Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Interpretation | Uses by pathologists | Prognostic factors | Microscopic (histologic) description | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Iqbal F, Lyapichev KA. MUM1 / IRF4. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/stainsmum1.html. Accessed April 28th, 2024.
Definition / general
- MUM1 / IRF4 is the abbreviation of multiple myeloma 1 / interferon regulatory factor 4
- Normally expressed in plasma cells, melanocytes, activated B cells and activated T cells (Appl Immunohistochem Mol Morphol 2010;18:301, Int J Clin Exp Pathol 2015;8:11372)
Essential features
- MUM1 / IRF4 is a nuclear marker that is normally expressed in activated B and T cells, plasma cells and melanocytes
- Involved in the differentiation of B cells and T cells
- Marker is expressed in lymphoid and some nonlymphoid malignancies including classic Hodgkin lymphoma, diffuse large B cell lymphoma (nongerminal center B cell-like subtype), multiple myeloma and malignant melanoma
- Fluorescence in situ hybridization (FISH) for 6p25 (IRF4 / DUSP22) gene rearrangement can be used to diagnose different entities
Terminology
- PU.1 interaction partner (PIP)
- Lymphocyte specific interferon response factor (LSIRF)
- Interferon consensus sequence binding protein for activated T cells (ICSAT) (Appl Immunohistochem Mol Morphol 2010;18:301, Blood 2000;95:2084)
Pathophysiology
- MUM1 was originally found to be involved in the t(6;14)(p25;q32) translocation of multiple myeloma, which causes the juxtaposition of the MUM1 gene, mapping at 6p25, to the IgH locus on 14q32 (Leukemia 2000;14:563)
