Table of Contents
Definition / general | Essential features | Physiology | Diagrams / tables | Gross description | Gross images | Bone cell types | Bone types | Microscopic (histologic) images | Electron microscopy description | Electron microscopy images | Videos | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Tahir U, Qureshi MB, Ud Din N. Histology-bone. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bonehistology.html. Accessed September 8th, 2025.
Definition / general
- Bone is a type of mesenchymal connective tissue derived from common primitive mesenchymal precursors
- Structure primarily consists of an extracellular matrix produced and modified by bone cells
- It is a composite biphasic mix of organic and inorganic components
Essential features
- Organic component (25%) includes type I fibrillar collagen (90%) and bone morphometric proteins and mucopolysaccharides (10%)
- Inorganic component (75%) predominantly comprises the mineral complex calcium hydroxyapatite (J Musculoskelet Neuronal Interact 2020;20:347)
- Organic portion provides tensile strength whereas the mineral portion gives stiffness to bone
Physiology
- Provides structural and mechanical support for movement and protection of viscera
- Helps in homeostatic mechanisms being the repository of calcium and phosphate in the body
- Acts as an endocrine organ to regulate important biologic phenomena
- Contains hematopoietic tissue
- Bone cells: osteoblasts and osteoclasts are involved in bone modeling, remodeling and repair
- Osteoblastic differentiation and maturation involve transcription factors such as runt related transcription factor 2 (RUNX2), osterix (OSX) and activating transcription factor 4 (ATF4) in addition to signaling pathways such as Wnt and Notch (Curr Opin Rheumatol 2018;30:59)
- Osteoblasts secrete type I collagen, the main component in osteoid matrix (Histochem Cell Biol 2018;149:289)
- Responsible for the production, transportation and arrangement of various components of the organic matrix (osteoid)
- Commence and regulate matrix mineralization
- Employ autocrine and paracrine mechanisms to organize the activity of adjacent osteoblasts, osteocytes and osteoclasts
