Table of Contents
Definition / general | Essential features | CPT coding | Sites | Laboratory | Radiology description | Radiology images | Case reports | Cytology description | Cytology images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Gutierrez Amezcua JM, Brandler TC. Nonneoplastic. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/salivaryglandsmilannonneoplastic.html. Accessed May 14th, 2024.
Definition / general
- Lacking cytomorphologic evidence of a neoplastic process
- Includes inflammatory, metaplastic, infectious and reactive changes
Essential features
- The Milan System for Reporting Salivary Gland Cytopathology provides a standardized system for reporting results (Faquin: The Milan System for Reporting Salivary Gland Cytopathology, 1st Edition, 2018)
- Nonneoplastic category includes inflammatory, metaplastic, infectious and reactive changes without cytomorphologic evidence of neoplasia
- Estimated risk of malignancy (ROM) is expected to be low (~10%) (Diagn Cytopathol 2017;45:820)
- Sialadenitis (acute, chronic and granulomatous) is the most common nonneoplastic lesion (J Am Soc Cytopathol 2021;10:349)
- Usual management involves clinical follow up with radiologic correlation
CPT coding
Sites
- Major salivary glands (parotid, submandibular, sublingual), less frequent in minor salivary glands
Laboratory
- Flow cytometry for lymphoid rich samples
Radiology description
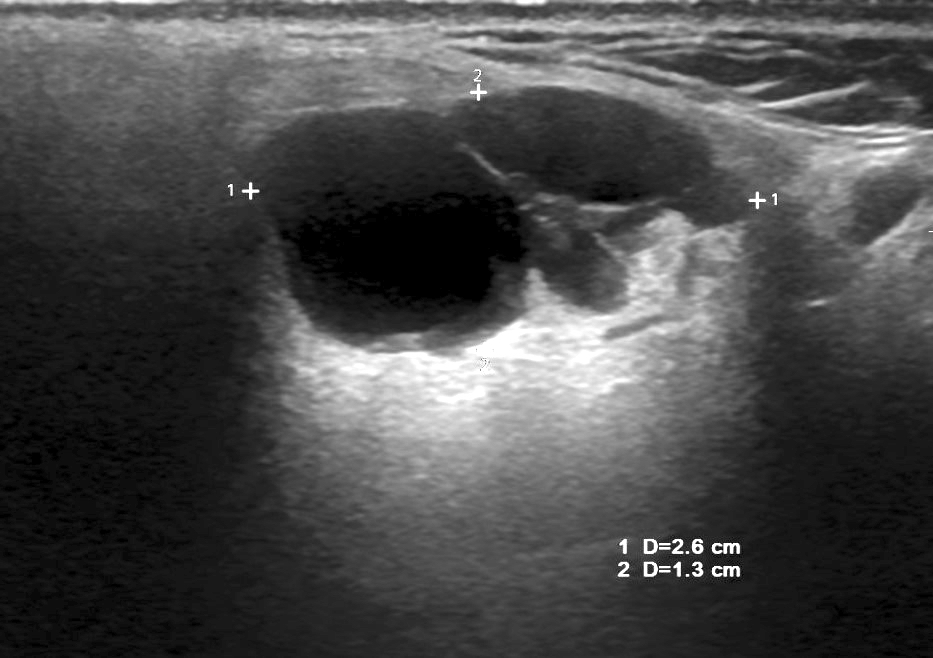
- Sialadenitis
- Enlarged, hypoechoic with heterogeneous echotexture (Br J Radiol 2003;76:271)
- Fat stranding and thickening of the superficial fascia and platysma muscles (J Clin Imaging Sci 2018;8:47)
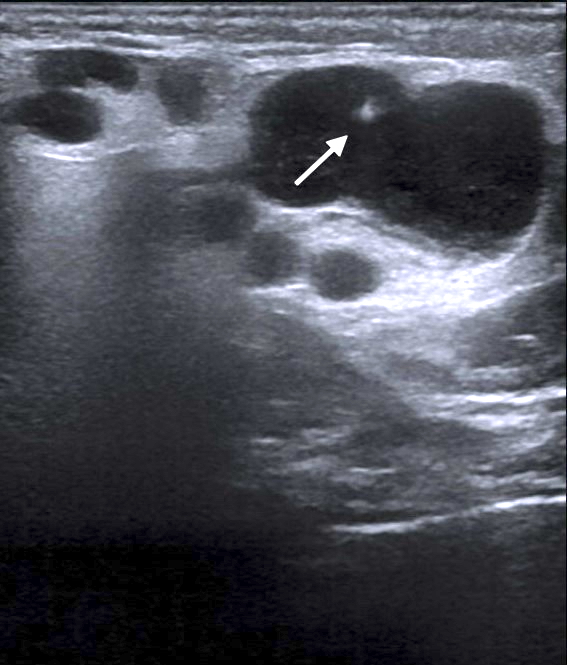
- Sialolithiasis
- Sialoliths can be detected using ultrasound (usually the initial examination imaging) or unenhanced computed tomography (Br J Radiol 2003;76:271)
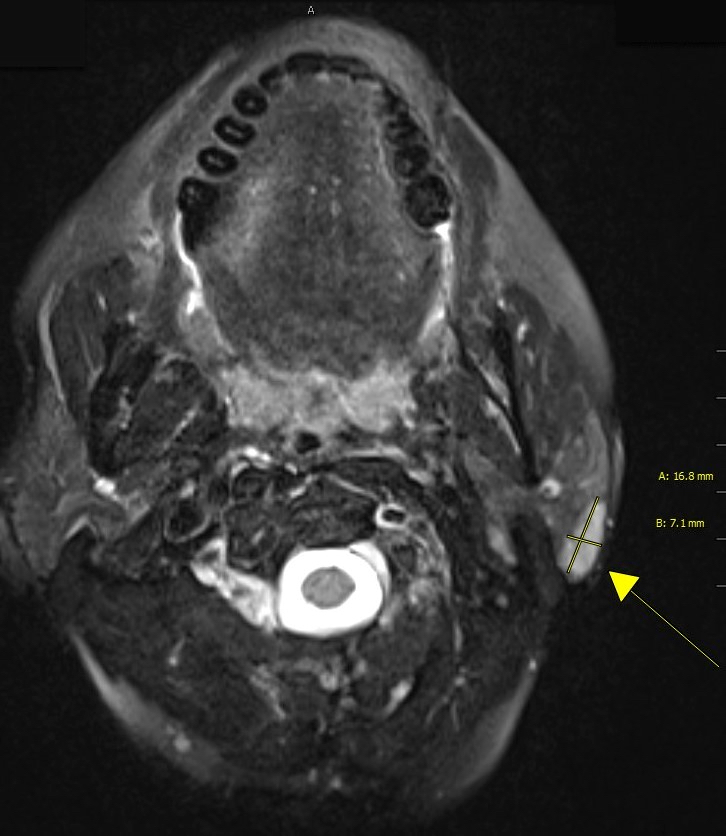
- Magnetic resonance sialography or conventional sialography can be performed in case of high suspicion for a nonradiopaque calculus (J Clin Imaging Sci 2018;8:47)
- Tumor-like lesions
- Some inflammatory conditions can produce salivary gland enlargement with homogeneous enhancement, mimicking neoplasia (e.g., chronic sclerosing sialadenitis) (J Clin Imaging Sci 2018;8:47)
- Simple cysts
