcinoma)
- Low grade carcinoma (e.g., low grade mucoepidermoid carcinoma)
Terminology
- Neoplasm: salivary gland neoplasm of uncertain malignant potential (SUMP) (category IVB)
Treatment
- Due to the high risk of neoplasm, complete surgical excision is usually the standard treatment for symptomatic patients with an FNA result of SUMP
- Imaging evaluation of the tumor border can provide further information regarding the extent of surgery
Cytology description
- SUMP subcategorization
- Recommended by the Milan system (Faquin: The Milan System for Reporting Salivary Gland Cytopathology, 1st Edition, 2018)
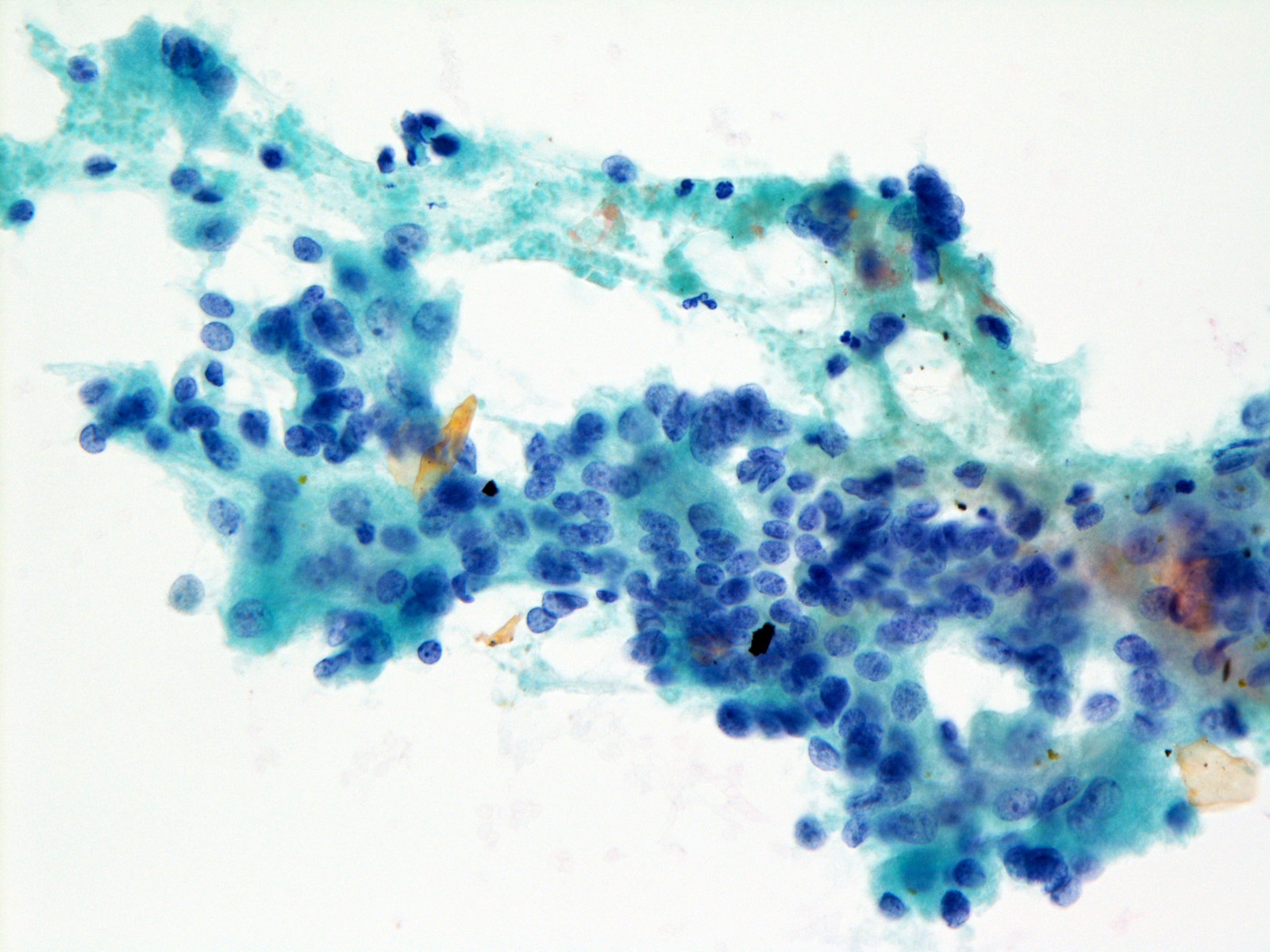
- Cellular basaloid neoplasm
- FNA with a predominant population of cells with scant cytoplasm that confers a basaloid cytomorphology
- Cellular oncocytic / oncocytoid neoplasm
- FNA with oncocytic or oncocytoid features that cannot be classified further
- Cellular neoplasm with clear cell features
- FNA with lesional cells with clear, foamy, granular, vacuolated cytoplasm or any combination thereof
- Uncommon and variably overlapping with the oncocytic / oncocytoid features
- Cellular basaloid neoplasm
- Modified scheme for subcategorizing SUMP proposed by Hang, et al. (Cancer Cytopathol 2022;130:511)
- Basaloid SUMP