- Osteocytes function as sensor cells in bone, responding to mechanical forces
- As mechanosensory cells, they convert mechanical stress into biologic activity
- Stimulated osteocytes manufacture and liberate intercellular messengers that focus on precursor cells, osteoblasts and osteoclasts
- These cells react by remodeling the bone
- Mineral homeostasis is another function of osteocytes
- Osteocytic osteolysis is a process through which osteocytes rapidly release calcium and phosphorus from mineralized matrix, which is histologically evident as distended lacunar spaces
- Osteocytes produce fibroblast growth factor 23 (FGF23), which downregulates parathyroid hormone (PTH)
- Controls osteoblastic activity by releasing sclerostin, which inhibits osteoblastic bone formation through Wnt / beta catenin pathway and osteoclastic activity through secretion of receptor activator of nuclear factor kappa beta ligand (RANKL) and osteoprotegerin (OPG) (Curr Opin Rheumatol 2018;30:59)
- Osteoclasts resorb mineralized bone more efficiently than nonmineralized tissue
- Osteoclastic development, maturation and activity involves diverse cytokines including interleukins (IL1, IL3, IL6, IL11), tumor necrosis factor (TNF), granulocyte macrophage colony stimulating factor (GM-CSF) and macrophage colony stimulating factor (M-CSF)
- These factors work by either stimulating osteoclast progenitor cells or influencing other bone cells in a paracrine manner
- This system is essential to bone metabolism and its mediators include the molecules RANK, RANKL and OPG
- RANK / RANKL signaling is important in bone metabolism as a stimulator of osteoclast production, differentiation, activation and survival
- RANKL can be blocked by another component of the TNF family of receptors, OPG, which is a soluble protein formed by various tissues including bone, hematopoietic marrow cells and immune cells
- OPG inhibits osteoclastogenesis, acting as a decoy receptor that binds to RANKL and prevents the interaction of RANK with RANKL
- The interplay permits osteoblasts and stromal cells to manage osteoclast development
- This ensures the tight pairing of bone formation and resorption, which is vital to the success of the skeleton
