12 September 2012 - Case #251
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Drs. Neha Ahuja, S. R. Desai, Neha Gajbi and N.J. Patil, Krishna Institute of Medical Sciences University (India), for contributing this case and the discussion.
Advertisement
Case #251
Clinical history:
A 68 year old man presented with multiple, brown-colored macules and plaques of varying sizes on the face and throughout his body. These lesions were initially small and limited, but increased in size and number over the past 7 years. There were no similar complaints by family members. Numerous tiny pits were seen over the palms and soles. The patient also had skeletal deformities, Sprengel's deformity and pectus deformity (Wikipedia: Sprengel's deformity [Accessed 11 April 2024], Nursing Times: Pectus deformities: causes and effects [Accessed 11 April 2024]).
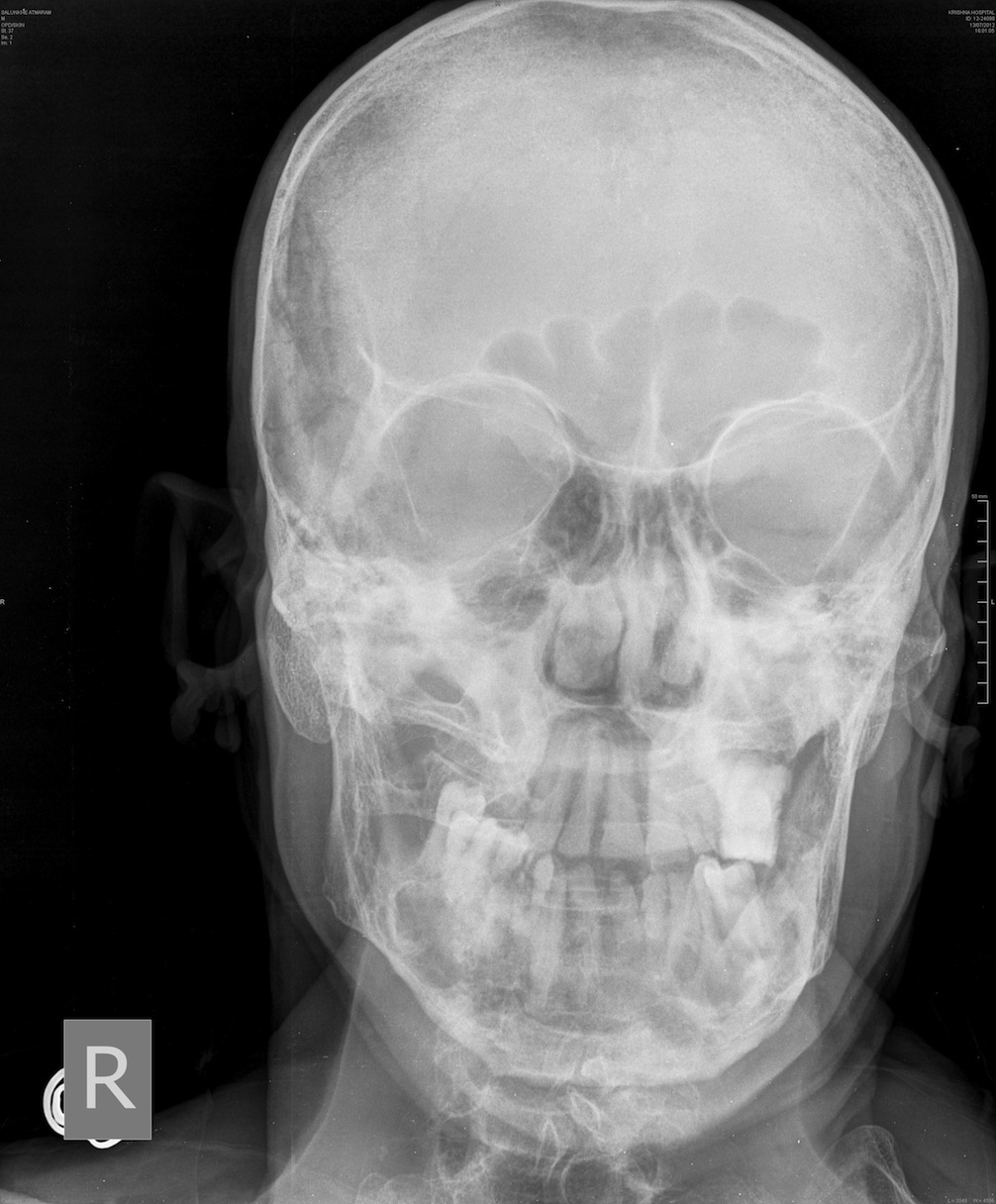
In addition, there was frontal bossing, broadening of the nasal bridge and displacement of premolar teeth. He had no history of seizures, loss of appetite or weight loss. The ulcerated lesions on the face were excised.
