Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Videos | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2 | Practice question #3 | Practice answer #3Cite this page: Ludwig KS, Gonzalez RS. Actinomycosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/colonactinomycosis.html. Accessed July 22nd, 2025.
Definition / general
- Intra-abdominal infection caused by Actinomyces spp., sometimes mimicking colon cancer
Essential features
- Rare, Gram positive bacterial infection involving the abdomen
- Symptoms and imaging often resemble malignancy
- Treatment is long term antibiotics but surgery may be necessary
Terminology
- Etymology: actin = ray / beam-like + mycosis = fungal
- Mycosis is a misnomer as the pathogen was previously thought to be fungus due to its branching, filamentous nature
ICD coding
- ICD-10: A42.8 - other forms of actinomycosis
Epidemiology
- Overall incidence of actinomycosis is 1:300,000
- Of these, 20% are abdominal cases
- More common between ages 20 and 60 years
- More common in men (M:F = 3:1)
- Risk factors
- Prior injury, such as trauma or surgery at the site
- Foreign device (e.g., intrauterine device [IUD])
- Immunosuppression (e.g., chemotherapy, human immunodeficiency virus [HIV], diabetes) (Cureus 2022;14:e23954)
Sites
- Actinomycosis most commonly occurs in cervicofacial, thoracic or genitourinary sites or as a disseminated disease (BMC Surg 2018;18:51)
- In the abdomen, most commonly found in the appendix, ileocecum and colon
- May involve pelvic organs or rarely liver
Pathophysiology
- Lesion / trauma / surgery → mucosal damage with defective mucosal barrier → infiltration of preexisting microorganism (infection) → inflammation, granulation, fibrosis, abscess → pseudotumor formation
Etiology
- Actinomyces spp., most commonly Actinomyces israelii
- Presence as normal gut flora combined with mucosal damage leads to pathogenic process
- Often leads to coinfection with other microorganisms (BMC Surg 2018;18:51)
Clinical features
- Clinical picture ranges from chronic mild to severe subacute presentation with nonspecific constitutional symptoms, including abdominal pain, palpable abdominal mass, constipation / diarrhea, low grade fever, anorexia / weight loss and night sweats