- FNA with monotonous basaloid tumor cells with scant cytoplasm and without a purely fibrillary extracellular matrix
- 47.7% of all SUMP FNA
- ROM: 36.5%; RON: 98.1%
- Histology correlation
- Benign neoplasm: pleomorphic adenoma (32.7%) > basal cell adenoma (25%)
- Malignancy: adenoid cystic carcinoma (16%) > basal cell adenocarcinoma (5.8%)
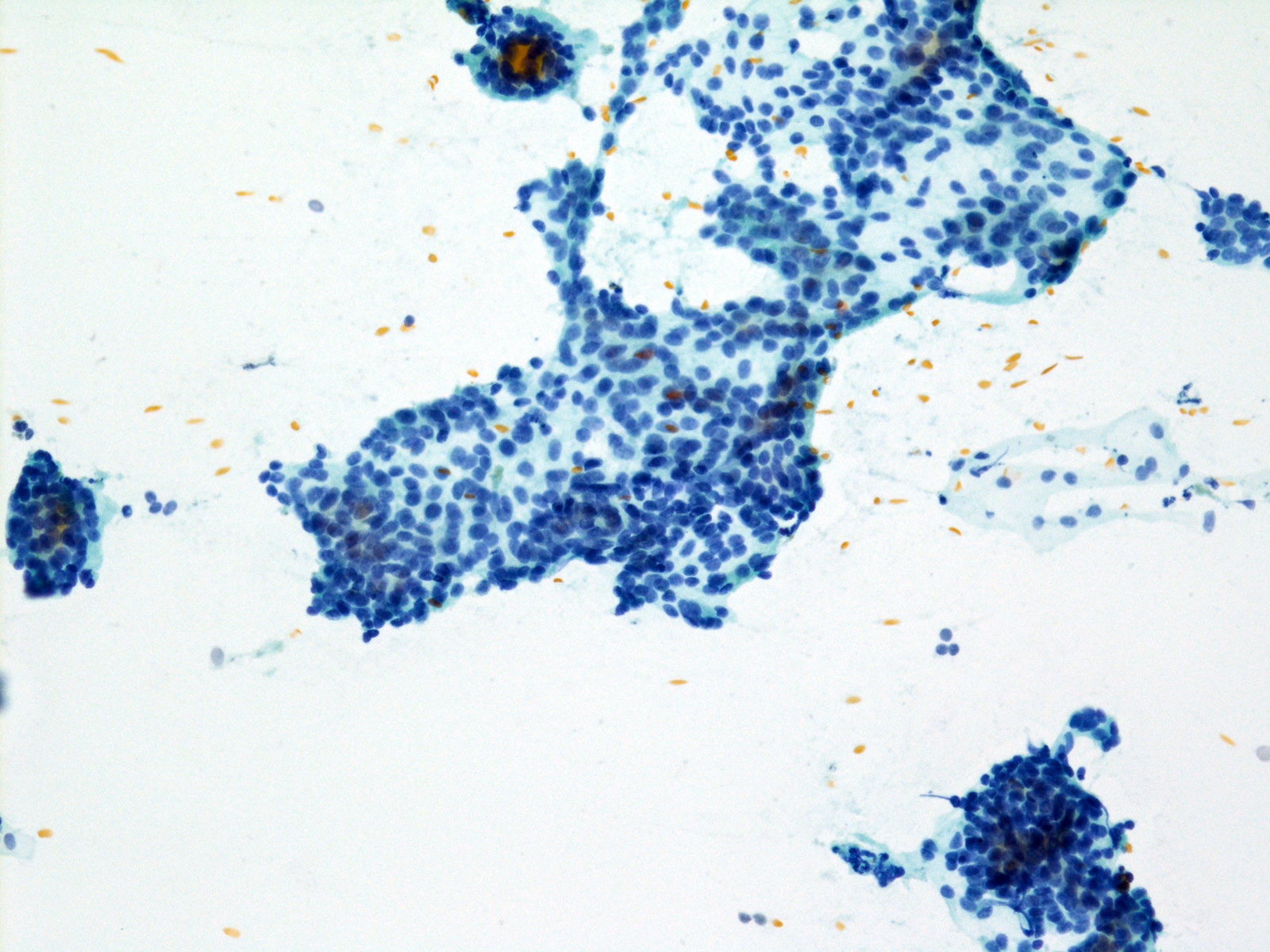
- Oncocytic / oncocytoid SUMP
- FNA with monotonous epithelioid tumor cells with moderate to abundant amounts of cytoplasm showing oncocytic or oncocytoid features
- Cases with coarsely granular, foamy, vacuolated or so called clear cytoplasm are considered within the spectrum of oncocytic / oncocytoid features
- 30.7% of all SUMP FNA
- ROM: 52.5%; RON: 91.1%
- Histology correlation
- Benign neoplasm: Warthin tumor (22.8%) > oncocytoma (10.9%)
- Malignancy: mucoepidermoid carcinoma (22.8%) > acinic cell carcinoma (14.9%)
- SUMP, not otherwise specified (NOS)
- SUMP cases that could not be comfortably placed in either basaloid or oncocytic / oncocytoid subcategory
- Common scenarios
- FNA with focal atypical features in a tumor otherwise favoring a benign neoplasm (e.g., cellular pleomorphic adenoma or pleomorphic adenoma with anisonucleosis that are indefinite for benign)