- Round / oval mass with well delineated borders, anechoic center and clear posterior acoustic enhancement
- May represent benign entities (reactive lymph nodes, salivary duct cyst, lymphoepithelial cyst) but it is noteworthy that benign and malignant neoplasms may also present standard features of a simple cyst (J Ultrason 2016;16:191)
- Intracystic attenuation or signal intensity are due to viscosity or increased protein concentration of the cystic fluid content (Jpn J Radiol 2019;37:627)
- HIV associated lymphoepithelial lesion
- Numerous entirely cystic, combined cystic and solid or entirely solid lesions, which are typically bilateral (Jpn J Radiol 2019;37:627)
Radiology images
Case reports
- 51 year old woman, 59 year old man, 67 year old woman and 88 year old man with chronic sclerosing sialadenitis (Küttner tumor) misinterpreted as neoplastic in the context of previous head and neck malignancy (Head Neck Pathol 2016;10:389)
- 54 year old woman with hydatid cyst of the parotid gland (Turk Patoloji Derg 2017;33:171)
- 57 year old man with unilateral cysticercosis of the parotid gland (Case Rep Otolaryngol 2021;2021:9999441)
- 68 year old man with left submandibular sialadenitis and abundant amylase crystalloids (Indian J Otolaryngol Head Neck Surg 2014;66:348)
- 71 year old woman with multifocal adenomatous oncocytic hyperplasia of the parotid gland (Case Rep Oncol 2014;7:819)
Cytology description
- Acute sialadenitis:
- Frequency: parotid > submandibular > sublingual glands
- Acute inflammation (neutrophils) with or without bacteria and background debris
- Rarely sampled since it is usually a clinical diagnosis
- Chronic sialadenitis:
- Frequency: submandibular > parotid > sublingual glands
- Hypocellular aspirate with basaloid (atrophic) or metaplastic ductal cells and few / absent acinar cells
- Chronic inflammation (lymphocytes and plasma cells)
- Fragments of fibrotic stroma
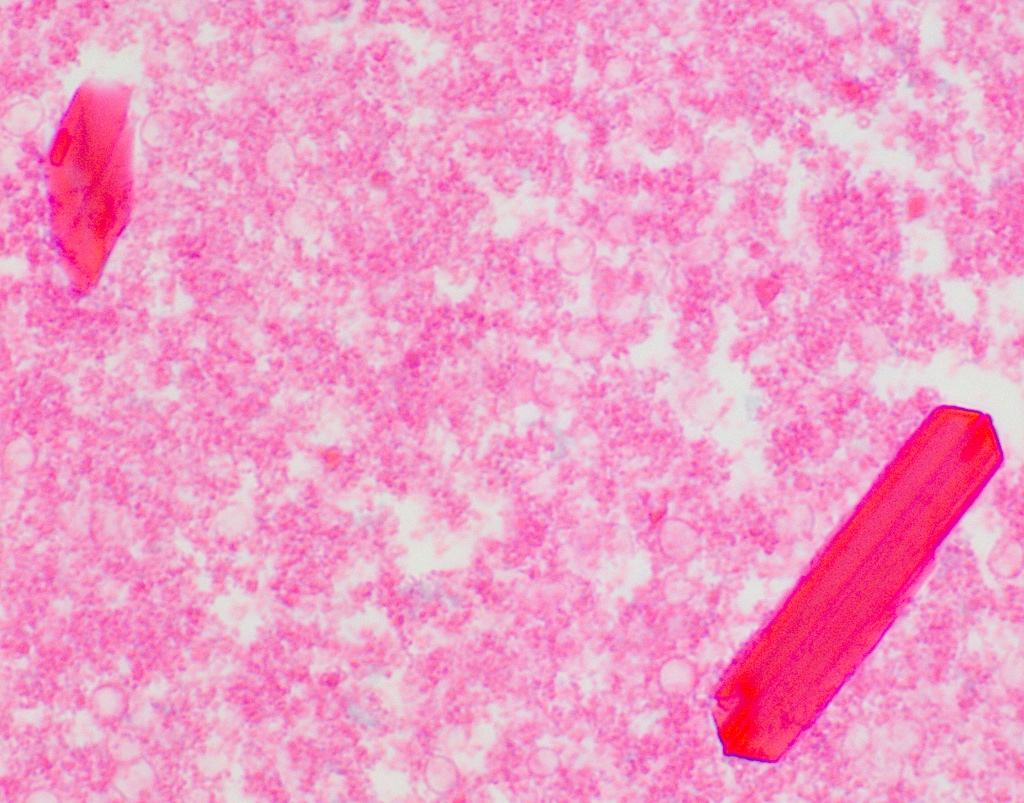
- With or without amylase crystalloids (rectangular or rhomboid nonbirefringent structures) (Cancer Cytopathol 2021;129:432)
- Chronic sclerosing sialadenitis (also known as Küttner tumor) is an IgG4 related disease that can present as firm mass simulating neoplasia
- Sialolithiasis:
- Frequency: submandibular > parotid > sublingual glands
