Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Pathophysiology | Etiology | Clinical features | Laboratory | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Gonzalez R S. Cholestasis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/livercholestasis.html. Accessed May 6th, 2024.
Definition / general
- Decrease in bile flow due to hepatocellular dysfunction or biliary obstruction
Essential features
- Microscopically visible bile, usually in hepatocyte cytoplasm or canaliculi
- Seen in most forms of biliary pattern injury
Terminology
- Bland cholestasis refers to cholestasis as an isolated microscopic finding
- Cholestatic hepatitis refers to microscopic cholestasis alongside inflammatory findings (that is, hepatitis)
- Histologic cholestasis sometimes referred to as bilirubinostasis
ICD coding
- ICD-10: K71.0 - toxic liver disease with cholestasis
Pathophysiology
- Bile is produced in hepatocytes and flows as follows: hepatocyte canaliculi → canals of Hering → bile ductules → interlobular bile ducts → larger bile ducts → duodenum
- Injury or obstruction at any point along biliary flow can lead to cholestasis
Etiology
- Most typically seen in biliary disease (primary sclerosing cholangitis, primary biliary cirrhosis) or drug induced liver injury (Hepatology 2011;53:1377)
- Other causes include pregnancy, benign familial recurrent cholestasis, sepsis (World J Gastroenterol 2009;15:2049)
Clinical features
- Patients with cholestasis may have jaundice, pruritus (due to bile acid deposition in skin), skin xanthomas (due to hyperlipidemia), deficiencies of fat soluble vitamins (A, D, E, K)
- Clinical cholestasis may not correlate with histologic cholestasis
Laboratory
- Elevated serum alkaline phosphatase (present in bile duct epithelium and hepatocyte canalicular membrane), elevated serum bilirubin
