Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Ricuarte Archila L, Hagen CE. Crohn's disease. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/coloncrohns.html. Accessed April 26th, 2024.
Definition / general
- Chronic, relapsing, idiopathic inflammatory gastrointestinal disease
- Involvement of the upper and lower gastrointestinal tract in a discontinuous and transmural manner
Essential features
- Segmental, patchy inflammatory bowel disease, often involving the ileum, colon and upper GI tract
- Histologically characterized by chronic active colitis with associated transmural lymphoid aggregates and fissuring ulcers
- Noncaseating granulomas are characteristic but neither sensitive nor specific
- Main differential diagnosis: ulcerative colitis, indeterminate colitis and infectious colitis
Terminology
- Terminal ileitis
- Granulomatous enterocolitis
- Regional enteritis
Epidemiology
- Incidence: 0.003 - 0.02%
- Prevalence: 0.3%
- Slight female predominance in adult onset Crohn's disease
- Onset of disease at 20 - 40 years of age with a second peak described at the fifth to sixth decade of life
- More prevalent in Ashkenazi Jewish populations
- Incidence in Hispanic and Asian populations has increased in recent decades
- Incidence and prevalence are higher in high income countries and in urban areas, compared to low income countries and rural areas
- References: Mayo Clin Proc 2017;92:1088, Lancet 2017;389:1741
Sites
- Ileocolonic involvement: 30 - 40%
- Exclusive colon involvement: 30 - 40%, 50% rectal sparing
- Small bowel involvement: 80%
- Exclusive small bowel involvement: 30 - 40%
- Of patients with colon disease, 20% will develop ileal involvement in the next 10 years
- Of patients with ileal disease, 20% will develop colon involvement in the next 10 years
- 52% have right sided colitis, 40% have left sided colitis and 6% have pancolitis
- Approximately 25% have perianal complications, including fissures and fistulas
