Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Immunofluorescence description | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Videos | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Canan F, White CL. Corticobasal degeneration. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/cnscorticobasaldegeneration.html. Accessed September 18th, 2025.
Definition / general
- Corticobasal degeneration (CBD) is a rare, progressive neurodegenerative disorder characterized by a 4 repeat tau isoform tauopathy
- Clinical features of CBD are marked by asymmetric cortical and basal ganglia dysfunction, leading to a combination of motor, cognitive and behavioral impairments, including apraxia, rigidity and alien limb phenomena (Clin Park Relat Disord 2019;1:66)
Essential features
- Neuropathological hallmark of CBD is the deposition of inclusions in neurons and glia composed of hyperphosphorylated tau with 4 microtubule binding repeats (4R tau)
- 4R tau positive glial (astrocytic) plaques and alpha B crystallin positive ballooned neurons are characteristic of CBD
- CBD clinical and neuropathological findings may show some overlap with other 4R tauopathies, such as progressive supranuclear palsy and argyrophilic grain disease
Terminology
- Corticobasal ganglionic degeneration
- Corticodentatonigral degeneration with neuronal achromasia (historical term; not recommended)
ICD coding
Epidemiology
- Age of onset of CBD is typically late adulthood, commonly between the fifth and seventh decades of life (Semin Neurol 2014;34:160)
- No sex difference (Mov Disord Clin Pract 2022;9:604)
- Data on incidence and prevalence of corticobasal degeneration are limited
- Prevalence rates for corticobasal syndrome (CBS) ranges from 0.83 (0.1 - 3.0) to 25 (0 - 59) per 100,000 (Mov Disord Clin Pract 2022;9:604, J Neurol 2023;270:4451)