Treatment
- Varies depending on etiology
- Ursodeoxycholic acid and obeticholic acid can improve symptoms of cholestatic liver disease (Hepatology 2002;36:525 GR)
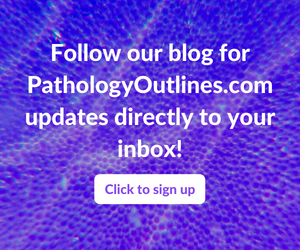
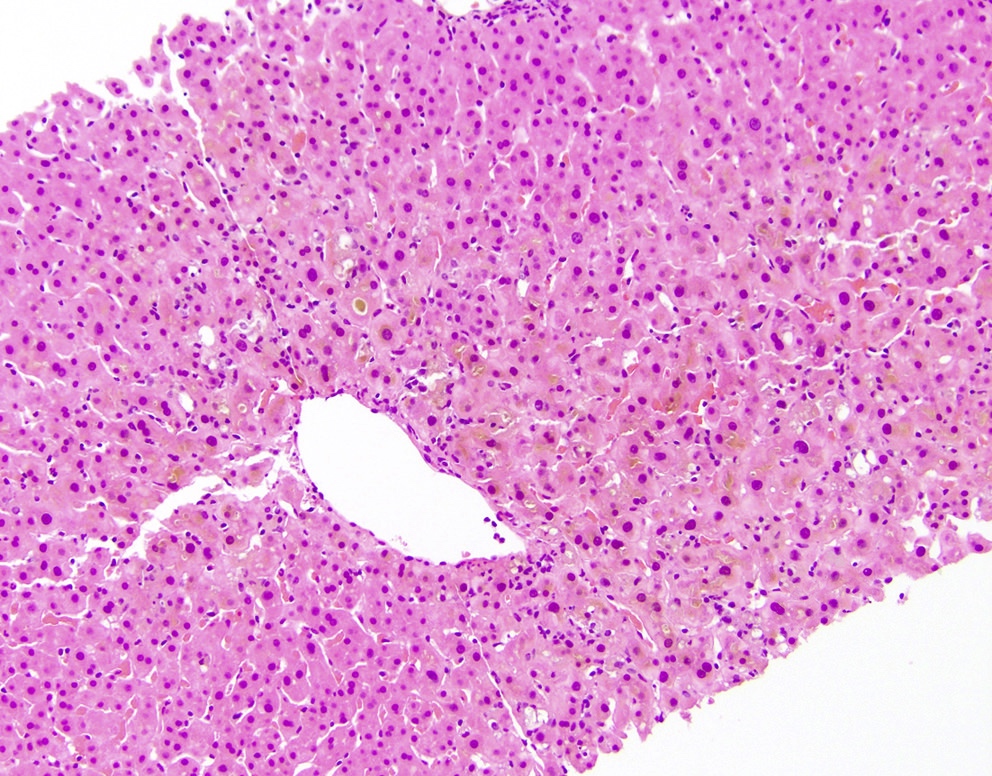
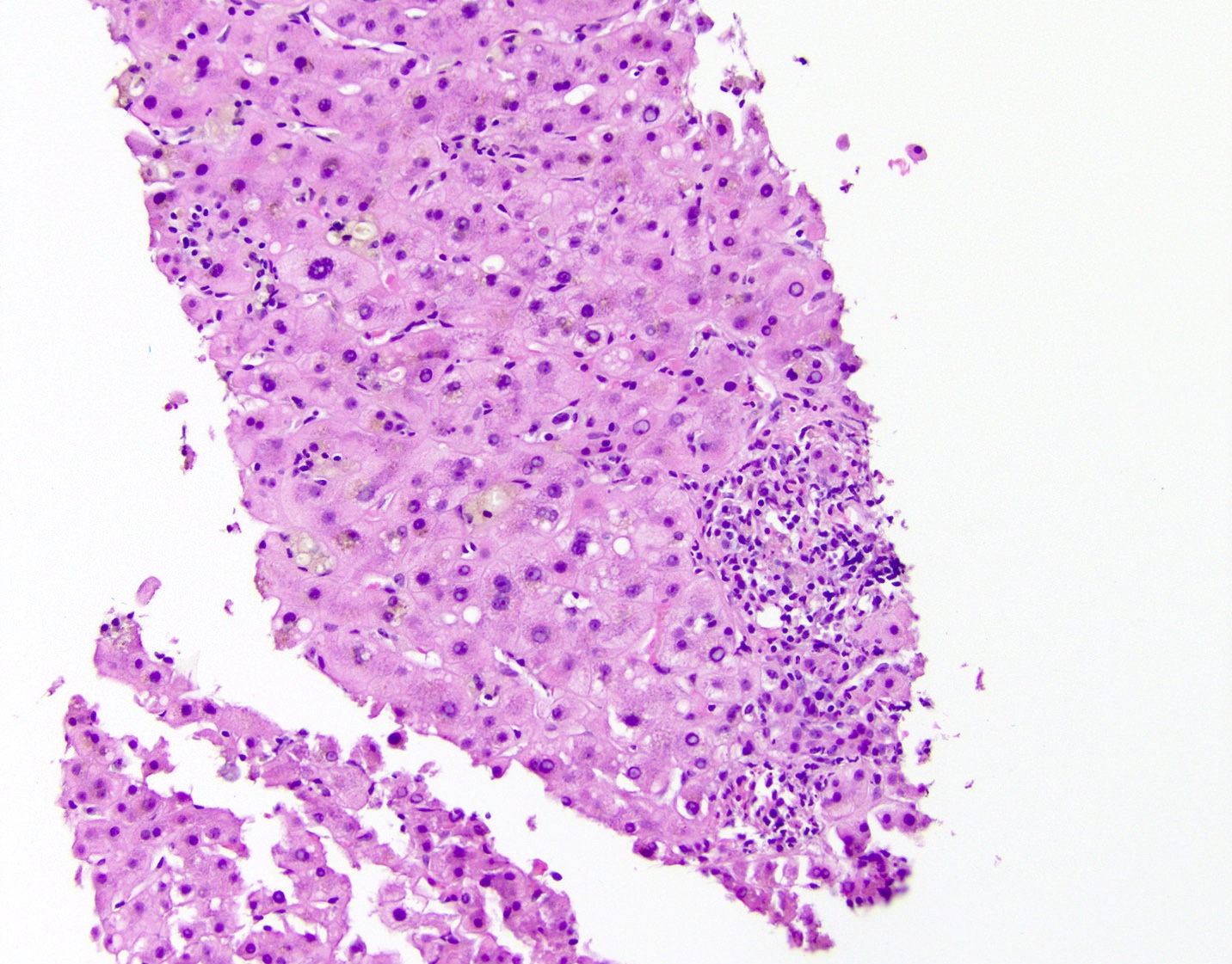
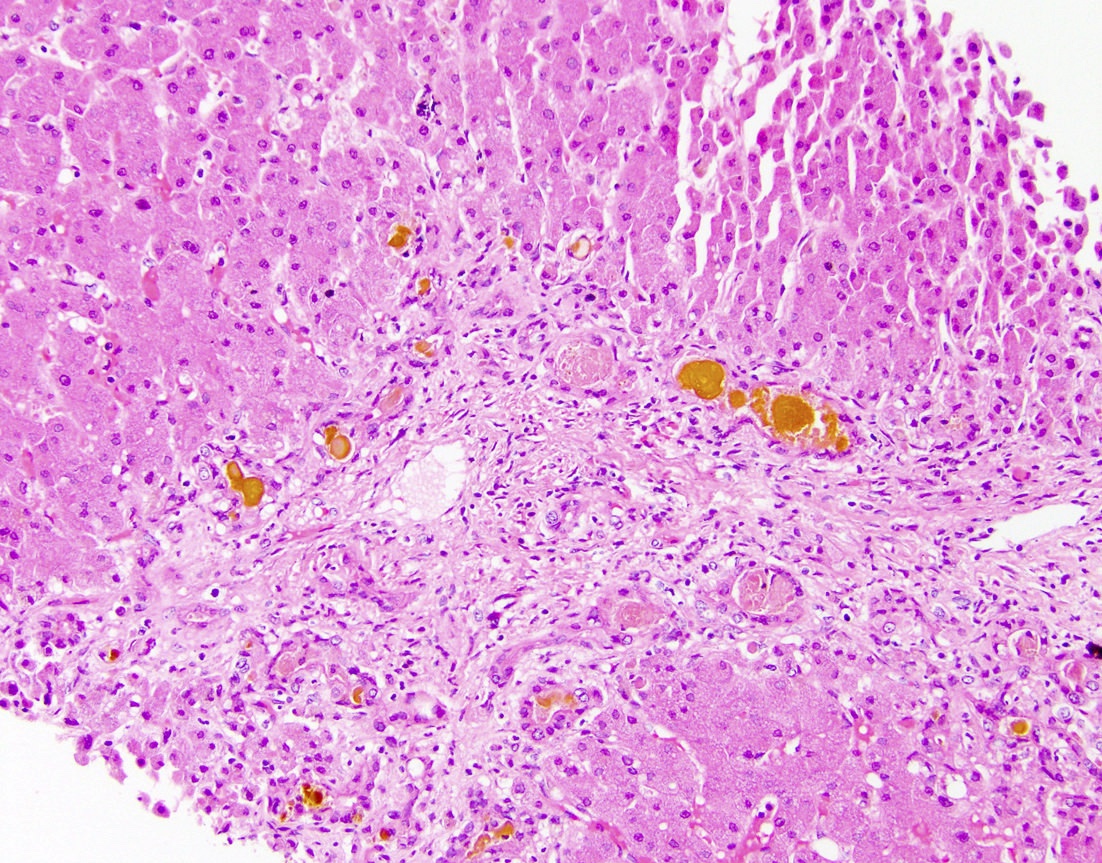
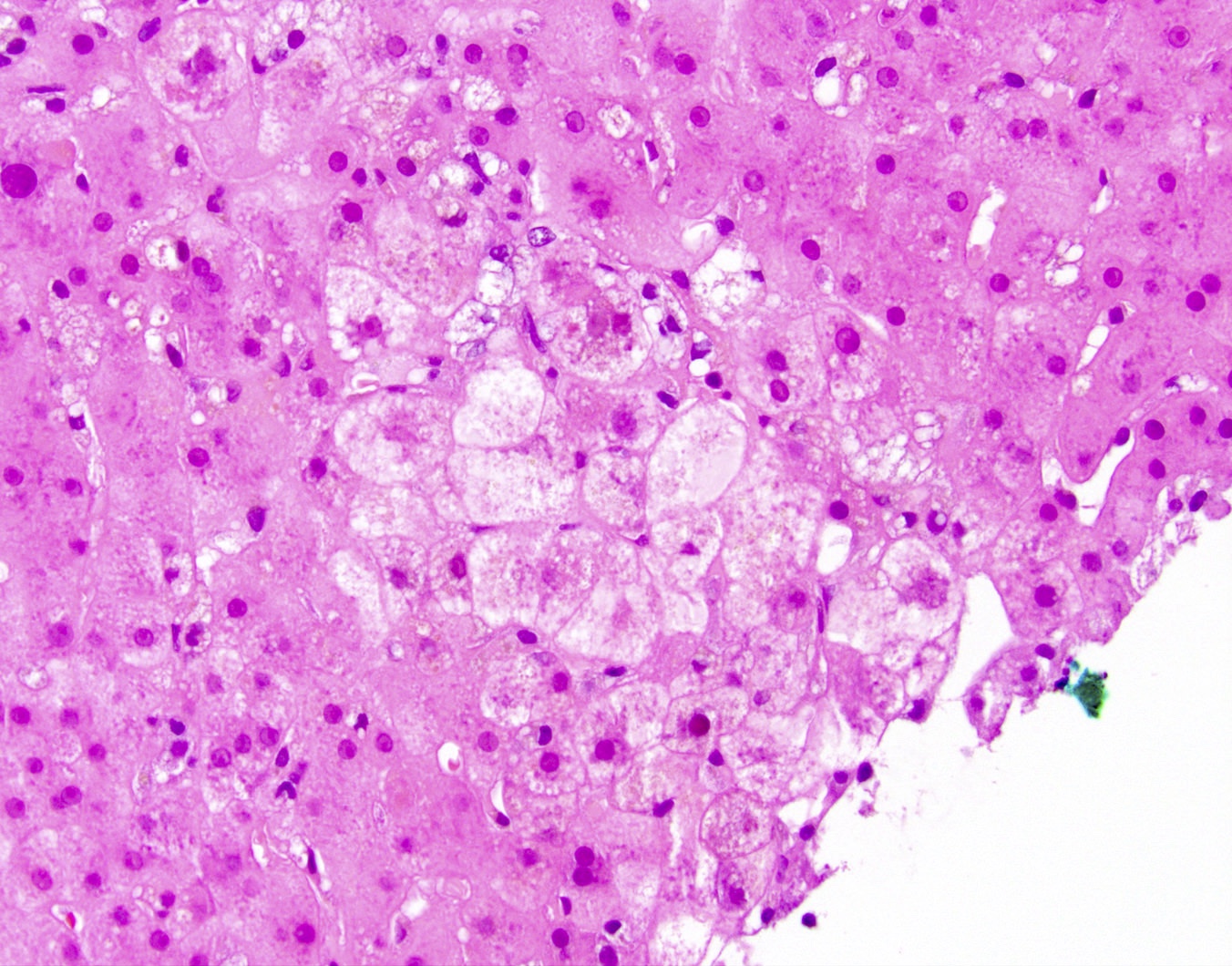
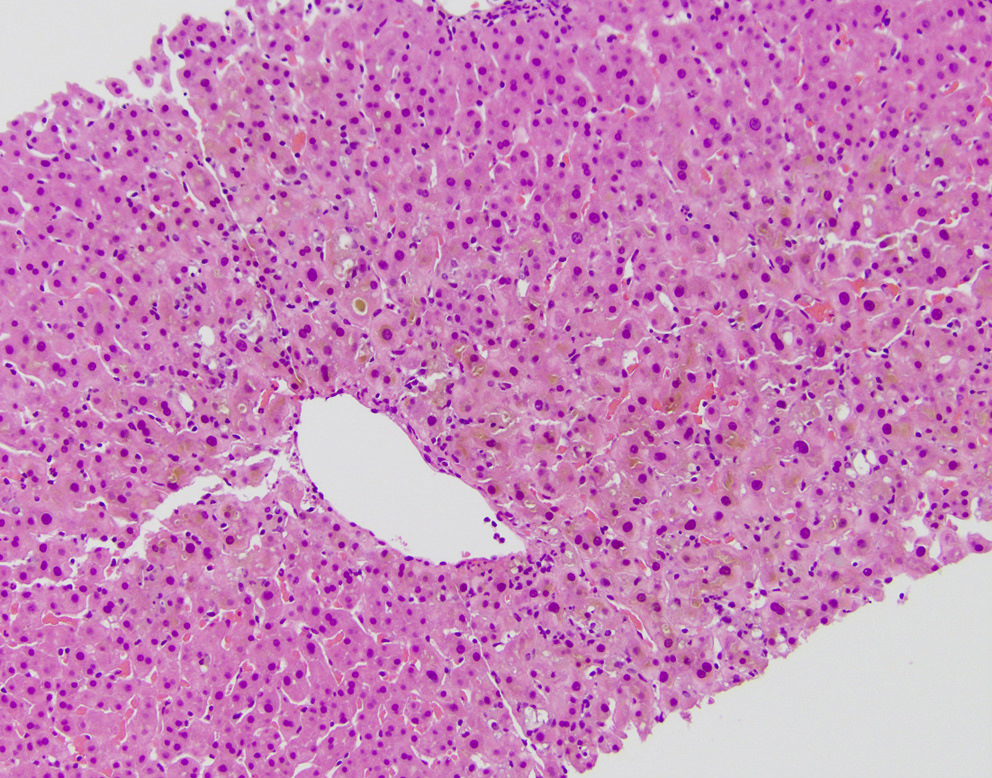
Microscopic (histologic) description
- Bile pigment (yellow / green / brown) visible histologically within hepatic parenchyma, usually perivenular
- May be present within hepatocyte cytoplasm, hepatocyte canaliculi, ductule lumens or large duct lumens
- Chronic cholestasis leads to cholate stasis / feathery degeneration of periportal hepatocytes – enlarged, swollen cells with clear / granular cytoplasm
Microscopic (histologic) images