Gross description
- Firm and stiff with high tensile strength
- Tan-white and smooth
- All bones generally have a
- Periosteum: fibrous connective tissue attached to the outer surface of the cortex (Eur J Radiol Open 2020:7:100249)
- Cortex: made up of compact (cortical) bone with the endosteal surface forming border with the medullary canal
- Medullary canal: contains variable amounts of cancellous (trabecular) bone with fatty tissue, hematopoietic elements, blood vessels and nerves
- Shafts (diaphysis) of weight bearing bones (such as bones of extremities) have almost all of their mass near the surface with dense cortex (compact bone) and a medullary cavity nearly devoid of bone
- There is a decrease in cortical thickness and increase in the content of cancellous bone towards the metaphysis
- Epiphysis is almost completely made of cancellous bone
- Less weight bearing bones of the trunk have thinner cortices and more hematopoietic marrow
Bone cell types
- Bone cells belong to the osteoprogenitor series and osteoclast series
- Osteoprogenitor series (primitive committed mesenchymal cells) is derivative of tissue bound mesenchymal stem cells
- Mesenchymal stem cells are multipotential stromal precursor cells with potential to form adipocytes, chondrocytes, myocytes and fibroblasts
- Present in the perianlage tissue of the fetus, periosteum, Haversian systems, Volkmann and medullary canals
- Osteoprogenitor cells have the ability to fabricate osteoblasts only; they have basic spindle morphology
- Osteoclast series is derived from monocyte granulocyte colony precursors in the bone marrow
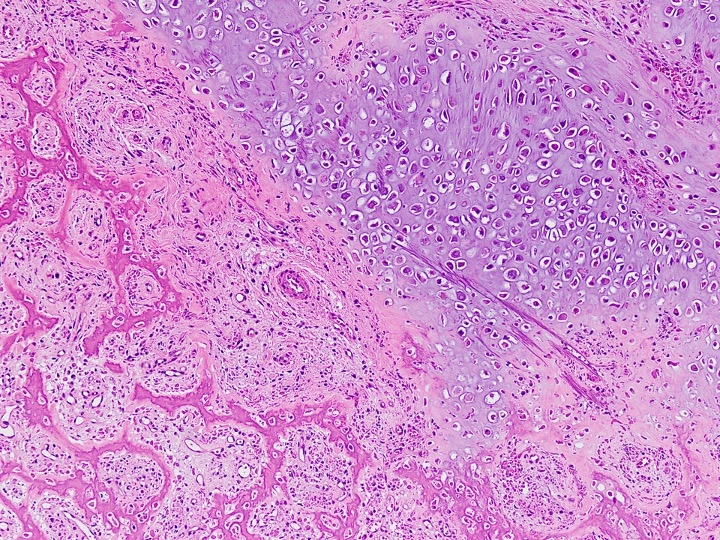
Osteoblasts
- Essential to the formation of bone tissue
- Located on actively growing bone surfaces
- Lifespan may range from months to many years
- Metabolic state is intimately associated with their morphology
- Active osteoblasts resemble plasma cells and range in size from 10 - 80 μm (average: 20 - 30 μm)
- Large cuboidal to pear shaped, polyhedral mononuclear cells when rapidly forming bone
- Contain copious amphophilic to basophilic cytoplasm that is in intimate contact with bone