- Incidence rates for CBS ranges from 0.03 (0 - 0.18) to 0.8 (0.4 - 1.3) per 100,000 person years (J Neurol 2023;270:4451)
Sites
- CBD primarily affects the central nervous system
- It affects several regions of the brain involved in motor control, cognition and sensory processing
- Mainly affected areas include the cerebral cortex (particularly posterior frontal and parietal lobes), basal ganglia, subthalamic nucleus, substantia nigra and thalamus (J Neuropathol Exp Neurol 2002;61:935, Am J Pathol 2002;160:2045)
- These regions' involvement accounts for the complex symptoms of CBD, which may overlap with or mimic other neurodegenerative disorders
Pathophysiology
- Tau dysfunction
- Tau proteins are produced through alternative splicing of the MAPT gene, generating 3R and 4R isoforms based on the presence or absence of exon 10 (Annu Rev Pathol 2024;19:345)
- 4R tau, which has 4 microtubule binding repeats, predominates in CBD pathology, while 3R tau, with 3 repeats, is less involved (J Neurochem 1999;72:1243, FEBS Lett 2018;592:2383)
- Altered post translational modifications of tau (e.g., phosphorylation, acetylation, methylation) may contribute to neurodegeneration (Cytoskeleton (Hoboken) 2024;81:95)
- Tau aggregation
- Monomeric tau assembles into tau filaments and deposits in cells, promoting pathological tau species and aggregate formation (Acta Neuropathol Commun 2017;5:99)
- Tau aggregation results in toxic gain of function and impairment of tau physiological roles, like axonal transport (Annu Rev Neurosci 2017;40:189)
- Glial tau accumulation
- Tau positive astrocytic and oligodendroglial inclusions are characteristic of CBD (Brain Pathol 1999;9:663)
- In CBD, tau pathology in astroglia might precede neuronal involvement (Brain 2016;139:3237)
- Microglial involvement