Sample pathology report
- Liver, biopsy:
- Hepatic parenchyma with mild chronic inflammation and lobular cholestasis (see comment)
- Comment: The findings suggest cholestatic hepatitis. Possible etiologies, depending on clinical findings, include primary biliary cirrhosis, drug induced liver injury, viral hepatitis, and primary sclerosing cholangitis.
Differential diagnosis
- Other brownish pigments that can mimic bile histologically include lipofuscin (may be present in cytoplasm but not canaliculi) and hemosiderin (darker, duskier brown)
- Differential for bland cholestasis:
- Drug induced liver injury (e.g., anabolic steroids), early duct obstruction, benign recurrent intrahepatic cholestasis, acute cholestasis of pregnancy
- Differential for cholestatic hepatitis:
- Primary sclerosing cholangitis (inflammation usually minimal), primary biliary cholangitis, viral hepatitis, large duct obstruction, progressive familial intrahepatic cholestasis
- Differential for ductular cholestasis:
- Sepsis, cirrhosis (any cause), dehydration, extrahepatic biliary atresia, ductal plate malformations
Board review style question #1
Board review style answer #1
B. Anabolic steroid injury
Comment here
Reference: Liver and intrahepatic bile ducts - nontumor - Cholestasis
Comment here
Reference: Liver and intrahepatic bile ducts - nontumor - Cholestasis
Board review style question #2
Liver injury with cholestasis typically results in an increase of what laboratory value?
- Alanine aminotransferase
- Albumin
- Alkaline phosphatase
- Aspartate aminotransferase
Board review style answer #2
C. Alkaline phosphatase
Comment here
Reference: Liver and intrahepatic bile ducts - nontumor - Cholestasis
Comment here
Reference: Liver and intrahepatic bile ducts - nontumor - Cholestasis