- Upper gastrointestinal complications are present in 5 - 30%, 50% in children and adolescents
- < 10% present with isolated perianal, upper gastrointestinal or extraintestinal complications
- Reference: Mod Pathol 2012;25:295
Pathophysiology
- Not fully understood
- Immunobiology: impaired intestinal barrier function and dysregulation of the innate and adaptative immune system responses, with an alteration of gut microbiota
- Deficient mucus biofilm barrier: decreased expression of mucin secretion genes (MUC1, MUC19 and PTGER4) in the terminal ileum in patients with Crohn's disease
- Permeability changes in the intestinal epithelium: altered expression of tight junction proteins (claudin)
- Paneth cell dysfunction
- Impaired autophagy of invasive microbes
- Imbalance of effector T cells and naturally regulatory T cells
- Recruitment and erratic retention of leukocytes
- Dysbiosis:
- Continuous alterations in intestinal microbiota resulting in clustering and reduced diversity in Firmicutes and Bacteroidetes phyla
- Reduction in Faecalibacterium prausnnitzii was associated with an increased recurrence of ileal Crohn's disease in the postoperative setting
- Genetic risk factors:
- Increased risk for individuals who have family history
- Concordance in monozygotic twins is 20 - 50% compared with 10% in dizygotic twins
- Wide genome association studies identified 200 loci associated to Crohn's disease; however, they contribute only a modest relative risk increase
- NOD2, ATG16L1, IL23R gene variants are responsible for some of the heritable risk
- Environmental risk factors:
- Cigarette smoking doubles the risk of developing Crohn's disease
- Reduced fiber dietary intake
- Antibiotic therapy during childhood increases the risk of developing Crohn's disease
- Other medications including nonsteroidal anti-inflammatory drugs, oral contraceptives and aspirin