- In CBD, microglial activation is increased and correlates with tau burden, with a distinctive pattern compared to progressive supranuclear palsy, showing more involvement in supratentorial structures (J Neuropathol Exp Neurol 2001;60:647)
- Microglial activation in CBD shows asymmetry, often corresponding to the side of symptom onset and affects primary motor and supplementary motor areas, as observed through positron emission tomography (PET) imaging (Signal Transduct Target Ther 2023;8:359)
Etiology
- CBD is a sporadic disease in the majority of cases
- Genetic susceptibility
- Genome wide association studies (GWAS) suggest link of susceptibility loci in CBD to vesicular trafficking and tau phosphorylation dysfunction (Nat Commun 2015;6:7247, Acta Neuropathol 2017;133:825)
- Rare cases with pathologically proven CBD are shown to exhibit p.V363I MAPT mutation (Neurol Genet 2019;5:e347)
Diagrams / tables
Clinical features
- CBD can manifest in a variety of clinical phenotypes
- Several diagnostic criteria for CBD have been proposed (Ann Neurol 2003;54:S15, J Neurol Neurosurg Psychiatry 2012;83:405, Neurology 2013;80:496)
- Progressive, asymmetric pyramidal motor neuron (rigidity, dystonia, akinesia or myoclonus) and cortical signs (apraxia or alien limb phenomenon) is universally proposed in all criteria
- Armstrong et al. described 4 CBD phenotypes (Neurology 2013;80:496)
- Corticobasal syndrome (CBS): most common clinical phenotype, associated with CBD pathology in 24 - 54% of cases (J Neurol Neurosurg Psychiatry 2022;93:919)
- Probable CBS: asymmetric presentation of at least 2 motor features (limb rigidity or akinesia, limb dystonia and limb myoclonus) and 2 higher cortical dysfunctions (apraxia, cortical sensory deficit, alien limb phenomena)
- Possible CBS: asymmetric or symmetric presentation of at least 1 motor feature (limb rigidity or akinesia, limb dystonia and limb myoclonus) and 1 higher cortical dysfunction (apraxia, cortical sensory deficit, alien limb phenomena)