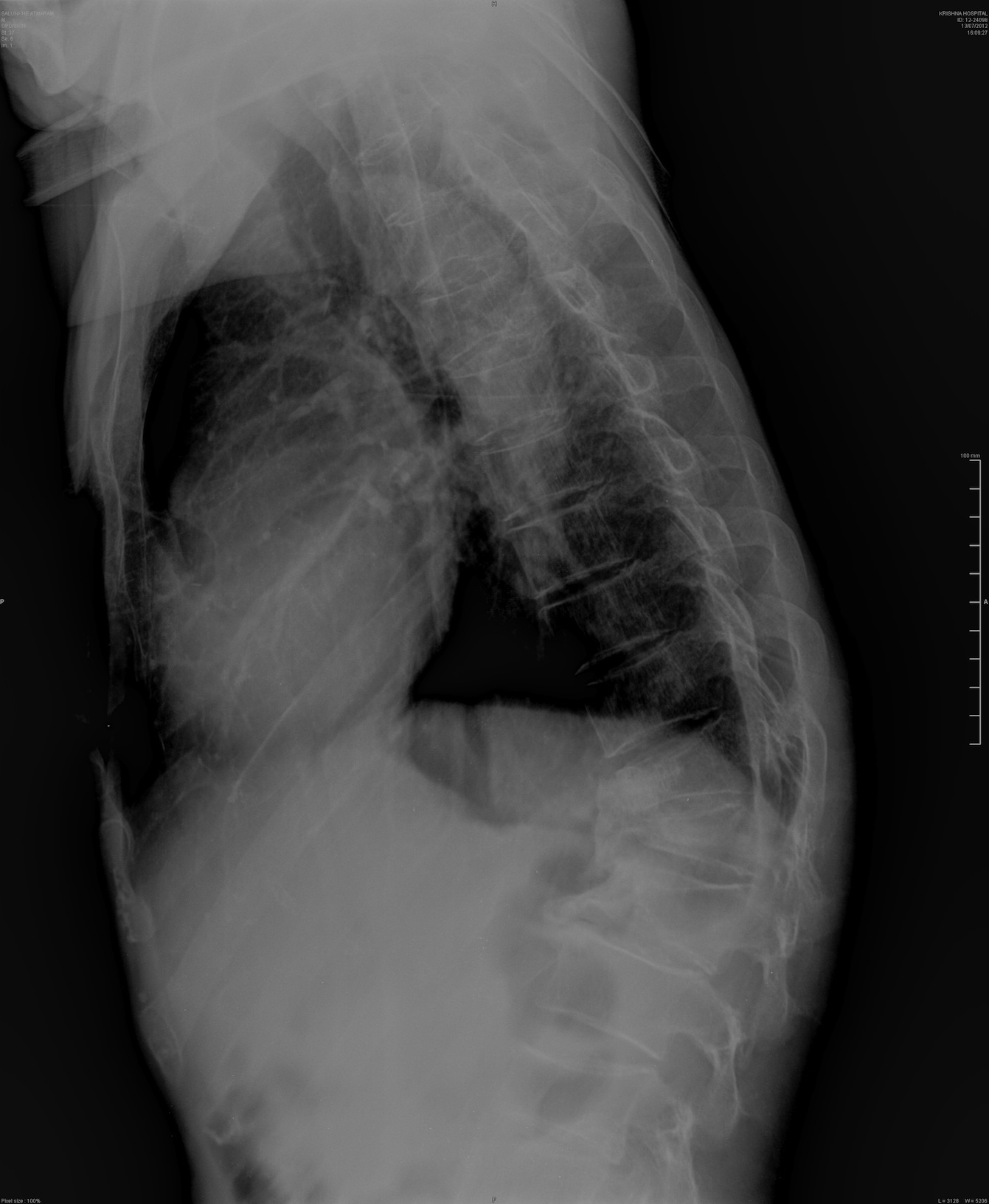
Radiology images:
Clinical images:
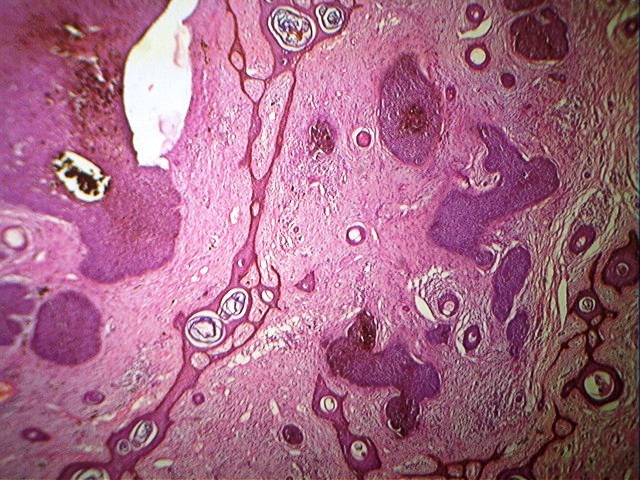
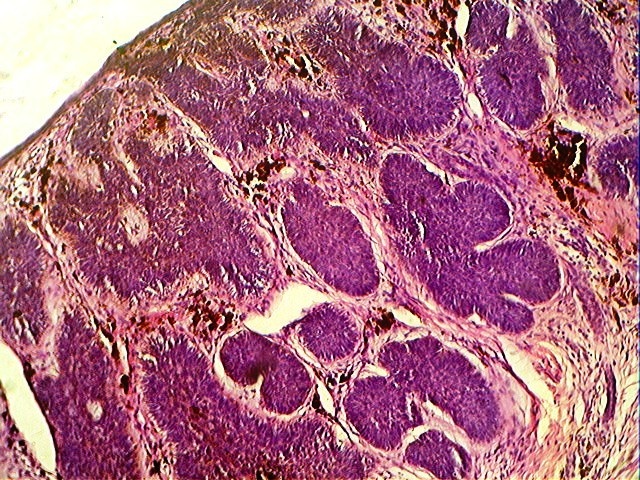