- Breastfeeding appears to be a protective factor against the development of Crohn's disease
- References: Nat Rev Dis Primers 2020;6:22, Lancet 2012;380:1590
Etiology
- Idiopathic
Clinical features
- Signs and symptoms: abdominal pain, diarrhea, fatigue and weight loss
- Involvement of other GI sites can present as oral painful aphthous ulcers, odynophagia and dysphagia, postprandial vomiting and nausea, and malabsorption (including diarrhea and steatorrhea with associated nutritional deficiencies)
- 3 phenotypic clinical subtypes:
- Inflammatory phenotype: inflammation of the GI tract with no fistula or stenosing process; classic symptoms
- Stricturing phenotype: inflammation can progress to fibrosis and stenosis; symptoms are associated with bowel obstruction (i.e., lack of bowel movements, nausea and vomiting)
- Fistulizing phenotype: continuous transmural inflammation can cause sinus tract formation resulting in fistulas between bowel and other organs (vagina and bladder)
- Extraintestinal manifestations:
- Musculoskeletal: arthritis or arthropathy and bone loss
- Ocular: uveitis, iritis and episcleritis
- Cutaneous: erythema nodosum and pyoderma gangrenosum
- Hepatobiliary: primary sclerosing cholangitis, pyogenic liver abscess
- Renal: secondary amyloidosis leading to renal disease, calcium oxalate and uric acid renal stones
- Pulmonary: bronchiectasis, chronic bronchitis, interstitial lung disease, bronchiolitis obliterans with organizing pneumonia, sarcoidosis
- There are several clinical scoring systems that categorize patients into low and high risk (e.g., Crohn's disease activity index and Harvey-Bradshaw index)
- Endoscopic findings:
- Ileocolonoscopy is the gold standard for diagnosis
- Ulceration: small aphthous ulcers (< 5 mm) and transmural ulcers
- Cobblestone appearance: linear and serpiginous ulcers with intervening nonulcerated mucosa
- Skip lesions: discontinuous lesions surrounded by adjacent normal tissue