- Nuclear membranes are distinct with eccentric (polarized away from the matrix) vesicular nuclei that possess 1 or more prominent nucleoli
- Visible perinuclear halo representing Golgi apparatus
- Inactive osteoblasts / lining cells are spindle shaped to flattened
- Present on the surface of bony trabeculae
- Have flattened, nonreactive nuclei with scant cytoplasm
- ~60 - 80% of osteoblasts go through apoptosis
- Remaining osteoblasts either develop into osteocytes enveloped by matrix or flatten and stretch forming cellular coating on bone surfaces (J Bone Miner Res 2021;36:1432)
- Active osteoblasts resemble plasma cells and range in size from 10 - 80 μm (average: 20 - 30 μm)
Osteocytes
- Most abundant cell type of bone (> 90% of bone cells in adult bone)
- Terminally differentiated osteoblasts that incorporate into bone matrix
- Half life approaches 25 years
- Appear as small blue dots within lacunar spaces in the bone matrix
- Cell body, nucleus and surrounding scant cytoplasm dwell inside a lacunar space
- Nuclei are small and not evident in every plane of section; therefore, in most slides of bone tissue, lacunae are empty
- Part of osteocyte cytoplasm pinches off into long and delicate cytoplasmic processes resembling axons
- These processes lie in canaliculi (channels traversing through the bone matrix)
- The ends of osteocyte cell processes connect to those of adjoining osteocytes and to surface osteoblasts through gap junctions (Annu Rev Physiol 2020:82:485)
- This creates a tremendous surface area of contact between the osteocyte and the matrix and extracellular fluid surrounding each cell
- In this way, osteocytes communicate with one another forming intricate and integrated systems all over the bone tissue
- Number, size, shape and position of osteocytes depend upon the type of bone they reside in
- Woven bone
- Abundant, big and plump
- Appears disordered and random microscopically as their long axes are parallel to the direction of adjacent collagen fibers
- Lamellar bone
- Less in number, smaller, spindly
- Seem to be organized as the cells are arranged in the same direction as the surrounding lamellae
- Osteocyte apoptosis increases with aging, causing reduced osteocyte density
- Woven bone
Osteoclasts