- FNA with a predominance of an unclassified cell type (e.g., plasmacytoid, spindle, mixed, etc.)
- 21.9% of all SUMP FNA
- ROM: 31.9%; RON: 98.6%
- Histology correlation (mostly myoepithelial cell rich tumors)
- Benign neoplasm: pleomorphic adenoma (47.2%) > myoepithelioma (6.9%)
- Malignancy: carcinoma ex pleomorphic adenoma (9.7%) > myoepithelial carcinoma (6.9%)
- Basaloid SUMP
- Recommended by the Milan system (Faquin: The Milan System for Reporting Salivary Gland Cytopathology, 1st Edition, 2018)
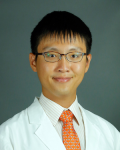
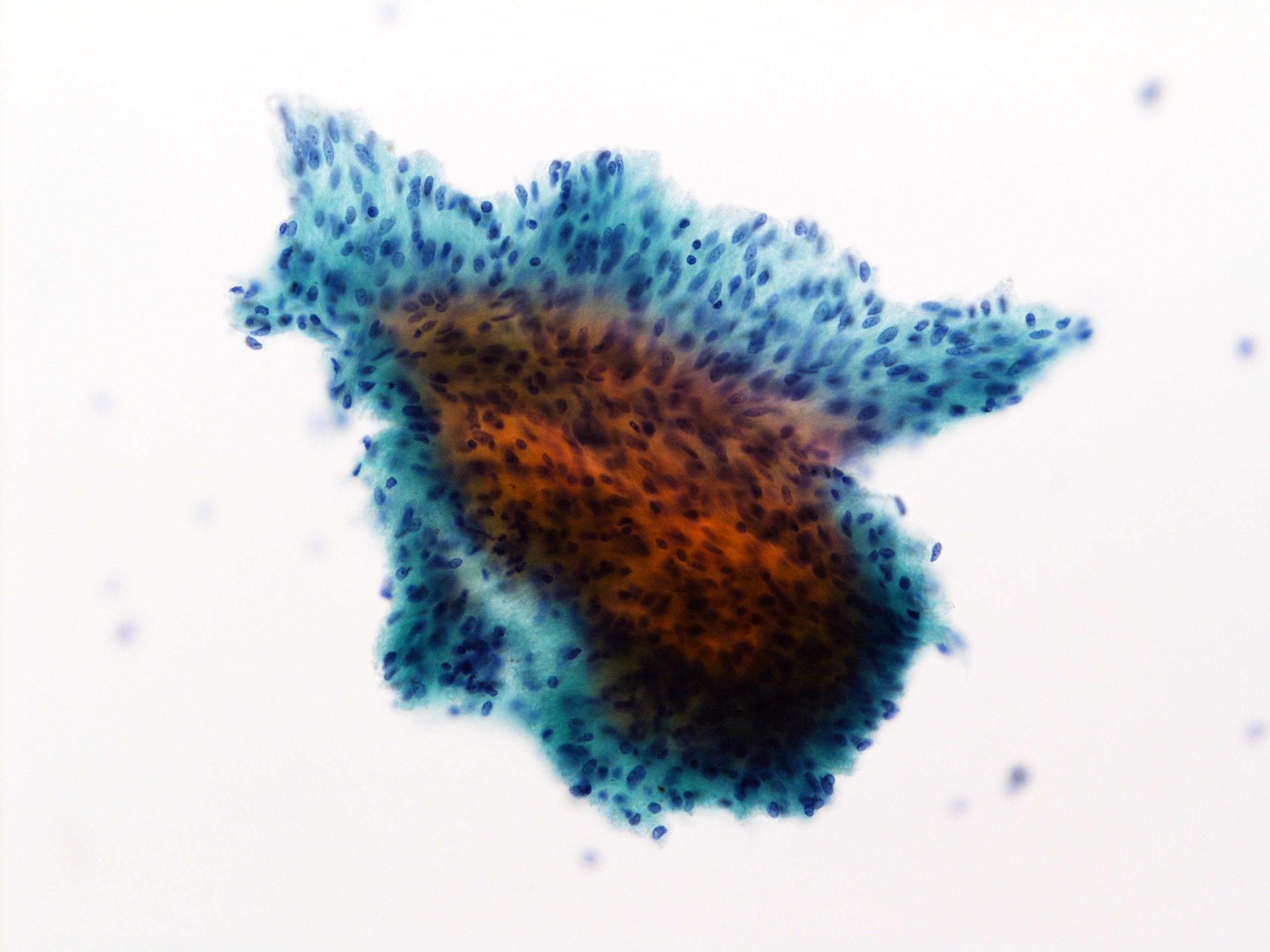
Cytology images
Molecular / cytogenetics description
- Immunocytochemical surrogates for molecular alterations
- Basaloid SUMP
- Pleomorphic adenoma (including carcinoma ex pleomorphic adenoma) (Cancer Cytopathol 2016;124:397)
- PLAG1 or HMGA2 (+)
- Sensitivity: 85%; specificity: 92%
- Adenoid cystic carcinoma (Cancer Cytopathol 2014;122:257)
- MYB (+)
- Sensitivity: 80%; specificity: 100%
- Pleomorphic adenoma (including carcinoma ex pleomorphic adenoma) (Cancer Cytopathol 2016;124:397)
- Oncocytic / oncocytoid SUMP
- Acinic cell carcinoma (Cancer Cytopathol 2022;130:949)
- NR4A3 (+)
- Sensitivity: 100%; specificity: 97%
- Secretory carcinoma (Diagn Cytopathol 2021;49:E329)
- Pan TRK (+)