- Other (less specific) findings:
- Normal rectal mucosa
- Inflammation of the terminal ileum with no colonic inflammation
- Ileocolonoscopy is the gold standard for diagnosis
- References: Mayo Clin Proc 2017;92:1088, Inflamm Bowel Dis 2011;17:471, Gastroenterol Rep (Oxf) 2018;6:75
Diagnosis
- Diagnosis consists of a combination of clinical findings and complementary diagnostic tests including blood tests, stool tests, upper and lower endoscopic studies, radiologic imaging and histologic evaluation
- The aim is to exclude differential diagnoses, establish a diagnosis and classify the severity of the disease
Laboratory
- C reactive protein: nonspecific marker for acute inflammation; correlates with disease activity
- ASCA (anti-Saccharomyces cerevisiae antibodies): positive in 60 - 70% of patients with Crohn's disease, 10 - 15% of patients with ulcerative colitis and < 5% of patients without inflammatory bowel disease
- pANCA (perinuclear antineutrophil cytoplasmic antibodies): positive in 10 - 15% of patients with Crohn's disease, positive in 60 - 70% of patients with ulcerative colitis
- Patients with Crohn's disease with positive pANCA tend to have an ulcerative colitis resembling phenotype
- Fecal calprotectin: fecal biomarker used to distinguish between inflammatory bowel disease and functional bowel disease; elevated levels of fecal calprotectin indicate the need for further investigation for inflammatory bowel disease
- Reference: Lancet 2017;389:1741
Radiology description
- Frequently used to assess disease in the small bowel: bowel ultrasonography, CT scan and MRI are helpful for the assessment of the extent of the disease and presence of complications
- Small bowel findings:
- Asymmetrical segmental mural hyperenhancement: specific to Crohn's disease; other types of segmental mural hyperenhancement are less specific
- Wall thickening
- Intramural edema: indicative of bowel inflammation