- Osteoclasts are terminally differentiated cells
- Lifespan of days to weeks
- Present in scalloped, cup shaped depressions on bone surface called Howship lacunae
- 40 - 100 μm in diameter
- Polarized with one part of cell membrane closely adhered to bone (ruffled border) while the other pole is exposed to extracellular fluid
- Have granular eosinophilic cytoplasm, may have 4 - 20 nuclei
- Metabolic activation of osteoclasts is initiated by anchorage
- Activated nuclei coordinate the complex and transitory cytoplasmic and cell membrane alterations necessary for bone digestion
- After osteoclastic activity, macrophages mobilize to the base of the resorption pit and phagocytize the organic remnants (Connect Tissue Res 2018;59:99)
- Osteoclast-like giant cells are multinucleated cells that were once osteoclasts but could not be defined at the moment because of absence of residual bone
Bone types
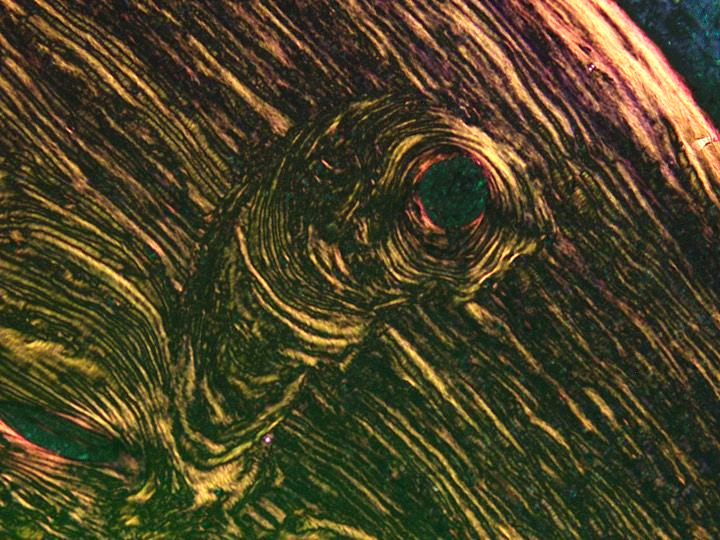
- Based on matrix arrangement (orientation of collagen type I), bone can be classified as
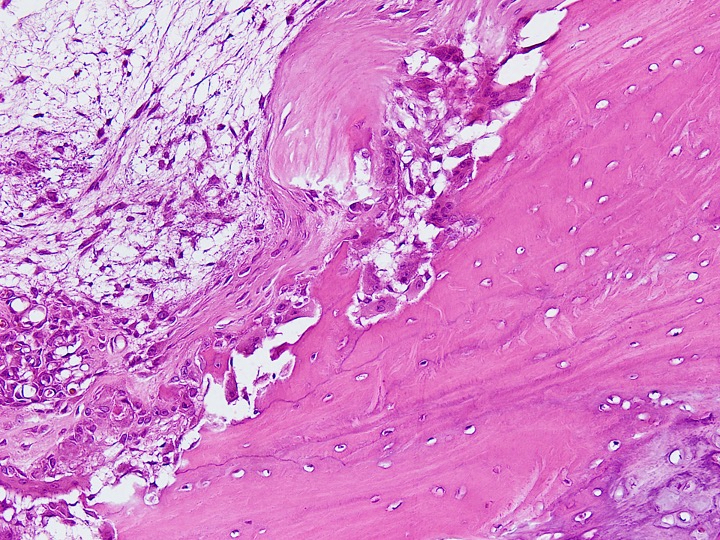
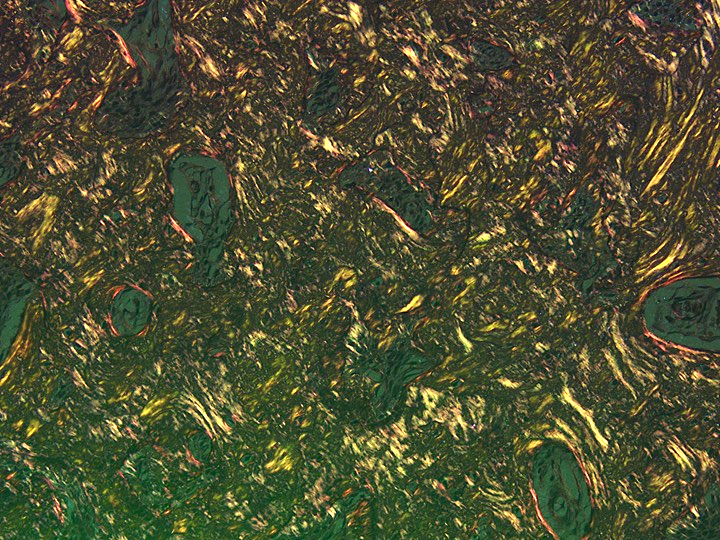
Woven bone / immature bone- Develops in utero and during phases of rapid bone formation
- Coarsely and haphazardly oriented collagen with thick and loosely packed collagen fibers
- Mineral content and osteocyte density are high
- Osteocytes and lacunae are larger than those of mature bone
- Calcification is irregular
- Resembles particle board
- Weaker, less rigid and more elastic than lamellar bone
Lamellar bone / mature bone- Synthesized following birth
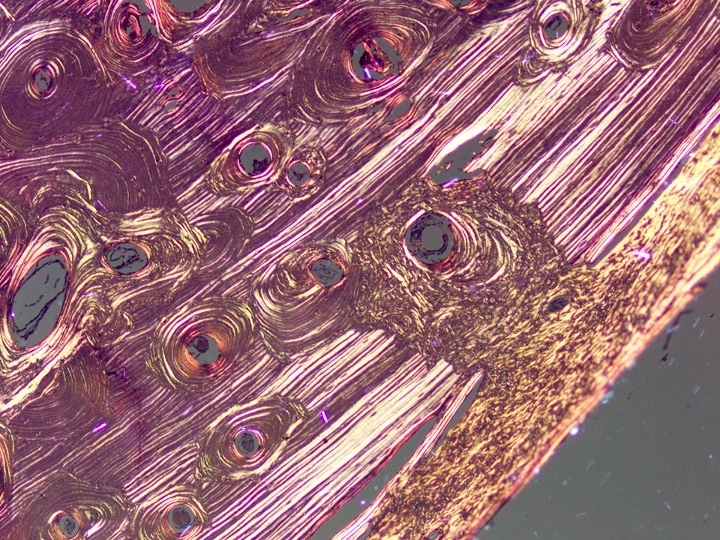
- Collagen is present in successive layers with delicate and more closely packed fibers in the same direction to each other
- Collagen bundles are organized in parallel layers or concentric layers / sheets called lamellae
- Mineral content and osteocyte density are low and collagen density is high
- Osteocytes and lacunae are smaller and organized
- Resembles plywood
- Firm with more tensile strength and less flexible than woven bone (Annu Rev Biomed Eng 2018:20:119)
- Based on texture, bone can be classified as
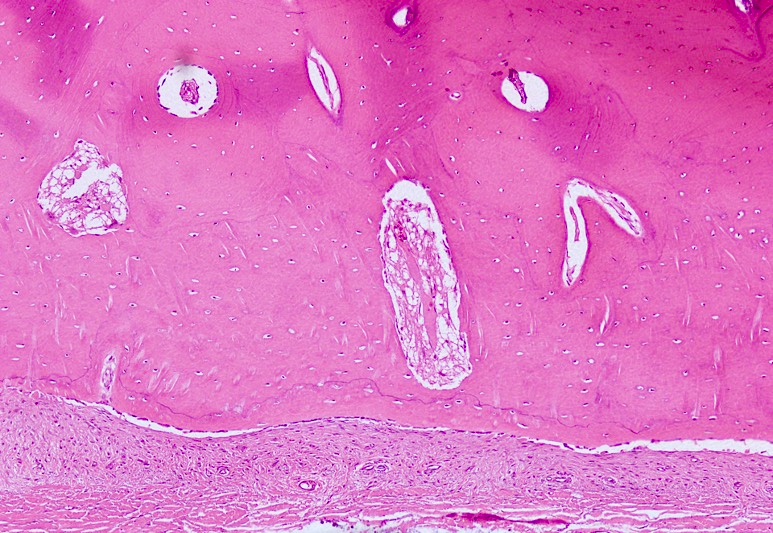
Cortical bone- Also known as compact bone