- Complications include bowel obstruction / perforation, impingement / invasion of other organs
Diagnosis
- Colonoscopy: possible stenosis or intraluminal lesion
- Percutaneous needle biopsy to obtain tissue for culture (BMC Surg 2018;18:51)
- Gold standard
- May grow other microorganisms, as infection may be polymicrobial
- Cultures are often falsely negative due to the anaerobic and slow growing nature of Actinomyces (J Surg Case Rep 2024;2024:rjad697)
- Histology can confirm the presence of Actinomyces microorganisms
- Intraoperative frozen section can exclude malignancy, preventing any unnecessary surgery (BMC Surg 2018;18:51)
Laboratory
- Leukocytosis, anemia, elevated inflammatory markers
Radiology description
- Ultrasound may show abdominal mass
- Contrast computed tomography (CT) may show masses and thickening of the colonic wall resembling colitis and mesenteritis
Prognostic factors
- Prognosis is excellent following treatment
Case reports
- 54 year old woman with abdominal pain, constipation, weight loss (Middle East J Dig Dis 2020;12:126)
- 54 year old woman with incidental tumors of colon, liver and abdominal wall (Cureus 2023;15:e50215)
- 55 year old woman with palpable abdominal mass (BMC Surg 2018;18:51)
- 58 year old woman with severe abdominal pain and palpable abdominal mass (J Surg Case Rep 2024;2024:rjad697)
Treatment
- Medical management (long term antibiotics) is sufficient for most cases
- Many patients will undergo surgery due to equivocal / unclear preoperative diagnosis, then start antibiotics
- Recommendation is to start empirical antibiotics preoperatively and then, after actinomycosis diagnosis, give postoperative long term beta lactam antibiotics (penicillin G or amoxicillin)
- Alternatively, can give ceftazidime and metronidazole
- Combination of surgery with antibiotics reduces the duration of antibiotics; however, antibiotics may be continued to reduce chance of recurrence (IDCases 2021;25:e01252)
Gross description
- Involved segment of colon may show stenosis, mural thickening, abscess formation and serosal adhesions
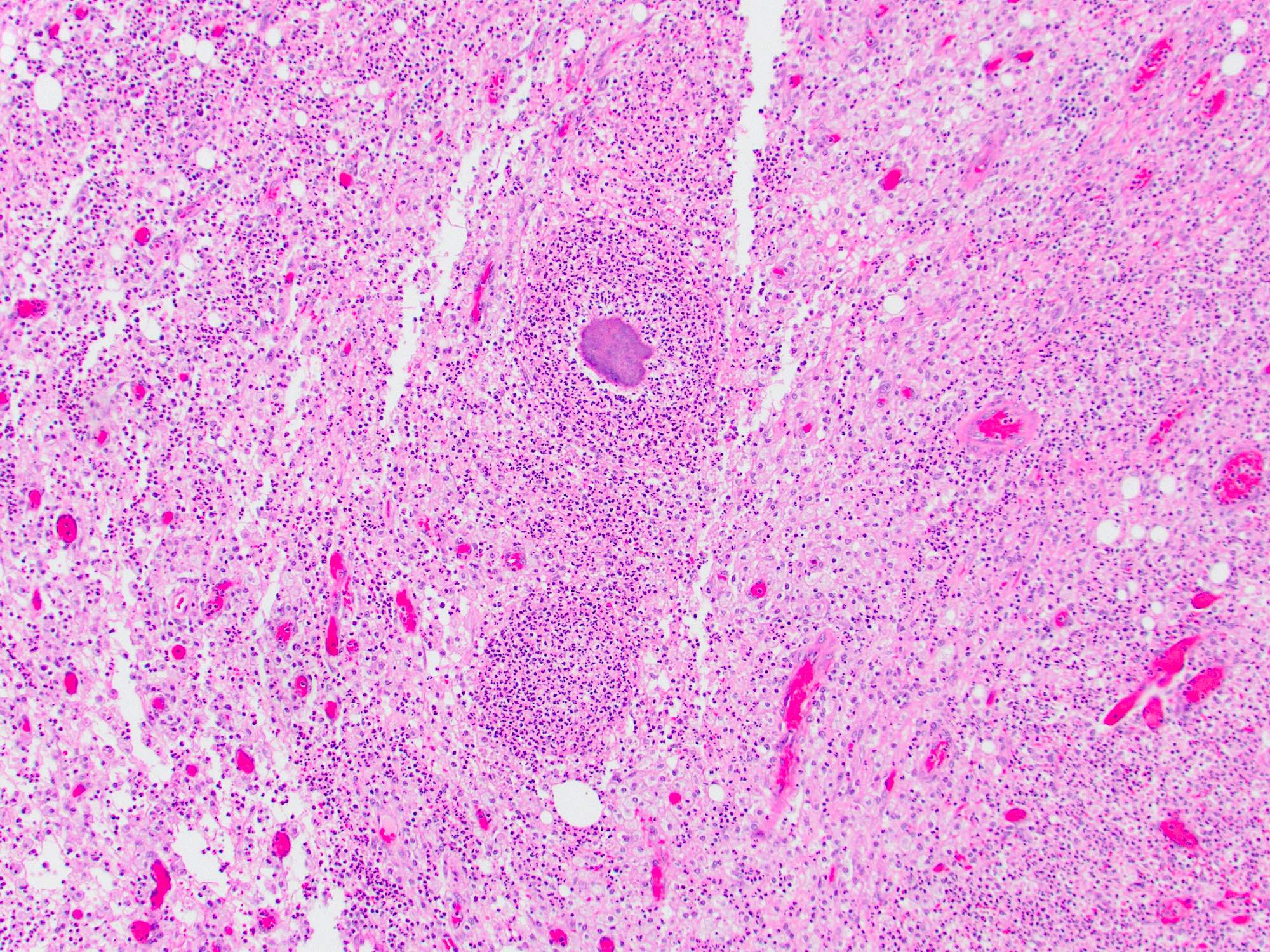