- Strictures: more common with fibrosis and inflammation; proximal bowel dilation can correlate with higher fibrotic burden
- Ulcers: indicative of severe inflammation (Radiology 2018;286:776)
- Pelvic MRI: used to evaluate and define perianal fistula tracts (Radiology 2017;282:628)
Radiology images
Prognostic factors
- Associated with a 1.38 increase in mortality
- Recurrence in approximately 95% of patients after 10 years of diagnosis, most commonly as ileocolonic disease
- Postoperative recurrence is dependent on disease location
- Isolated ileal disease recurrence is proximal to anastomosis
- Ileocolitis disease recurrence frequently occurs both proximal and distal to the anastomosis (Gut 2012;61:1140)
- Increased risk for relapse, surgery or complications:
- Patient features:
- Young age at diagnosis (< 40 years)
- Smoking
- Disease features:
- High disease burden and prolonged duration of disease
- Perianal disease
- Stricturing disease
- Involvement of the upper GI tract
- Requiring corticosteroids during first flare
- Lack of epithelial healing after clinical remission
- Presence of deep ulcers
- Granulomas on biopsy specimen
- Laboratory tests:
- High C reactive protein and ASCA
- High fecal calprotectin levels
- Low serum levels of albumin and hemoglobin
- Patient features:
- Patients with Crohn's disease have an increased risk for:
- Colorectal cancer and death from colorectal cancer (Lancet Gastroenterol Hepatol 2020;5:475)
- Small bowel carcinoma (Ann Oncol 2009;20:574, Dig Liver Dis 2021;53:809)
- Anal squamous cell carcinoma (Cancers (Basel) 2021;13:1445, J Crohns Colitis 2017;11:1011)
- Lymphoproliferative disorders (Ann Oncol 2009;20:574, Dig Liver Dis 2021;53:809)
Case reports
- 3 year old boy with a case of early childhood Crohn's disease (Hosp Pediatr 2016;6:248)
- 12 year old girl with the cobblestone sign (Dtsch Arztebl Int 2017;114:472)