- Acinic cell carcinoma (Cancer Cytopathol 2022;130:949)
- Basaloid SUMP
- Gene rearrangement testing (by FISH or next generation sequencing [NGS]) (J Am Soc Cytopathol 2019;8:157)
- Basaloid SUMP
- Pleomorphic adenoma: PLAG1 or HMGA2 rearrangement
- Adenoid cystic carcinoma: MYB or MYBL1 rearrangement
- Oncocytic / oncocytoid SUMP
- Mucoepidermoid carcinoma: MAML2::CRTC1 / 3
- Acinic cell carcinoma: NR4A3 rearrangement
- Secretory carcinoma: ETV6::NTRK3
- Hyalinizing clear cell carcinoma: EWSR1::AFT1
- Basaloid SUMP
- Gene mutation testing (by PCR or NGS)
- Basaloid SUMP
- Basal cell adenoma: CTNNB1 mutation
- Adenoid cystic carcinoma: NOTCH1 mutation in a subset
- Polymorphous adenocarcinoma: PRKD1 E710D
- Basaloid SUMP
Sample pathology report
- Parotid gland, right, fine needle aspiration:
- Neoplasm: salivary gland neoplasm of uncertain malignant potential (SUMP)
- Cellular basaloid neoplasm (see comment)
- Comment: The specimen shows monotonous basaloid cells with minimal nuclear atypia and scattered hyaline globules. There are no high grade features, such as mitoses or necrosis. The differential diagnosis includes basal cell adenoma / adenocarcinoma, pleomorphic adenoma and adenoid cystic carcinoma. Suggest correlation with clinical and radiologic findings.