Microscopic (histologic) description
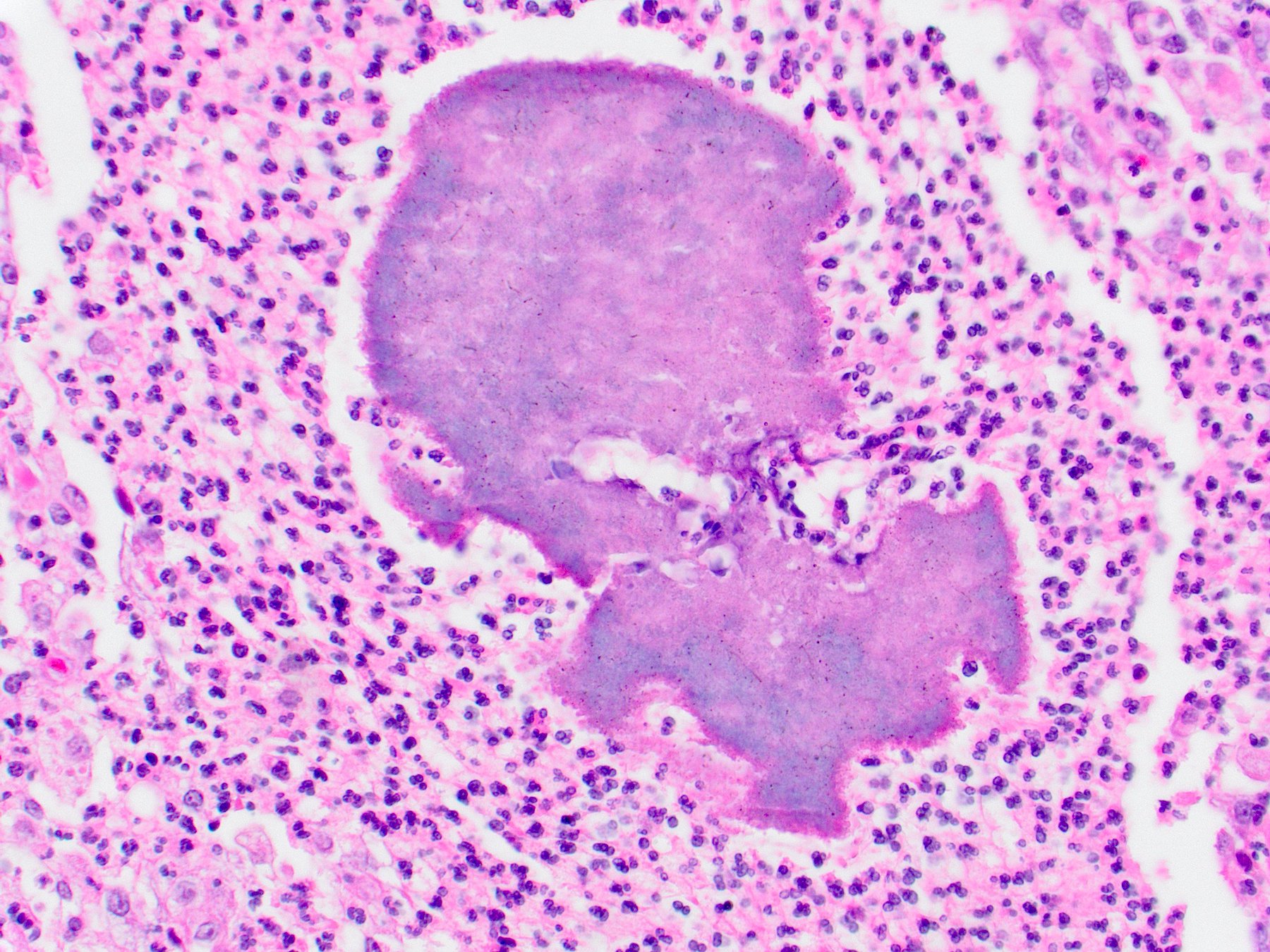
- Actinomyces visible as slender, filamentous, fungal-like organisms
- These are usually aggregated into sulfur granules
- Mural organisms intermixed with neutrophils, plasma cells, eosinophils and lymphocytes in a necrotic background
- Multinucleated giant cells and noncaseating granulomas may also be present
- Local lymph nodes may show reactive change
- References: Middle East J Dig Dis 2015;7:41, World J Gastrointest Surg 2009;1:62
Microscopic (histologic) images
Positive stains
- Gram stain
- GMS (nonfungal filamentous bacteria)
Negative stains
Videos
Colonic actinomycosis
Sample pathology report
- Colon, right hemicolectomy:
- Colon with extensive mural necrosis and abscess formation
- Aggregates of filamentous organisms, consistent with Actinomyces, are present within abscesses
- Negative for malignancy
Differential diagnosis
- Colorectal adenocarcinoma:
- Actinomyces may clinically mimic malignancy due to mass formation within the colon
- Tissue sampling should readily confirm diagnosis or at least rule out adenocarcinoma
- Diverticulitis:
- Mural inflammatory process may be similar in severe cases of perforated diverticulitis
- Sulfur granules are not seen
- Pulse granuloma:
- May also form a prominent inflammatory mass in the colon wall, simulating malignancy
- Sulfur granules are not seen
Practice question #1
A patient presents with abdominal pain and is found to have mural thickening of the colon. Symptoms persist and the colon is resected. Based on the histologic image above, which of the following is the most likely diagnosis?
- Actinomyces infection
- Inflammatory bowel disease
- Schistosoma infection
- Yersinia infection
Practice answer #1
A. Actinomyces infection. The presence of sulfur granules (aggregates of filamentous bacteria) in the wall of the colon indicates Actinomyces as the culprit. Answer C is incorrect because Schistosoma infection would show eggs or worms. Answer D is incorrect because Yersinia infection would not show any visible microorganisms. Answer B is incorrect because inflammatory bowel disease would also not demonstrate visible organisms.
