Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Sites | Pathophysiology | Etiology | Diagnosis | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Molecular / cytogenetics descriptionCite this page: Obeng R. PMS2. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/stainspms2.html. Accessed May 13th, 2024.
Definition / general
- PMS2 is a component of the DNA mismatch repair system
- The PMS2 gene (on chromosome 7) encodes an endonuclease that forms a heterodimer with MLH1 to form the MutL alpha complex which is activated upon recognition of DNA mismatches, insertions or deletions by MutS alpha and MutS beta heterodimers
Essential features
- Germ line mutations in PMS2 are associated with increased risk of colorectal cancer, hereditary nonpolyposis colon cancer, Lynch syndrome, Turcot syndrome and endometrial cancer
- Milder microsatellite instability (less risk of developing cancer compared to MLH1 mutations)
- Deficiency in PMS2 is usually due to epigenetic repression (via mutations in or hypermethylation of MLH1)
Terminology
- PMS1 homolog 2, mismatch repair system component, HNPCC4, PMS2L, PMSL2, MLH4
Epidemiology
- Mutations in PMS2 have low penetrance for Lynch syndrome (35%) (Gastroenterology 2008;135:419)
- Colorectal cancer in patients with Lynch Syndrome:
- PMS2 mutations are associated with 15% - 20% in males and females (Exp Rev Mol Diagnostics 2016;16:591)
- Endometrial cancer:
- PMS2 mutation is associated with 12% - 15% increased risk of endometrial cancer (J Clin Oncol 2015;33:319, Exp Rev Mol Diagnostics 2016;16:591)
Sites
- Ubiquitous nuclear expression in normal tissue
Pathophysiology
- Genetic alterations in PMS2 contribute to DNA mismatch repair deficiency that leads to microsatellite instability and increased risk of cancer