- MUM1+ cells are mainly located in the light zone of the germinal center but the highly proliferating, follicle colonizing B blasts (centroblasts) of the dark zone fail to express the protein; thus, it is unlikely that the MUM1 protein is involved in the process of clonal expansion known to occur in the dark zone of the germinal center (Blood 2000;95:2084)
- MUM1 expression may denote the final step of intragerminal center B cell differentiation (i.e., the stage known as centrocyte, as well as subsequent steps of B cell maturation toward plasma cells) (Leukemia 2000;14:563)
- Loss of MUM1 function results in the absence of activated lymphoid cells and Ig secreting plasma cells (Science 1997;275:540, Leukemia 2000;14:563)
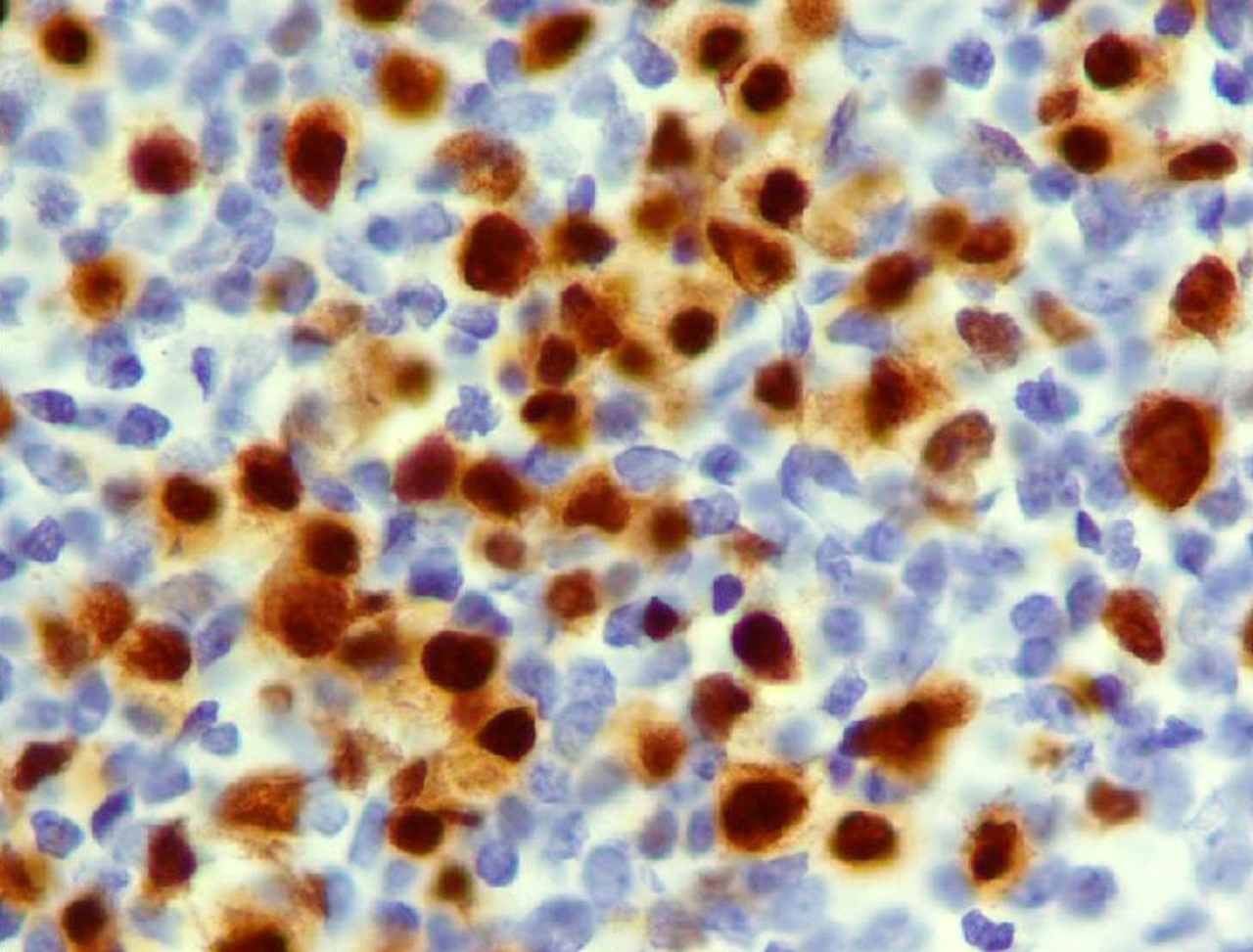
Interpretation
- Nuclear stain
Uses by pathologists
