Table of Contents
Definition / general | Essential features | Terminology | Pathophysiology | Clinical features | Interpretation | Uses by pathologists | Prognostic factors | Microscopic (histologic) images | Positive staining - normal | Positive staining - disease | Negative staining | Molecular / cytogenetics description | Sample pathology report | Board review style question #1 | Board review style answer #1Cite this page: Abdelmalak M, Pendse A. Alpha-1 antitrypsin. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/stainsa1a.html. Accessed April 29th, 2024.
Definition / general
- Acute phase plasma protein
- Inhibits neutrophil elastase, which causes tissue damage and maintains protease / antiprotease balance in the lung (J Proteome Res 2014;13:3131)
- Most abundant circulating serine protease inhibitor predominantly derived from hepatocytes (J Proteome Res 2014;13:3131)
- Member of serpin superfamily; homologous to alpha-1 antichymotrypsin (Biochem Soc Trans 2002;30:93)
Essential features
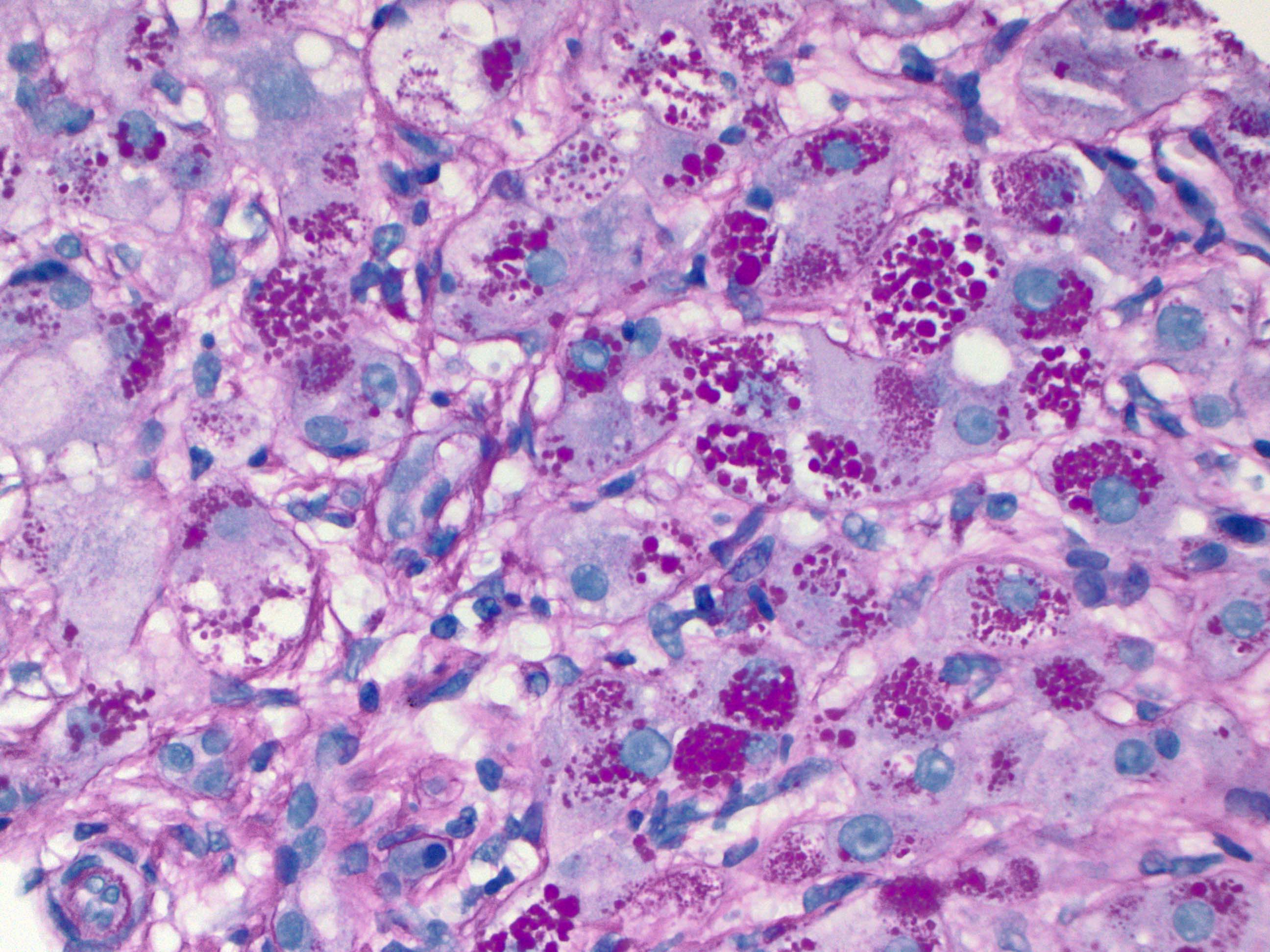
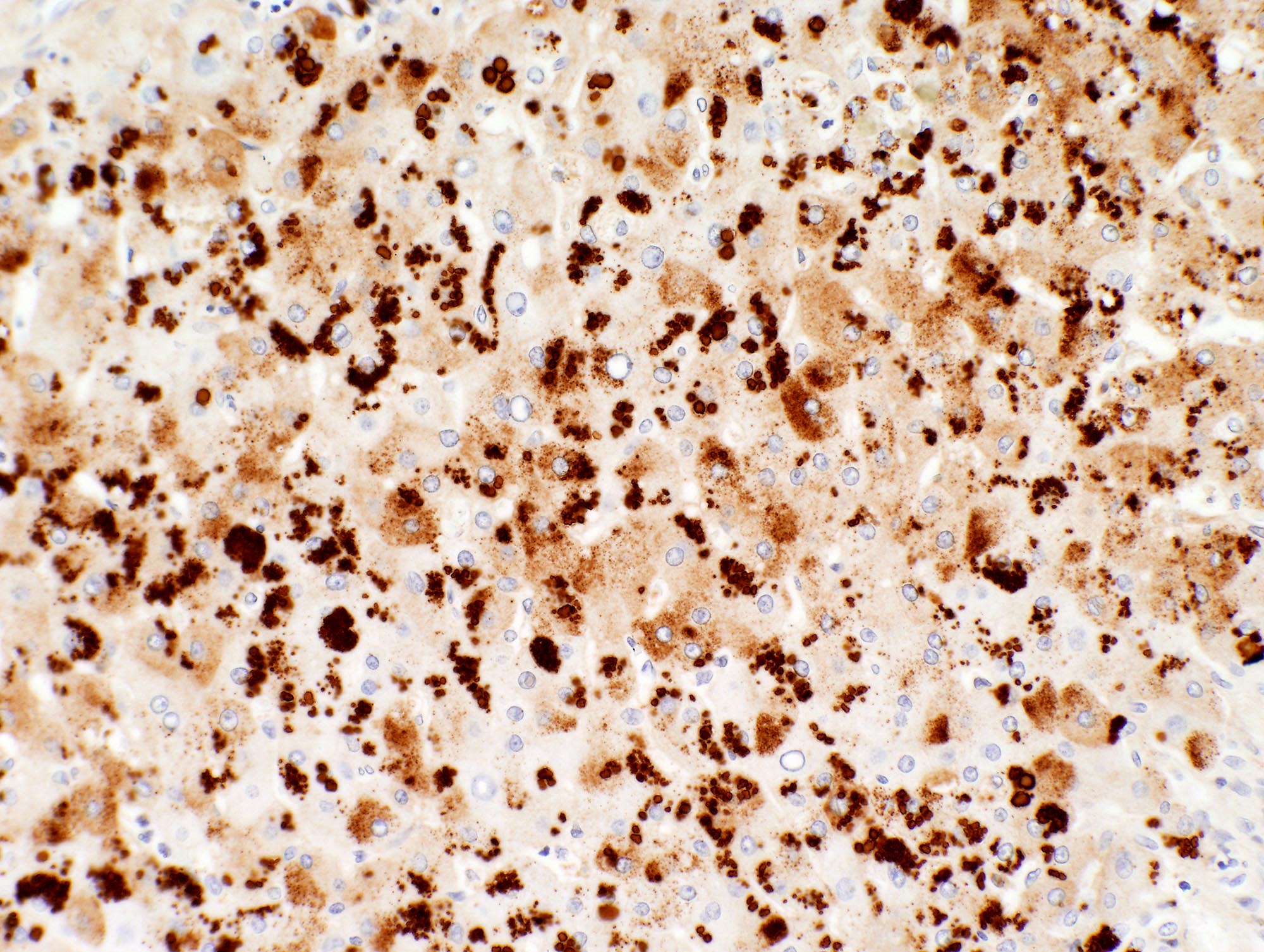
- Intracytoplasmic globules in hepatocytes, preferentially in zone 1 near the portal tracts; can be patchy
- Alpha-1 antitrypsin positive globules will also be highlighted by periodic acid-Schiff diastase (PASD) stain
- Presence of alpha-1 antitrypsin globules does not differentiate between homozygous versus heterozygous deficiency states (J Hepatol 2000;32:406)
- Expressed in a variety of tumors and pathologic processes, though not commonly used for diagnostic purposes in such entities