- PMS2 is unstable in absence of MLH1
- Loss of expression of MLH1 due to mutations generally leads to loss of expression PMS2 as well (Adv Anat Pathol 2009;16:405; Exp Rev Mol Diagnostics 2016;16:591)
Etiology
- Germline or sporadic mutations in PMS2 lead to microsatellite instability
Diagnosis
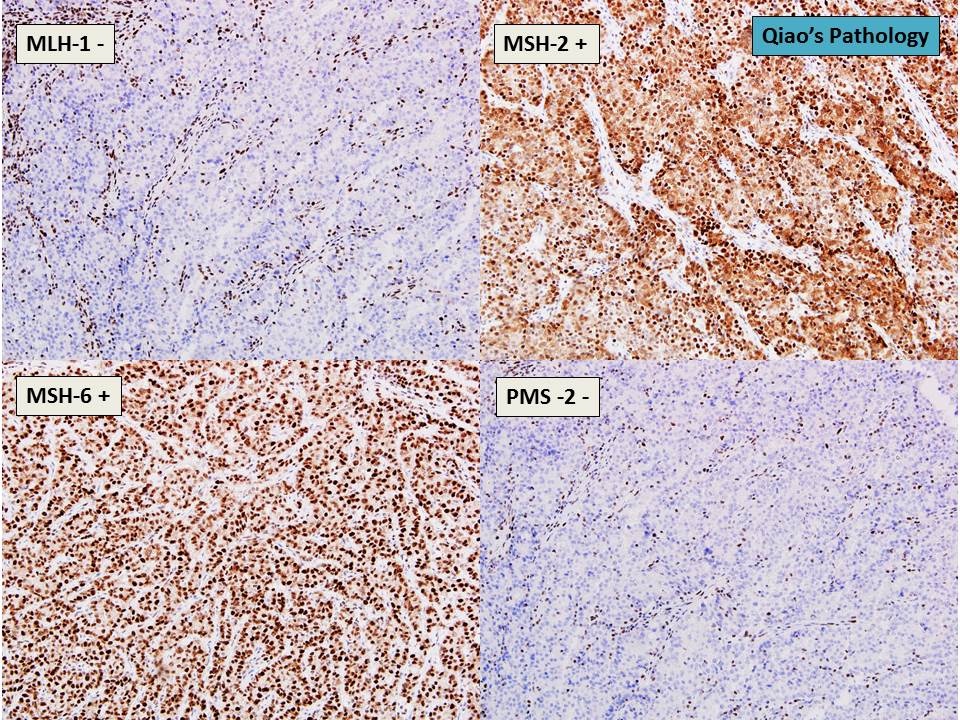
- Screening: immunohistochemical (IHC) stain. Loss of nuclear
staining suggests microsatellite instability
- Lack of PMS2 staining is generally due to mutations in MLH1 and raises suspicion for germline mutations (Cancer Treat Rev 2016;51:19)
- Missense and point mutations that lead to nonfunctional protein can result in false negative results on IHC
- Confirmatory: molecular studies (PCR for microsatellite instability)
- High (MSI-H): at least 2 of 5 unstable markers or greater than or equal to 30% of unstable markers
- Low (MSI-L): one of five unstable markers or less than 30% of unstable markers