- 90% bone and 10% space by volume
- Found in diaphysis of long bones
- Surrounds the cancellous compartment of epiphysis and metaphysis of long bones
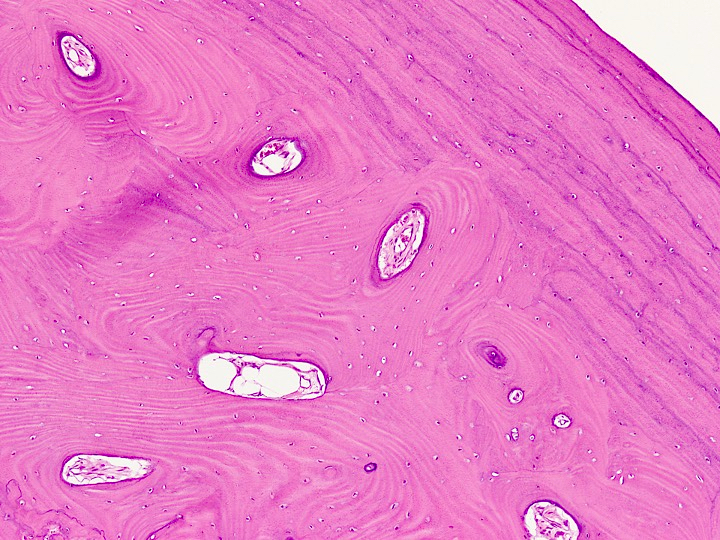
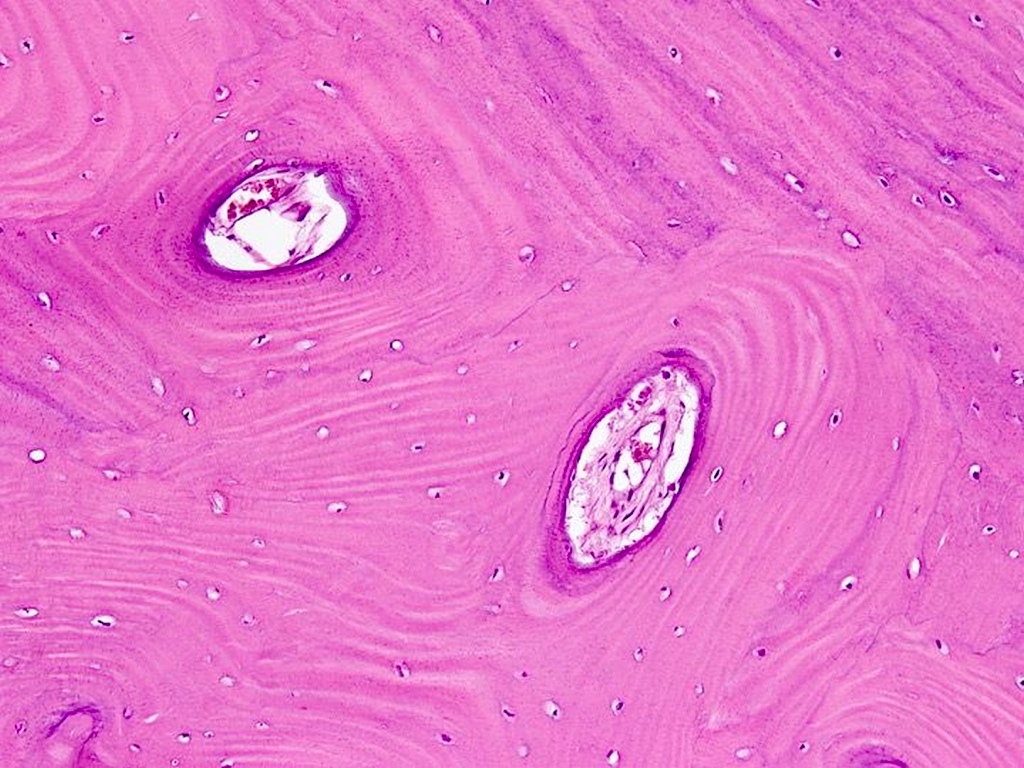
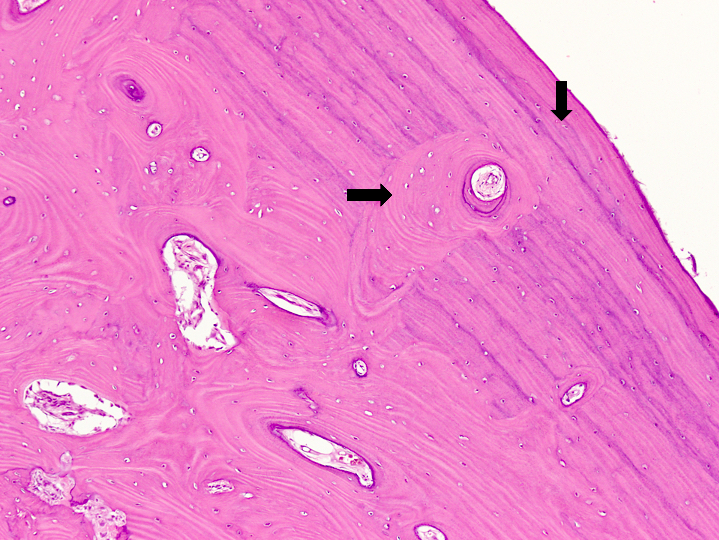
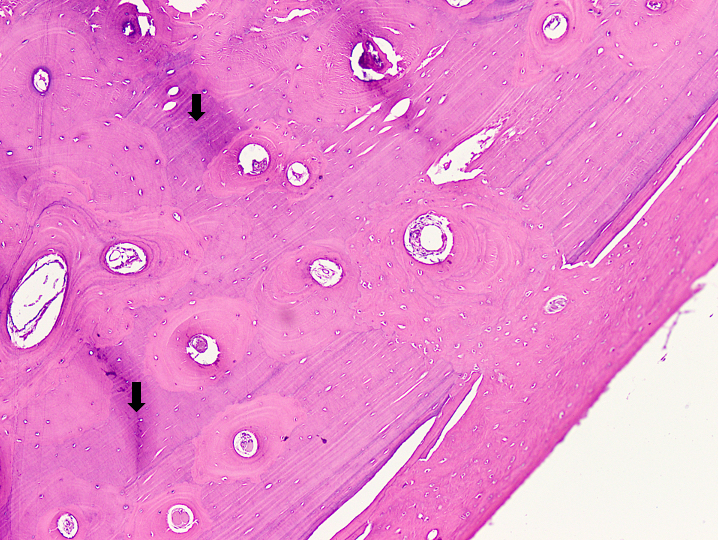
- Interior of bone consists of Haversian canals, Volkmann canals, osteocyte lacunae and osteocyte canaliculi
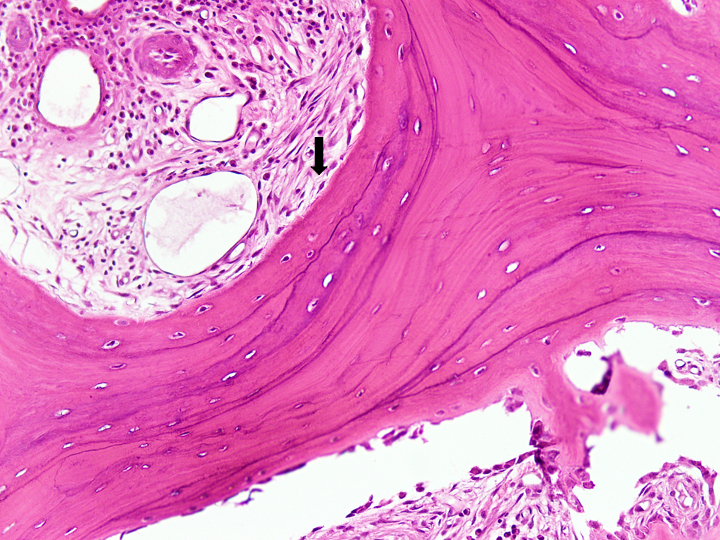
- Bulk of compact bone is lamellar in type and comprises circumferential lamellae and secondary osteons
- Haversian canals are tubes or tunnels in cortical bone that contain nerve fibers and a few capillaries
- Circumferential lamellae encircle the entire bone
- Earliest circumferential lamellae made during development lie on the inside of bony cortex (called inner circumferential lamellae), whereas the newest cortical lamellae deposited by periosteum lie on the outer surface of the cortex and are called outer circumferential lamellae
- Secondary osteons are circumferential lamellae that encircle Haversian canals (Materials (Basel) 2019;12:913)
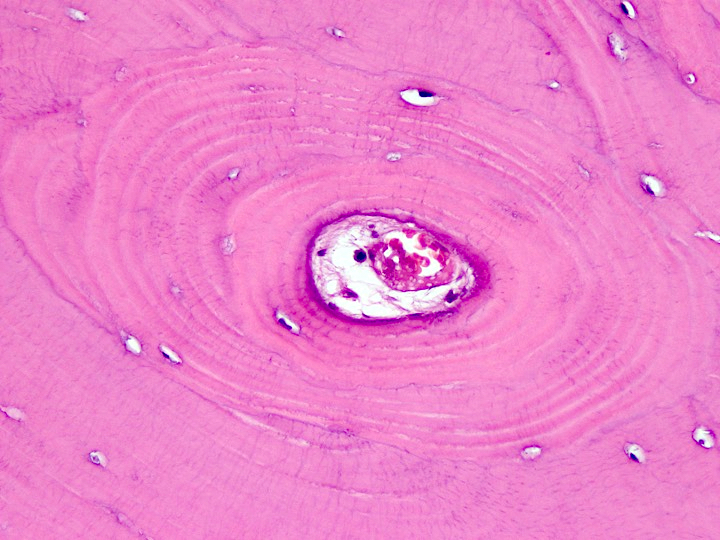
- Osteon (Haversian units) are structural and functional elements of cortical bone
- Osteons are cylinders with hollow centers oriented in the same axis as the long axis of bone
- They branch and twist to connect with other osteons via lateral vascular channels called Volkmann canals
- They replace circumferential lamellae in weight bearing bones
- Osteocytes are present in spaces called osteocyte lacunae, which are ovoid spaces at the junctures of adjacent lamellae
- Osteocyte canaliculi house the cell processes of osteocytes and are oriented radially to the Haversian canal between the osteocyte lacunae
- Blood vessels and nerve fibers traverse Haversian canals
- Osteoclasts and osteoblast progenitor cells pass through Haversian canals to initiate cortical bone remodeling
- When parts of osteons or circumferential lamellae are remodeled by osteoclasts, the residual bone not supplied by previous blood supply becomes interstitial lamellae
- Interstitial lamellae appear as randomly arranged pieces of bone in the cortex
- Have necrotic bone matrix and lacunae devoid of osteocytes