Terminology
- Sometimes abbreviated AAT or A1AT
Pathophysiology
- See Alpha-1 antitrypsin deficiency in Liver & intrahepatic ducts chapter
Clinical features
- See Alpha-1 antitrypsin deficiency in Liver & intrahepatic ducts chapter
- AAT deficiency is highly underdiagnosed
- Due to overlap of clinical symptoms, testing should be performed in individuals with chronic obstructive pulmonary disease (COPD), liver disease, poorly responsive asthma, cANCA vasculitis, panniculitis or bronchiectasis, in addition to first degree relatives of people with AAT deficiency (N Engl J Med 2020;382:1443)
Interpretation
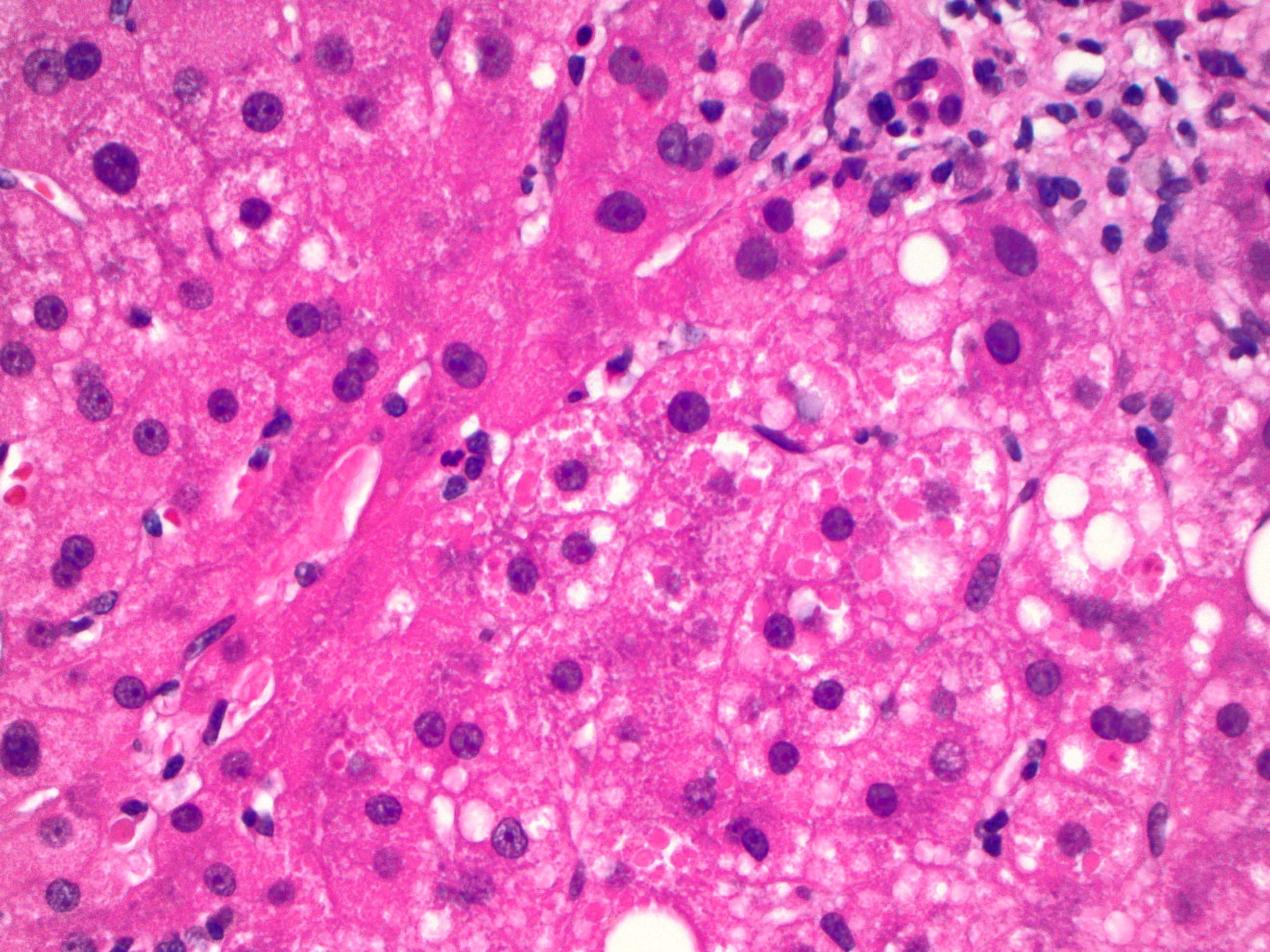
- Intracytoplasmic globules in hepatocytes (Clin Liver Dis 2018;22:643)
- May be difficult to visualize in neonates, who may show finely granular cytoplasmic staining (Clin Liver Dis 2018;22:643)
Uses by pathologists
- To diagnose alpha-1 antitrypsin deficiency in the appropriate clinical context
- Initial laboratory test is serum AAT, which is decreased in AAT deficiency (< 1.1 g/L)
- Correlation with enzyme phenotype (e.g., PiMZ or PiZZ) is recommended to confirm the diagnosis and determine heterozygous versus homozygous deficiency state
- Note: there is no direct correlation between the serum AAT value, the Pi phenotype and the presence or absence of immunoreactive periportal AAT granules; thus, IHC alone cannot confirm or exclude AAT deficiency (J Clin Pathol 1986;39:58)