Prognostic factors
- Microsatellite instability due to mutations in PMS2 or other proteins is associated with better prognosis in comparison with microsatellite stable colorectal cancers (Ann Surg 1998;227:51; Clin Cancer Res 2005;11:8332; Ann Oncol 2013;24:1274; Cancer Epidemiol Biomarkers Prev 2001;10:917)
Case reports
- 15 year old girl with rectal cancer, with a novel MLH1 and MSH6 biallelic inheritance (Int J Colorectal Dis 2015;30:435)
- 34 year old woman with Lynch syndrome associated rectal cancer and novel PMS2 mutation (Jpn J Clin Oncol 2015;45:987)
Treatment
- Anti-PD-1 pathway blockade therapy for mismatch repair deficient colorectal cancers are in clinical trials with some showing significant objective response (Mod pathol 2009;22:1186; Clin Cancer Res 2013;19:462; N Engl J Med 2015;372:2509)
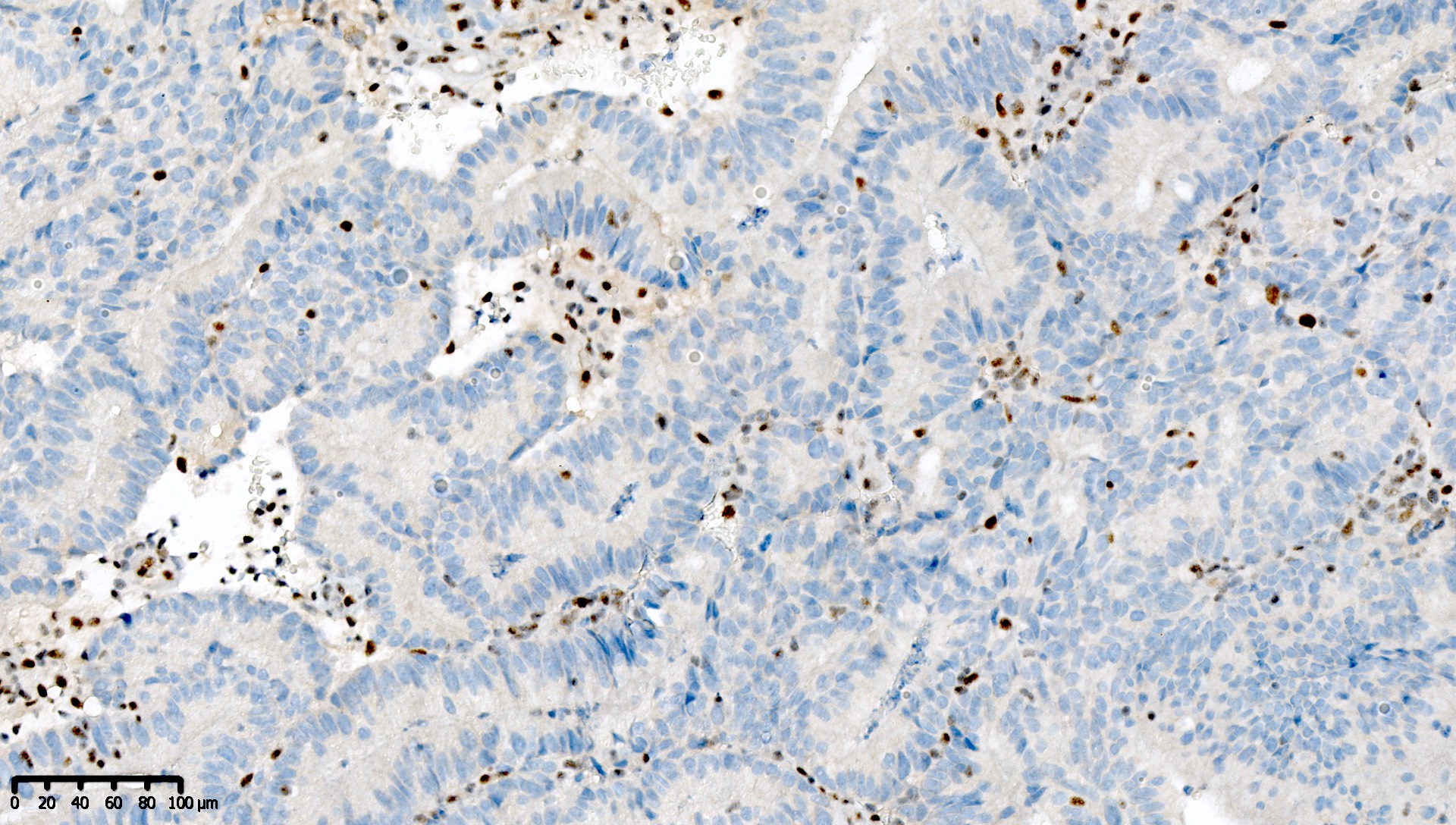