- Hypocellular aspirate with scant acinar cells and benign ductal cells
- Ductal cells may exhibit squamous and mucinous metaplasia
- Calcifications (liths) in an (usually chronic) inflammatory background
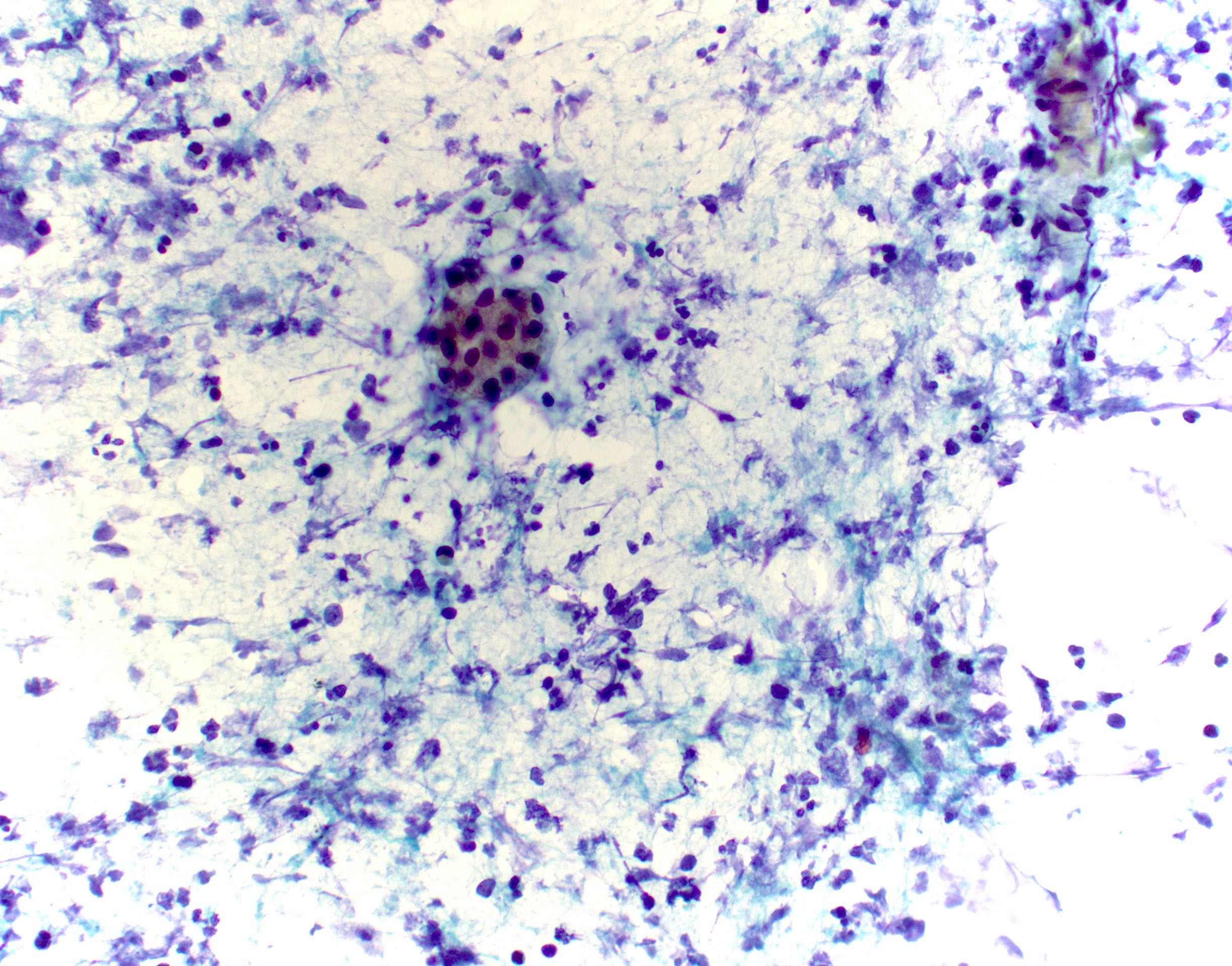
- Granulomatous sialadenitis:
- Hypocellular aspirate with groups of epithelioid histiocytes with or without multinucleated giant cells
- Variable inflammatory and necrotic debris background
- Differential diagnosis: mucin extravasation (most common), infectious (tuberculosis, actinomycosis, cat scratch, tularemia), systemic disease (e.g., sarcoidosis)
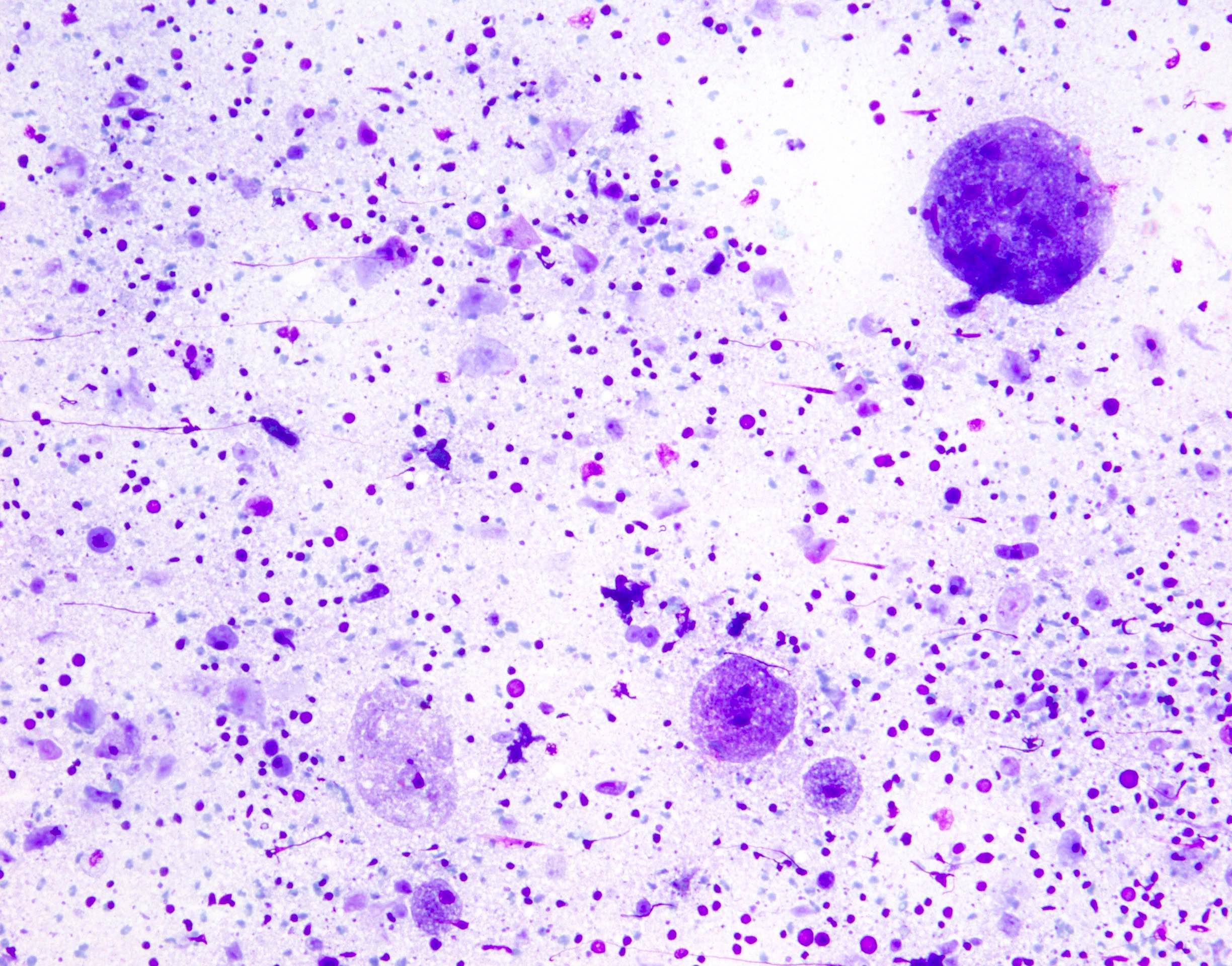
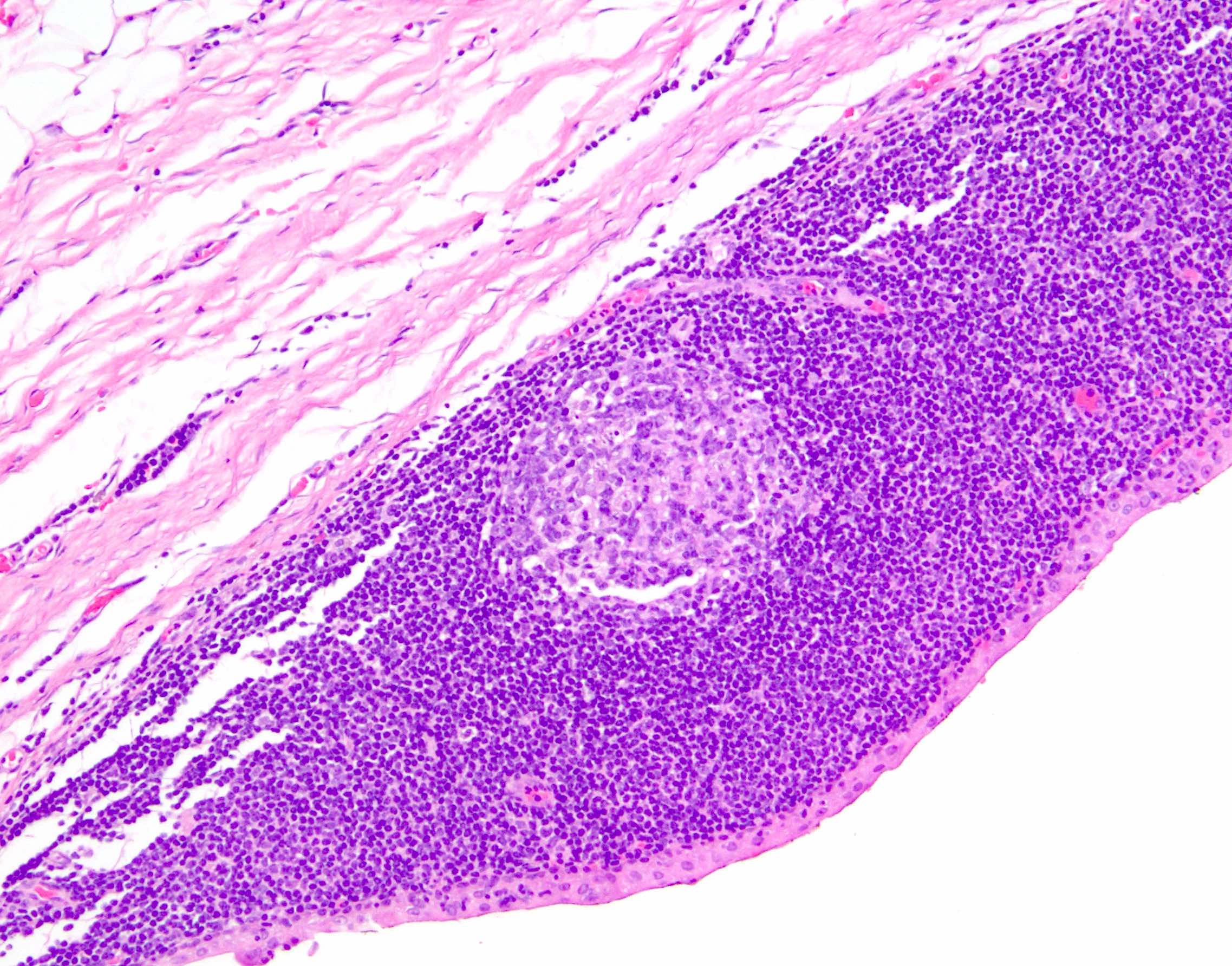
- Reactive lymph node hyperplasia:
- Almost exclusively in the parotid (intra or periparotid lymph nodes)
- Cellular aspirates with characteristics similar to a reactive lymph node:
- Mixed, heterogeneous population of mature lymphocytes and background lymphoglandular bodies
- Tingible body macrophages
- Lymphohistiocytic aggregates (fragments of germinal center)
- Collect material for flow cytometry whenever lymphoma is in the differential diagnosis
- Lymphoepithelial cyst:
- Associated with autoimmune disease (e.g., Sjögren syndrome) or young HIV+ individuals (usually multiple and bilateral) (Diagn Cytopathol 2012;40:684)
- Proteinaceous and keratin debris with squamous cells (without significant atypia), lymphocytes and lymphohistiocytic aggregates
- May see glandular (columnar / ciliated) cyst lining
- Lymphoepithelial sialadenitis (LESA):
- More common in parotid gland (~90% of cases), in women and associated with autoimmune conditions like Sjögren syndrome
- Cellular aspirate with large sheets of reactive ductal cells with or without squamous metaplasia and percolating mature lymphocytes
- Ductal cells have enlarged nuclei with distinct nucleoli but lack significant pleomorphism or atypia
- Mixed population of mature lymphocytes, dendritic cells and tingible body macrophages
- Sialadenosis or sialosis:
- Frequency: parotid (often bilaterally) > submandibular glands
- Infrequent cause of enlargement of salivary glands associated with systemic metabolic conditions (e.g., diabetes, metabolic syndrome, hypothyroidism, alcohol abuse, malnutrition, liver disease, etc.)
- Cellular aspirate with hypertrophic acinar cells without cytologic or architectural alterations
- Clinicoradiological correlation is essential for diagnosis (no discrete mass)
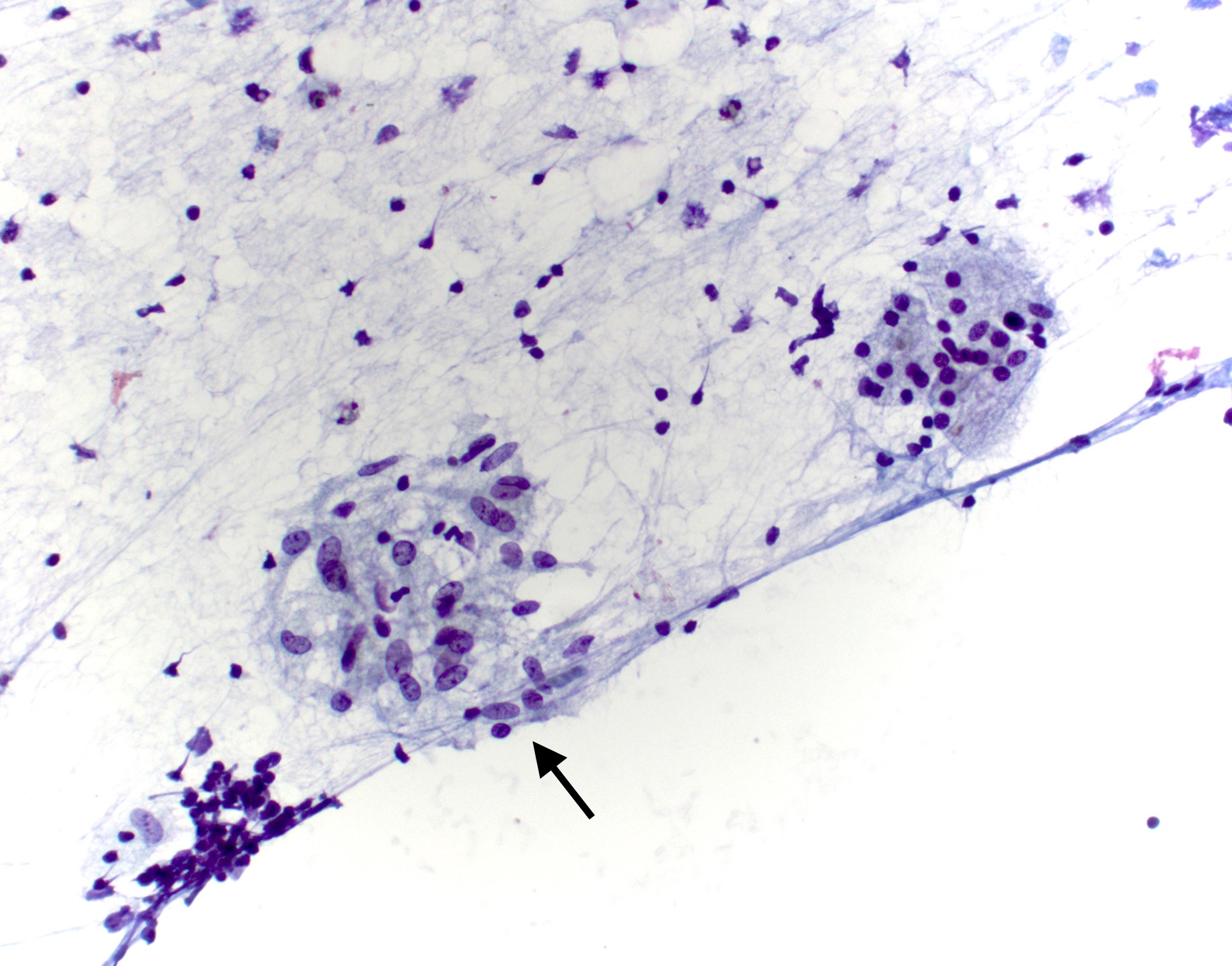
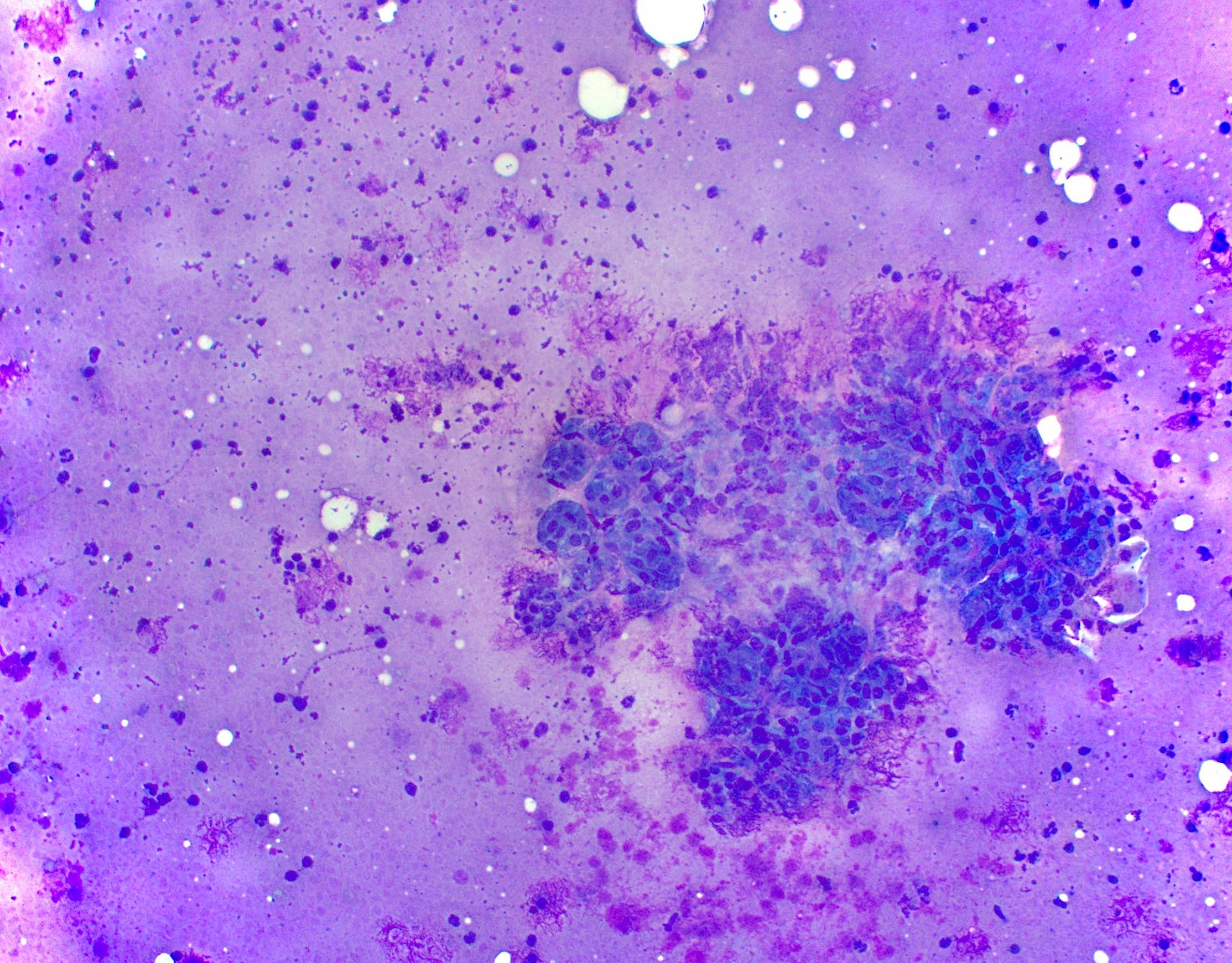
- Salivary duct cyst:
- Also known as salivary retention cyst, mucus retention cyst, sialocyst
- Frequency: minor salivary glands > parotid gland (particularly superficial lobe) (J Clin Imaging Sci 2013;3:3)
- Reactive lesion to salivary gland duct obstruction and buildup of salivary contents that results in duct ectasia
- Acellular or paucicellular aspirate of benign acinar / ductal cells, background debris containing macrophages (cyst contents), with or without inflammatory cells and amylase crystalloids
- Presence of mucin precludes classification as nonneoplastic (Diagn Cytopathol 2002;27:197)
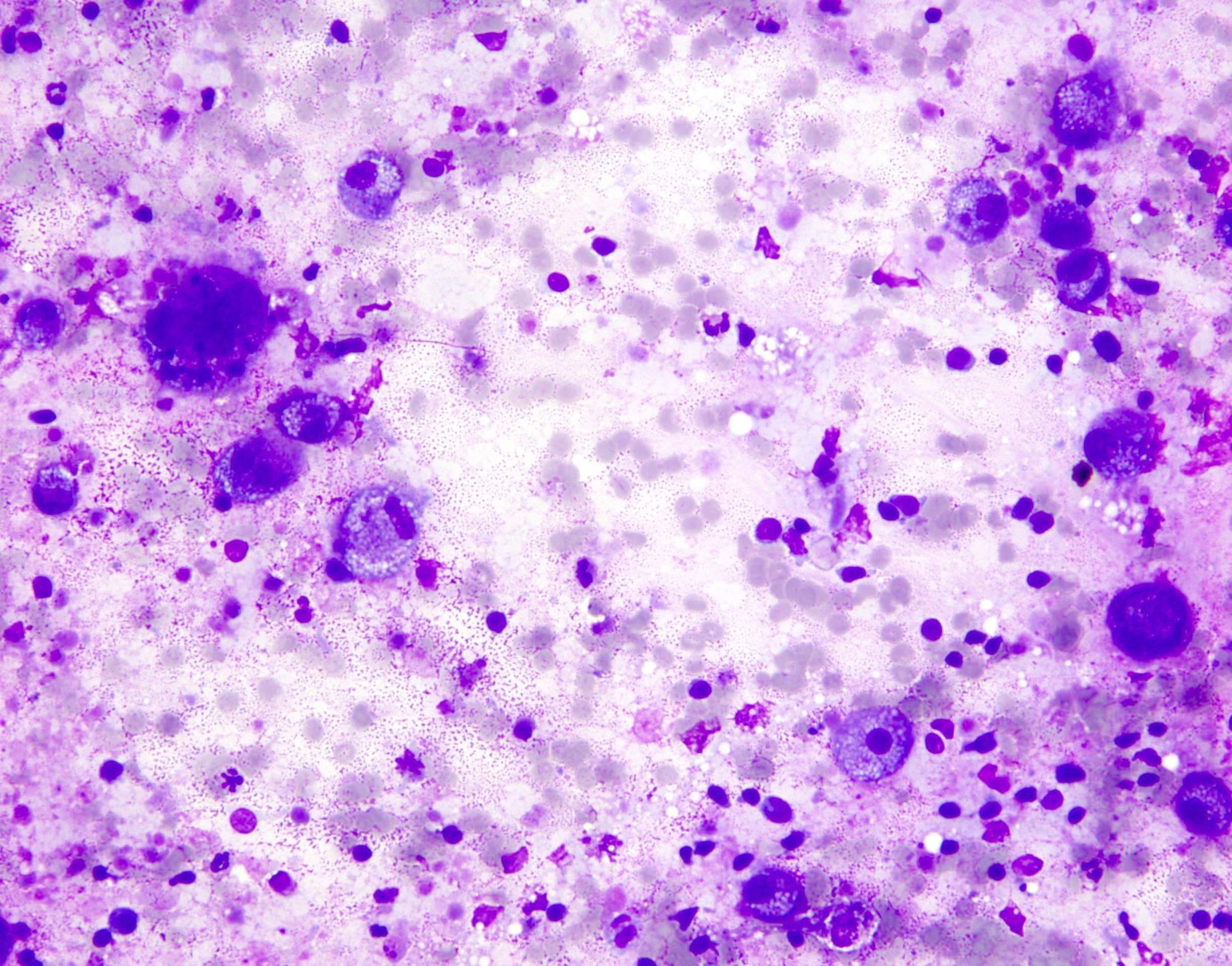
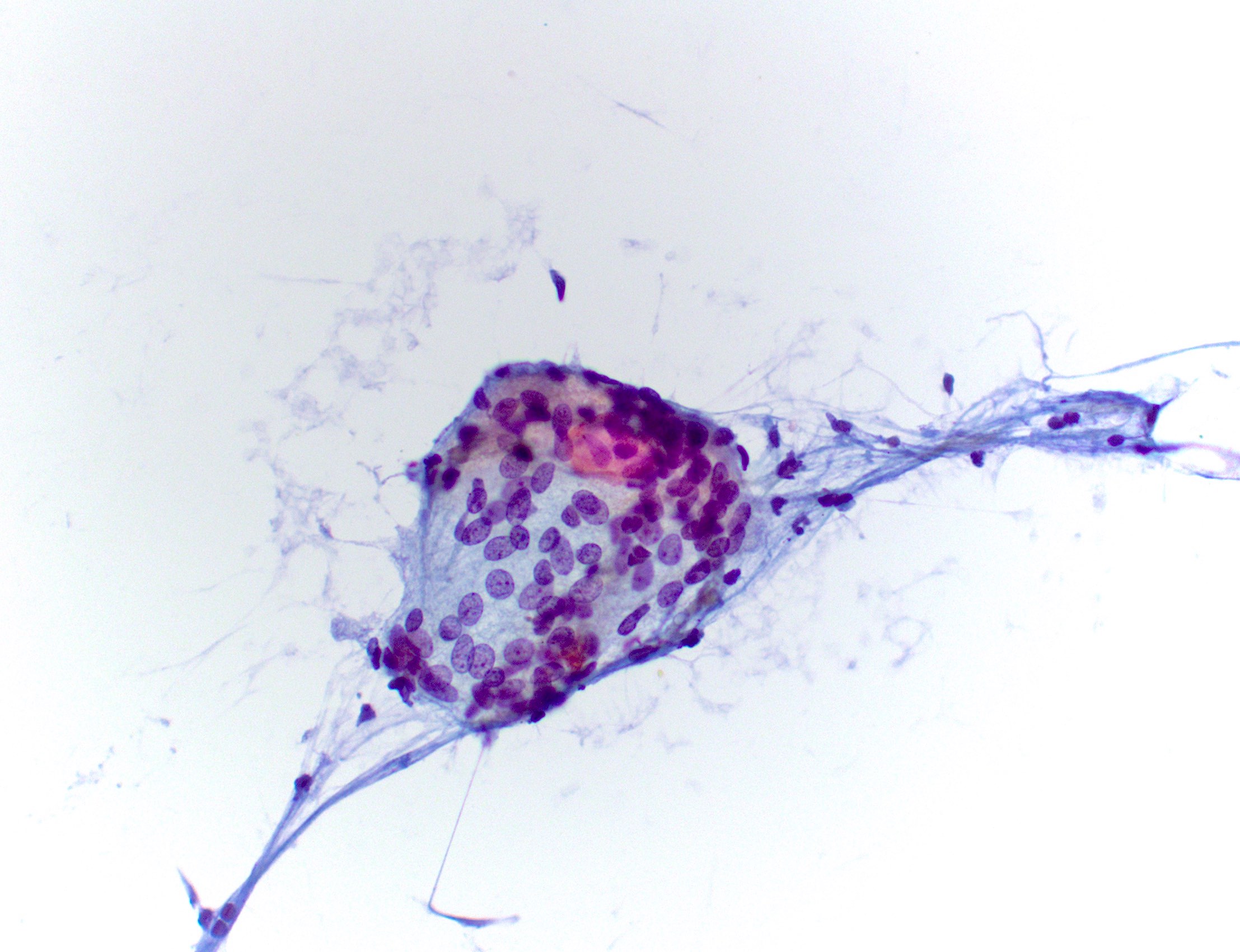
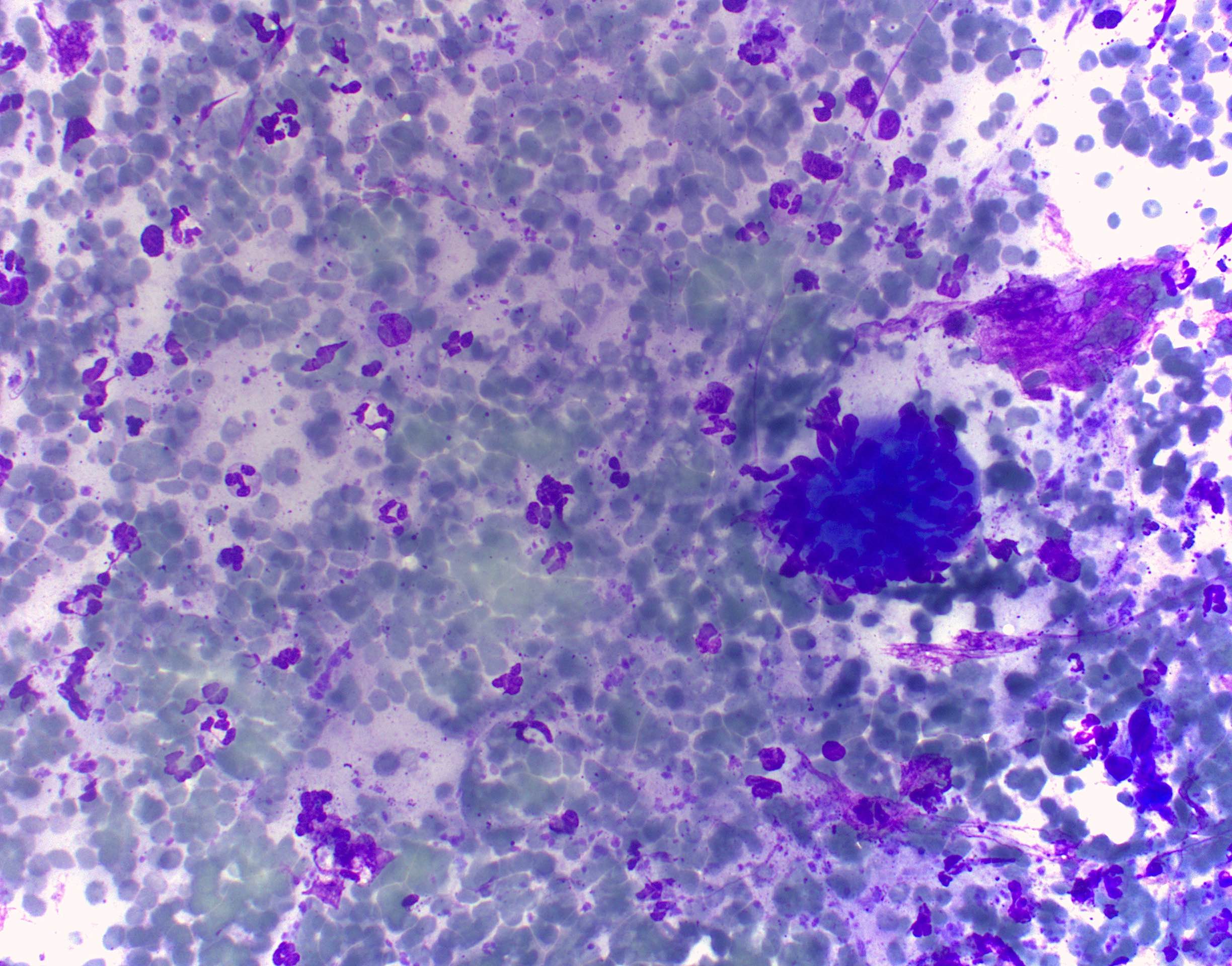
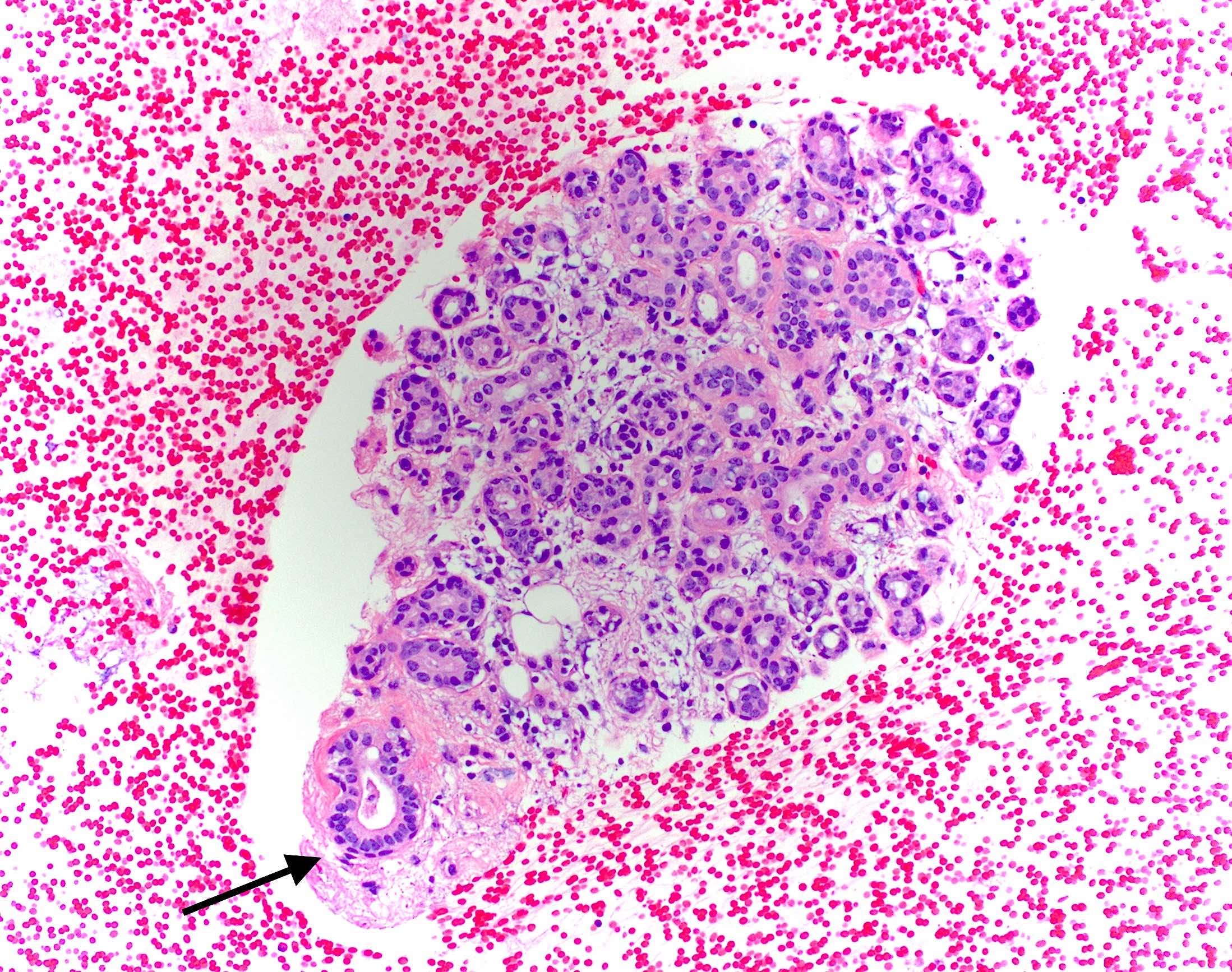
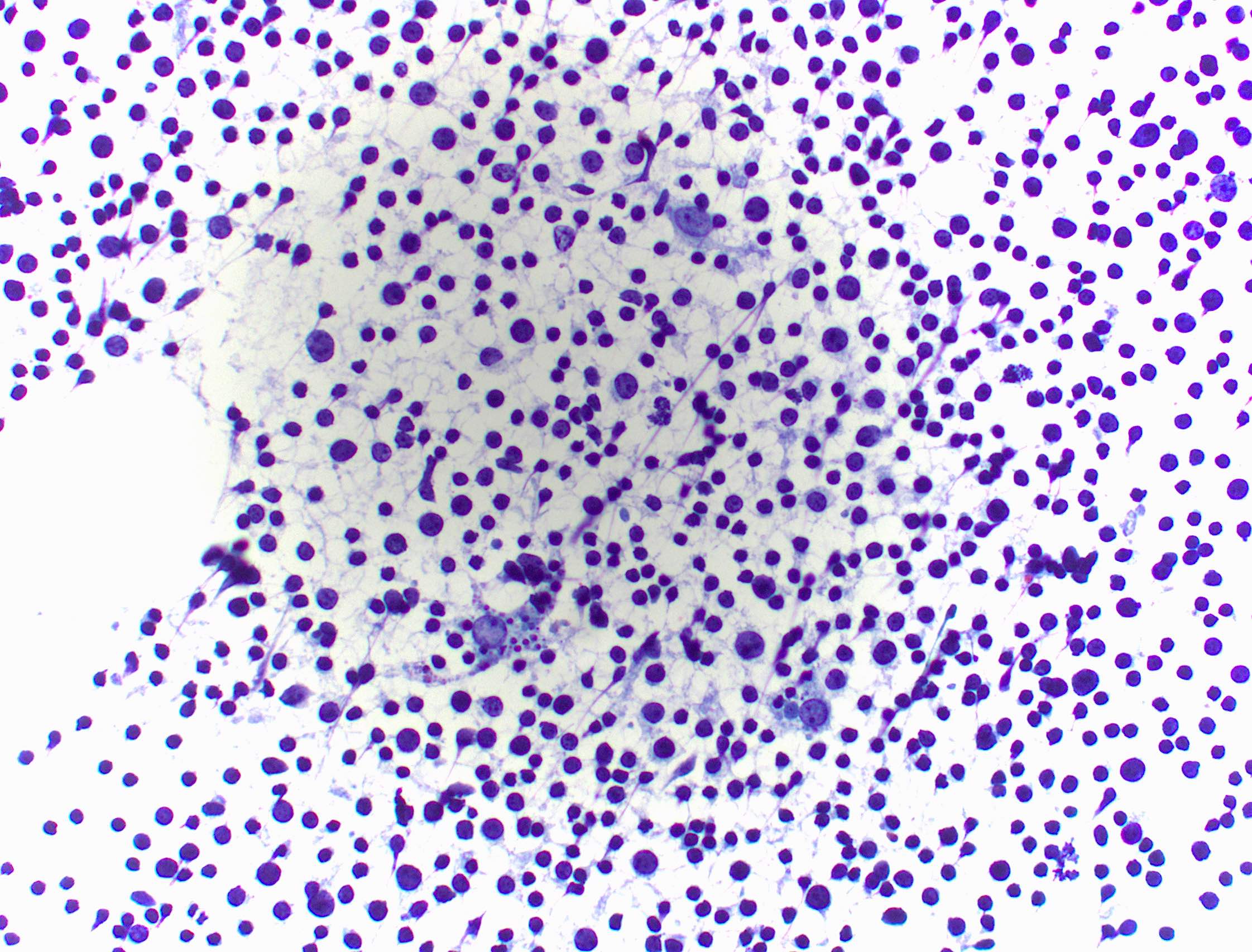
Cytology images
Contributed by Jose Manuel Gutierrez Amezcua, M.D., Pascale G. Levine, M.D. and Tamar C. Brandler, M.D., M.S.