- Can be used to study AAT protein expression within the human liver or exogenous AAT that is delivered through gene therapy (Methods Mol Biol 2017;1639:139)
Prognostic factors
- See Alpha-1 antitrypsin deficiency in Liver & intrahepatic ducts chapter
Microscopic (histologic) images
Positive staining - normal
- In addition to hepatocytes, A1AT is secreted from monocytes and macrophages, small intestinal enterocytes and bronchial epithelial cells (Clin Immunol Immunopathol 1980;16:84, J Clin Invest 1993;92:2022, J Clin Invest 1986;77:1952, J Biol Chem 1997;272:8250)
Positive staining - disease
- A1AT globules seen in the livers of patients with alpha-1 antitrypsin deficiency (Clin Gastroenterol Hepatol 2012;10:575)
- Pitfall: globules can sometimes also be seen in cirrhotic livers of any etiology
- Various tumor types have been shown to have positive AAT staining; however, such immunohistochemistry is currently not used for diagnosis of specific tumor types
Negative staining
- Similar appearing globules that are negative for AAT IHC are present in other diseases, such as alpha-1 antichymotrypsin deficiency, antithrombin III deficiency and fibrinogen storage disorders (Gonzalez: Non-Neoplastic Liver Pathology - A Pathologist's Survival Guide, 1st Edition, 2016)
Molecular / cytogenetics description
- See Alpha-1 antitrypsin deficiency in Liver & intrahepatic ducts chapter
- SERPINA1 gene
- Allele: Glu342Lys is most common SERPINA1 point mutation (J Hepatol 2016;65:413)
Sample pathology report
- Liver, random, ultrasound guided needle core biopsy:
- Alpha-1 antitrypsin deficiency (see comment)