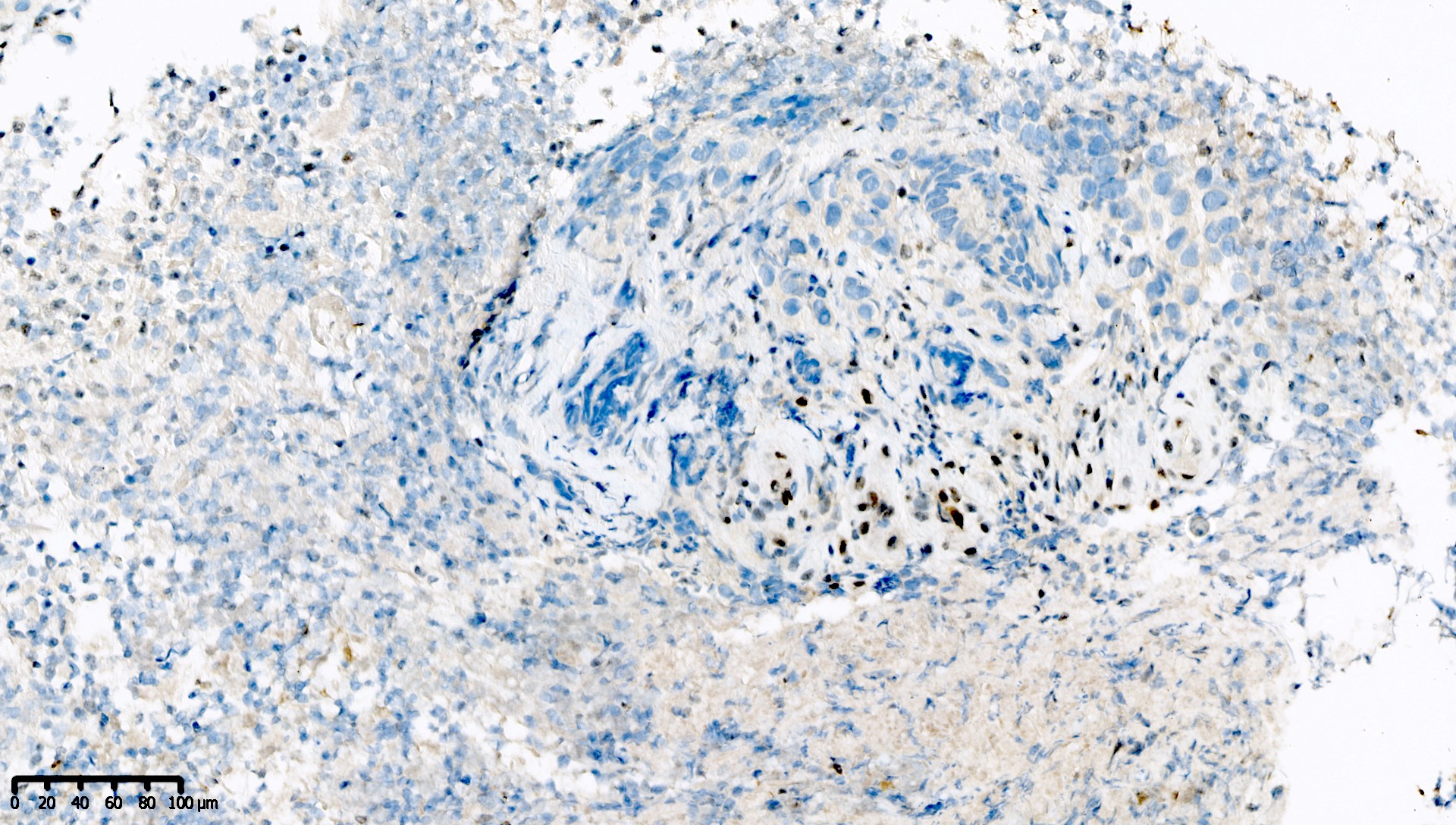
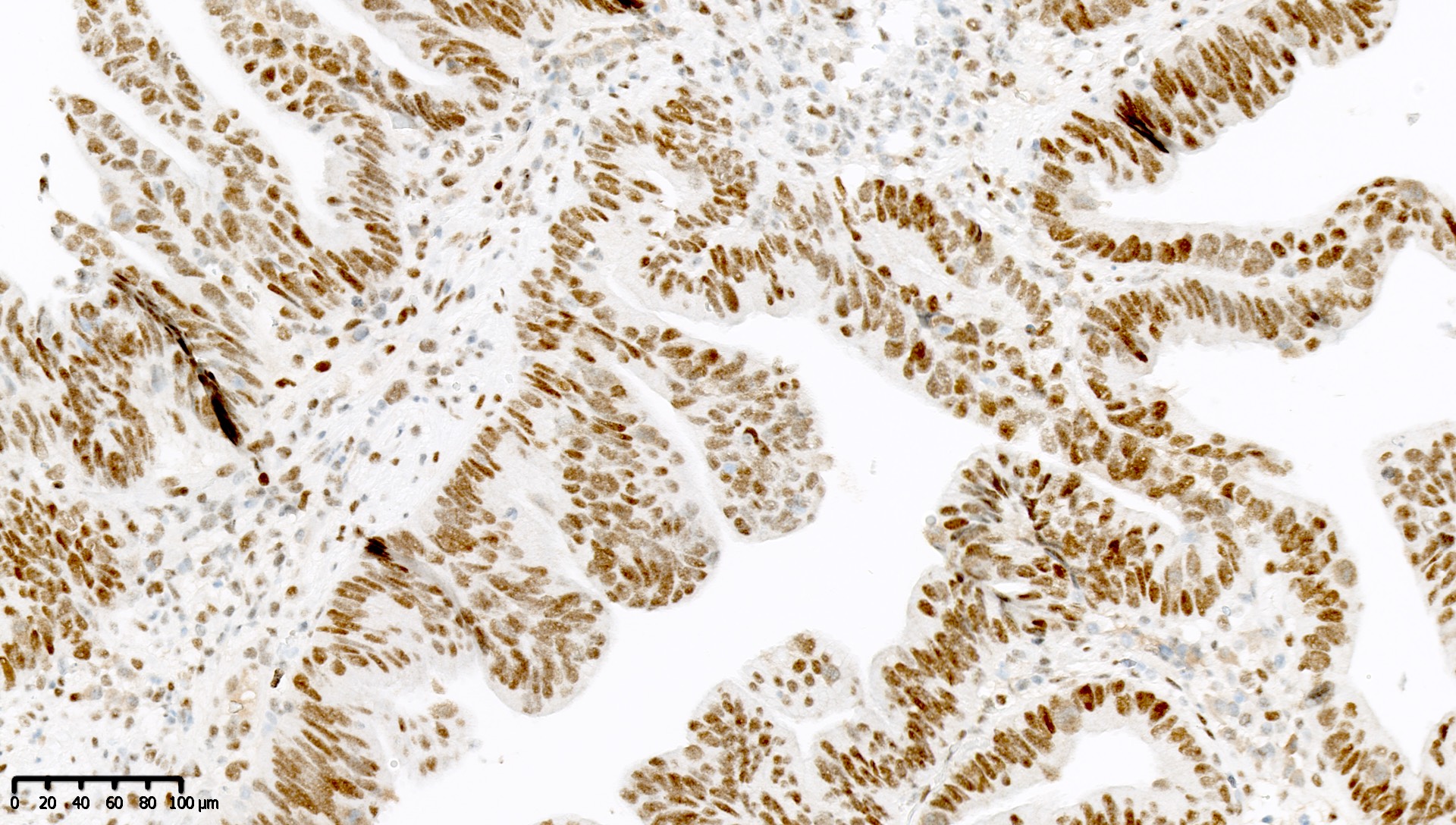
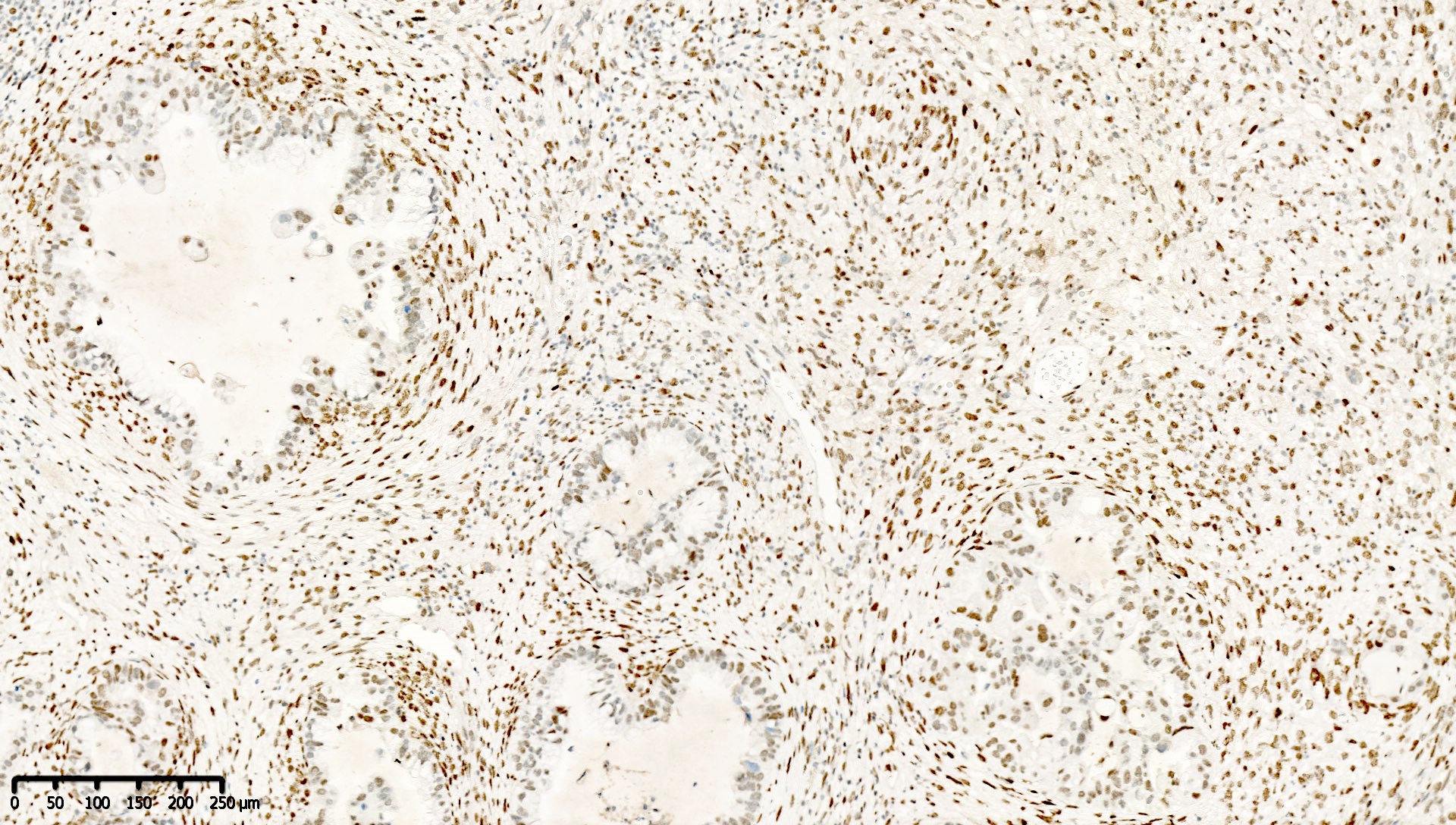
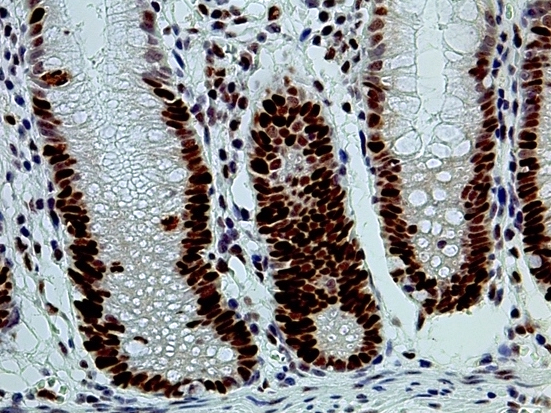
Microscopic (histologic) description
- Normal staining pattern: nuclear
- Cytoplasmic staining is abnormal and should not be misinterpreted as normal staining
Microscopic (histologic) images
Contributed by Mieke R. Van Bockstal, M.D., Ph.D., Jian-Hua Qiao, M.D. and Epitomics
Images hosted on other servers:
Molecular / cytogenetics description
- National Cancer Institute recommendations: 5 microsatellite markers (BAT25, BAT26, N2S123, N5S346 and D17S250) for sequencing (Cancer Res 1998;58:5248) (additional markers may be used, however, there is no consensus on which markers to use)
- Sanger sequencing for germline mutations
- Multiplex ligation dependent probe amplification for large copy number variant detection
- Next generation sequencing