Sample pathology report
- Nonneoplastic:
- Granulomatous sialadenitis (see comment)
- Comment: Smears show predominantly benign salivary gland acinar cells, chronic inflammation, epithelioid histiocytes forming granulomas and scattered multinucleated giant cells. These findings may be related to chronic sialadenitis, duct obstruction or sarcoidosis. Clinical and radiologic correlation is recommended.
- Nonneoplastic:
- Reactive intraparotid lymph node (see comment)
- Comment: Smears show a mixed lymphoid population with a predominance of mature lymphocytes, scattered tingible body macrophages and germinal center fragments (lymphohistiocytic aggregates). Please correlate with concurrent flow cytometry.
- Nonneoplastic:
- Consistent with salivary duct cyst (see comment)
- Comment: Smears show groups of ciliated respiratory type columnar cells, abundant amylase crystals, scattered macrophages, few groups of oncocytic metaplastic cells, benign salivary acinar cells and some background inflammation and debris. No atypia, mucin or malignancy is seen. These cytologic findings are compatible with a nonneoplastic cyst.
Differential diagnosis
- Cystic salivary gland lesions:
- Interpretation is challenging due to overall low cellularity and not well established diagnostic criteria
- ~45% will fall under the nonneoplastic category of the Milan system (Cancer Cytopathol 2021;129:214)
- Specimens containing nonmucinous cystic fluid only are best classified as nondiagnostic
- Specimens containing benign acinar or ductal epithelial components, background debris with macrophages (cyst contents) with or without inflammatory cells and amylase crystals are best classified as nonneoplastic (Cancer Cytopathol 2021;129:214)
- Specimens containing abundant mucin with or without epithelial cells are best classified as atypia of undetermined significance (AUS) due to the possibility of underlying mucoepidermoid carcinoma (Head Neck Pathol 2018;12:548)
- Lymphoma:
- Lymphomas originating from the salivary glands are rare, accounting for ~3% of all malignant tumors which more commonly affect the parotid glands (World J Clin Cases 2020;8:2717)
- Risk factors include certain viral infections (HIV, EBV), immunosuppression and autoimmunity, particularly Sjögren syndrome
- Usually presents with a unilateral asymptomatic mass that enlarges over a period of time, with or without cervical lymphadenopathy
- Whenever non-Hodgkin lymphoma is in the differential, additional passes for flow cytometry evaluation are recommended
- Reassuring features of benignity in specimens with abundant lymphoid tissue include:
- Mixed, heterogeneous population of mature lymphocytes and background lymphoglandular bodies
- Tingible body macrophages
- Lymphohistiocytic aggregates (fragments of germinal center)
Board review style question #1
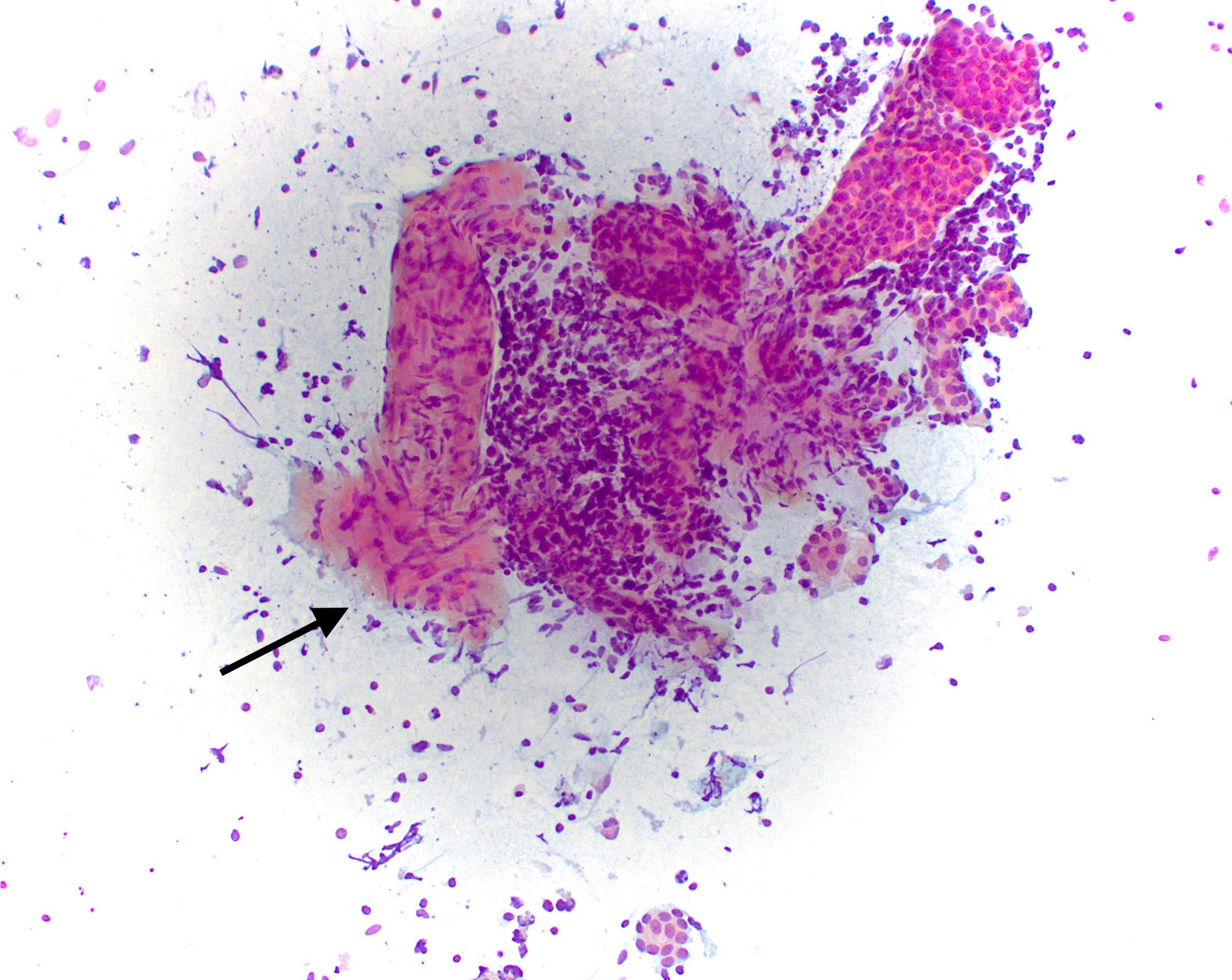
A 40 year old patient undergoes ultrasound guided fine needle aspiration (FNA) of a 2.1 cm cystic lesion in the inferior aspect of the parotid gland. The aspirate smear stained with Diff-Quik is shown above. Which of the following would be the appropriate way to characterize this lesion?
- Atypia of undetermined significance
- Nondiagnostic
- Nonneoplastic
- Salivary gland neoplasm of uncertain malignant potential
- Suspicious for malignancy
Board review style answer #1
Board review style question #2
Which of the following findings on fine needle aspiration (FNA) would preclude classification of a salivary gland lesion as nonneoplastic?
- Abundant mucin with or without epithelial cells
- Granulomas and scattered multinucleated giant cells
- Heterogeneous lymphocytes with tingible body macrophages
- Metaplastic ductal cells with calcification and chronic inflammation
- Nonmucinous background debris with macrophages
Board review style answer #2