- MUM1 is one of the markers used in Hans algorithm (requires immunostains CD10, BCL6 and MUM1); it is used in subclassification of diffuse large B cell lymphoma (DLBCL) into germinal center B cell-like subtype and nongerminal center B cell-like subtype (Blood 2004;103:275, Med J Malaysia 2020;75:98, Cancer Cytopathol 2016;124:135)
- May help differentiate classic Hodgkin lymphoma (cHL) (MUM1 positive) from nodular lymphocyte predominant Hodgkin lymphoma (MUM1 negative) (Rom J Morphol Embryol 2011;52:69)
- Helps differentiate the double hit lymphomas (MUM1 positive > 45%) from Burkitt and diffuse large B cell lymphoma (usually MUM1 negative if germinal center phenotype) (Am J Surg Pathol 2010;34:327)
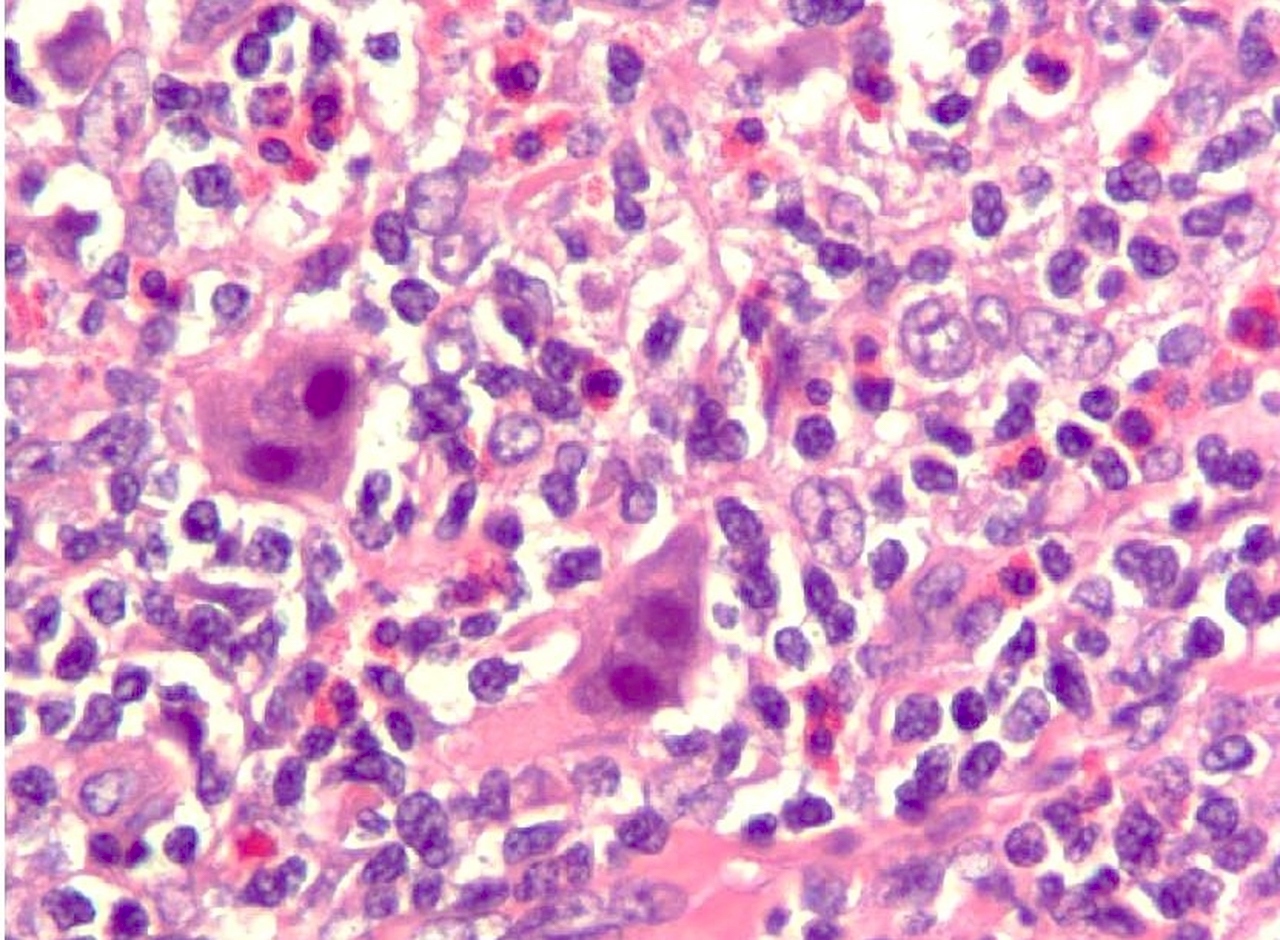
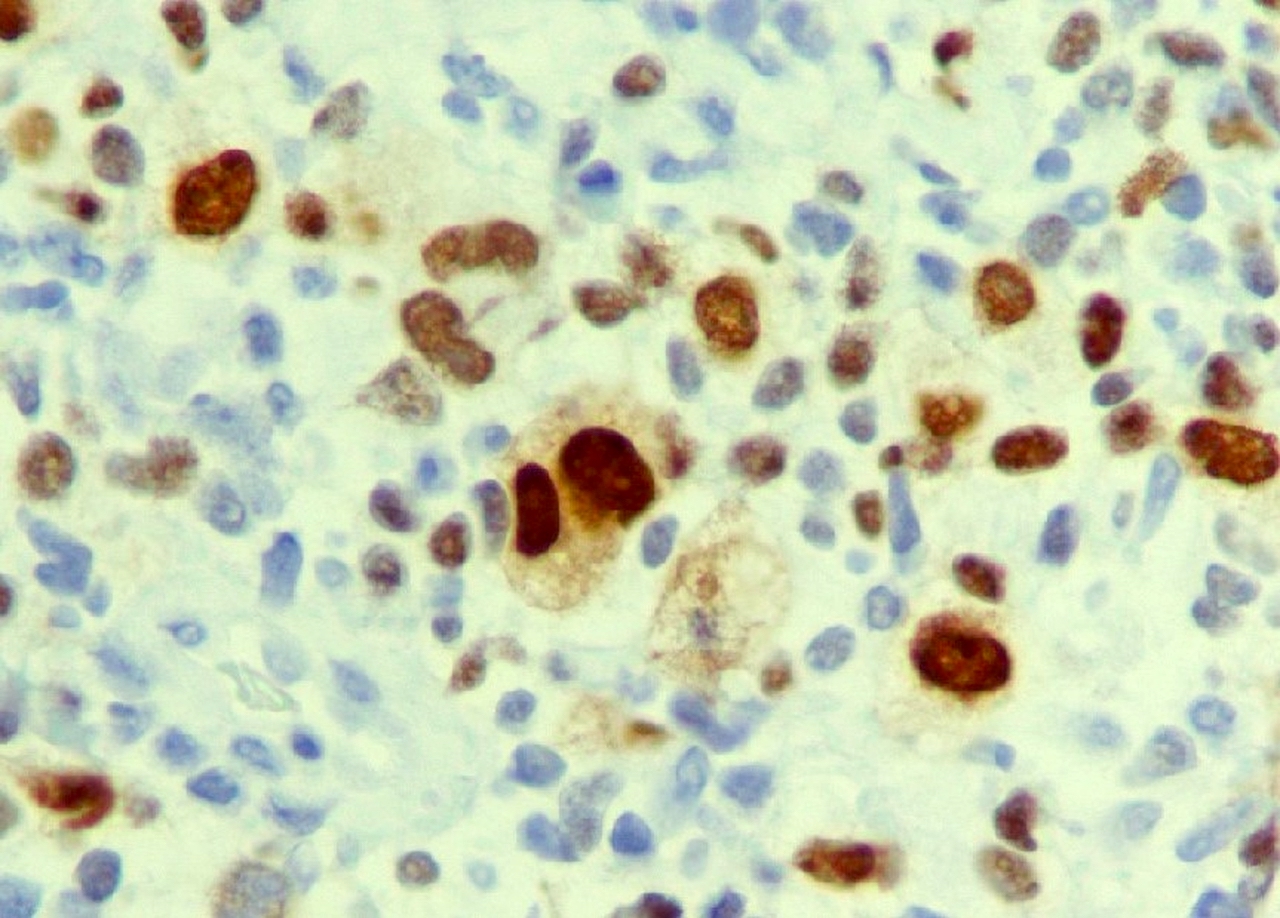
- To differentiate angioimmunoblastic T cell lymphoma (AITL) with Hodgkin / Reed-Sternberg (HRS)-like cells from classic Hodgkin lymphoma (Int J Clin Exp Pathol 2015;8:11372):