Comment Here
Reference: Actinomycosis
Comment Here
Reference: Actinomycosis
Practice question #2
Which of the following is true about Actinomyces infection of the colon?
- It can be treated with antibiotics
- It is a risk factor for colonic adenocarcinoma
- It is asymptomatic
- It is the most common site for Actinomyces infection
Practice answer #2
A. It can be treated with antibiotics. While colonic actinomycosis may first be diagnosed on a resection specimen, it can be treated with antibiotics if identified earlier. Answer B is incorrect because Actinomyces is not a risk factor for development of colon cancer, though it can mimic it clinically. Answer C is incorrect because infection leads to symptoms such as abdominal pain and fever. Answer D is incorrect because Actinomyces infection is most common in cervicofacial sites.
Comment Here
Reference: Actinomycosis
Comment Here
Reference: Actinomycosis
Practice question #3
What is the pathophysiological process of developing actinomycosis in the colon?
- It is a contagious bacterial gastroenteritis, where a virulent microorganism transmitted by the fecal - oral route infects and infiltrates the intestinal wall
- It is a fungal overgrowth commonly seen after antibiotic use
- It is iatrogenic and a risk of surgical procedures that introduce the bacteria into the gut
- It results from normal gut flora that has become pathogenic due to breach of defective mucosal barriers
Practice answer #3
D. It results from normal gut flora that has become pathogenic due to breach of defective mucosal barriers. Actinomyces is found as a commensal organism in the gut but can lead to opportunistic infection once there is any damage to the gut mucosa, allowing it to infiltrate the gut wall. Answer A is incorrect because actinomycosis is not contagious and does not spread to humans from animals or other humans. Answer B is incorrect because although Actinomyces resembles fungi, it is a bacterium and is treated with antibiotics. Answer C is incorrect because Actinomyces does not live on fomites and thus does not spread via surgical contamination.
Comment Here
Reference: Actinomycosis
Comment Here
Reference: Actinomycosis