- Frontal behavioral spatial syndrome: at least 2 of the following
- Executive dysfunction
- Behavioral or personality changes
- Visuospatial deficits
- Nonfluent / agrammatic variant of primary progressive aphasia: effortful, agrammatic speech plus at least 1 of the following
- Impaired grammar / sentence comprehension with relatively preserved single word comprehension
- Groping, distorted speech production (apraxia of speech)
- Progressive supranuclear palsy (PSP) syndrome: at least 3 of the following
- Axial or symmetric limb rigidity or akinesia
- Postural instability or falls
- Urinary incontinence
- Behavioral changes
- Supranuclear vertical gaze palsy or decreased velocity of vertical saccades
- Corticobasal syndrome (CBS): most common clinical phenotype, associated with CBD pathology in 24 - 54% of cases (J Neurol Neurosurg Psychiatry 2022;93:919)
- Patient / caregiver reported functional scale for CBD (the Cortical Basal ganglia Functional Scale, CBFS) is freely available (Parkinsonism Relat Disord 2020;79:121)
- Accuracy of antemortem prediction of CBD is currently limited by lack of definitive clinical and biomarker specificity (Ann Neurol 2011;70:327)
Diagnosis
- Brain autopsy is the gold standard for CBD diagnosis (see Microscopic (histologic) features description)
- First standardized neuropathological criteria for CBD were published in 2002 (J Neuropathol Exp Neurol 2002;61:935)
Laboratory
- Fluid and tissue biomarkers for CBD is an area of active research (J Neurol Neurosurg Psychiatry 2022;93:919, Acta Neuropathol 2020;139:79)
Radiology description
- Asymmetrical cortical atrophy, which is more pronounced in the peri-Rolandic region (precentral and postcentral gyrus), posterior frontal and parietal lobes, contralateral to the clinically more severely affected side
Prognostic factors