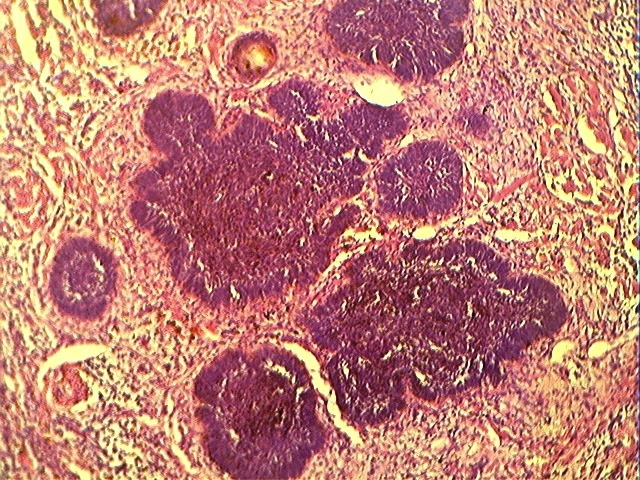
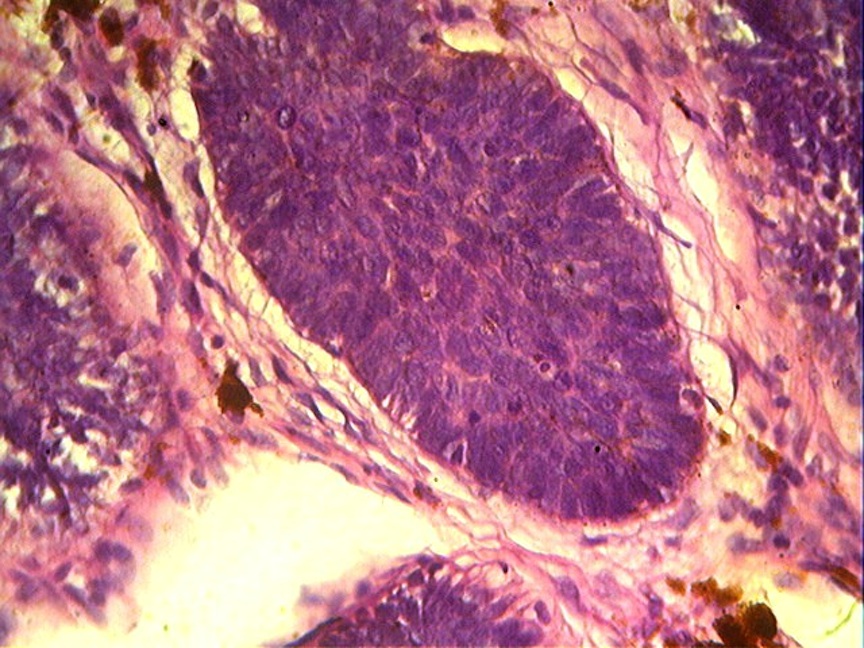
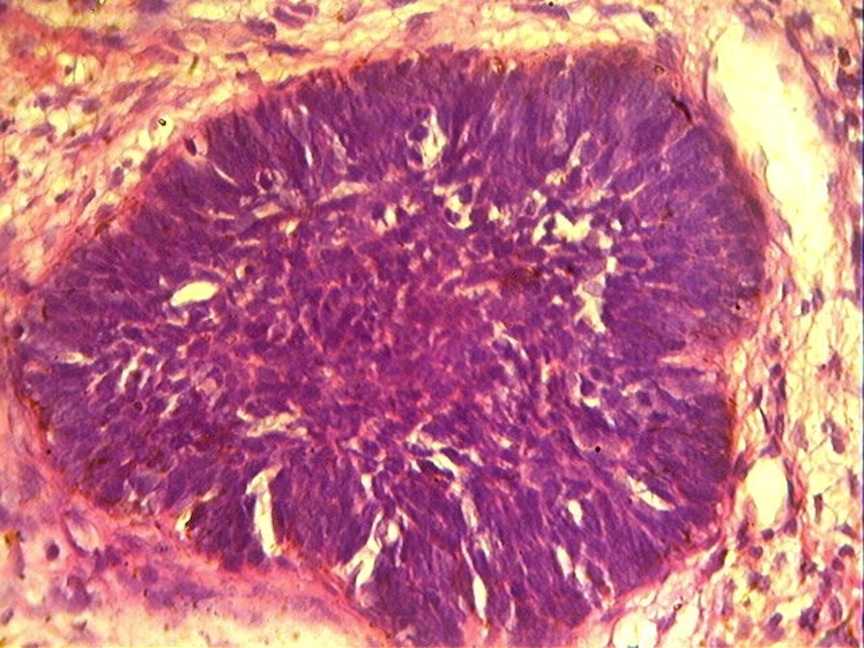
Microscopic images:
What is your diagnosis?
Diagnosis: Gorlin syndrome (nevoid basal cell carcinoma syndrome)
Discussion:
Histology showed tumor nests with basaloid cells, atypical nuclei, melanin pigment and peripheral palisading.