- In AITL, MUM1 is expressed not only in HRS-like cells but also in the neoplastic T cells around the HRS-like cells, forming a rosette pattern (Int J Clin Exp Pathol 2015;8:11372)
- FISH for IRF4 favors cutaneous anaplastic large cell lymphoma versus other cutaneous T cell lymphoproliferative disorders (Mod Pathol 2011;24:596)
- MUM1 expression differentiates tumors in the PEComa family from clear cell sarcoma and melanoma (Int J Surg Pathol 2012;20:29)
- Can be used to differentiate primary effusion lymphoma among other lymphomatous effusions (Br J Haematol 2000;111:247)
Prognostic factors
- In diffuse large B cell lymphomas, MUM1 identifies cases of the nongerminal center B cell-like subtype and has been linked to poor survival (Leukemia 2008;22:441)
- MUM1 mRNA expression has been found to be an independent risk factor for poor survival in myeloma (Leukemia 2008;22:441)
- High expression of MUM1 was in addition to β2 microglobulin, the only myeloma risk factors analyzed in the study that were found to be independently associated with overall survival
- Combined score between these 2 parameters allowed a strong discrimination between high and low risk groups
- Lack of MUM1 expression was found to be associated with worse outcome in classic Hodgkin lymphoma (Haematologica 2007;92:1343)
- IRF4 / MUM1 expression was associated with poor survival outcomes in peripheral T cell lymphoma (PTCL) (J Cancer 2017;8:1018)
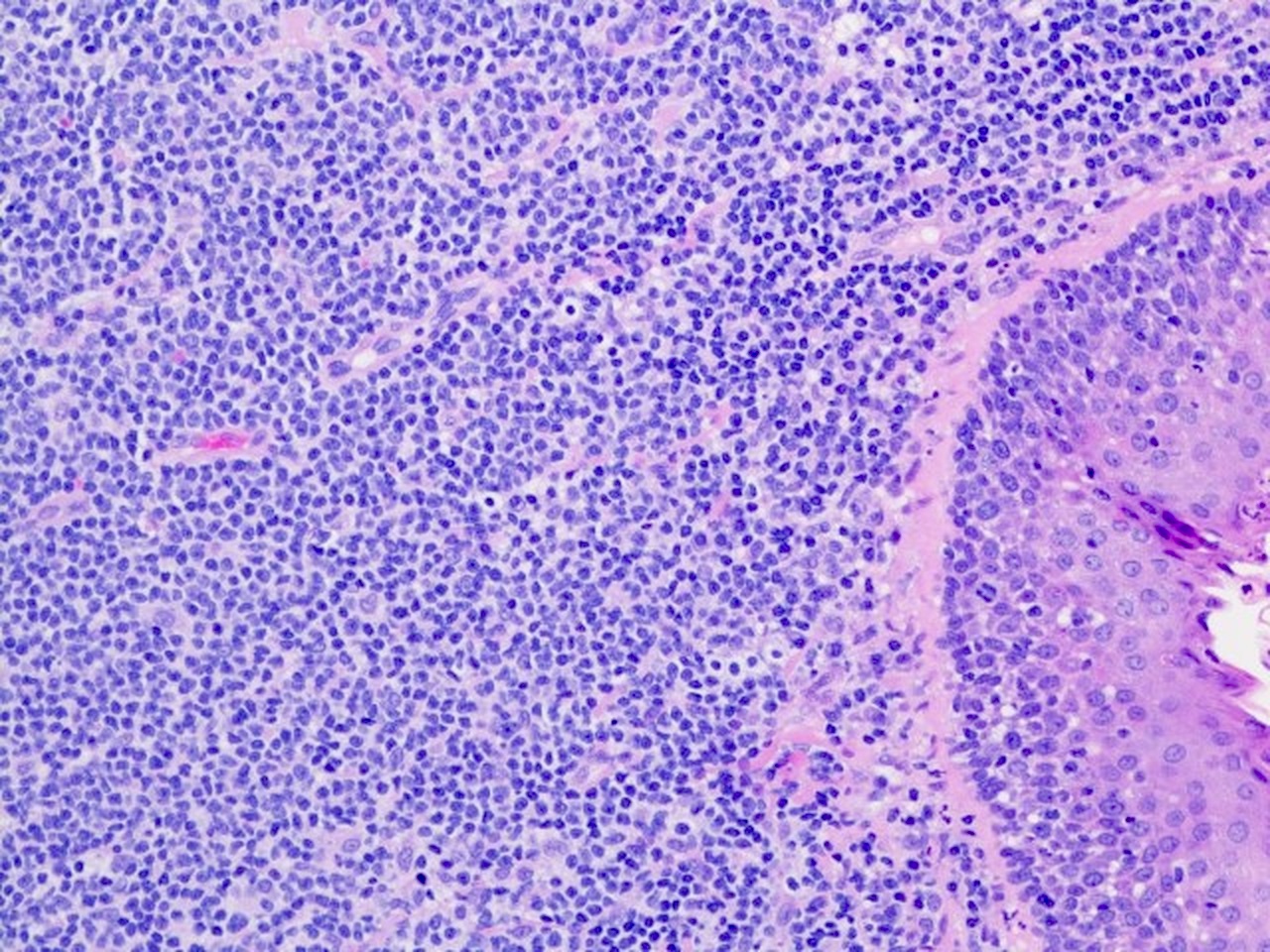
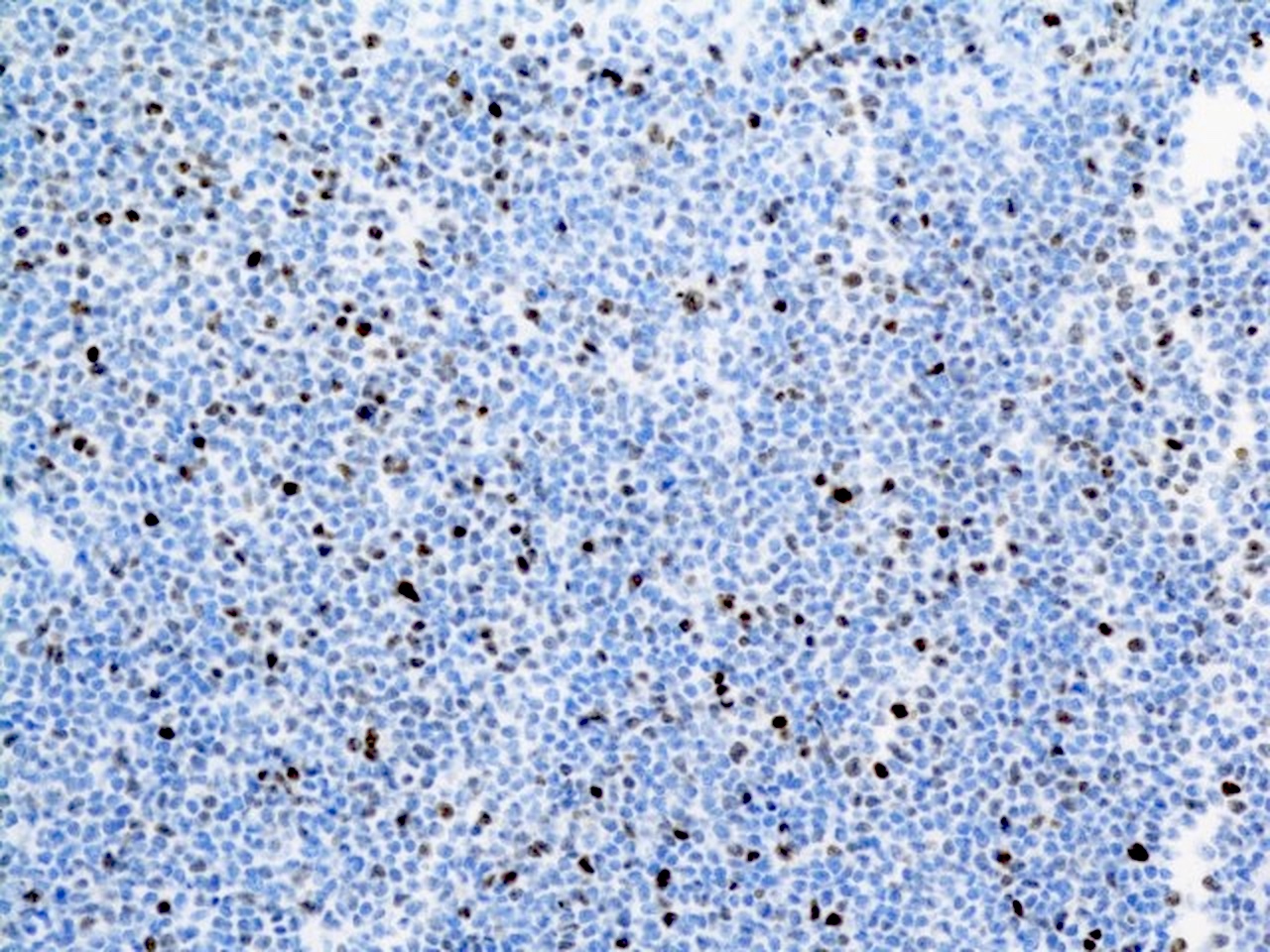
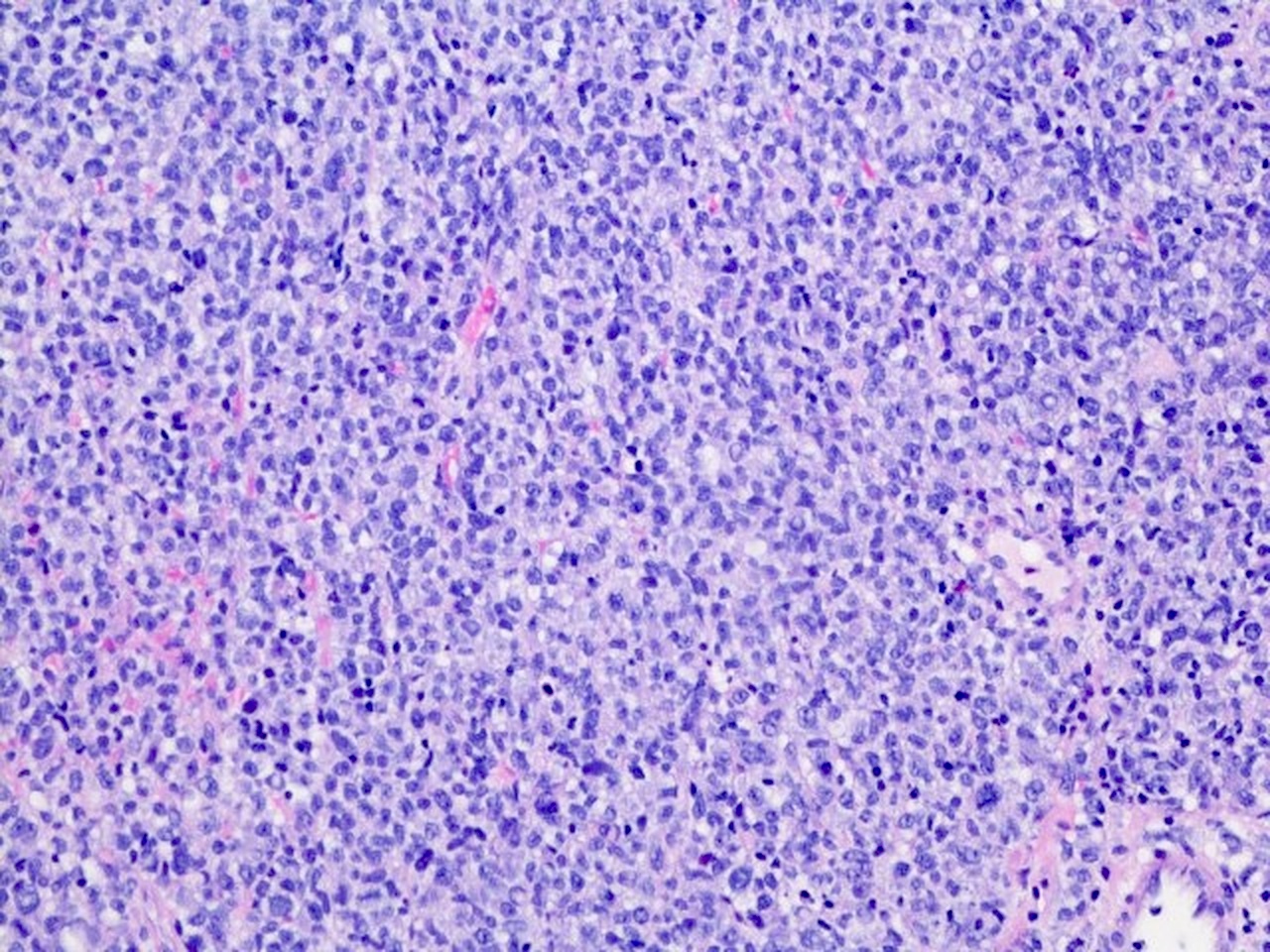
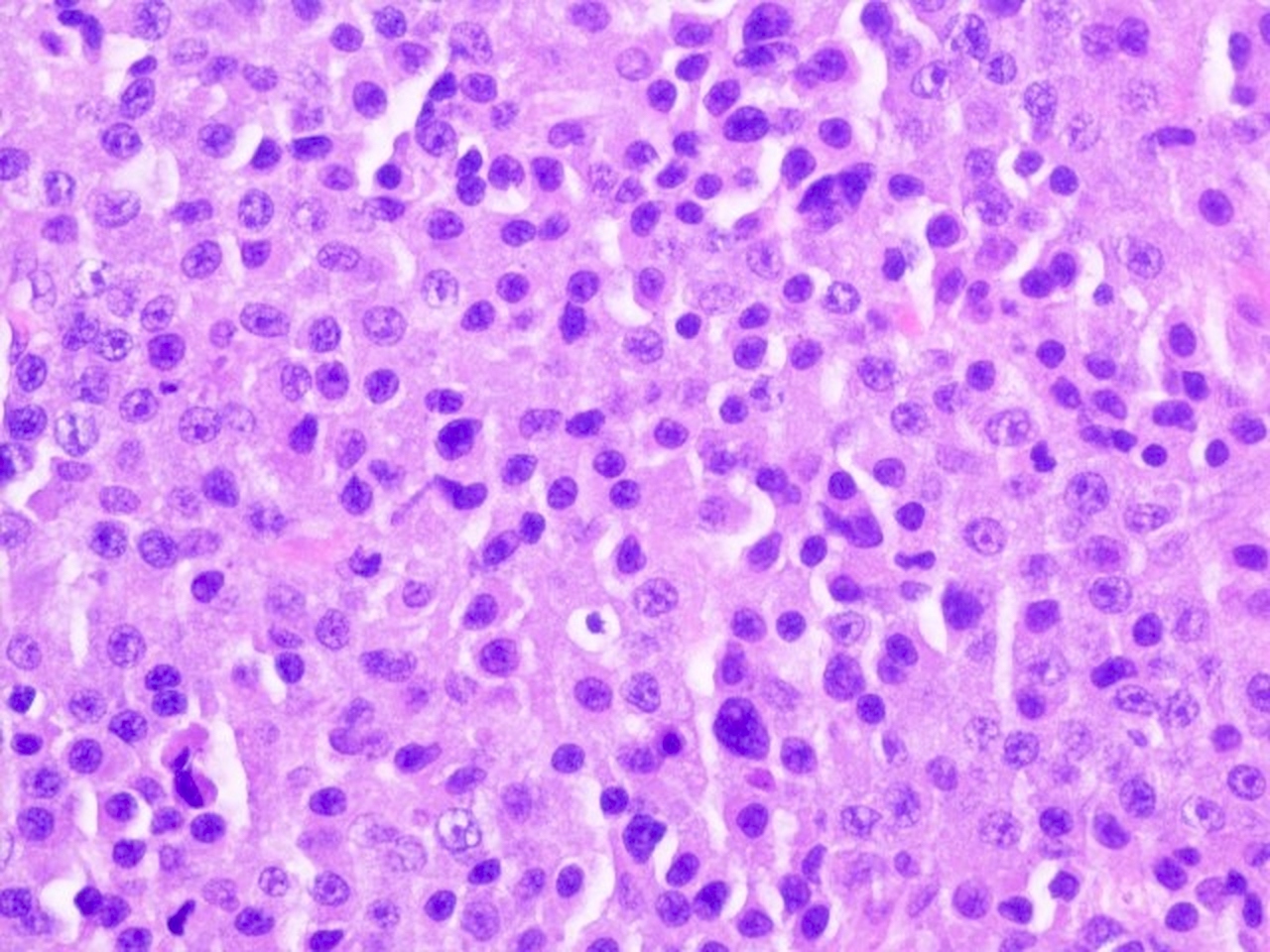
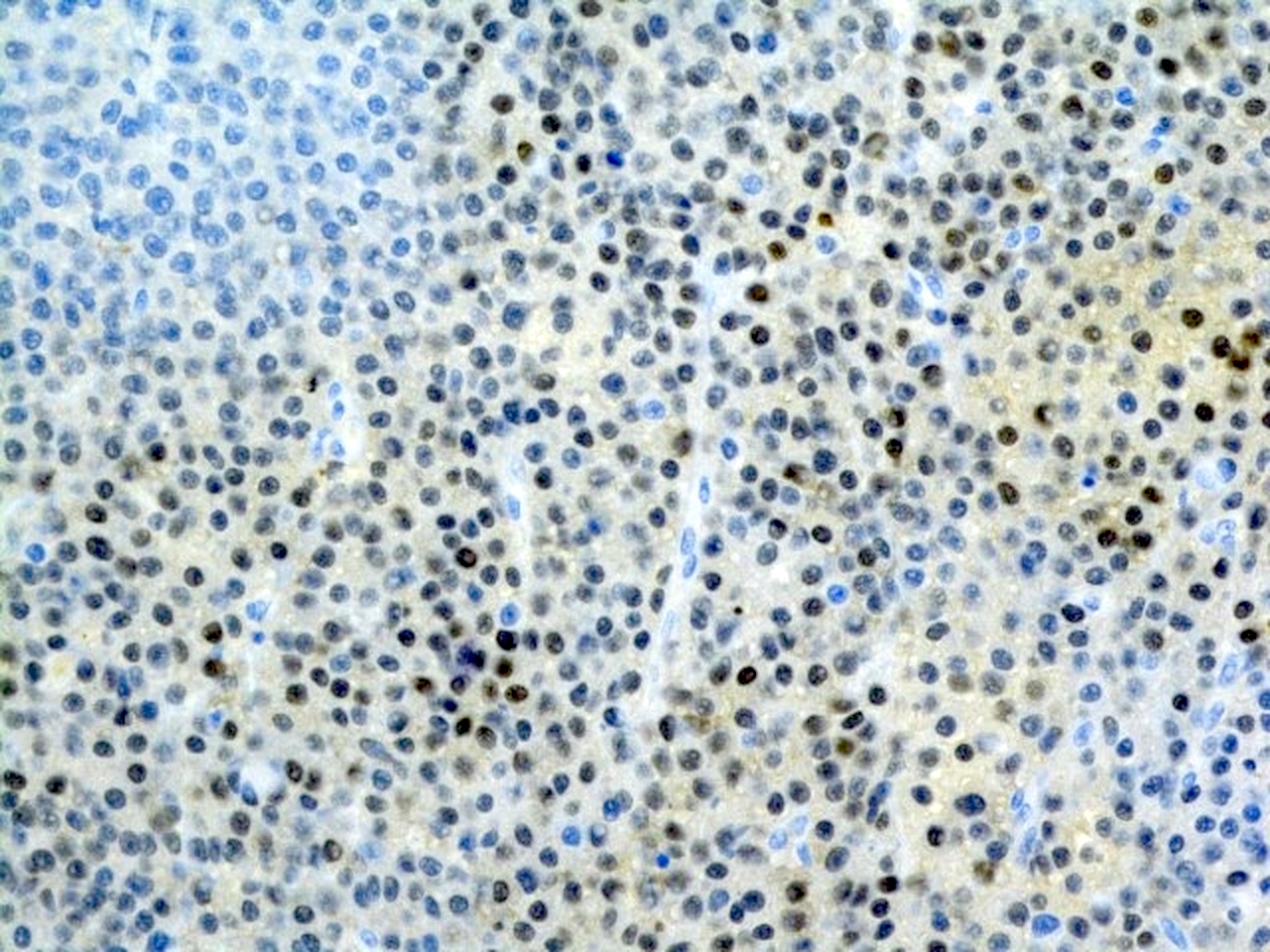