- Survival in individuals with clinical CBS is similar to that in progressive supranuclear palsy (PSP), estimated at about 7 years from symptom onset (Continuum (Minneap Minn) 2022;28:1364)
- Survival in autopsy confirmed cases ranges from 2.5 to 12.5 years (Continuum (Minneap Minn) 2022;28:1364)
- In CBS, death usually results from complications of immobility or dysphagia (J Neurol Neurosurg Psychiatry 1998;64:184)
Case reports
- 62 year old man with acute ataxia that began at age 58 (BMC Neurol 2021;21:148)
- 72 year old man presented with frequent freezing of gait and recurrent falls from age 68 (J Korean Med Sci 2022;37:e183)
- 78 year old man with REM sleep behavior disorder and visual hallucinations (Mov Disord Clin Pract 2022;9:383)
Treatment
- No effective pharmacological interventions (Dement Neuropsychol 2020;14:243)
- Symptom based treatment may be useful for improving motor (Parkinsonism, dystonia and myoclonus) and nonmotor (cognitive behavioral) symptoms (Parkinsonism Relat Disord 2016;22:S96)
- Several disease modifying therapeutics are being tested in clinical trials for the treatment of 4R tauopathies (Neurotherapeutics 2020;17:1563)
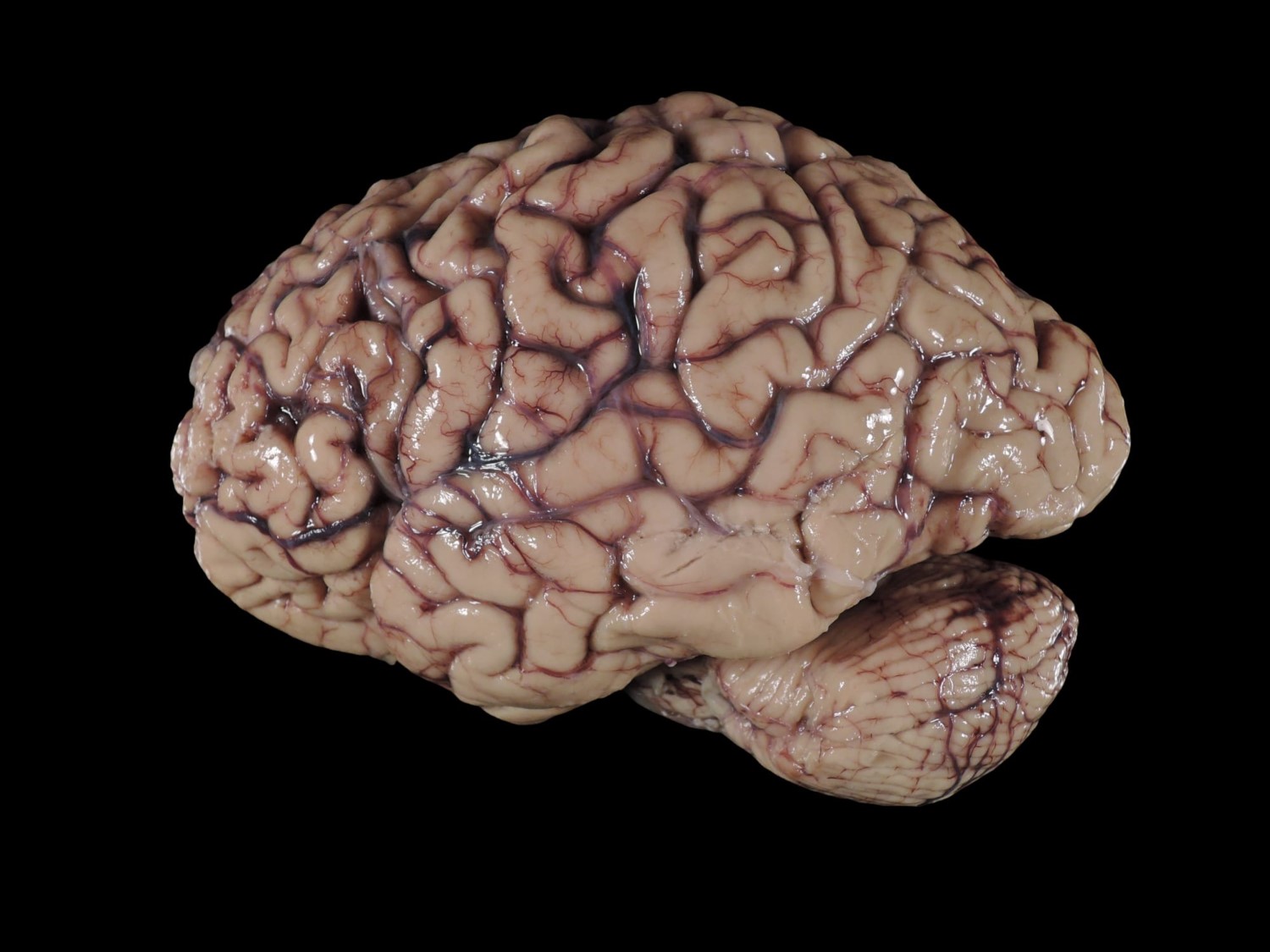
Gross description
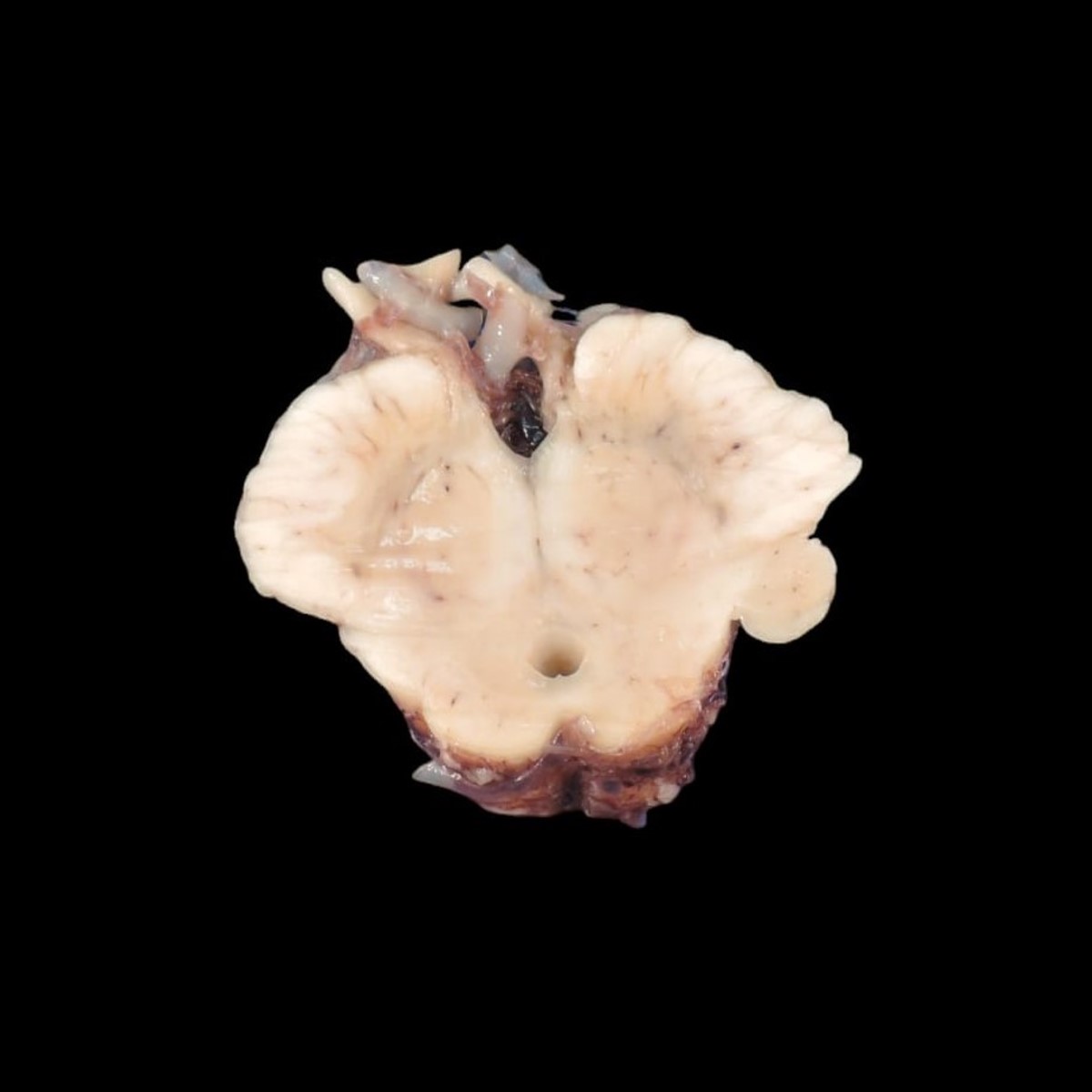
- Focal and asymmetric cortical atrophy mostly in the superior frontal and parietal parasagittal regions, in a peri-Rolandic distribution (J Neuropathol Exp Neurol 2002;61:935)
- Frontotemporal atrophy can be seen
- Atrophy and flattening of the caudate nucleus
- Attenuation of the cerebral white matter and thinning of the corpus collosum
- Substantia nigra can show depigmentation
Gross images
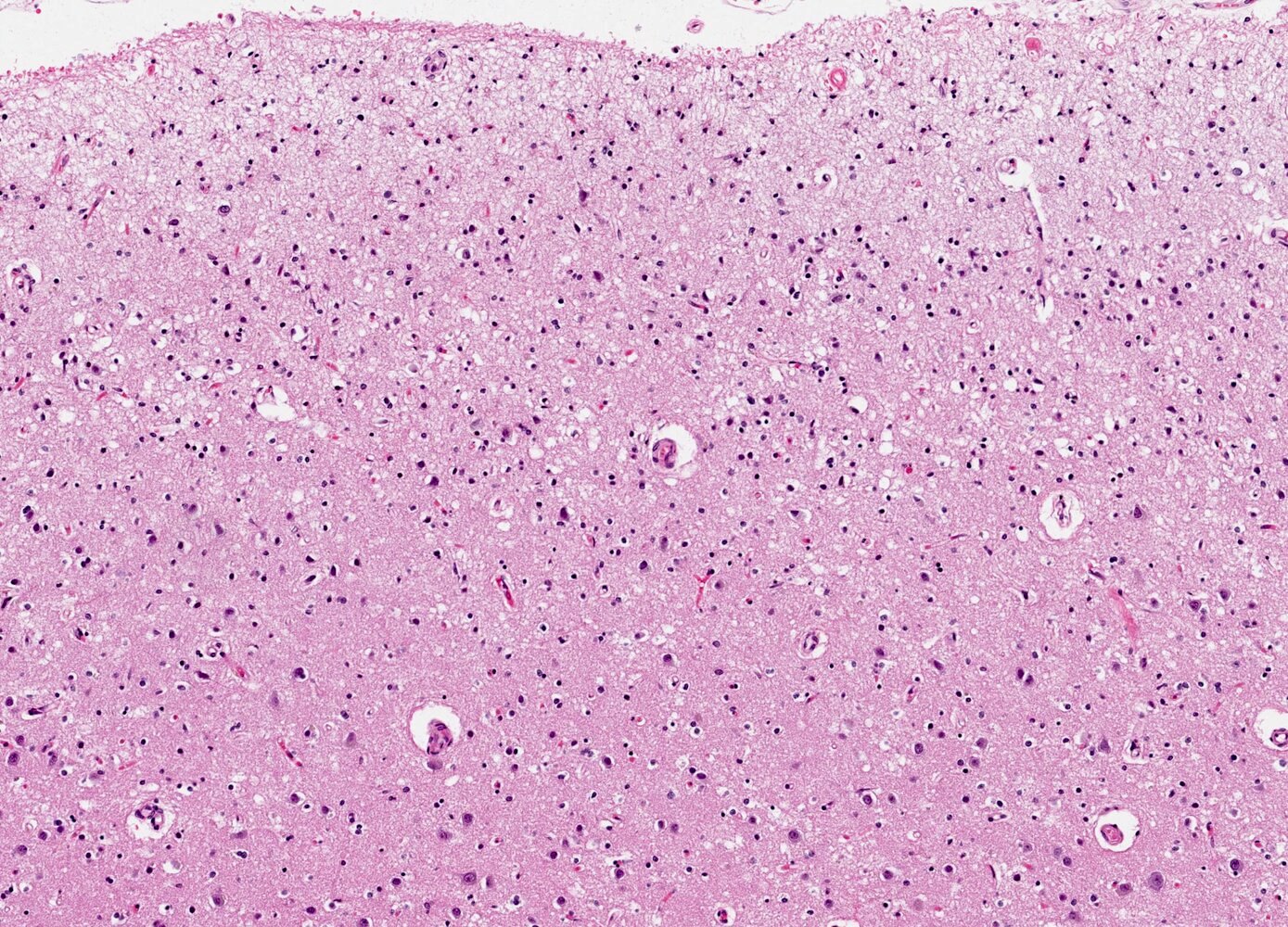
Microscopic (histologic) description
- CBD is characterized by the accumulation of pathological aggregates of the 4R tau isoform (Prog Neurobiol 2019;180:101644)
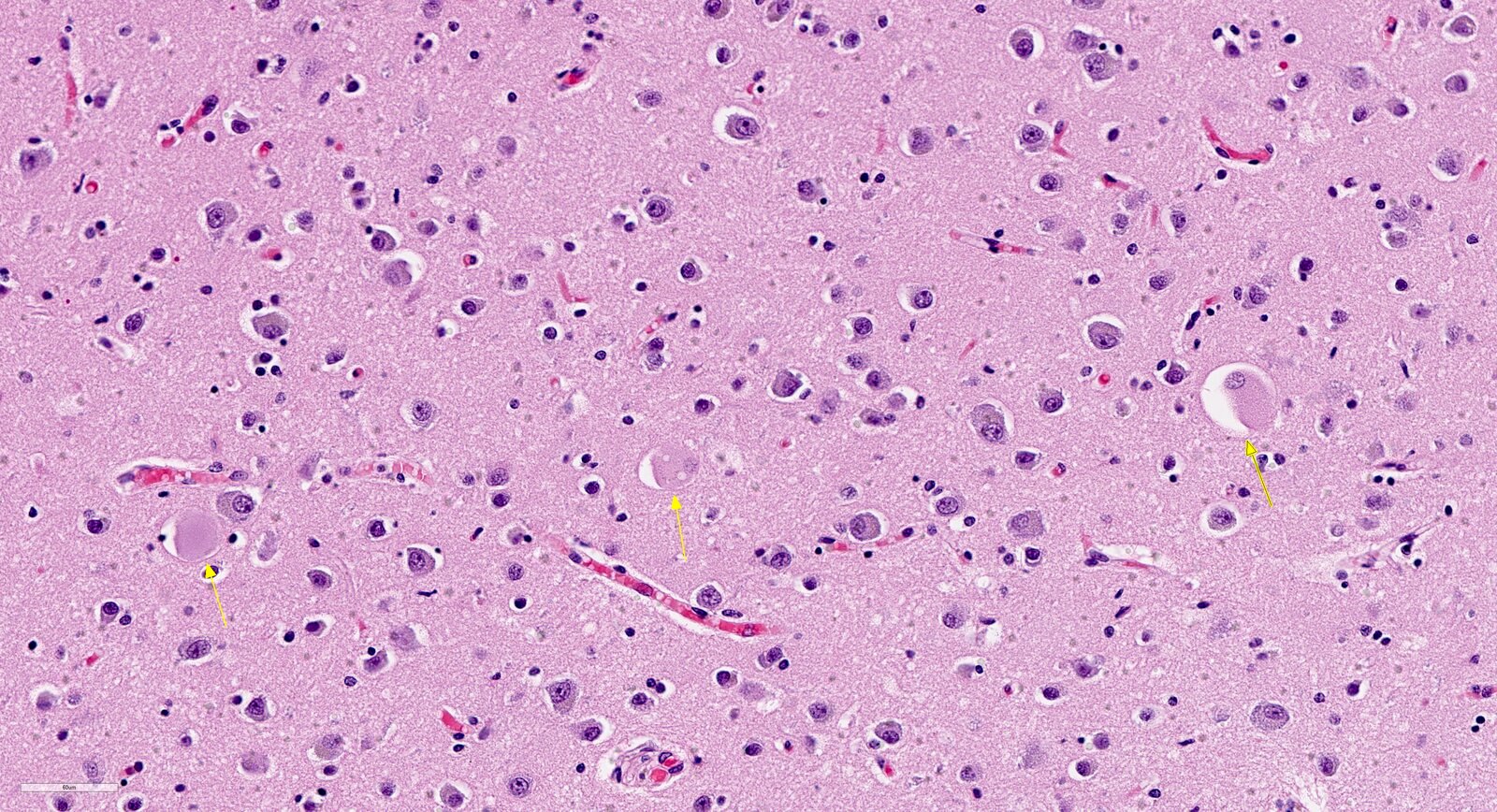