Gorlin syndrome (also called Gorlin-Goltz syndrome) is a rare, autosomal dominant disorder due to mutation of the human patched gene (PTCH1 gene), which provides embryonic structuring and regulatory guidance (Orphanet J Rare Dis 2008 Nov 25;3:32). The mutation causes multiple basal cell carcinomas (BCC) and other associated malignancies, structural anomalies including odontogenic keratocyst of the jaw and skeletal abnormalities including palmar and plantar pits.
The syndrome was first reported by Jarish and White in 1894 and in detail by Gorlin and Goltz in 1960 (N Engl J Med 1960;262:908). The diagnostic criteria was initially outlined by Evans in 1993 and modified by Kimonis et. al. in 1997 (J Med Genet 1993;30:460, Am J Med Genet 1997;69:299). 2 major, or 1 major and 2 minor criteria are essential for diagnosis.
Major criteria:
Minor criteria:
Life expectancy in patients with Gorlin syndrome is not significantly different from normal, but there are cosmetic problems related to the multiple skin tumors and jaw keratocyst.
Differential diagnosis includes rare skin disorders such as Bazex syndrome, trichoepithelioma papulosum multiplex and Muir-Torre syndrome. Establishing the diagnosis helps prevent fatal consequences from skin cancers and other tumors; referral to a genetic counselor is recommended.
Treatment options for the basal cell carcinomas include excision, laser ablation, cryotherapy, photodynamic therapy, fluorouracil cream and oral retinoids. Regular dermatological check up is advised. Odontogenic cysts are removed surgically. Radiotherapy, nonessential diagnostic Xrays and excessive sun exposure should be avoided.
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Drs. Neha Ahuja, S. R. Desai, Neha Gajbi and N.J. Patil, Krishna Institute of Medical Sciences University (India), for contributing this case and the discussion.
November 10, 2012
The Henry, Autograph Collection
Dearborn, Michigan (USA)
8th Annual Course
Contemporary Issues In
Diagnostic Surgical Pathology

Sponsored by the Wayne State University School of Medicine,
Detroit Medical Center and Karmanos Cancer Institute

Course Director: Rouba Ali-Fehmi, M.D.
Website
Schedule
Hotel
Register
Telephone: 313 / 745-2520
Email: rali@med.wayne.edu
Website news:
(1) Thanks for visiting us at CAP '12. We would like your feedback on our plans for the next year, including (a) completing our new Topic format for all chapters, (b) independent reviews and updates of each topic every 1-2 years, (c) making each topic more complete with a more standard format, more content, references and images, (d) adding more images from AFIP fascicles (3rd edition) and contributors, (e) more frequent link checking of images to remove bad links, (f) better formating of website for tablets and smart phones.
(2) The Forensics chapter is now complete, written by Lindsey Harle, M.D. Recent chapter updates include Prostate gland and seminal vesicles, based on reviews by Ali Amin, M.D., Komal Arora, M.D. and Gladell Paner, M.D., and Kidney Tumor (adult malignant), now combined with Kidney tumor (children, benign), based on reviews by Sean Williamson, M.D.
(3) Recent new articles on our Management page include, Medicare Changes Enrollment Guidelines From 30 days to 60 days, by Leigh Polk, PSA, LLC, click here and ACO's, Practice Buy-outs and Dj vu All over Again, by Mick Raich, Vachette Pathology, click here.
Visit and follow our Blog to see recent updates to the website.
(1) Thanks for visiting us at CAP '12. We would like your feedback on our plans for the next year, including (a) completing our new Topic format for all chapters, (b) independent reviews and updates of each topic every 1-2 years, (c) making each topic more complete with a more standard format, more content, references and images, (d) adding more images from AFIP fascicles (3rd edition) and contributors, (e) more frequent link checking of images to remove bad links, (f) better formating of website for tablets and smart phones.