- 20 year old man with type 2 autoimmune pancreatitis with Crohn's disease (Intern Med 2018;57:2957)
- 31 year old man with pulmonary Crohn's disease (Dig Dis Sci 2017;62:64)
- 37 year old woman with unusual presentation of Crohn's disease (BMJ Case Rep 2021;14:e242703)
- 6 cases of colorectal cancer in Crohn's disease (Surg Case Rep 2021;7:152)
Treatment
- Mainstay of treatment is medical therapy with a goal to achieve clinical, endoscopic and histologic remission, demonstrated by complete mucosal healing
- Chosen based on disease stage, severity and location
- Low risk patients: step up therapy; initially less potent medications with better adverse effect profile are used, while more potent medications are reserved for patients who do not respond to the initial approach
- High risk patients: top down therapy; potent therapies, including biologic therapy and immunomodulators, are used early in the disease to prevent complications
- Medical therapies:
- Corticosteroids
- Thiopurines
- Methotrexate
- Anti-TNF agents
- Surgical therapy: approximately 50% of patients with Crohn's disease will have at least 1 surgical procedure due to disease complications
- Stricturing disease: irreversible with medical therapy; if obstructive symptoms are ongoing, surgery may be indicated
- Fistulizing disease: cases of enterovesicular, enterovaginal and enterocutaneous fistulas or sinus tract and abscess formation
- Perianal disease: perianal fistula or abscess
- Reference: Gastroenterology 2014;147:702
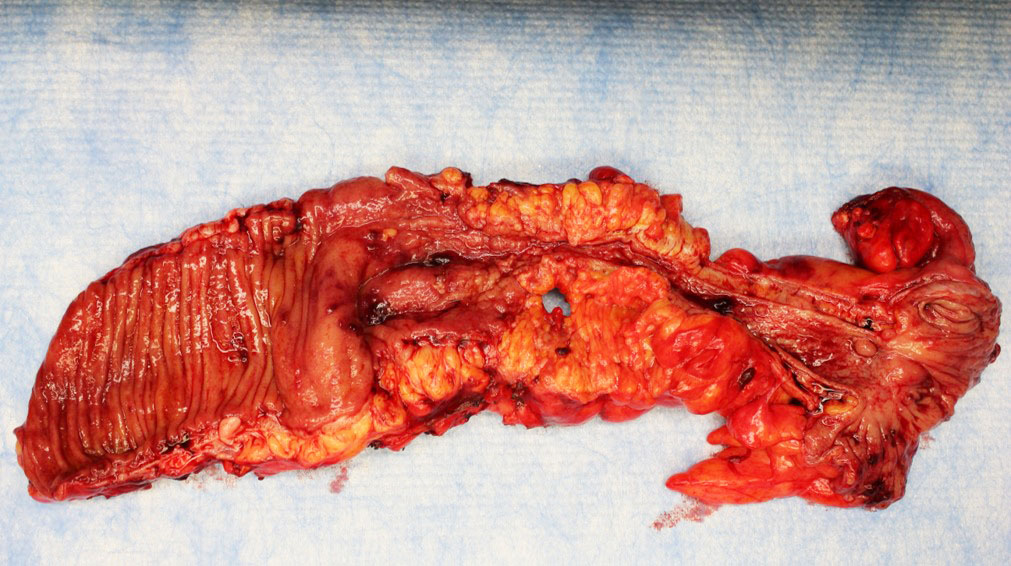
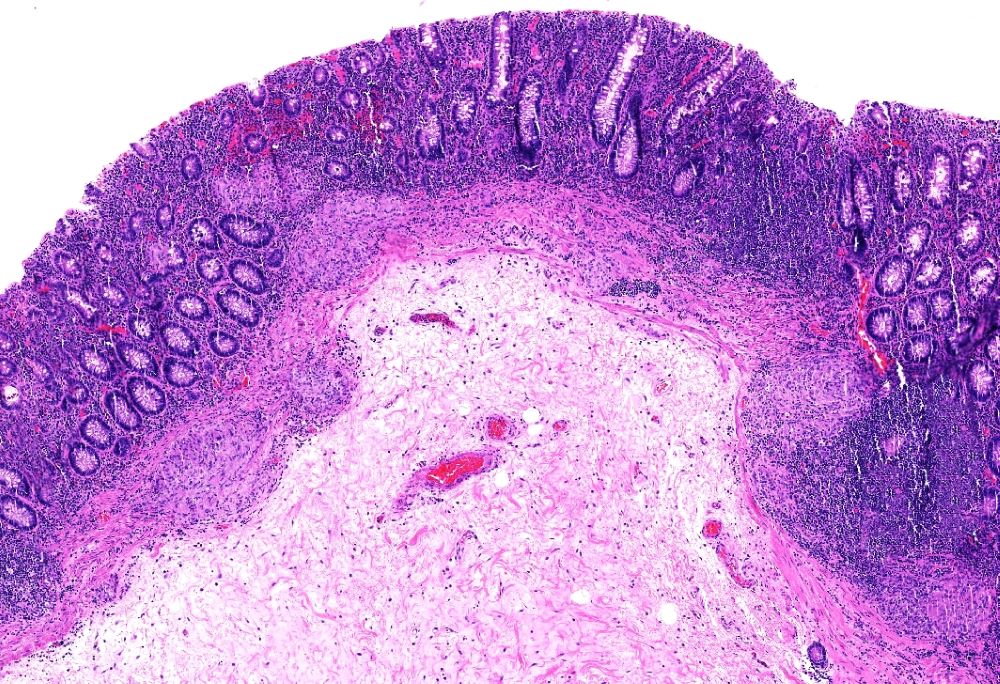
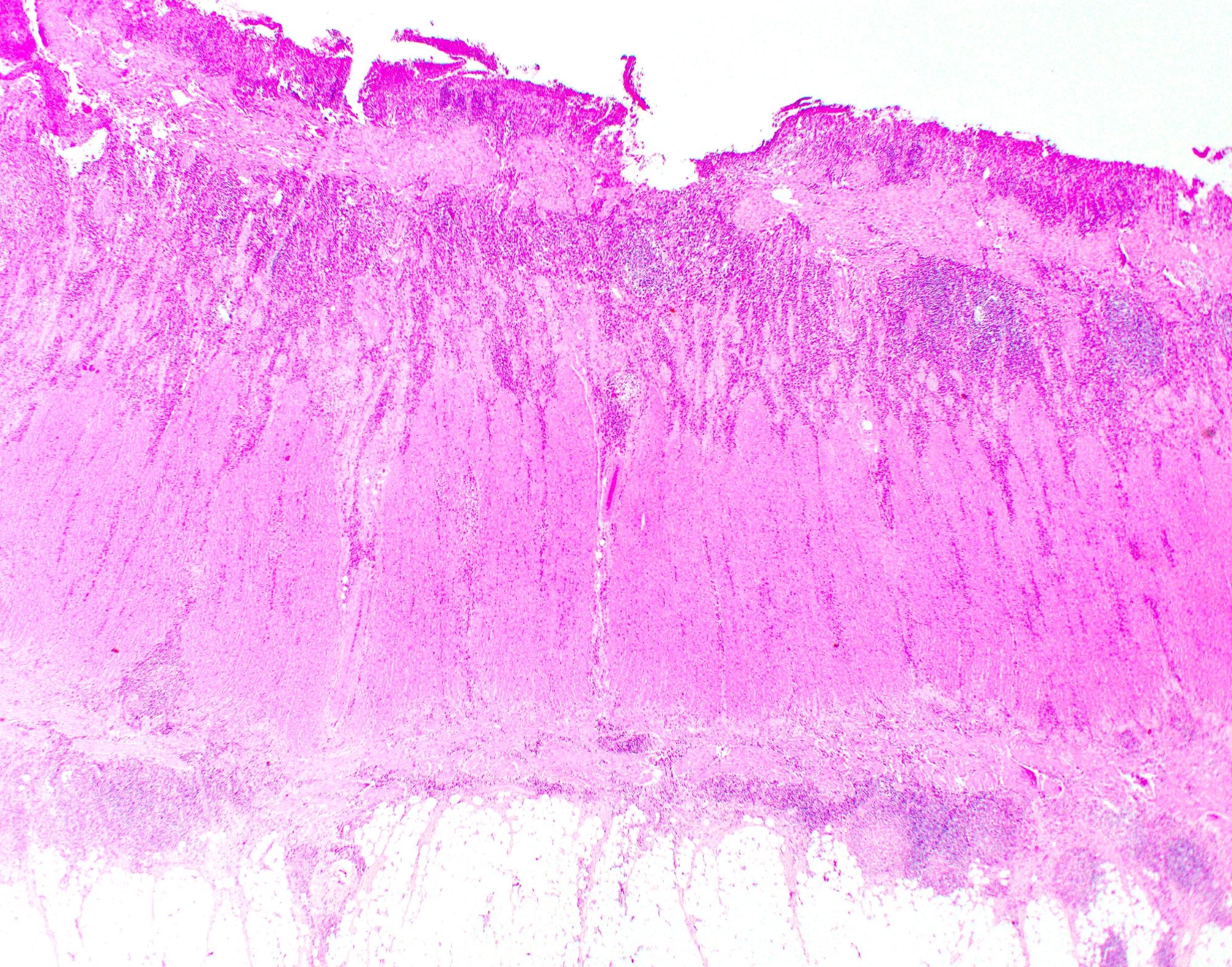
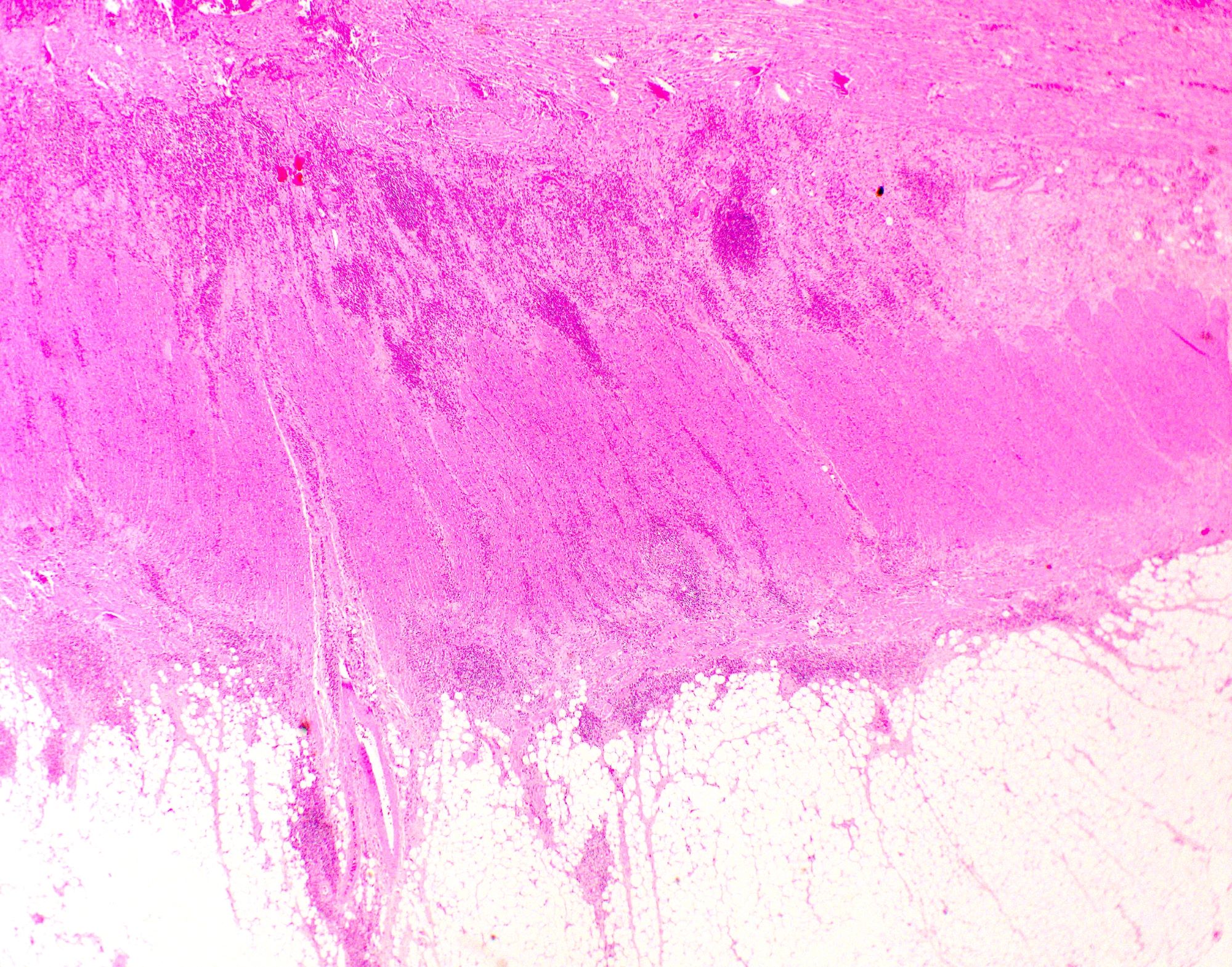
Gross description
- Segmental involvement of the bowel
- Creeping fat due to transmural inflammation
- Thickened and fibrotic bowel walls with stricture formation
- Mucosal aphthous ulcers surrounded by hyperemia with eventual formation of a cobblestone appearing mucosa