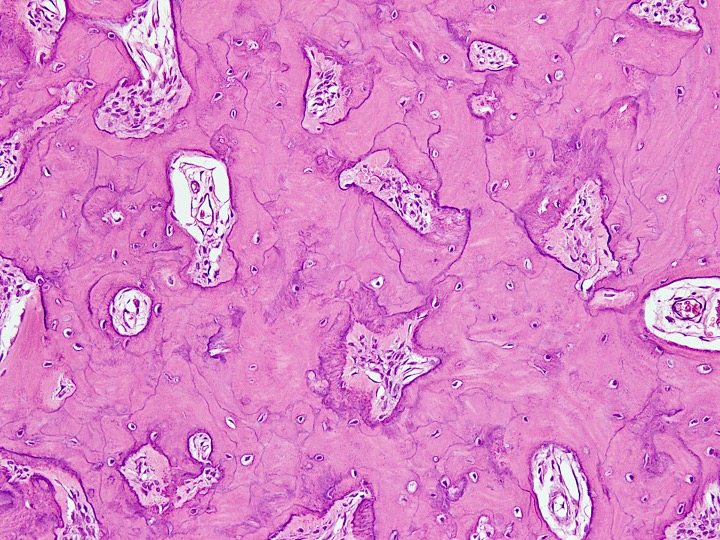
Trabecular bone- Also known as spongy or cancellous bone
- 25% bone and 75% space by volume in long bone
- Found in vertebrae, epiphysis and metaphysis of long bones (J Musculoskelet Neuronal Interact 2020;20:347)
- Vertical plates of lamellar bone interconnected by short and thick lateral struts
- Intertrabecular spaces contain bone marrow
Cement lines- Basophilic lines produced by osteoblasts that separate osteons, interstitial lamellae and circumferential lamellae from one another (Bone 2018:110:187)
- Have more calcium and mucopolysaccharides than surrounding bone
- When bone is produced on a resorbed surface after osteoclastic activity, the cement lines produced by osteoblasts are called reversal cement lines
- Cement lines produced by osteoblasts after prolonged inactivity are called arrest cement lines
- Lamellae are oriented in different planes on the opposite sides of reversal cement lines, whereas lamellae in arrest cement lines are oriented in the same plane on opposite sides
Periosteum- Slender, vascularized layer of tan-white fibrous connective tissue that immediately surrounds the outer surface of all cortices (Eur J Radiol Open 2020:7:100249)
- Composed of an outer fibrous layer and an inner cellular (cambium) layer in children
- Cambium layer is composed of spindle shaped fibroblasts, osteoprogenitor cells and mature osteoblasts
- In adults, the periosteum is just a fibrous covering
- Fibrous layer contains fibroblasts and type I collagen fibers that are in continuation with the joint capsule, tendons and muscle fascia
- Periosteum is connected to bone by collagen fibers called Sharpey fibers
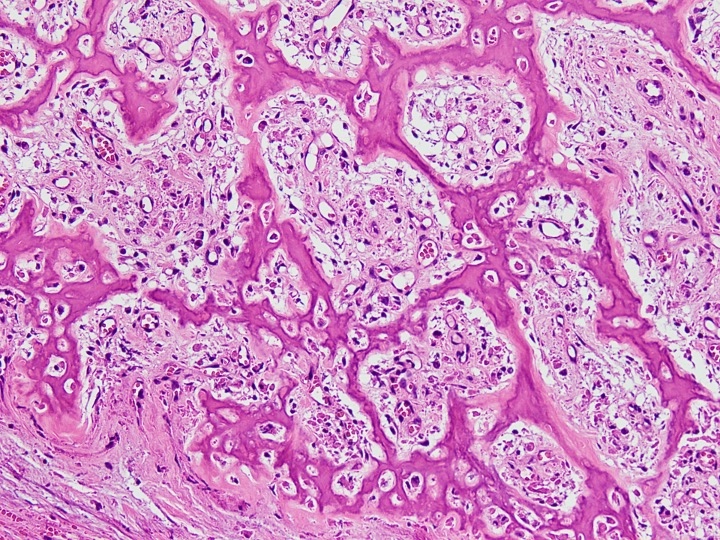
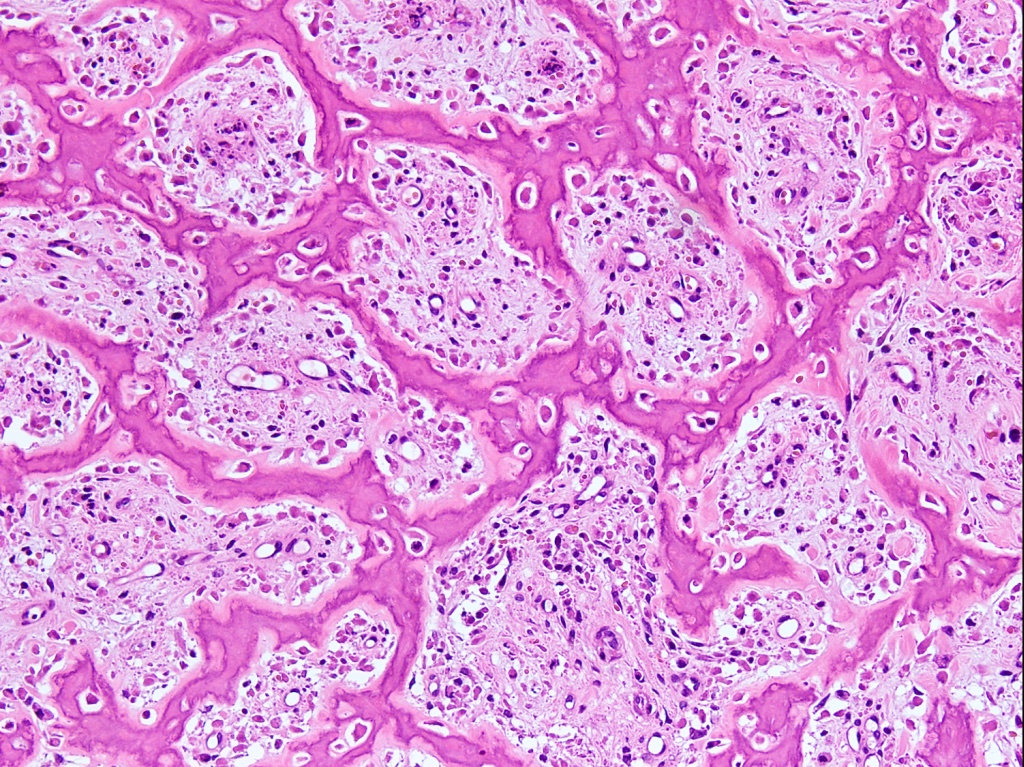
Microscopic (histologic) images
Electron microscopy description
- Osteoblasts
- Cytoplasm of active osteoblasts contains widespread granular endoplasmic reticulum, a large, prominent Golgi apparatus, abundant mitochondria and lysosomes
- In contrast, the cytoplasm of inactive osteoblasts resembles that of quiescent fibroblasts
- Osteoclasts