(2) The Forensics chapter is now complete, written by Lindsey Harle, M.D. Recent chapter updates include Prostate gland and seminal vesicles, based on reviews by Ali Amin, M.D., Komal Arora, M.D. and Gladell Paner, M.D., and Kidney Tumor (adult malignant), now combined with Kidney tumor (children, benign), based on reviews by Sean Williamson, M.D.
(3) Recent new articles on our Management page include, Medicare Changes Enrollment Guidelines From 30 days to 60 days, by Leigh Polk, PSA, LLC, click here and ACO's, Practice Buy-outs and Dj vu All over Again, by Mick Raich, Vachette Pathology, click here.
Visit and follow our Blog to see recent updates to the website.
Case #251
Clinical history:
A 68 year old man presented with multiple, brown-colored macules and plaques of varying sizes on the face and throughout his body. These lesions were initially small and limited, but increased in size and number over the past 7 years. There were no similar complaints by family members. Numerous tiny pits were seen over the palms and soles. The patient also had skeletal deformities, Sprengel's deformity and pectus deformity (Wikipedia: Sprengel's deformity [Accessed 11 April 2024], Nursing Times: Pectus deformities: causes and effects [Accessed 11 April 2024]).
In addition, there was frontal bossing, broadening of the nasal bridge and displacement of premolar teeth. He had no history of seizures, loss of appetite or weight loss. The ulcerated lesions on the face were excised.
Radiology images:
Clinical images:
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Gorlin syndrome (nevoid basal cell carcinoma syndrome)
Discussion:
Histology showed tumor nests with basaloid cells, atypical nuclei, melanin pigment and peripheral palisading.
Gorlin syndrome (also called Gorlin-Goltz syndrome) is a rare, autosomal dominant disorder due to mutation of the human patched gene (PTCH1 gene), which provides embryonic structuring and regulatory guidance (Orphanet J Rare Dis 2008 Nov 25;3:32). The mutation causes multiple basal cell carcinomas (BCC) and other associated malignancies, structural anomalies including odontogenic keratocyst of the jaw and skeletal abnormalities including palmar and plantar pits.
The syndrome was first reported by Jarish and White in 1894 and in detail by Gorlin and Goltz in 1960 (N Engl J Med 1960;262:908). The diagnostic criteria was initially outlined by Evans in 1993 and modified by Kimonis et. al. in 1997 (J Med Genet 1993;30:460, Am J Med Genet 1997;69:299). 2 major, or 1 major and 2 minor criteria are essential for diagnosis.
Major criteria:
- Multiple (> 2) basal cell carcinomas or one under 20 years
- Odontogenic keratocysts of the jaws proven by histopathology
- Palmar or plantar pits (3 or more)
- Bilamellar calcification of the falx cerebri
- Bifid, fused or markedly splayed ribs
- First degree relatives with this syndrome
Minor criteria:
- Macrocephaly determined after adjustment for height
- Congenital malformation: cleft lip or palate, frontal bossing, coarse face, moderate of severe hypertelorism
- Other skeletal abnormalities: sprengel deformity, marked pectus deformity, marked syndactyly of the digits
- Radiological abnormalities: bridging of the sella turcica, vertebral anomalies such as hemivertebrae, fusion or elongation of the vertebral bodies, modeling defects of the hands and feet, or flame shaped lucencies of the hands or feet
- Ovarian fibroma
- Medulloblastoma
Life expectancy in patients with Gorlin syndrome is not significantly different from normal, but there are cosmetic problems related to the multiple skin tumors and jaw keratocyst.
Differential diagnosis includes rare skin disorders such as Bazex syndrome, trichoepithelioma papulosum multiplex and Muir-Torre syndrome. Establishing the diagnosis helps prevent fatal consequences from skin cancers and other tumors; referral to a genetic counselor is recommended.
Treatment options for the basal cell carcinomas include excision, laser ablation, cryotherapy, photodynamic therapy, fluorouracil cream and oral retinoids. Regular dermatological check up is advised. Odontogenic cysts are removed surgically. Radiotherapy, nonessential diagnostic Xrays and excessive sun exposure should be avoided.