Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Electron microscopy description | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Mullins CI, Pendse A. Alpha-1 antitrypsin deficiency. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/liveraat.html. Accessed September 12th, 2025.
Definition / general
- Genetic metabolic disorder causing deficiency of alpha-1 antitrypsin deficiency (AAT) and leading to disease in the lungs and liver
Essential features
- Different phenotypes have different clinical presentations
- Should be included in the differential diagnosis for all cases of early onset cirrhosis
- PASD and AAT positive eosinophilic intracytoplasmic globules within hepatocytes
- Absence does not rule out AAT deficiency
ICD coding
- ICD-10: E88.01 - Alpha-1 antitrypsin deficiency
Epidemiology
- Age at diagnosis: 20 - 50 (Methods Mol Biol 2017;1639:9)
- Smoking: younger age at presentation
- Infants (small subset of patients)
- Caucasian / Northern European descent (Methods Mol Biol 2017;1639:9)
- M = F (Methods Mol Biol 2017;1639:9)
- Genetic mutation: codominant inheritance (see Etiology)
Sites
- Liver
- Lungs
Pathophysiology
- AAT is a serine proteinase inhibitor
- From the serpin superfamily
- Secreted by hepatocytes (primary source) and also epithelial cells in the lung and GI tract, neutrophils and macrophages (Trends Mol Med 2014;20:116)
- AAT structure = beta pleated sheets and alpha helices (Methods Mol Biol 2017;1639:9, Mutat Res 2017 Jul;773:14)
- Normal process (Methods Mol Biol 2017;1639:9):
- Folding and glycosylation occur in the endoplasmic reticulum, which allows for export from the cell
- Reactive loop of AAT is cleaved by proteinase binding
- Cleaved reactive loop binds to the beta sheet
- Mutated process (Methods Mol Biol 2017;1639:9, Mutat Res 2017 Jul;773:14, Trends Mol Med 2014;20:116):
- Mutation causes a change in the tertiary structure
- Noncleaved reactive loops from AAT can bind to other beta sheets, resulting in molecular linkage
- Process is called loop sheet polymerization
- Misformed AAT cannot be exported from the cell
- Leads to AAT accumulation and endoplasmic reticulum stress response
Etiology
- AAT encoded by SERPINA1 gene located on chromosome 14 (Methods Mol Biol 2017;1639:9, Trends Mol Med 2014;20:116)
- Multiple genetic variants:
- "M" = wild type allele
- "Z" and "S" = most common mutant alleles (Methods Mol Biol 2017;1639:9)
- "Z" mutant allele accounts for 90% of disease (Methods Mol Biol 2017;1639:9)
- Numerous other rare alleles (J Biol Chem 1995;270:16864)
- Mmalton, etc.
- 4 phenotypes (Methods Mol Biol 2017;1639:9, Orphanet J Rare Dis 2008;3:16):
- Normal = normal function and plasma levels of AAT
- "M" phenotype (PiMM)
- Present in > 99% of world population
- Deficient = abnormal function and low plasma levels of AAT
- Mutant phenotype with "Z" or "S" alleles (PiSZ, PIZZ, etc.)