- Parotid gland, left, fine needle aspiration:
- Neoplasm: salivary gland neoplasm of uncertain malignant potential (SUMP)
- Cellular oncocytic / oncocytoid neoplasm (see comment)
- Comment: The specimen shows monotonous oncocytic / oncocytoid cells with minimal nuclear atypia in a lymphoplasmacytic background. Scattered mucinous extracellular materials are noted but no mucous cells are present. The differential diagnosis includes Warthin tumor with mucinous metaplasia and low grade mucoepidermoid carcinoma with oncocytic change. Suggest correlation with clinical and radiologic findings.
Differential diagnosis
- SUMP category is only reserved for cases with a predominance of monomorphic cytomorphology and cases with pleomorphic tumor cells are recommended to be classified as either suspicious for malignancy (category V) or malignant (category VI)
- Basaloid SUMP cases with a purely fibrillary extracellular matrix are compatible with a pleomorphic adenoma and are recommended to be classified as benign neoplasm (category IVA)
Additional references
Board review style question #1
A 62 year old man presents with a 3.6 cm left parotid nodule. The fine needle aspiration shows a cellular smear, which is composed of fragments of bland looking, basaloid cells intermingled with magenta colored hyaline globules. What is the best diagnosis according to the Milan System for Reporting Salivary Gland Cytopathology?
- Category III: atypia of undetermined significance
- Category IVA: benign neoplasm, pleomorphic adenoma
- Category IVB: salivary gland neoplasm of uncertain malignant potential, with basaloid features
- Category VI: malignant, adenoid cystic carcinoma
Board review style answer #1
C. Category IVB: salivary gland neoplasm of uncertain malignant potential, with basaloid features. Basaloid neoplasms showing overlapping morphology of bland basal cells and extracellular nonfibrillary matrix are better classified as salivary gland neoplasm of uncertain malignant potential, with basaloid features. The final pathology of the same case showed a basal cell adenoma with prominent hyaline globules.