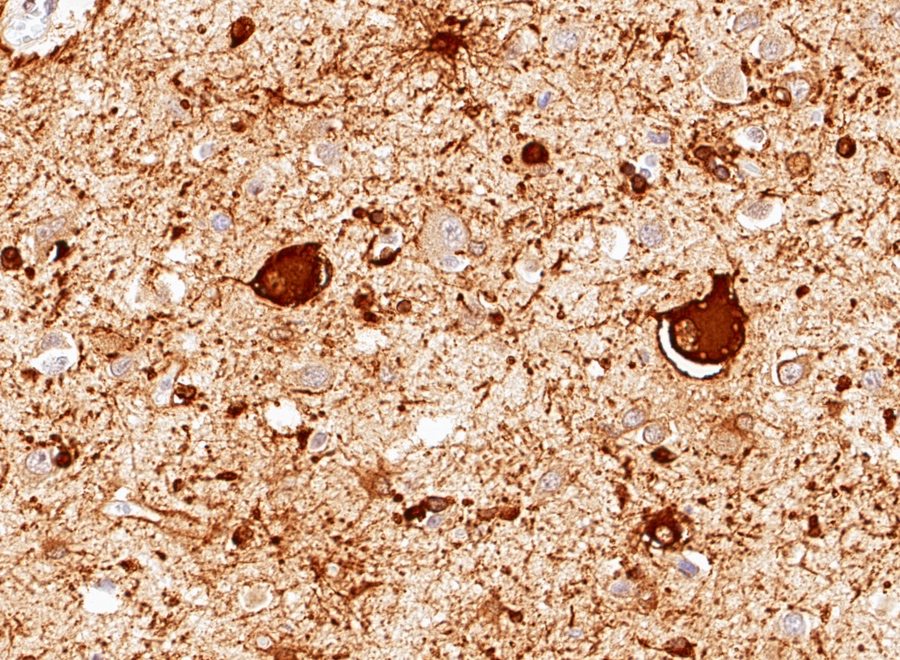
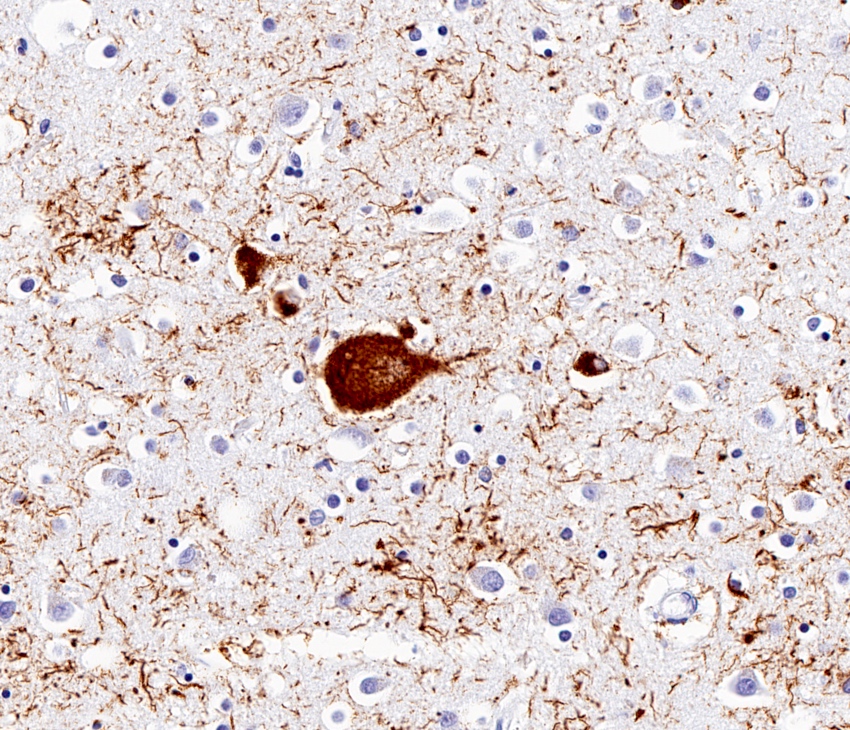
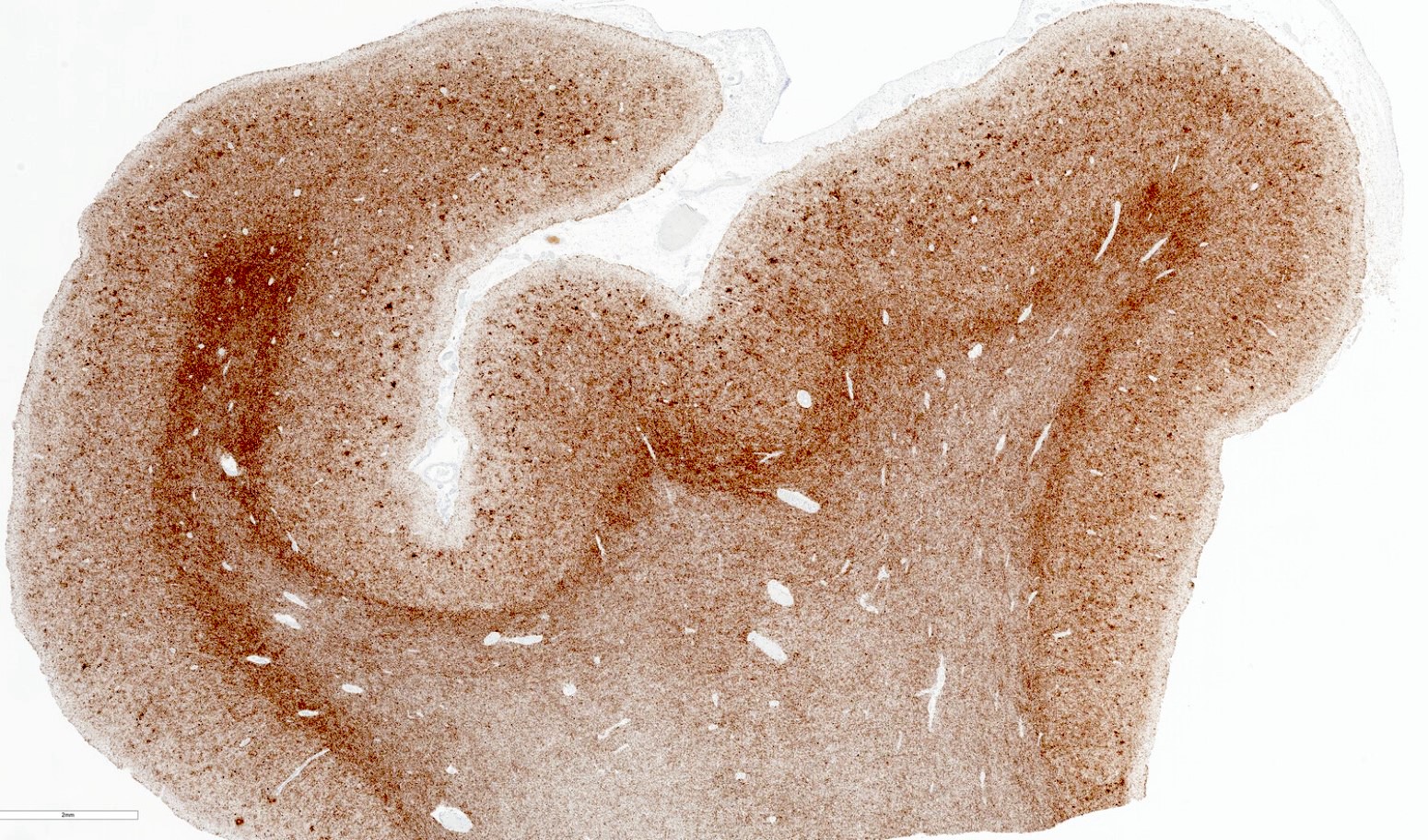
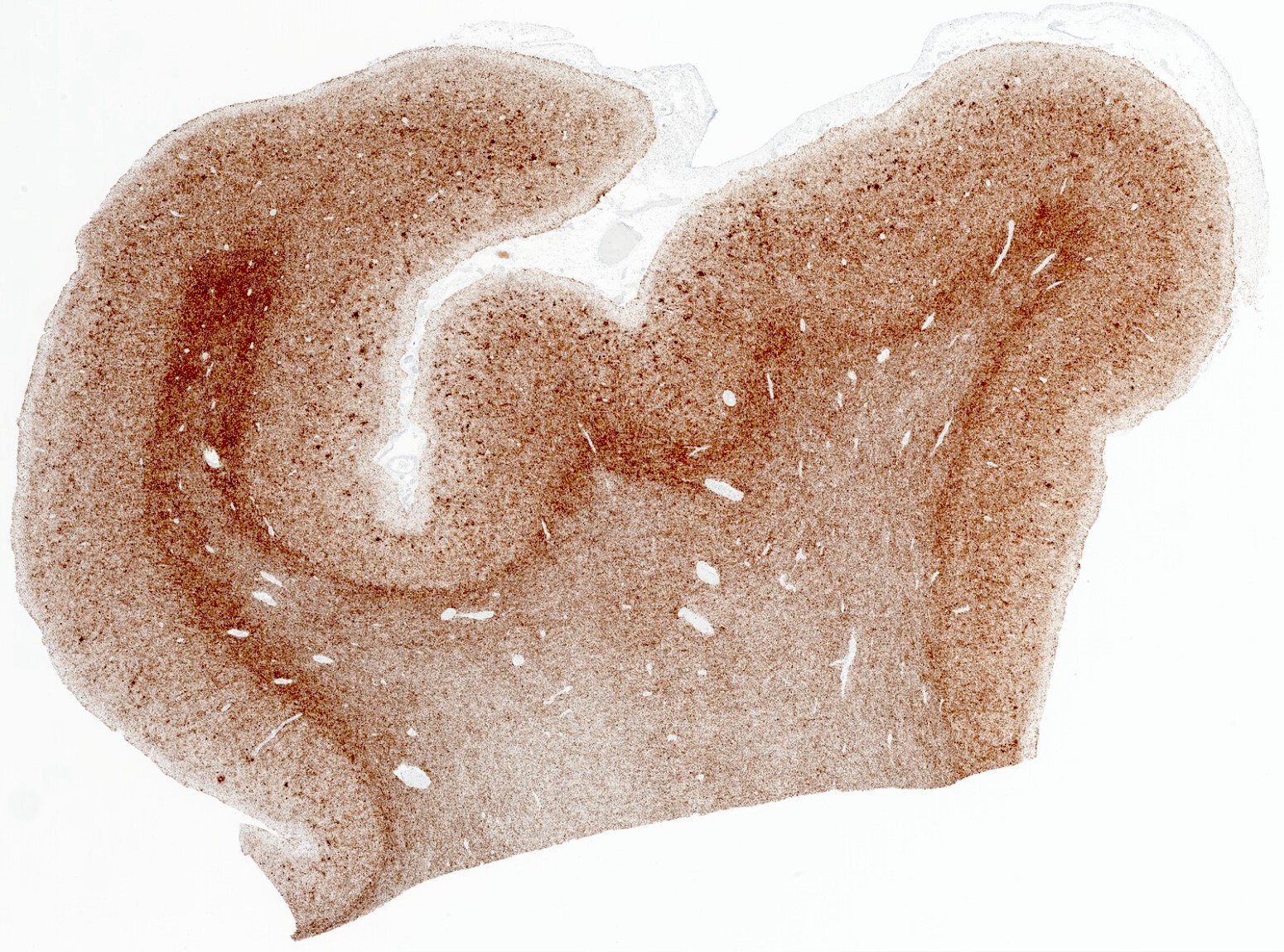
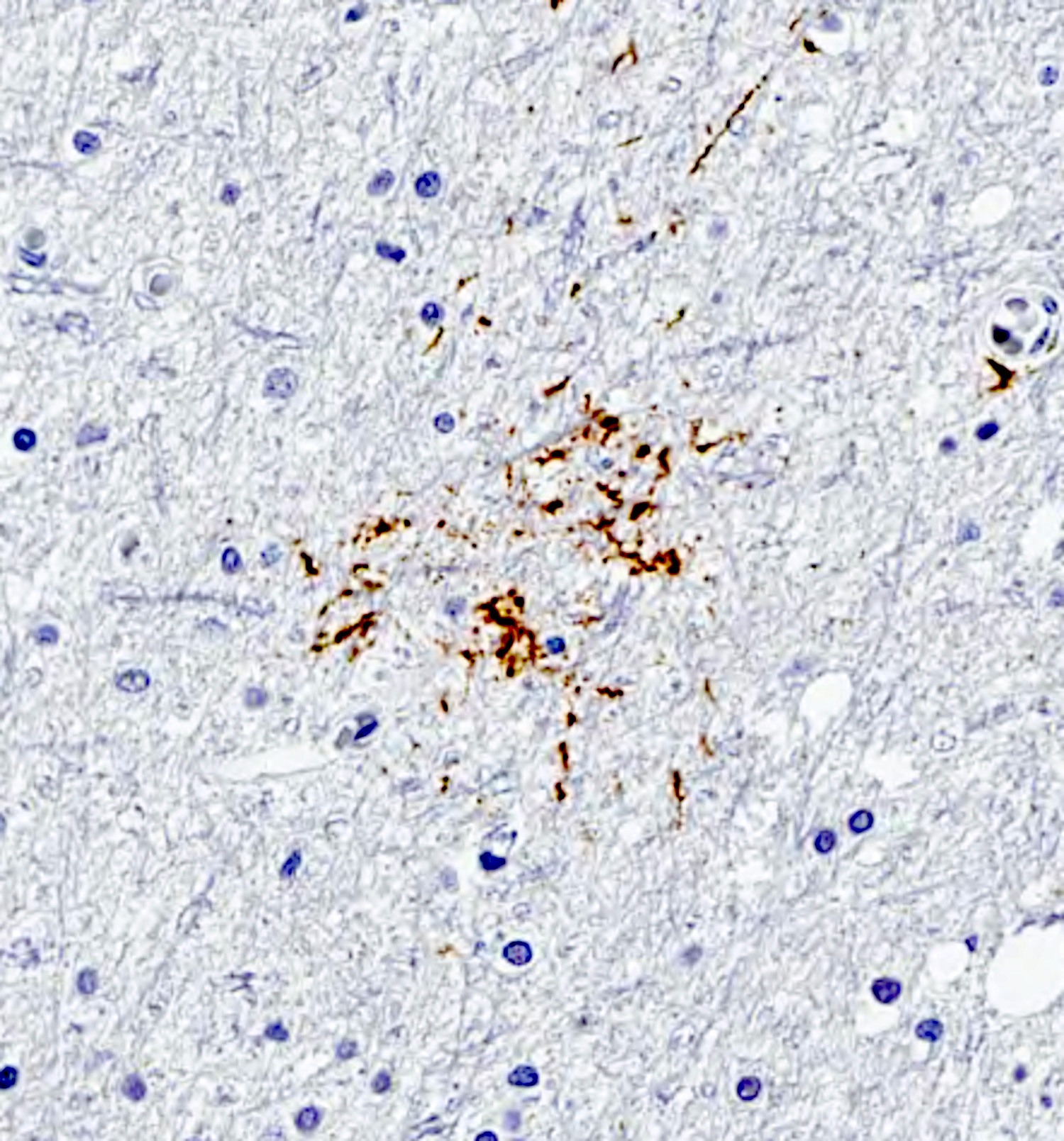
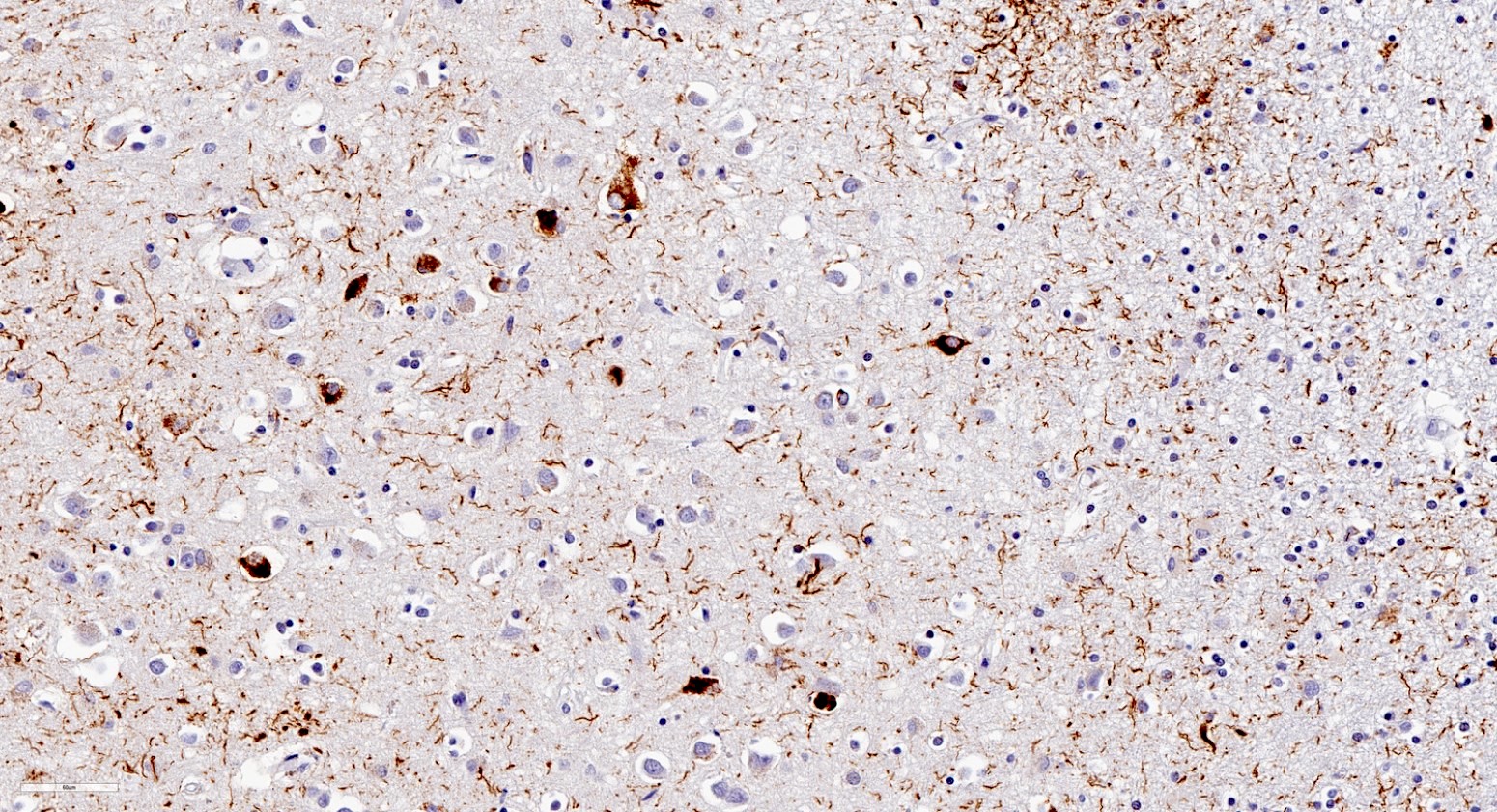
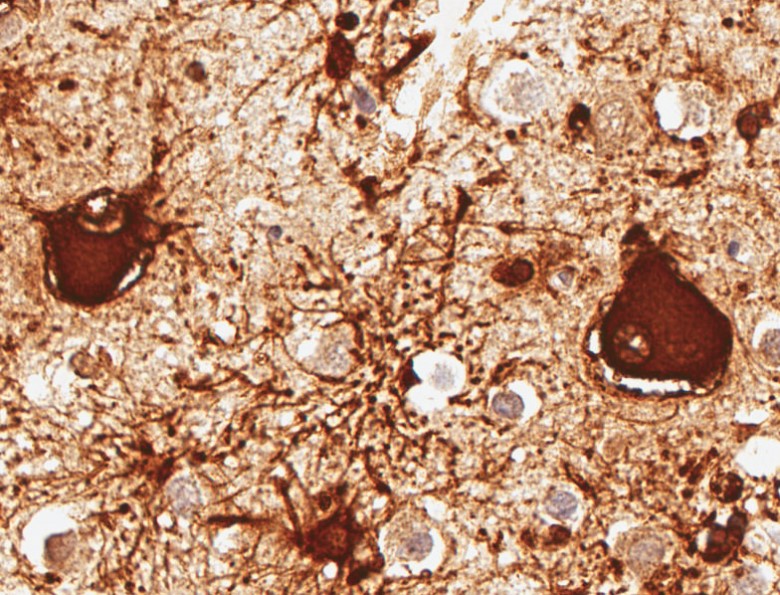
- Astrocytic plaques, which are annular clusters of short and stubby processes forming plaque-like lesions, are found in the cortex and basal ganglia
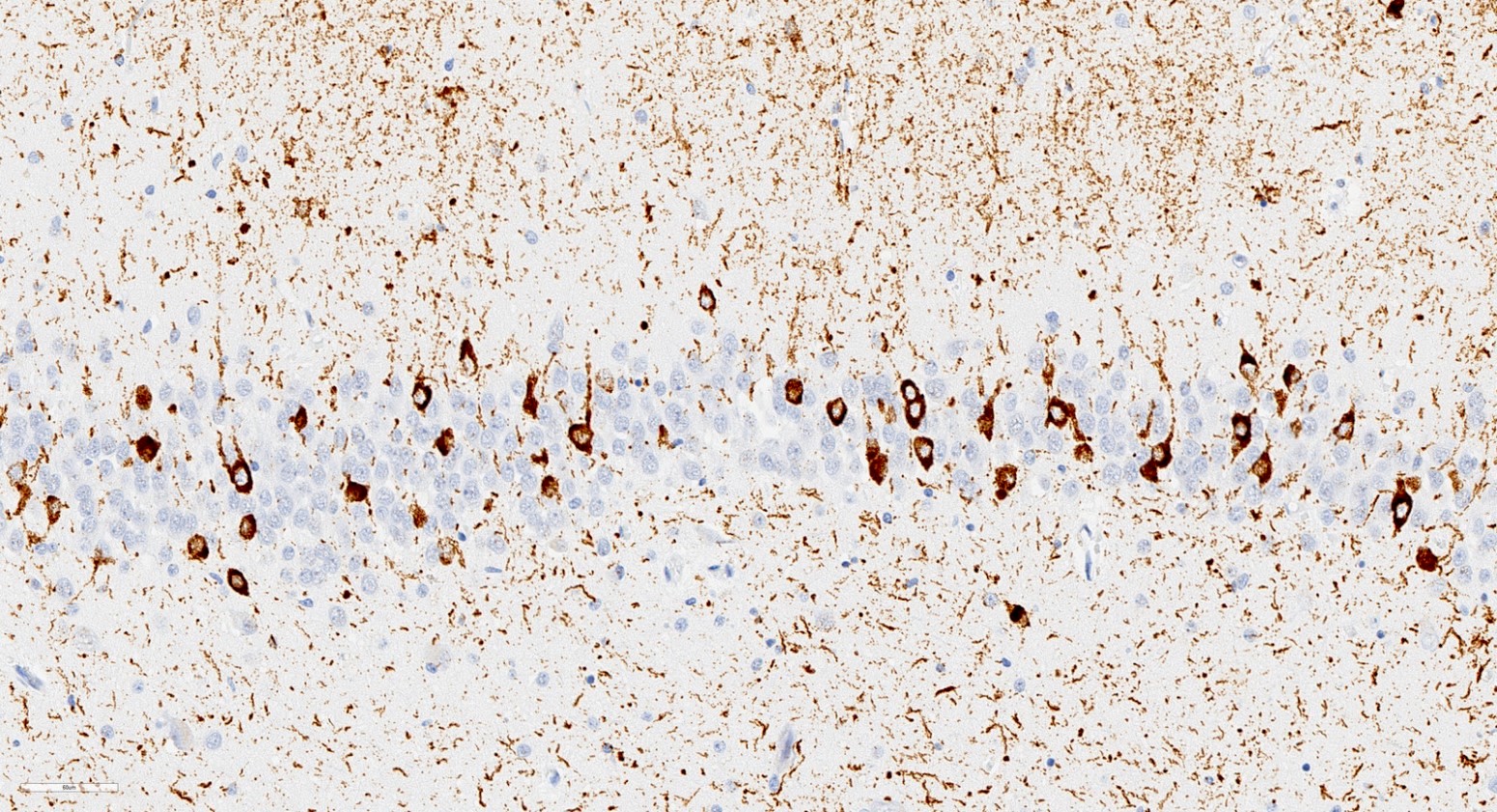
- Ballooned (achromatic) neurons are characterized by swelling of the perikarya and proximal dendrites, along with loss of Nissl substance in pyramidal neurons
- They are immunoreactive for alpha B crystallin (Neuropathol Appl Neurobiol 1992;18:341)
- Neuronal and glial inclusions are present in the cerebral cortical and subcortical gray matter
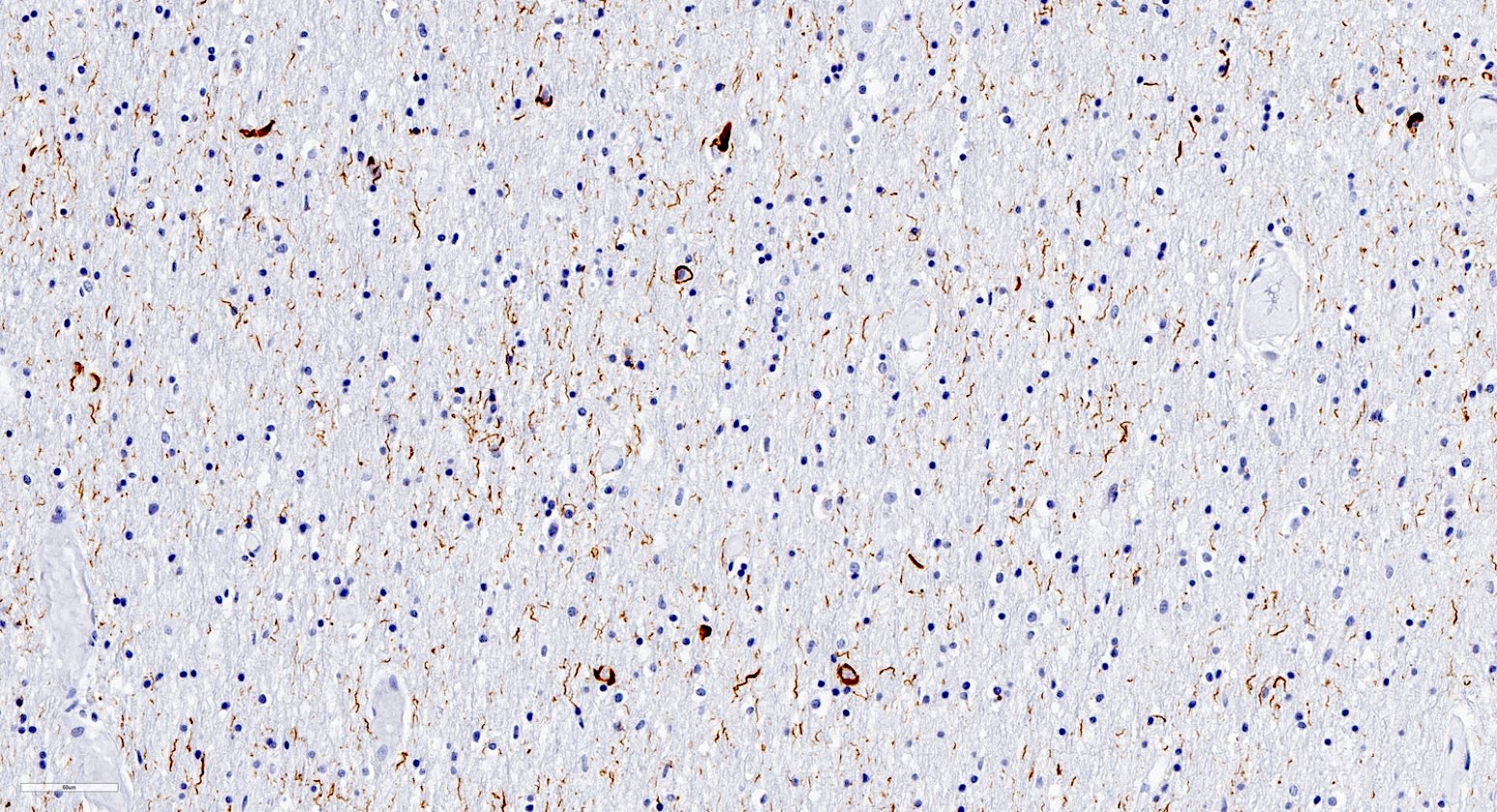
- Neuropil threads and coiled bodies are found in both white and gray matter
- Indistinct boundary between white and gray matter is often observed due to the abundance of neuropil threads in both compartments
- Superficial or laminar spongiosis is seen in the cerebral cortex
- Pattern of tau accumulation in the white matter CBD can be used to differentiate it from progressive nuclear palsy and Alzheimer disease (Acta Neuropathol Commun 2021;9:170)
Microscopic (histologic) images
Contributed by Charles L. White, III, M.D.
Immunofluorescence description
- Thioflavin S fluorescent microscopy does not detect the 4R isoform tau of CBD (Acta Neuropathol 1994;88:379)
Positive stains
- AT8 antibody is the most widely used phospho-tau stain, although it does not discriminate between 3R and 4R isoforms (J Neuropathol Exp Neurol 2002;61:935)
- 4R tau antibody stains tau accumulation in the form of threads, pretangles, tangles, cytoplasmic inclusions, coiled bodies and astrocytic plaques (Nat Rev Neurol 2011;7:263)