- Present in < 1% of world population
- Null = no detectable AAT in plasma
- Proteins are truncated or unstable; leads to degradation
- Very rarely causes liver disease and no hepatocyte inclusions will be present
- Does cause lung disease
- Present in < 0.1% of world population
- Dysfunctional = normal plasma levels of AAT
- AAT does not function correctly
- Present in < 0.1% of world population
- Normal = normal function and plasma levels of AAT
Clinical features
- Liver complications are variable (Clin Liver Dis 2018;22:643)
- May be asymptomatic until adulthood (Clin Liver Dis 2017;21:355)
- Adults: cirrhosis, chronic hepatitis, portal hypertension, jaundice, hepatocellular carcinoma, liver failure (rare) (Clin Liver Dis 2018;22:643, Aliment Pharmacol Ther 2018;47:877)
- Neonates: neonatal hepatitis syndrome, cholestasis (Clin Liver Dis 2018;22:643)
- Children: chronic hepatitis, portal hypertension (isolated), hepatomegaly, splenomegaly, jaundice (Clin Liver Dis 2018;22:643, Aliment Pharmacol Ther 2018;47:877)
Diagnosis
- Low serum concentration of AAT (Methods Mol Biol 2017;1639:9, Mutat Res 2017 Jul;773:14)
- < 50% of the normal reference range = no further tests needed (Mutat Res 2017 Jul;773:14)
- Caution: AAT is an acute phase reactant and so may show small elevations with systemic inflammatory states
- Absence of alpha-1 band on serum protein electrophoresis (Methods Mol Biol 2017;1639:9)
- Genotype analysis (Mutat Res 2017 Jul;773:14, Clin Liver Dis 2018;22:643)
- Phenotype of AAT protein (Clin Liver Dis 2018;22:643)