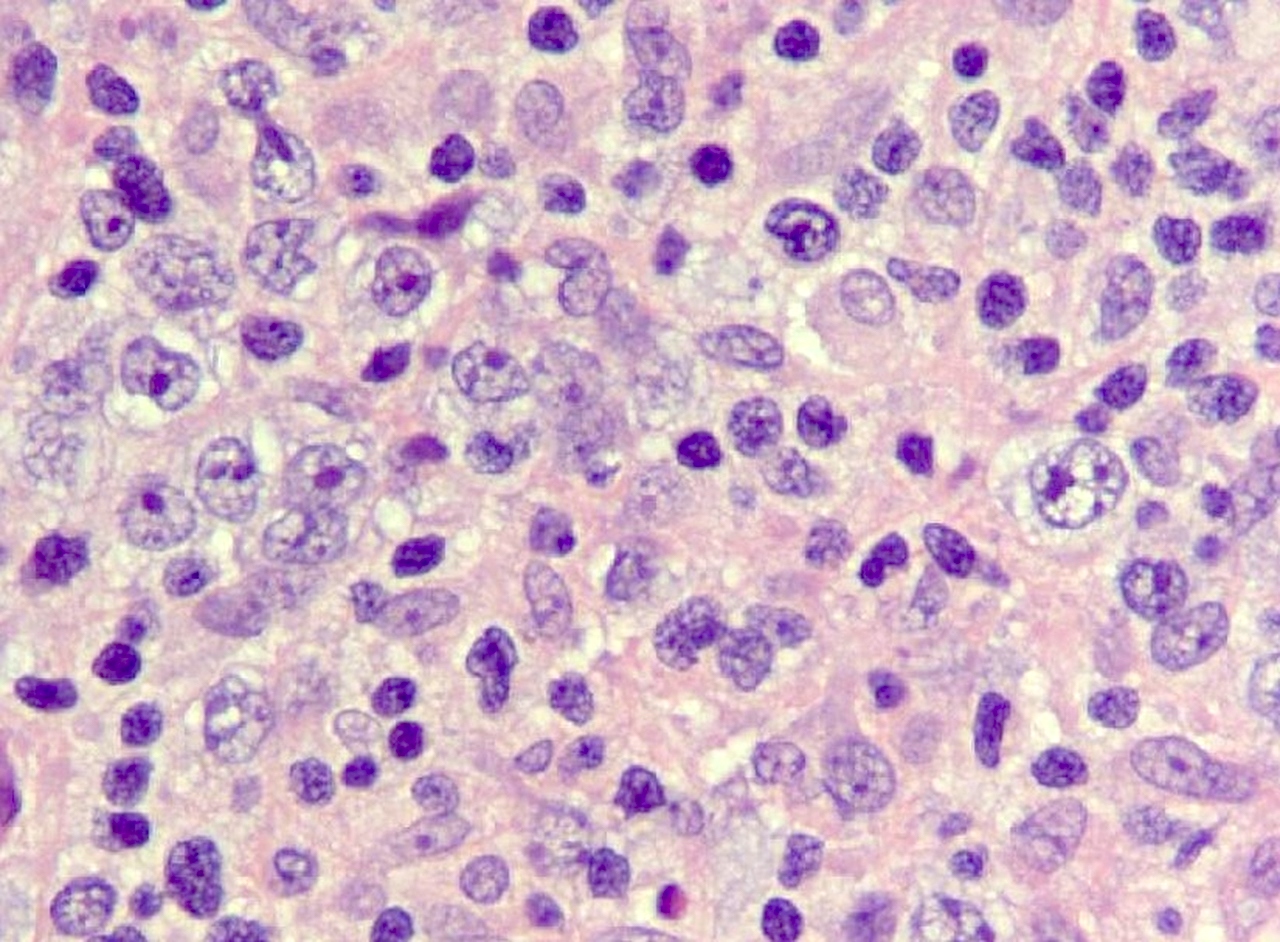
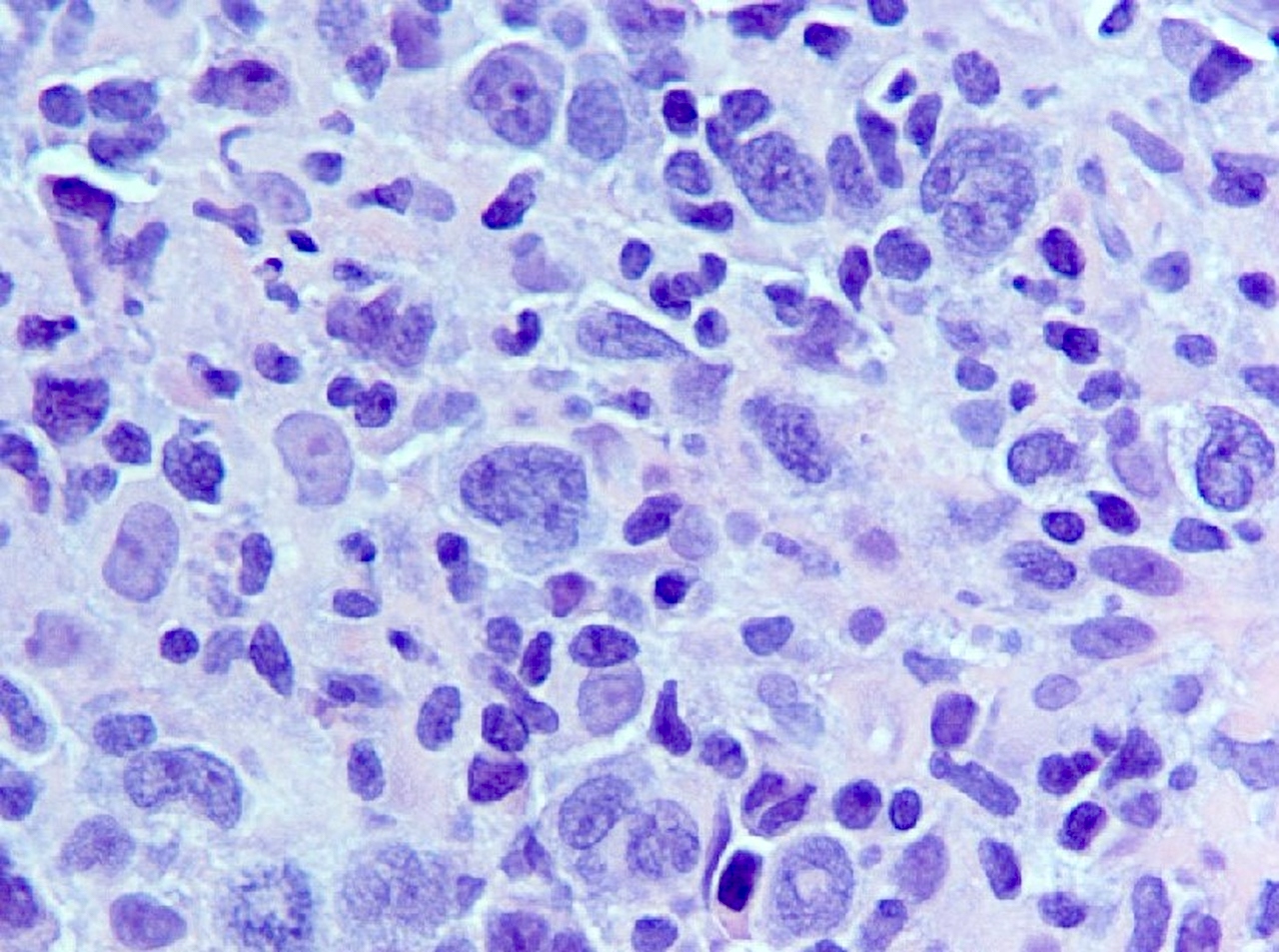
Microscopic (histologic) description
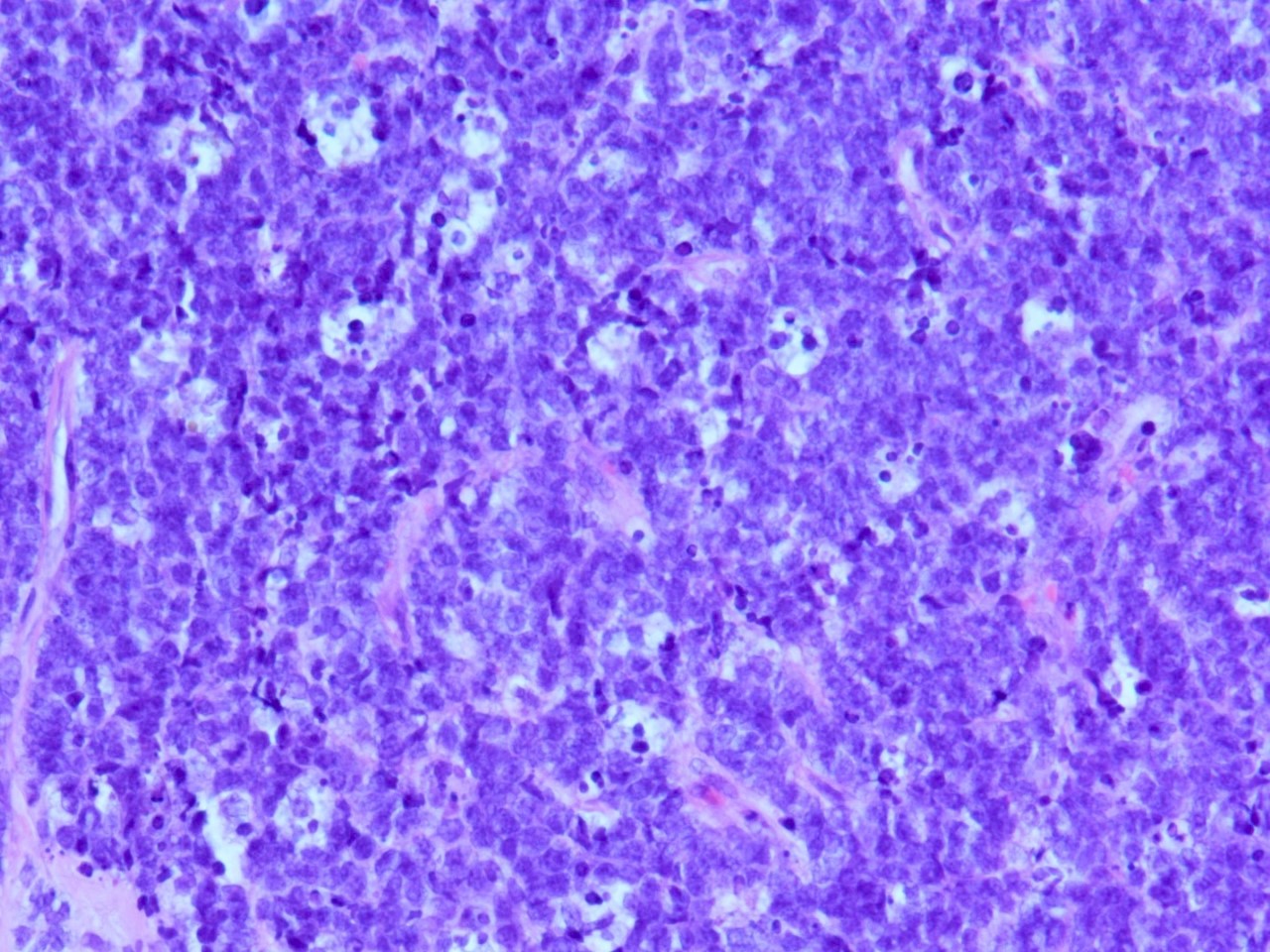
- Percentage of nuclei with positive staining in tumor cells is scored to subclassify diffuse large B cell lymphoma (DLBCL) into germinal center B cell-like subtype and nongerminal center B cell-like subtype
- > 30% - nongerminal center B cell-like subtype if CD10 is negative and BCL6 is positive
- < 30% - germinal center B cell-like subtype if CD10 is negative and BCL6 is positive
- Reference: Blood 2004;103:275
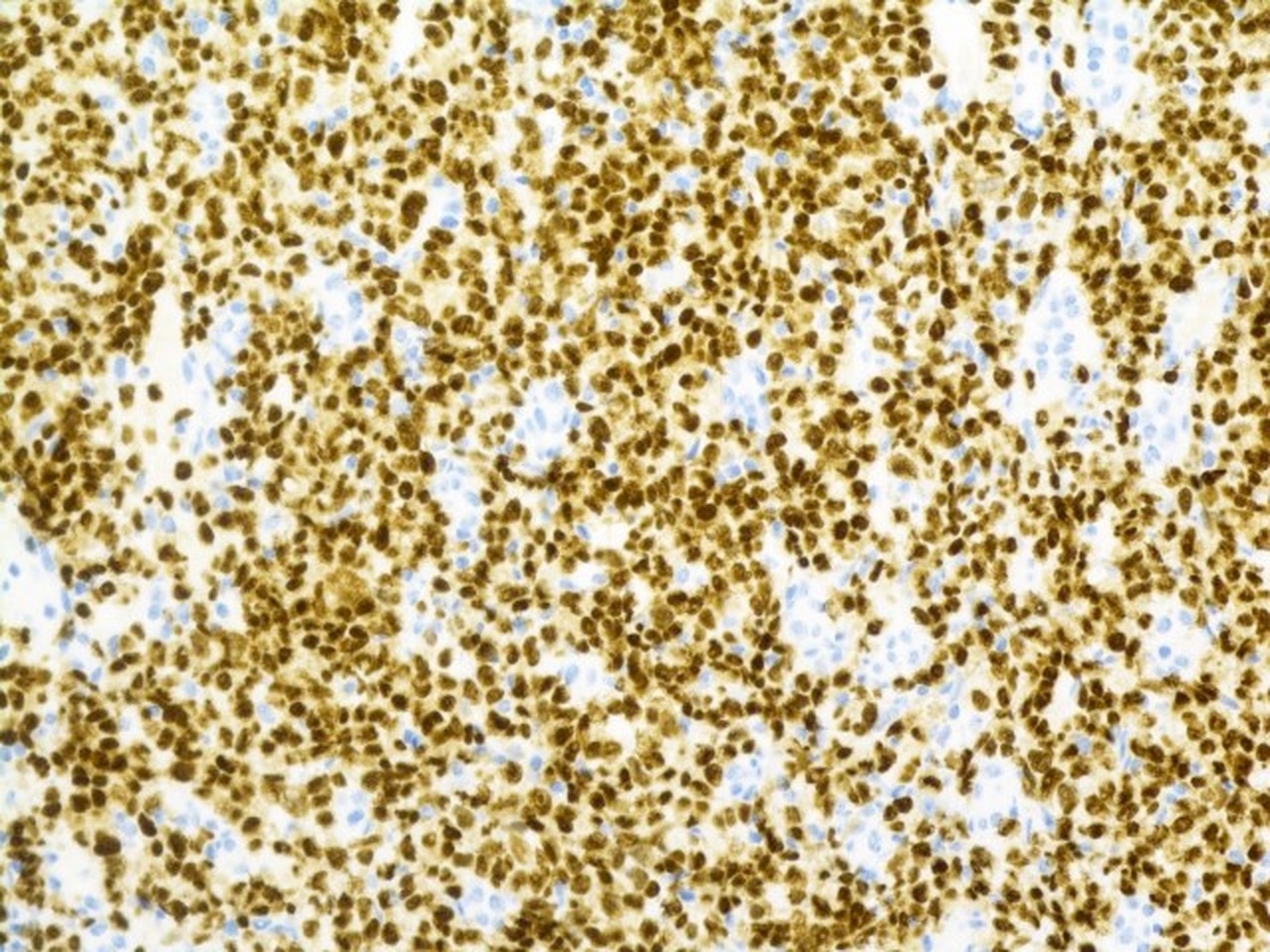
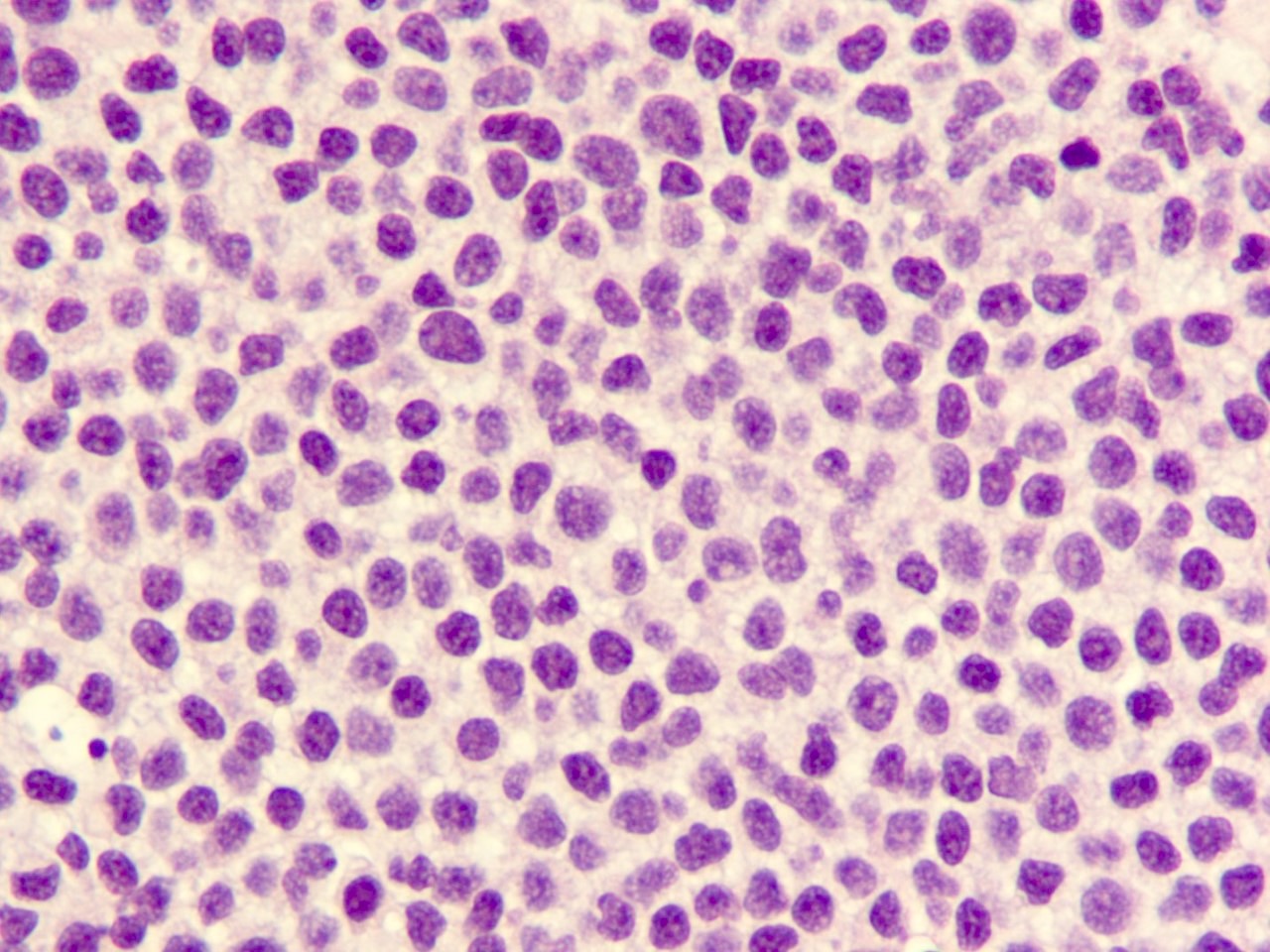
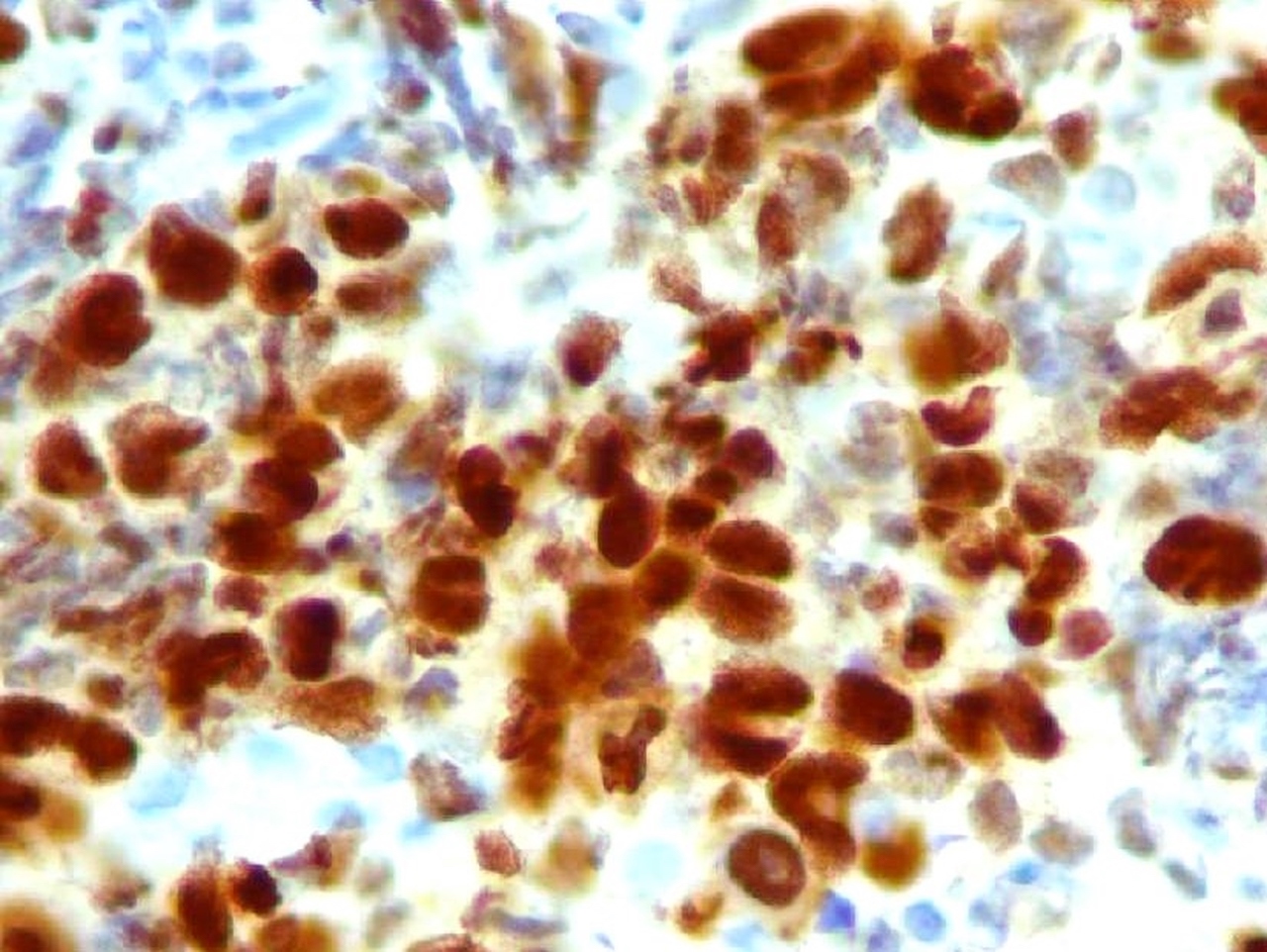
Microscopic (histologic) images
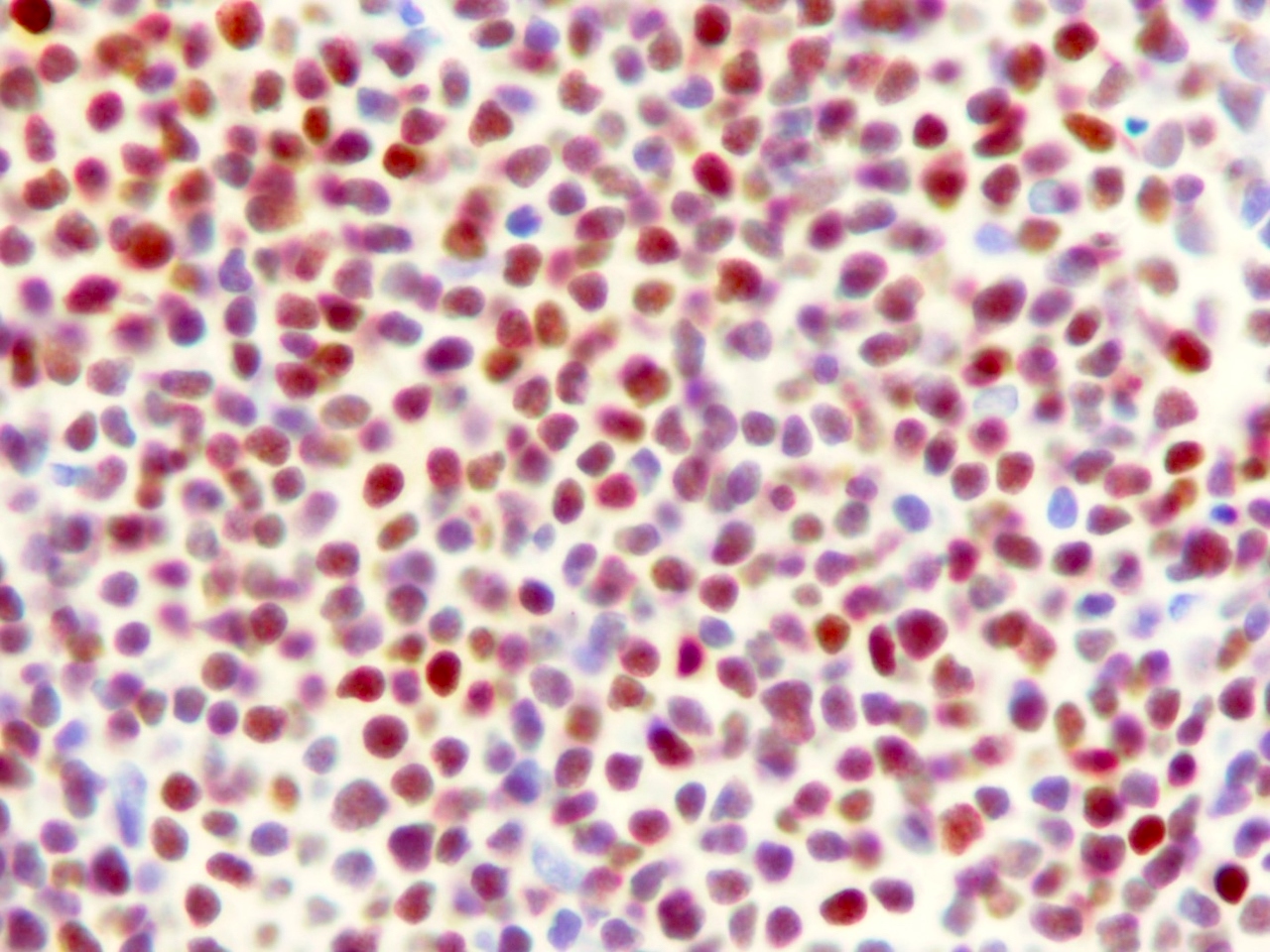
Contributed by Fatima Iqbal, M.D. and Kirill A. Lyapichev, M.D.