- More specific than phospho-tau stain
- p62, ubiquitin: these antibody stains show nonselective immunoreactivity in pathological inclusions of several neurodegenerative disorders, though ubiquitin can be negative in CBD (Acta Neuropathol Commun 2016;4:22, Acta Neuropathol 1994;88:379)
Negative stains
- Amyloid beta antibody staining is negative in astrocytic plaques but may label coexisting Alzheimer pathology
- 3R tau antibody stains should not show aggregates unless other neurodegenerative pathologies, such as Alzheimer disease, are present
- Silver stains do not detect neuronal and glial lesions of CBD (J Neuropathol Exp Neurol 2002;61:935)
- Alpha-synuclein antibody stains should not show additional aggregates unless other neurodegenerative pathologies are present
- TDP-43 antibody stains should not show additional aggregates unless other neurodegenerative pathologies are present
- Thioflavin S fluorescent staining highlights Alzheimer pathology and is typically negative in CBD inclusions
Electron microscopy description
- Electron microscopy assessment is not routinely used for diagnosis of CBD
- Pretangles in CBD are tau positive straight filaments sparsely distributed throughout neuronal cytoplasm and neurites, like Alzheimer disease (AD)
- While AD pretangles exhibit a strong propensity to mature into compact neurofibrillary tangles, CBD tau aggregates may persist as pretangles even at advanced stages (Acta Neuropathol Commun 2014;2:161)
Videos
Neuropathology of tauopathies
Sample pathology report
- Adult brain (1,080 grams), autopsy:
- Histopathological features consistent with corticobasal degeneration (CBD) (see comment)
- Gross description
- Received for examination are the formalin fixed brain and dura mater. External examination of the brain reveals severe frontotemporal gyral atrophy and moderate parietal gyral atrophy.