- Comment: Scattered hepatocytes with PAS diastase positive intracytoplasmic globules, highlighted by immunohistochemistry for alpha-1 antitrypsin, suggestive of alpha-1 antitrypsin deficiency. Correlation with laboratory testing for serum levels and alpha-1 antitrypsin phenotype is recommended.
Board review style question #1
A 38 year old man with clinical concern for early onset liver fibrosis has longstanding mild to moderate elevation in transaminases. Viral hepatitis serology is negative and there is no recent history of medication changes or herbal supplement use. A liver biopsy was performed and showed mild portal inflammation with no significant interface activity. A trichrome stain showed bridging fibrosis. Many hepatocytes showed periodic acid-Schiff diastase (PASD) positive cytoplasmic globules. What is the likely etiology of the patient's liver disease and the confirmatory immunohistochemistry that would aid with diagnosis?
- Alcohol; glutamine synthetase
- Alpha-1 antitrypsin deficiency; alpha-1 antitrypsin
- Autoimmune hepatitis; CD138
- Steatohepatitis; heat shock protein
- Viral hepatitis; hepatitis B surface antigen
Board review style answer #1
B. Alpha-1 antitrypsin deficiency; alpha-1 antitrypsin. Answers A, C, D and E are incorrect because although liver fibrosis has a variety of etiologies, intracytoplasmic globules that express alpha-1 antitrypsin in hepatocytes are compatible with alpha-1 antitrypsin deficiency.
Comment Here
Reference: Alpha-1 antitrypsin
Comment Here
Reference: Alpha-1 antitrypsin