Positive staining - normal
- Germinal center B cells, activated T cells, plasma cells (Appl Immunohistochem Mol Morphol 2010;18:301, Mod Pathol 2001;14:686, Int J Clin Exp Pathol 2015;8:11372, Nat Immunol 2006;7:773)
- Melanocytes (Appl Immunohistochem Mol Morphol 2010;18:301, Int J Clin Exp Pathol 2015;8:11372)
Positive staining - disease
- Adult T cell leukemia / lymphoma (ATLL) (Appl Immunohistochem Mol Morphol 2010;18:301)
- Anaplastic large cell lymphoma (100%) (Blood 2000;95:2084)
- Angioimmunoblastic T cell lymphoma (Hodgkin / Reed-Sternberg [HRS]-like cells) (Int J Clin Exp Pathol 2015;8:11372)
- Burkitt lymphoma (40%) (Hum Pathol 2009;40:565, Appl Immunohistochem Mol Morphol 2010;18:301)
- Chronic lymphocytic leukemia (variable expression) (Leuk Lymphoma 2008;49:273, Appl Immunohistochem Mol Morphol 2010;18:301)
- Classic Hodgkin lymphoma (100%) (Appl Immunohistochem Mol Morphol 2010;18:301)
- Diffuse large B cell lymphoma (76% adult cases and 44% pediatric cases) (Appl Immunohistochem Mol Morphol 2010;18:301, Arch Pathol Lab Med 2010;134:759)
- Extranodal NK / T cell lymphoma, nasal type (Am J Surg Pathol 2012;36:481)
- Follicular lymphoma, high grade (Appl Immunohistochem Mol Morphol 2010;18:301, Haematologica 2007;92:267)
- Infectious mononucleosis (Mod Pathol 2012;25:1149)
- Intravascular large B cell lymphoma (95%) (Arch Pathol Lab Med 2012;136:333)
- Lymphomatoid papulosis (87%) (Br J Dermatol 2008;158:1280, Appl Immunohistochem Mol Morphol 2010;18:301)
- Malignant melanoma (92%) (Appl Immunohistochem Mol Morphol 2010;18:301)
- Mantle cell lymphoma (35%) (Appl Immunohistochem Mol Morphol 2010;18:103)
- Marginal zone lymphoma (30 - 50%) (Blood 2000;95:2084)
- Mycosis fungoides (40%) (Blood 2000;95:2084)
- Peripheral T cell lymphoma, NOS (7%) (Leukemia 2009;23:574, Appl Immunohistochem Mol Morphol 2010;18:301)
- Plasma cell myeloma (strong expression) (Appl Immunohistochem Mol Morphol 2010;18:301)
- Primary cutaneous diffuse large B cell lymphoma (70%) (Appl Immunohistochem Mol Morphol 2010;18:301)
- Primary effusion lymphoma (all positive cases) (Br J Haematol 2000;111:247, Appl Immunohistochem Mol Morphol 2010;18:301)
- Primary diffuse large B cell lymphoma of the CNS (45%) (Invest Ophthalmol Vis Sci 2005;46:3957, Appl Immunohistochem Mol Morphol 2010;18:301)
- Primary mediastinal (thymic) large B cell lymphoma (70%) (Appl Immunohistochem Mol Morphol 2010;18:301)
Negative staining
- B acute lymphoblastic lymphoma / leukemia (Leukemia 2000;14:563)
- Carcinoma (Adv Anat Pathol 2007;14:25, Appl Immunohistochem Mol Morphol 2010;18:301)
- Follicular lymphoma, low grade (Haematologica 2007;92:267)
- T acute lymphoblastic lymphoma / leukemia (Adv Anat Pathol 2007;14:25)
Molecular / cytogenetics description
- In the proper context, the presence of the 6p25 gene rearrangement supports a diagnosis of large B cell lymphoma with IRF4 rearrangement or ALK negative anaplastic large cell lymphoma with IRF4 / DUSP22 rearrangement (Blood 2014;124:1473, Blood 2011;118:139)
- FISH detection of IG-IRF4 fusion detects lymphomas associated with younger patient age and favorable outcome (Blood 2011;118:139)
- t(6;14)(p25;q32), causing MUM1 / IRF4-IgH, present in 20% of myeloma (Leukemia 1999;13:1812)
- Recurrent translocations involving the IRF4 oncogene locus were identified in peripheral T cell lymphomas (Leukemia 2009;23:574)
- FISH for IRF4 favors cutaneous anaplastic large cell lymphoma versus other cutaneous T cell lymphoproliferative disorders (Mod Pathol 2011;24:596)
Sample pathology report
- Lymph node, left groin, excision:
- Diffuse large B cell lymphoma, nongerminal center B cell-like immunophenotype
- CD10 negative in malignant cells < 30%
- BCL6 positive in malignant lymphoid cells > 30%
- MUM1 positive in malignant lymphoid cells > 30%
Board review style question #1
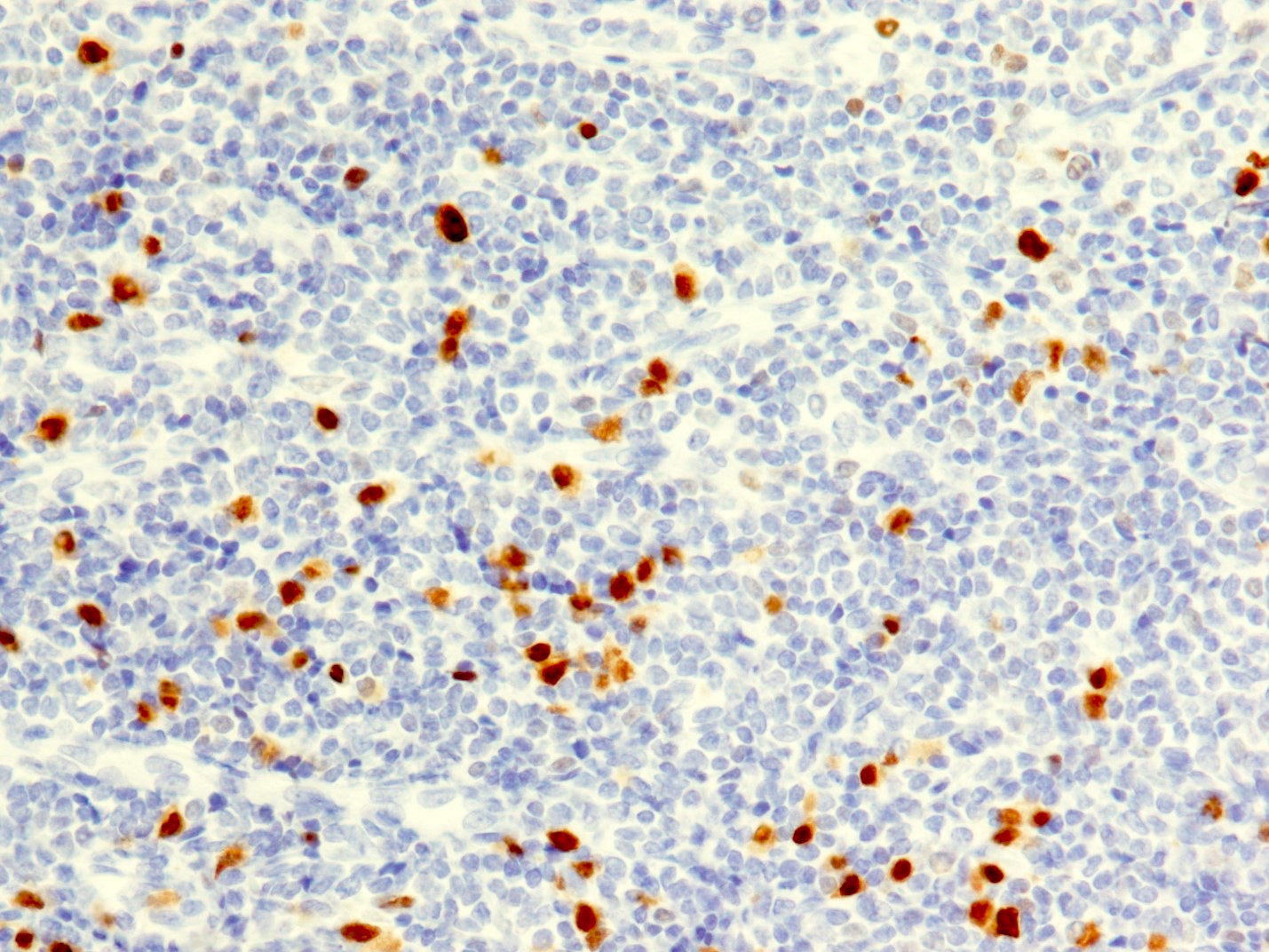
The above figure shows a MUM1 immunostain result. What is needed to confirm it as positive in diffuse large B cell lymphoma, nongerminal center B cell-like immunophenotype?
- Positive nuclear and cytoplasmic staining pattern
- Positive nuclear staining in > 30% malignant lymphoid cells
- Positive nuclear staining in > 50% malignant lymphoid cells
- Positive nuclear staining pattern
Board review style answer #1
B. Positive nuclear staining in > 30% malignant lymphoid cells. According to Han's algorithm, more than 30% malignant lymphoid cells (nuclear staining) is required to call it positive in diffuse large B cell lymphoma, nongerminal center B cell-like immunophenotype (Blood 2004;103:275).
Comment Here
Reference: MUM1 / IRF4
Comment Here
Reference: MUM1 / IRF4
Board review style question #2
Which of the following immunophenotypic findings is consistent with nongerminal center B cell-like immunophenotype of diffuse large B cell lymphoma (non-GCB, DLBCL)?
- CD10-, BCL6+, MUM1-
- CD10+, BCL6-, MUM1-
- CD10-, BCL6+, MUM1+
- CD10+, BCL6+, MUM1-
Board review style answer #2
C. CD10-, BCL6+, MUM1+. According to Hans algorithm, if CD10- (< 30% expression), BCL6+ (> 30% expression) and MUM1+ (> 30% expression), it represents nongerminal center B cell-like subtype of diffuse large B cell lymphoma (Blood 2004;103:275).
Comment Here
Reference: MUM1 / IRF4
Comment Here
Reference: MUM1 / IRF4