- Either genotype or phenotype analysis can be used as gold standard
Laboratory
- Elevated: bilirubin (conjugated or unconjugated), ALT, AST (Clin Liver Dis 2018;22:643)
- Decreased: albumin, vitamin K (Clin Liver Dis 2018;22:643)
- Advanced disease: decreased platelet count and synthetic function of liver
- See also Diagnosis
Prognostic factors
- Depends on the genetic phenotype (see also Etiology)
Case reports
- Infant girl with jaundice (Pediatr Dev Pathol 2017;20:176)
- 33 and 63 year old men with tuberculosis and AAT deficiency (Int J Mycobacteriol 2017;6:187)
- 39 year old man with ongoing respiratory and abdominal symptoms (Cureus 2018;10:e3494)
- 60 year old man with liver failure following partial hepatectomy (World J Gastroenterol 2016;22:3289)
Treatment
- Liver transplant is the only curative option (Clin Liver Dis 2017;21:355)
- AAT replacement (Mutat Res 2017 Jul;773:14)
- IV purified pooled human AAT
- Inhaled in aerosolized form
Gross description
- Most common specimen: explanted native liver at the time of transplant
- Hepatomegaly (Aliment Pharmacol Ther 2018;47:877)
- Nodular and fibrotic (Aliment Pharmacol Ther 2018;47:877)
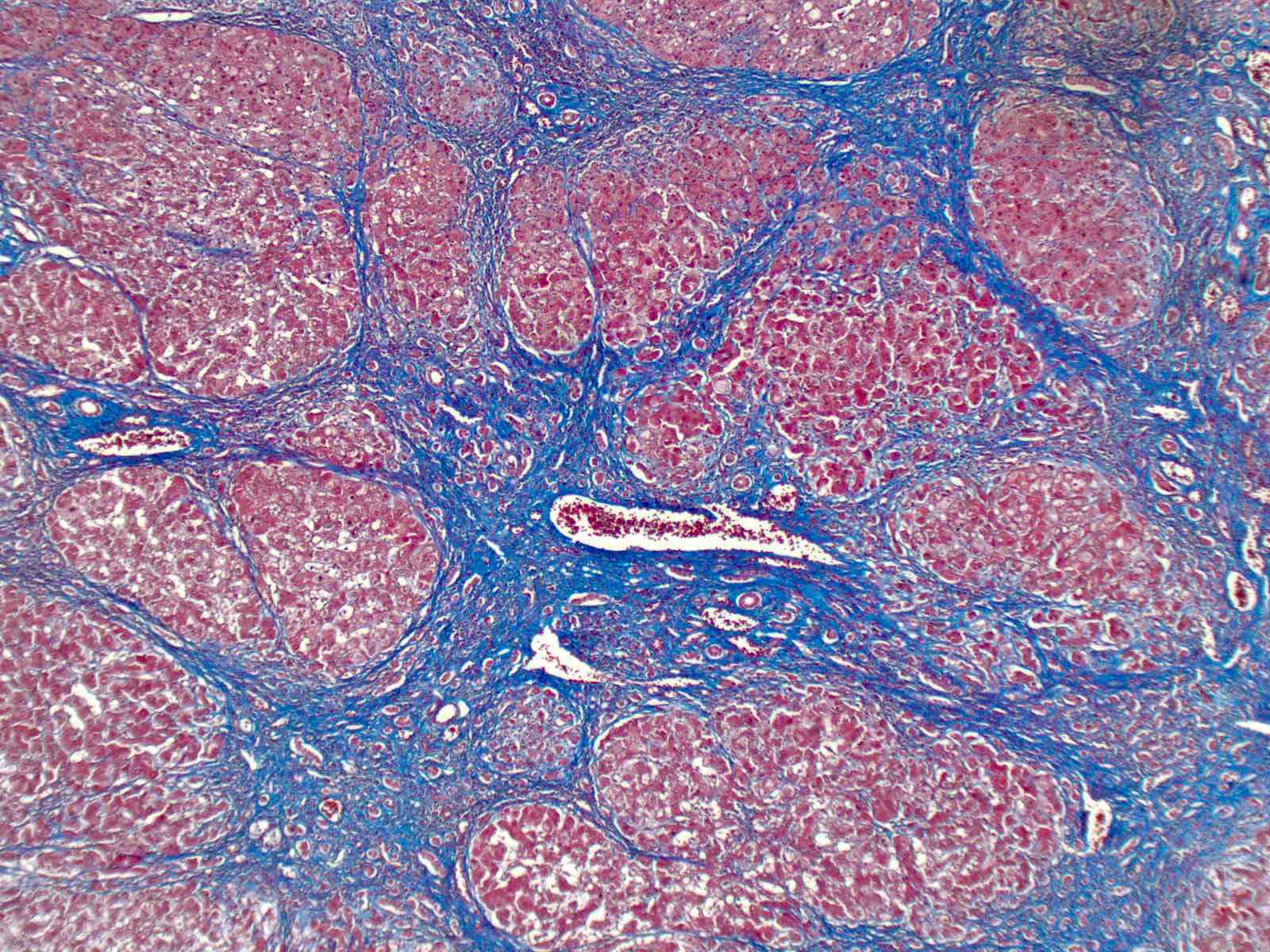
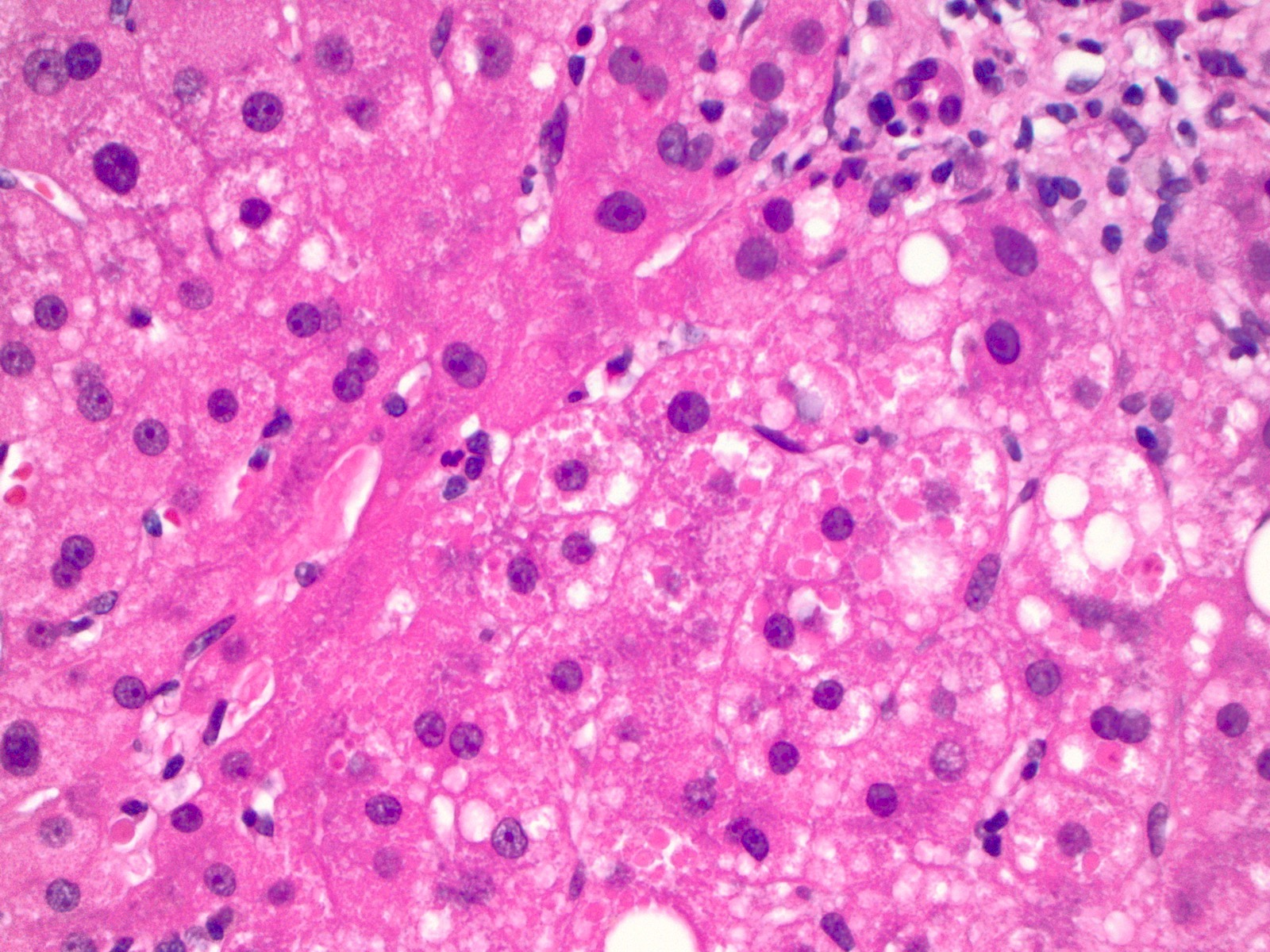
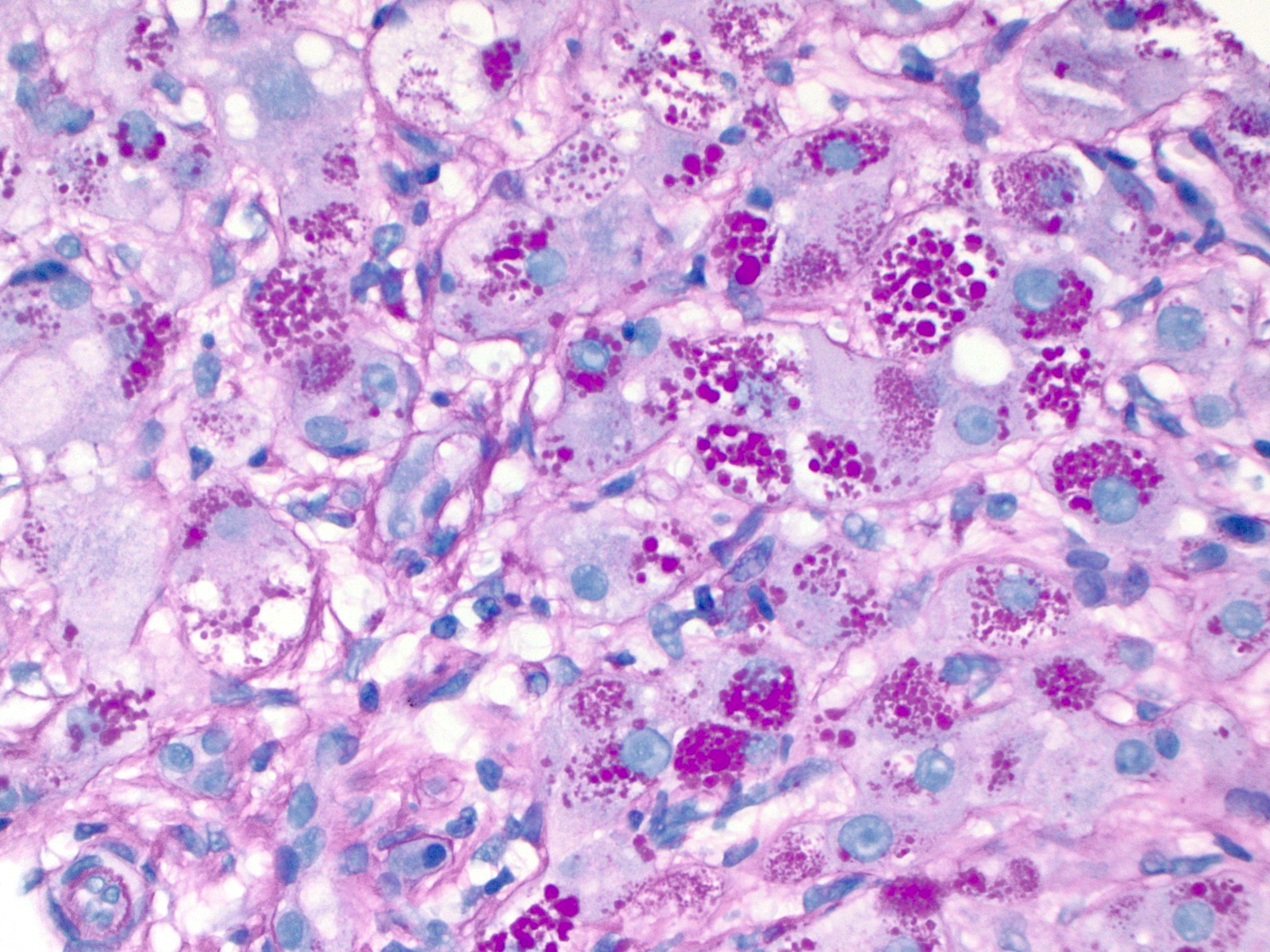
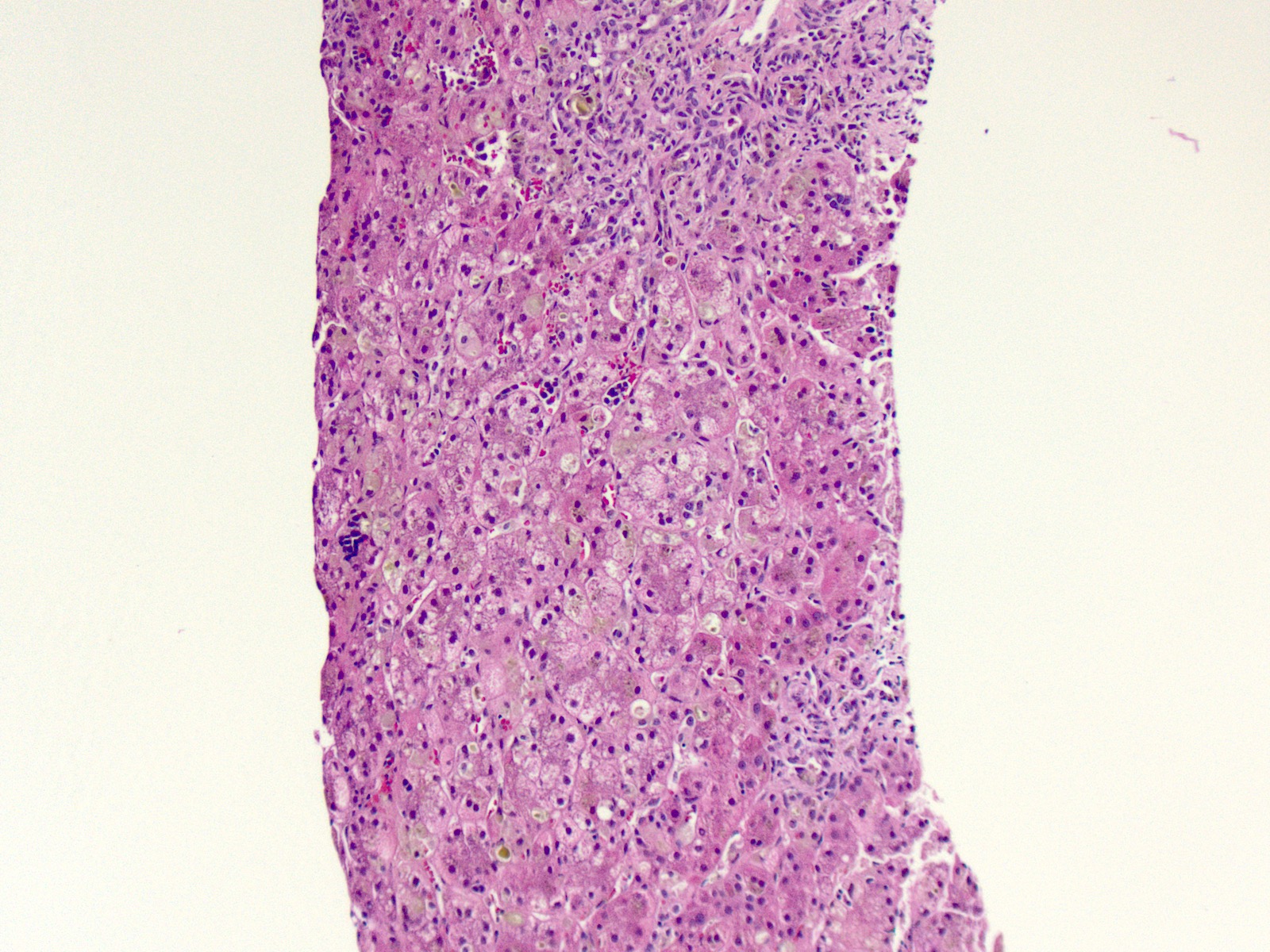
Microscopic (histologic) description
- Adults: range of following findings (Aliment Pharmacol Ther 2018;47:877)
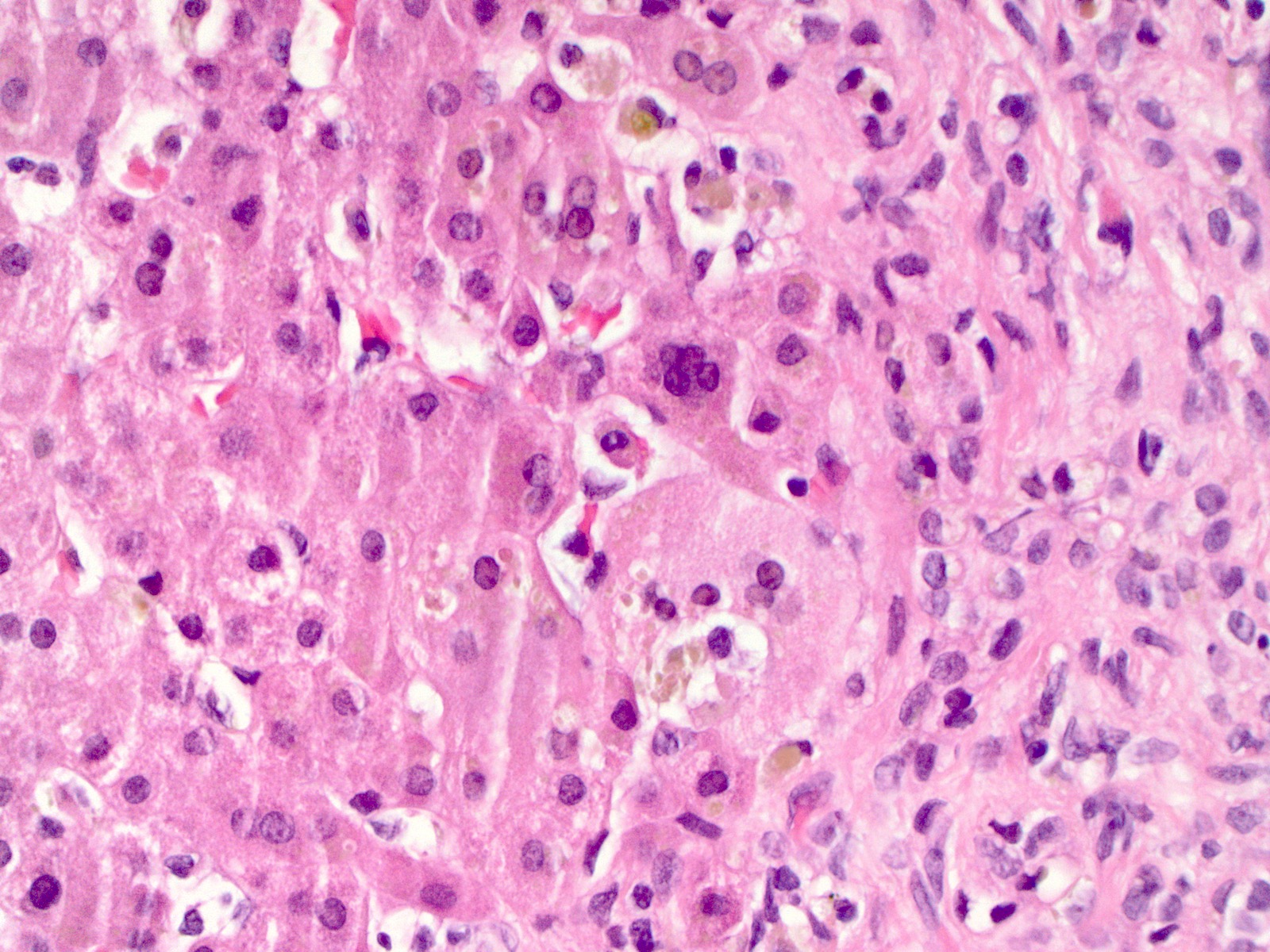
- Eosinophilic intracytoplasmic globules in hepatocytes
- Usually in zone 1, near portal triads