- In the cytoplasm, a network of interrelated actin filaments extends from the site where the osteoclast cell membrane attaches to the bone (clear zone) directly to the nuclei
- Reference: StatPearls: Histology, Osteoblasts [Accessed 7 November 2023]
Videos
Normal bone histology & embryology 101 with Dr. Andrew Rosenberg
Bone cells and bone formation
Practice question #1
Practice answer #1
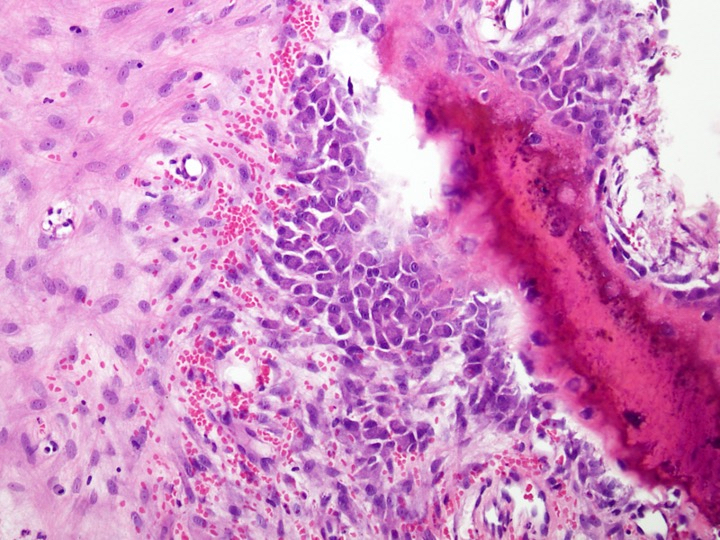
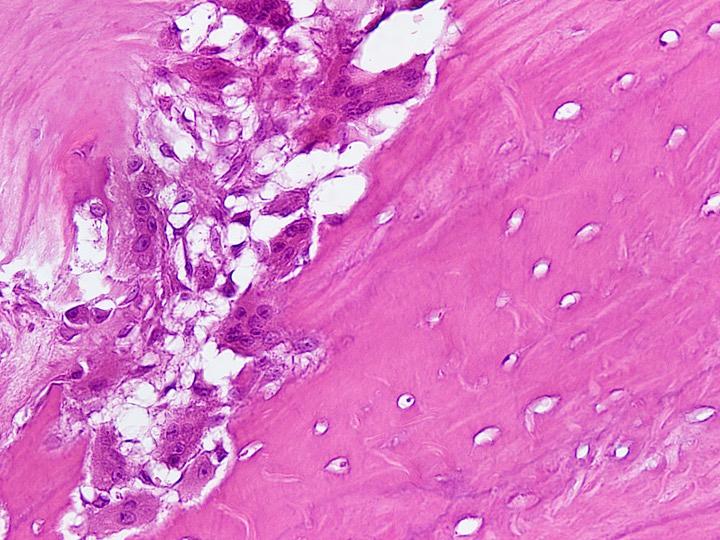
E. Weaker, less rigid and more flexible than lamellar bone. The image depicts woven bone, which is weaker, less rigid and more flexible than lamellar bone. Answer C is incorrect because woven bone has a higher mineral content than lamellar bone. Answer B is incorrect because woven bone is more hypercellular than lamellar bone. Answer D is incorrect because woven bone is fabricated during rapid bone formation. Answer A is incorrect because collagen bundles are arranged haphazardly in woven bone.
Comment Here
Reference: Histology-bone
Comment Here
Reference: Histology-bone
Practice question #2
Which of the following corresponds to this structure?
- Does not go through apoptosis
- Has abundant cytoplasm and is multinucleated
- Most abundant cell type of bone tissue
- Resembles plasma cells, is polyhedral, with copious amphophilic cytoplasm and eccentrically placed nuclei with 1 or more nucleoli
- Spindle shaped
Practice answer #2
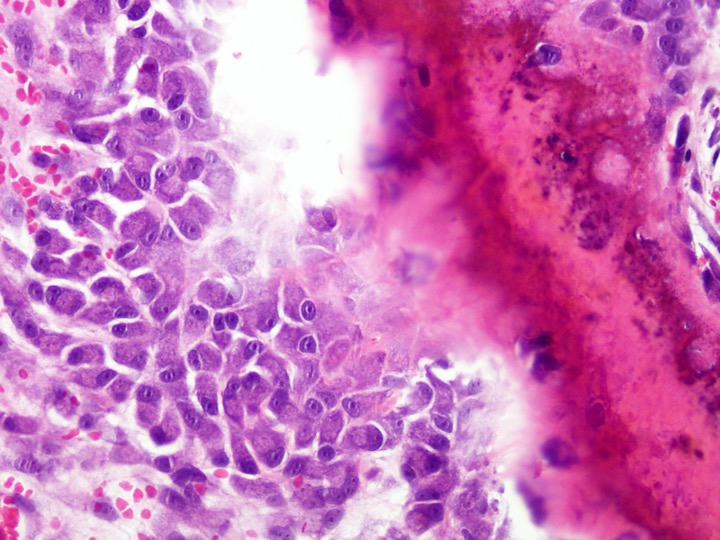
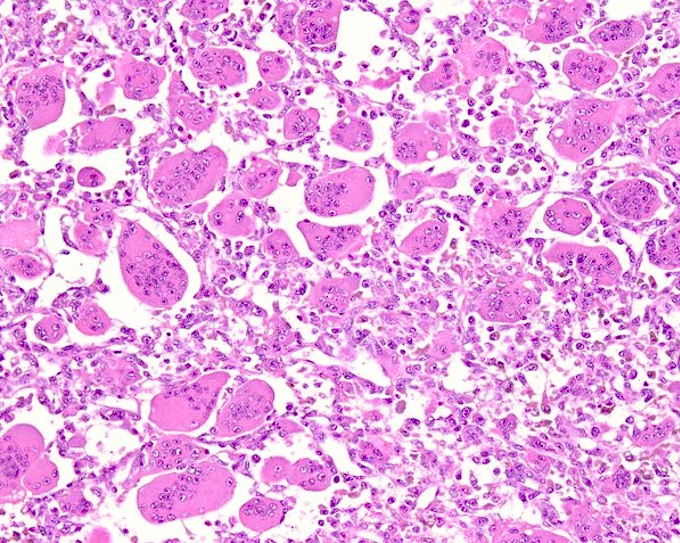
D. Resembles plasma cells, is polyhedral, with copious amphophilic cytoplasm and eccentrically placed nuclei with 1 or more nucleoli. This is a description of activated osteoblasts, which resemble plasma cells in that they have an eccentrically placed nucleus with copious amphophilic cytoplasm. Answer E is incorrect because inactive osteoblasts are spindle shaped to flattened, not active osteoblasts as shown here. Answer B is incorrect because osteoclasts have abundant cytoplasm and multiple nuclei, not active osteoblasts. Answer A is incorrect because ~80% of active osteoblasts undergo apoptosis. Answer C is incorrect because osteocytes are the most abundant cell type in bone tissue, not active osteoblasts.
Comment Here
Reference: Histology-bone
Comment Here
Reference: Histology-bone