- Inflammatory pseudopolyps
- Fissures, sinus and fistulous tracts and abscesses in the setting of complicated disease
- Perforations, rarely
- Reference: Odze and Goldblum: Surgical Pathology of the GI Tract, Liver, Biliary Tract and Pancreas, 3rd Edition, 2015
Gross images
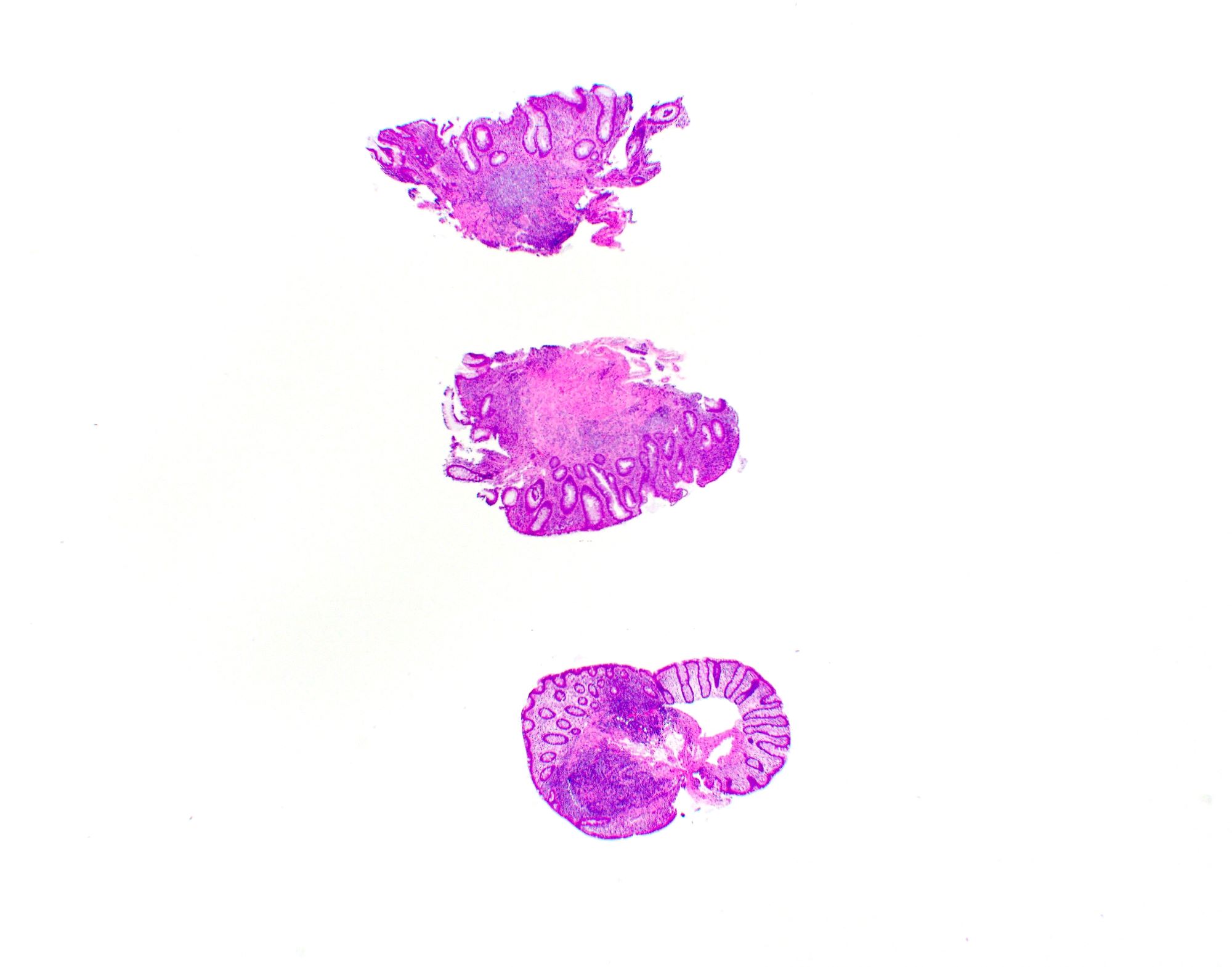
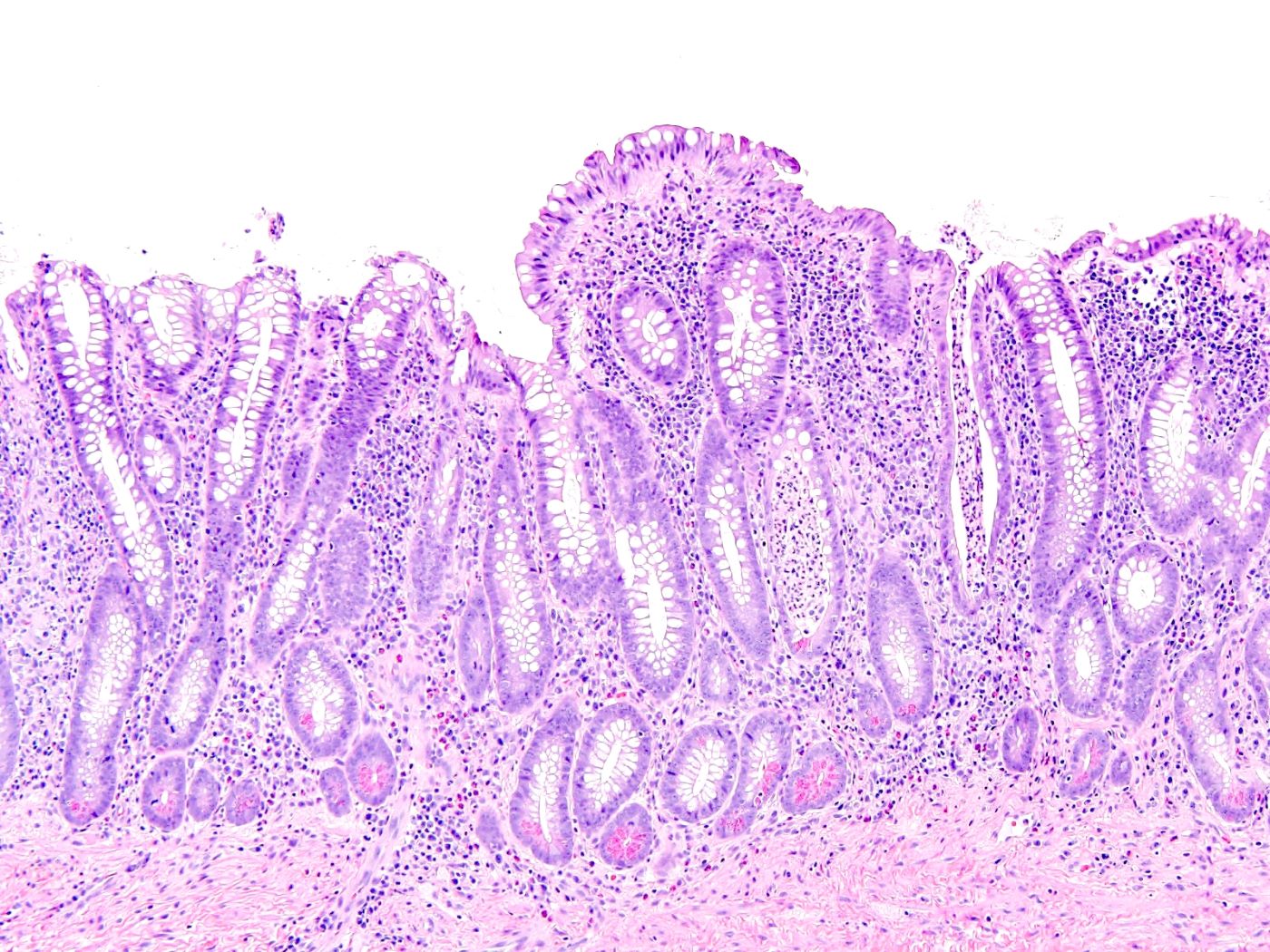
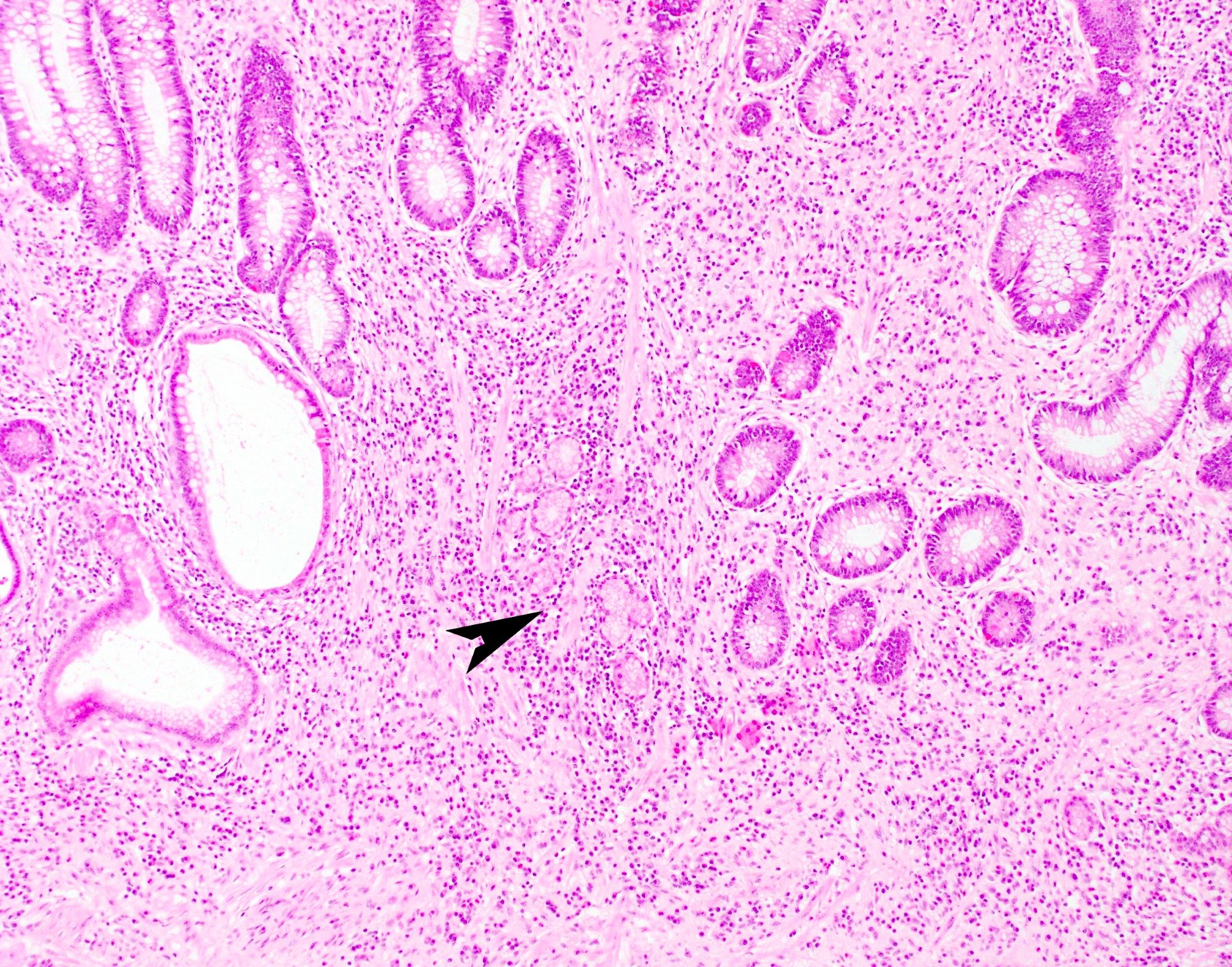
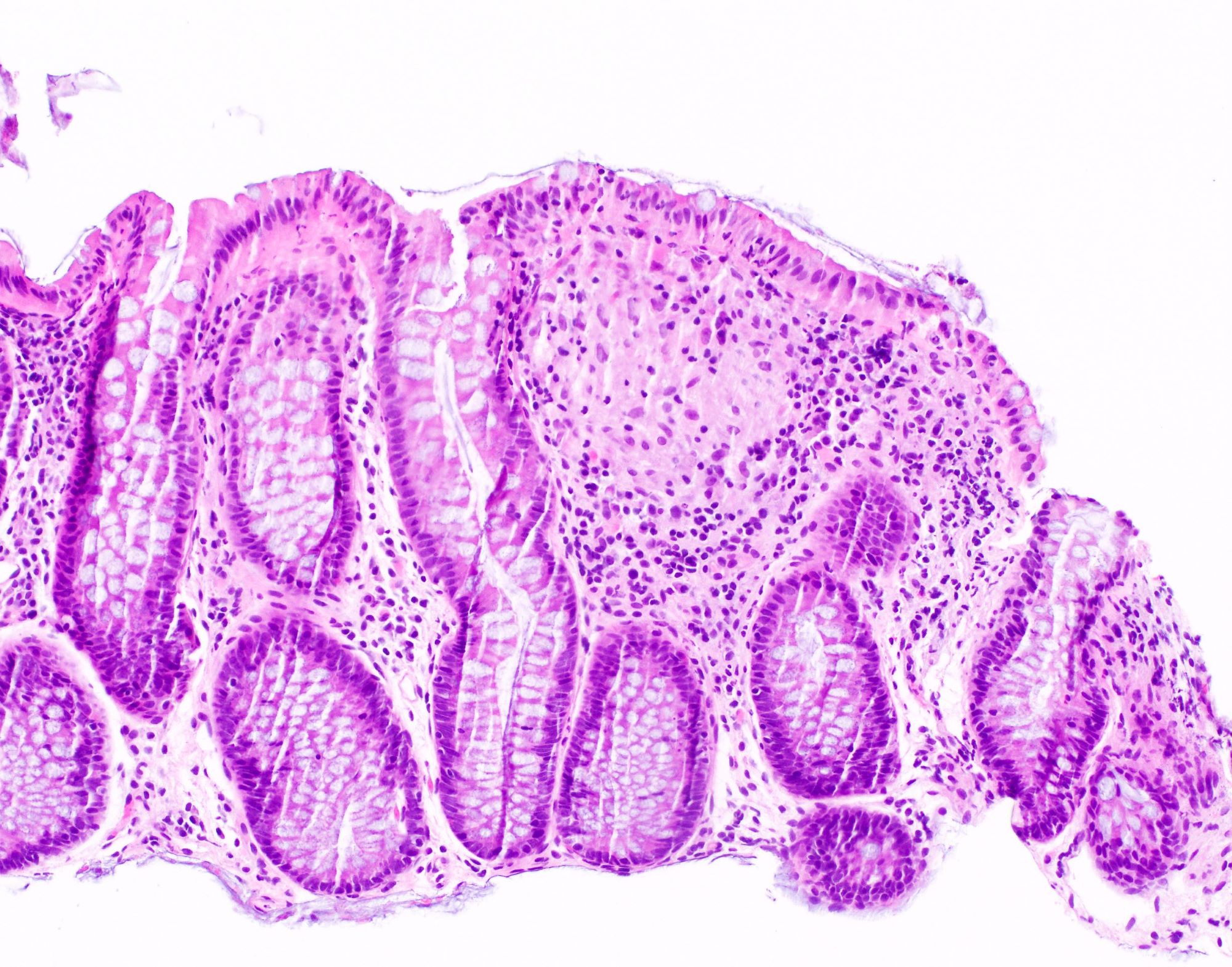
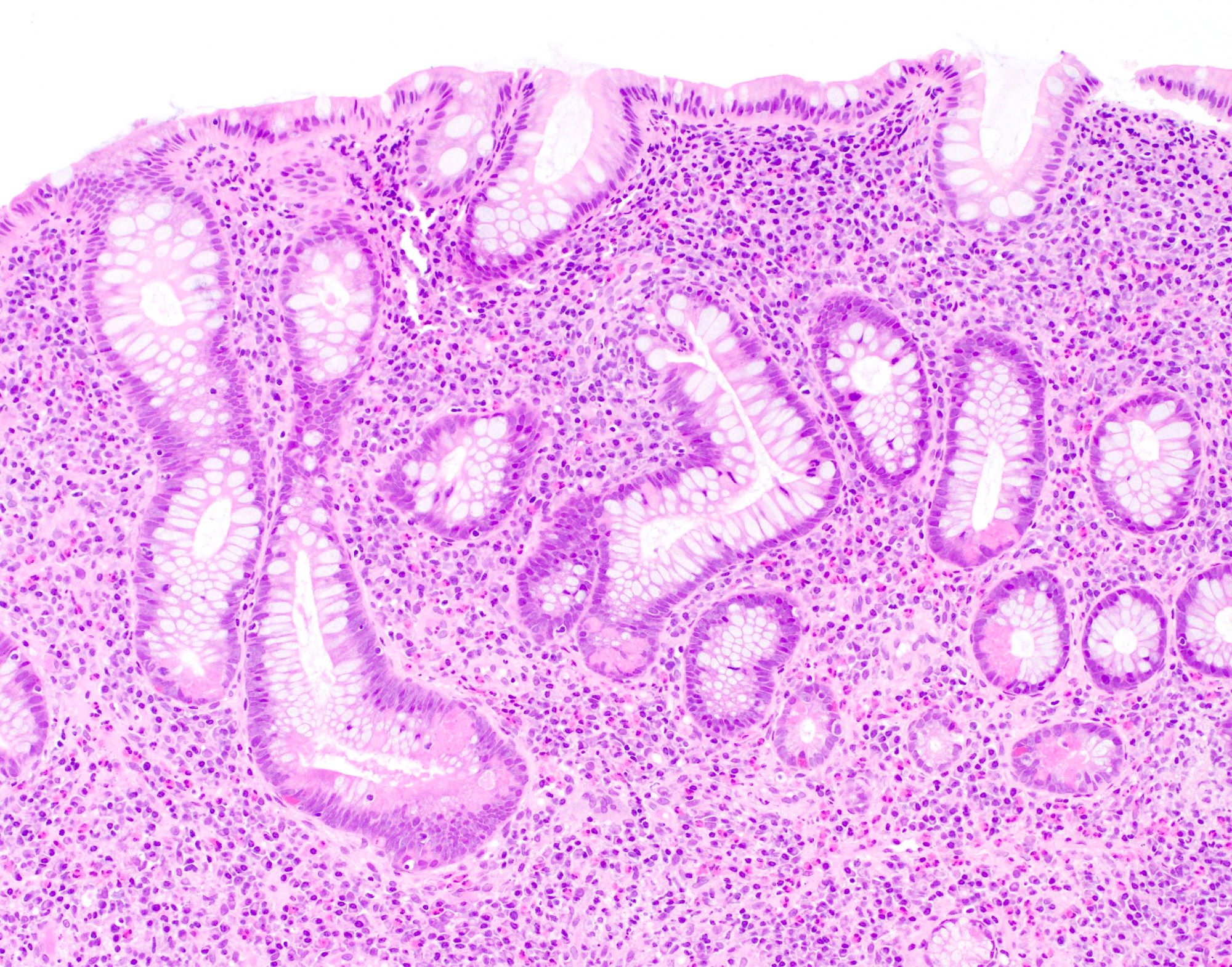
Microscopic (histologic) description
- Similar to ulcerative colitis, untreated cases typically show features of active chronic colitis
- Features of chronicity include:
- Crypt architectural distortion
- Inflammatory expansion of the lamina propria with basal lymphoplasmacytosis
- Paneth cell metaplasia or hyperplasia
- Pyloric gland metaplasia of small bowel and right colon
- Features of activity include neutrophilic inflammation with cryptitis, crypt abscess and ulceration
- Patchy and segmental distribution with skip lesions
- Aphthous ulcers and deep fissuring ulcers
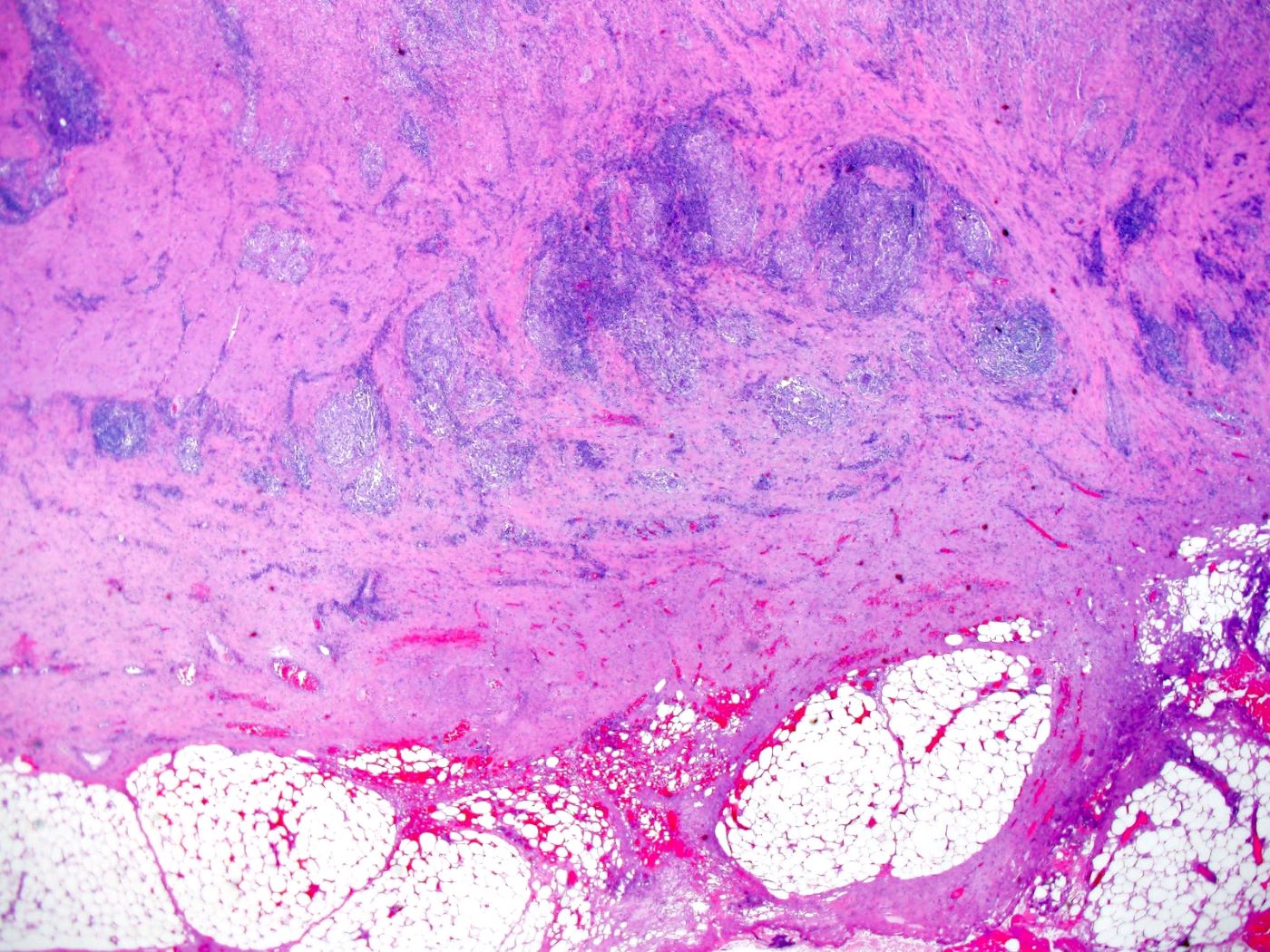
- Granulomas are characteristic but only present in approximately 50% of patients (Colorectal Dis 2011;13:1142)
- Often well formed and sarcoid-like but may be poorly formed or consist of giant cells
- Should be distinguished from crypt rupture granuloma
- Transmural inflammation with lymphoid aggregates in the subserosal adipose tissue
- Sinus tracts and fistula formation
- Biopsies are limited in determining the depth and distribution of inflammation; therefore, diagnosis is often reliant on clinical correlation or examination of the resection specimen (Histopathology 2014;64:317)
- Dysplasia may be present in patients with longstanding disease
- Activity is usually graded similar to ulcerative colitis (Gastroenterology 2007;133:1099):
- Inactive: absence of neutrophils
- Mild: activity involving < 50% of the mucosa