- Most suggestive feature of AAT deficiency
- Fibrosis: ranges from minimal periportal fibrosis to cirrhosis
- Mild portal inflammation: predominantly lymphocytic
- Mild steatosis: often in periportal hepatocytes
- Eosinophilic intracytoplasmic globules in hepatocytes
- Neonates (Hepatology 1988;8:307, Am J Surg Pathol 2010;34:1498):
- Intracytoplasmic globules may be absent or difficult to detect in neonates
- Hepatitis
- Extrahepatic biliary atresia like features including:
- Lobular cholestasis
- Bile ductular reaction
- Giant cell transformation of hepatocytes
- Variable fibrosis
Microscopic (histologic) images
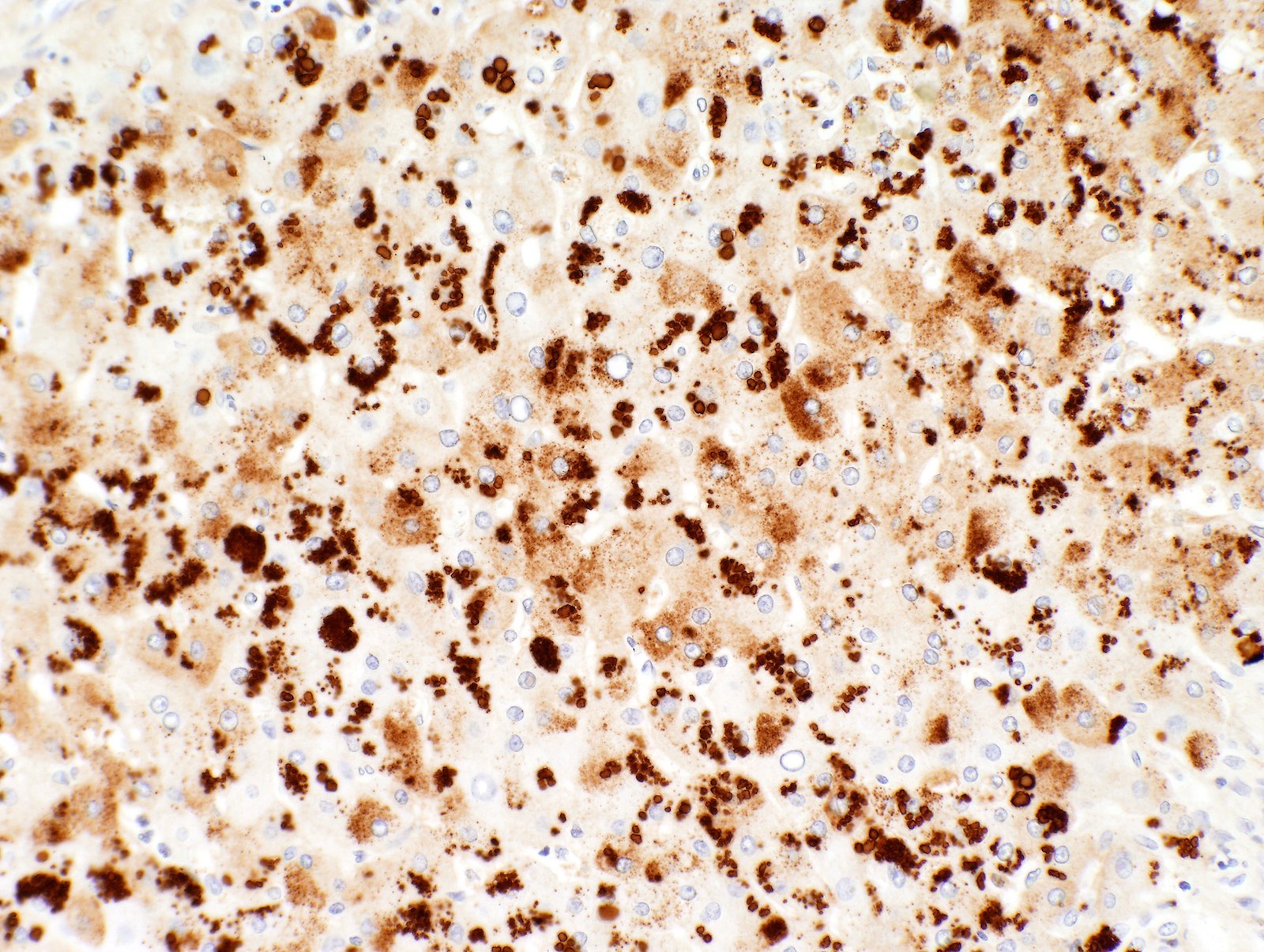
Positive stains
- Diastase resistant periodic acid Schiff (PAS) positive globules
- AAT positive globules
- Caution: inflamed and reactive hepatocytes may show background staining in the absence of AAT deficiency
Electron microscopy description
- Enlarged endoplasmic reticulum with moderately electron dense fibrillary inclusions (Ultrastruct Pathol 2020;44:32)
Sample pathology report
- Liver biopsy in an adult with elevated transaminases and total bilirubin:
- Liver, random, ultrasound guided needle core biopsy:
- Hepatocytes with cytoplasmic PAS diastase positive globules compatible with alpha-1 antitrypsin deficiency
- Cholestasis and mild portal chronic inflammation
- Periportal fibrosis noted on trichrome stain
- See comment and microscopic description
- Comment: Immunohistochemistry for AAT is positive in the cytoplasmic globules and supports the diagnosis. Correlation with laboratory findings is recommended.