- Coronal sections through the cerebral hemispheres demonstrate severe hydrocephalus ex vacuo and severe hippocampal atrophy. Cross sections of the brain stem and mid and parasagittal sections of the cerebellum reveal moderate pallor of substantia nigra and locus coeruleus. Gross photographs are taken.
- Microscopic description
- Microscopic sections are prepared from 17 brain regions after fixation, including hippocampus; neocortex from the frontal, temporal, parietal and occipital lobes; supracallosal and pregenual cingulate cortex; amygdala; basal ganglia / nucleus basalis; subthalamic nucleus; brainstem (3 levels); cerebellum; olfactory bulb; and dura mater, using H&E, fluorescent thioflavin S stain (hippocampal and neocortical sections), AT8 phospho-tau immunostains (hippocampal, neocortical and midbrain sections), 3R tau and 4R tau immunostains (hippocampal, frontal neocortical and basal ganglia / nucleus basalis sections) and alpha B crystallin immunostains (neocortical and amygdala sections).
- An H&E stained section of the frontal neocortex demonstrates superficial spongiosis. No neuritic plaques are identified.
- AT8 immunostaining demonstrates pretangles and tangles in the neocortex, entorhinal cortex, dentate gyrus and all cornu ammonis subfields of the hippocampus and substantia nigra. There is diffuse and strong AT8 immunostaining in the underlying white matter of the neocortex, obscuring the gray-white junction and numerous coiled bodies in oligodendroglial cells. There are prominent astrocytic plaques in the neocortex, circular cytoplasmic inclusions in the neurons of the dentate gyrus, tau staining in the white matter and corticobasal bodies in midbrain nuclei. Immunohistochemical staining for 3R tau and 4R tau confirms that the vast majority of neuronal and glial tau immunoreactivity identified by AT8 is attributed to 4R tau. Tau immunoreactive aggregates failed to demonstrate thioflavin S stain positivity. Large alpha B crystallin immunoreactive balloon neurons are scattered throughout the deeper cortical layers of the frontal, temporal and parietal neocortical sections as well as in the amygdala. These findings are all characteristic of corticobasal degeneration (CBD).
- Comment: The neuropathologic findings in this case are diagnostic of corticobasal degeneration (CBD), a rare neurodegenerative disorder characterized by widespread 4R tau accumulation.
Differential diagnosis
- Progressive supranuclear palsy (PSP):
- Sporadic 4 repeat tauopathy with glial and neuronal involvement, similar to CBD
- Clinical and neuropathological features can overlap with CBD; some argue that they should be considered part of the same disease spectrum (Neurology 2001;56:1702, Mov Disord Clin Pract 2018;5:141)
- Midbrain and subthalamic nuclei atrophy are more common than in CBD
- Cortical involvement is less frequent or less pronounced than in CBD
- Characteristic glial pathology is in the form of tufted astrocytes, radial arrangement of thin, long, branching aggregates of tau in proximal processes of astrocytes (Neuropathology 2014;34:555)
- Ballooned neurons are less frequent compared to CBD; when detected, they are usually associated with concurrent argyrophilic grain disease (Acta Neuropathol 2002;104:53)
- Argyrophilic grain disease (AGD):
- Sporadic 4 repeat tauopathy with glial and neuronal involvement, similar to CBD
- Clinical and neuropathological features can overlap with CBD (Brain 2008;131:1416)
- Pathology is mainly limited to medial temporal lobe structures including the amygdala, hippocampus and entorhinal cortex (Neuropathol Appl Neurobiol 1989;15:13)
- Characteristic pathology is the presence of argyrophilic grains, tau immunoreactive, spindle shaped, rod-like, button-like or round bodies in the neuropil (Brain 2008;131:1416)
- Ballooned neurons, typically found in amygdala (Neurosci Lett 1998;246:165)
- Globular glial tauopathy (GGT):
- Sporadic 4 repeat tauopathy with only glial involvement (Acta Neuropathol 2013;126:537)
- Clinical picture of a frontotemporal dementia syndrome and asymmetric brain atrophy may resemble CBD (Eur J Neurol 2023;30:321)
- Characterized by globular inclusions in both oligodendrocytes and astrocytes but not in neurons (Psychiatr Clin North Am 2020;43:331)
- Astrocytic plaques are not seen (Acta Neuropathol 2013;126:537)
- Frontotemporal lobar degeneration (FTLD, tau-):
- Group of disorders with frontotemporal atrophy and frontotemporal dementia clinical syndrome
- Subclassified based on the type of proteinopathy (Psychiatr Clin North Am 2020;43:331)
- TAR DNA binding protein 43 (TDP-43) related FTLD: tau-, TDP-43+ inclusions
- FTLD fused in sarcoma gene (FUS): tau-, ubiquitin+, p62+ and FUS+ inclusions
- Frontotemporal dementia with Parkinsonism linked to chromosome 17 (FTDP-17):
- Autosomal dominant inherited disorder usually caused by mutations in the MAPT gene, which is located on chromosome 17 (Folia Neuropathol 2005;43:258)
- Clinical and neuropathological features can overlap with CBD (Folia Neuropathol 2005;43:258)
- Positive family history and earlier age of onset (average of 45 years) (J Hum Genet 2015;60:281)
- Alzheimer disease (AD):
- Progressive dementia characterized by amyloid plaques and neurofibrillary tangles (Alzheimers Dement 2012;8:1)
- Clinical features may overlap with CBD; approximately 1 in 4 clinical CBS cases show postmortem AD pathology instead of CBD (Brain 2010;133:2045)
- Both 3 repeat and 4 repeat tau isoforms are present (Int J Mol Sci 2022;23:12841)
- Much more prevalent than CBD (Nat Rev Dis Primers 2015;1:15056, J Neurol 2023;270:4451)
- Pick disease (PiD):
- Sporadic 3 repeat tauopathy with neuronal and glial involvement (Ann Neurol 2002;51:730)
- Clinical features can overlap with CBD (Neurology 1997;48:119)
- Atrophy spares the pre and postcentral gyri (Neurology 2001;56:S16)
- Characteristic pathology consists of round cytoplasmic neuronal tau inclusions called Pick bodies (Handb Clin Neurol 2008;89:415)
- Alpha synucleinopathies (Lewy body dementia, Parkinson disease, multiple system atrophy, etc.):
- Alpha-synuclein+, tau- aggregates
- Cortical atrophy is not as pronounced
- Atrophy of the cerebellum or putamen (multiple system atrophy)
Practice question #1
Practice answer #1
B. Corticobasal degeneration. These are alpha B crystallin immunoreactive ballooned (achromatic) neurons, which are generally seen in the third, fifth and sixth cortical layers and are considered an important histological feature of CBD. Answers A and D are incorrect because balloon cells are not characteristic for Alzheimer disease or Pick disease, although they can occasionally be seen in these entities. Answer C is incorrect because balloon neurons are not usually seen in Lewy body disease.
Comment Here
Reference: Corticobasal degeneration
Comment Here
Reference: Corticobasal degeneration
Practice question #2
Practice answer #2
A. 4R tau. Astrocytic plaques are a distinct annular array of 4R tau immunoreactive processes that are reminiscent of the senile plaques of Alzheimer disease but lack amyloid beta immunoreactivity, differentiating them from Alzheimer disease associated senile plaques. They are also positive for GFAP, indicating a glial, rather than a neuronal, origin (Neuropathology 2014;34:555). Answer D is incorrect because TDP-43 is negative in CBD but positive in other neurodegenerative diseases, such as frontotemporal lobar degeneration with TDP-43 proteinopathy (FTLD TDP), amyotrophic lateral sclerosis and limbic predominant age related TDP-43 encephalopathy (LATE NC). Answer C incorrect because senile plaques of Alzheimer disease show co-occurring immunoreactivity for both tau and amyloid beta but astrocytic plaques of CBD are positive only for tau. Answer B is incorrect because CBD is a tauopathy, not a synucleinopathy like Lewy body disease or multiple systemic atrophy.
Comment Here
Reference: Corticobasal degeneration
Comment Here
Reference: Corticobasal degeneration