- Moderate: activity involving > 50% of the mucosa; crypt abscesses often seen
- Severe: presence of surface ulceration or erosion
- References: Histopathology 2014;64:317, Best Pract Res Clin Gastroenterol 2019;38:101601
Microscopic (histologic) images
Negative stains
Sample pathology report
- Colon, biopsy:
- Mildly active chronic colitis with multiple nonnecrotizing granulomas (see comment)
- Comment: The histologic findings are suggestive of idiopathic inflammatory bowel disease. Presence of multiple nonnecrotizing granulomas favors Crohn's disease over ulcerative colitis but clinical correlation with distribution of disease is required.
- Colon, resection:
- Severely active chronic colitis with transmural inflammation and fissuring ulcers compatible with Crohn's colitis; no dysplasia or malignancy
Differential diagnosis
- Ulcerative colitis:
- Diffuse involvement of the colon and rectum
- Absence of skip lesions, except in treated cases
- Absence of granulomas, except when associated with ruptured crypts
- Backwash ileitis: in the setting of severe cecal disease, frequently without severe activity or chronic changes
- Indeterminate colitis:
- Diagnosis of exclusion when it is impossible to distinguish between ulcerative colitis and Crohn's disease
- This term is only used when a resection specimen is available
- Infectious colitis:
- Presence of noncaseating granulomas
- Yersinia:
- Central necrosis within granulomas and lack of transmural inflammation
- Salmonella and Campylobacter:
- Poorly circumscribed microgranulomas
- Tuberculosis:
- Florid coalescent granulomatous inflammation, extensive caseous necrosis and nodal granulomas with no intramural granulomas
- Segmental colitis associated with diverticulitis:
- Inflammation limited to segment of colon with diverticulosis
Board review style question #1
Board review style answer #1
Board review style question #2
Board review style answer #2