- Liver, random, ultrasound guided needle core biopsy:
- Hepatectomy at the time of transplant:
- Liver, native, hepatectomy:
- Liver with cirrhosis / stage 4 fibrosis
- PAS positive, diastase resistant hepatocyte cytoplasmic globules present, consistent with patient's history of AAT deficiency
- Negative for malignancy
- Liver, native, hepatectomy:
Differential diagnosis
- Megamitochondria (Hepatology 2004;39:1423):
- Tend to be smaller
- Do not preferentially occur in zone 1 hepatocytes
- Congestive hepatopathy (Am J Clin Pathol 1983;79:697):
- Alpha-1 antichymotrypsin deficiency (Histopathology 1990;16:221, Hum Pathol 2000;31:575):
- Neonatal hepatitis (Am J Surg Pathol 2010;34:1498):
- Wide variety of causes resulting in this injury pattern
- Cirrhosis:
- AAT like globules sometimes seen in end stage liver of any etiology
Practice question #1
Which of the following is true of alpha-1 antitrypsin (AAT) deficiency in the liver?
- Electron microscopy would show intramitochondrial fibrillary inclusions
- Globules are negative for PASD and positive for AAT immunohistochemistry
- Globules represent misfolded protein within the endoplasmic reticulum
- Intracytoplasmic globules are the diagnostic feature
- Number of globules correlates with disease severity
Practice answer #1
C. Globules represent misfolded protein within the endoplasmic reticulum. Although the intracytoplasmic globules are highly suggestive of alpha-1 antitrypsin deficiency, they are not diagnostic. In fact, there are no definitive diagnostic criteria for this disease (Answer D). Additionally, the globules are variably present and may be absent in some cases. There is also no correlation between the number of globules and disease severity (Answer E). When present, the globules are positive for both PASD and AAT (Answer B). These globules represent collections of misfolded protein. On electron microscopy the fibrillary inclusions are located within the endoplasmic reticulum, not within the mitochondria (Answer A).
Comment Here
Reference: Alpha-1 antitrypsin deficiency
Comment Here
Reference: Alpha-1 antitrypsin deficiency
Practice question #2
Which of the following additional findings is most often seen associated with alpha-1 antitrypsin (AAT) deficiency in the liver of adult patients?
- Early onset cirrhosis
- Elevated tissue concentration of AAT
- High AST and low ALT
- Mild steatosis
- No detectable AAT in plasma
Practice answer #2
A. Early onset cirrhosis. Although AAT does indeed collect in the hepatocytes due to its inability to be released from the ER, tissue levels are not routinely tested (Answer B). Rather, AAT levels are measured in the plasma. An AAT deficient phenotype is most common and would have a low but still detectable plasma level of AAT. This phenotype has the mutant "z" or "s" alleles. A null phenotype is much rarer and no AAT can be detected in the plasma of such patients due to degradation of the protein entirely (Answer E). A dysfunctional phenotype is also rare, but although the protein does not function properly there are normal plasma levels of AAT. Other laboratory abnormalities would be elevations in both AST and ALT (Answer C) indicating hepatocyte stress. A sole elevation in AST would be more consistent with alcoholic liver injury. Histologically, hepatic steatosis may be present but this finding is variable and much less common than fibrosis or cirrhosis (Answer D). In fact, early onset cirrhosis should prompt suspicion and testing for alpha-1 antitrypsin deficiency.
Comment Here
Reference: Alpha-1 antitrypsin deficiency
Comment Here
Reference: Alpha-1 antitrypsin deficiency