Comment Here
Reference: Neoplasm-salivary gland neoplasm of uncertain malignant potential (SUMP)
Comment Here
Reference: Neoplasm-salivary gland neoplasm of uncertain malignant potential (SUMP)
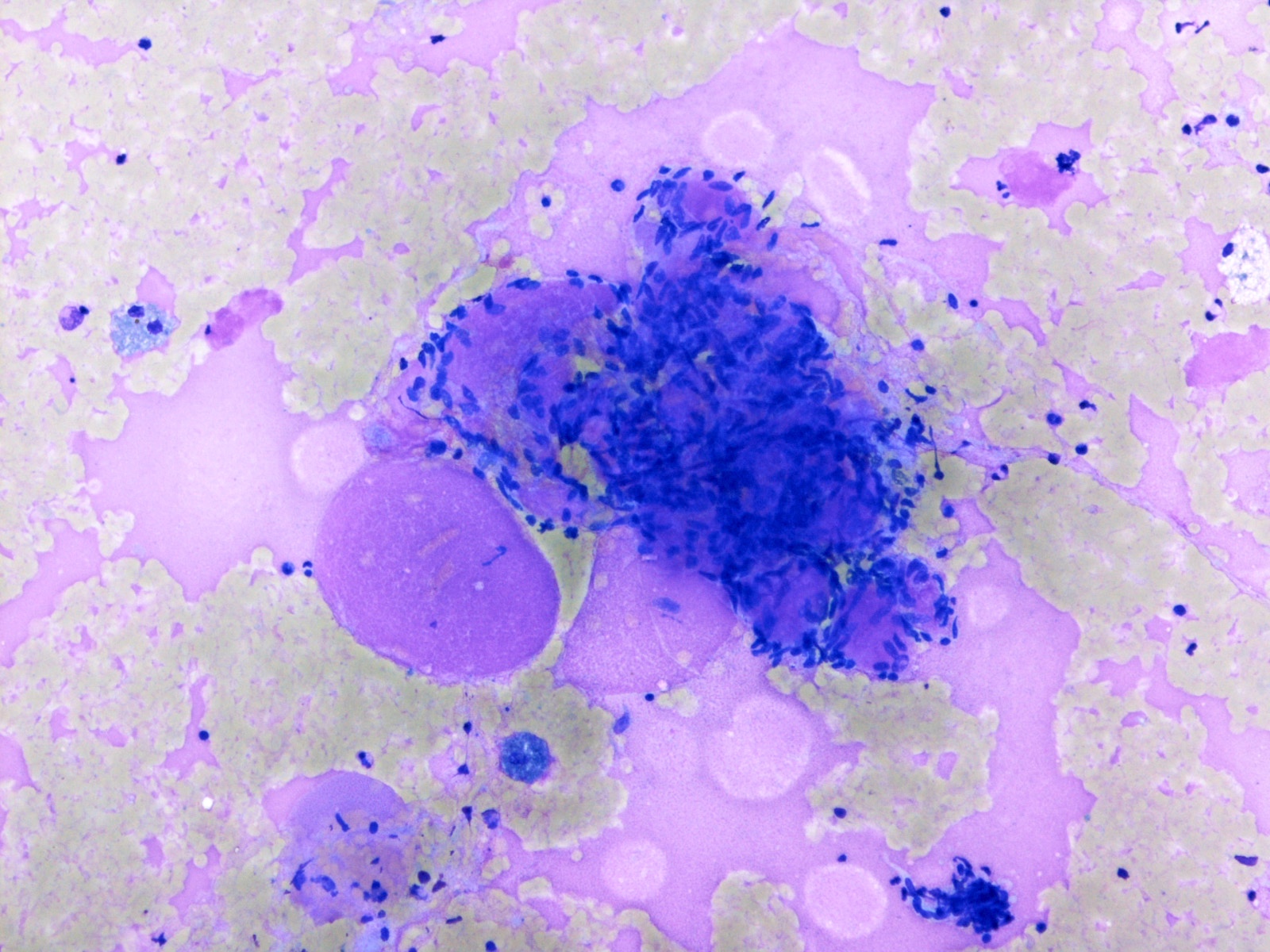
Board review style question #2
A 49 year old woman presents with a 2.5 cm right parotid nodule. Fine needle aspiration cytology is performed and the result is shown in the figure. What would be the most likely diagnosis if the patient receives surgical excision?
- Basal cell adenoma
- Mucoepidermoid carcinoma
- Secretory carcinoma
- Warthin tumor
Board review style answer #2
A. Basal cell adenoma. The figure shows a proliferation of basaloid cells admixed with extracellular matrix. It is consistent with the cytologic diagnosis of SUMP with basaloid features. The differential diagnosis includes matrix producing tumors with basaloid cells, such as basal cell adenoma / adenocarcinoma and adenoid cystic carcinoma. Answers B - D are incorrect because Warthin tumor, mucoepidermoid carcinoma and secretory carcinoma are the less likely options since they usually present with neoplastic cells harboring more abundant cytoplasm and often would be interpreted as SUMP with oncocytic / oncocytoid features.
Comment Here
Reference: Neoplasm-salivary gland neoplasm of uncertain malignant potential (SUMP)
Comment Here
Reference: Neoplasm-salivary gland neoplasm of uncertain malignant potential (SUMP)