Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Videos | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: McCloskey A, Hutchings D. Mucosal prolapse polyp. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/colonmucosalprolapsepolyp.html. Accessed September 25th, 2025.
Definition / general
- Nonneoplastic polyp / lesion
- May be seen in association with diverticular disease or polypoid phase of solitary rectal ulcer syndrome (SRUS)
Essential features
- Can occur anywhere in the colon but is most common in the rectosigmoid
- May be seen in association with diverticular disease or polypoid phase of solitary rectal ulcer syndrome (SRUS)
- Characterized by fibromuscular obliteration of lamina propria and splayed hypertrophic muscularis mucosae (Diagnostics (Basel) 2022;12:966)
- Crypts may be distorted and elongated or show hyperplastic and serrated changes
- Secondary changes, including surface erosion, inflammation, vascular ectasia and congestion may be present
Terminology
- Prolapsing mucosal polyp
- Mucosal prolapse changes
- Mucosal prolapse syndrome (MPS)
- Solitary rectal ulcer syndrome (SRUS)
Epidemiology
- M > F (3:1) (Cureus 2023;15:e37958)
- Fourth to sixth decades of life (GE Port J Gastroenterol 2016;23:214)
- Risk factors
- Diverticular disease
- Repeated colonic spastic contractions
- Excessive straining
Sites
- Most common in rectum and sigmoid colon but may be found throughout the colon
Pathophysiology
- Unknown, although postulated that spastic contraction of the bowel wall leads to mucosal redundancy (Am J Surg Pathol 1991;15:871)
Etiology
- Often but not always associated with diverticular disease (Am J Surg Pathol 1991;15:871)
- Constipation / repetitive straining
- Solitary rectal ulcer syndrome (SRUS)
Clinical features
- Rectal bleeding, abdominal pain and constipation
- Colonoscopy examination
- Solitary or multiple polyps or elevated patches with smooth and bright red colored surface
- Sharply contrasted bright red color due to hyperemia or congestion with surface smoothness devoid of coarse lobulation and irregular nodularity, which are common features in neoplastic or dysplastic lesions (Intern Med 2007;46:1701)
Diagnosis
- Clinical history including rectal bleeding, abdominal pain and constipation
- Diagnosis is made on histological examination
Radiology description
- Abdominal computed tomography (CT): may show segmental wall thickening with layered pattern wall enhancement (Intern Med 2007;46:1701)
- Endoscopic ultrasound (EUS) shows 3 patterns (Dig Liver Dis 2021;53:427)
- Polypoid / nodular lesion with thickening of mucosa
- Ulcerative lesions with diffuse thickening of mucosa / submucosa and loss of architecture
- Flat lesions with thickening of the muscularis propria
Radiology images
Prognostic factors
- Overall favorable prognosis
Case reports
- 15 year old boy with mucosal prolapse polyps mimicking Peutz-Jeghers syndrome (JPGN Rep 2024;5:170)
- 18 year old man and 62 year old woman with rectal polyposis in mucosal prolapse syndrome (Diagnostics (Basel) 2022;12:966)
- 60 year old man with rectal polypoid lesion with nodular surface (Intest Res 2019;17:281)
- 65 year old man with incidentally discovered mucosal prolapse polyps during colorectal cancer screening (Cureus 2023;15:e37958)
Treatment
- Endoscopic biopsy or removal often performed for diagnosis
- Larger symptomatic lesions may require additional endoscopic (e.g., argon plasma coagulation or endoscopic resection) or surgical therapy (ACG Case Rep J 2021;8:e00563)
Clinical images
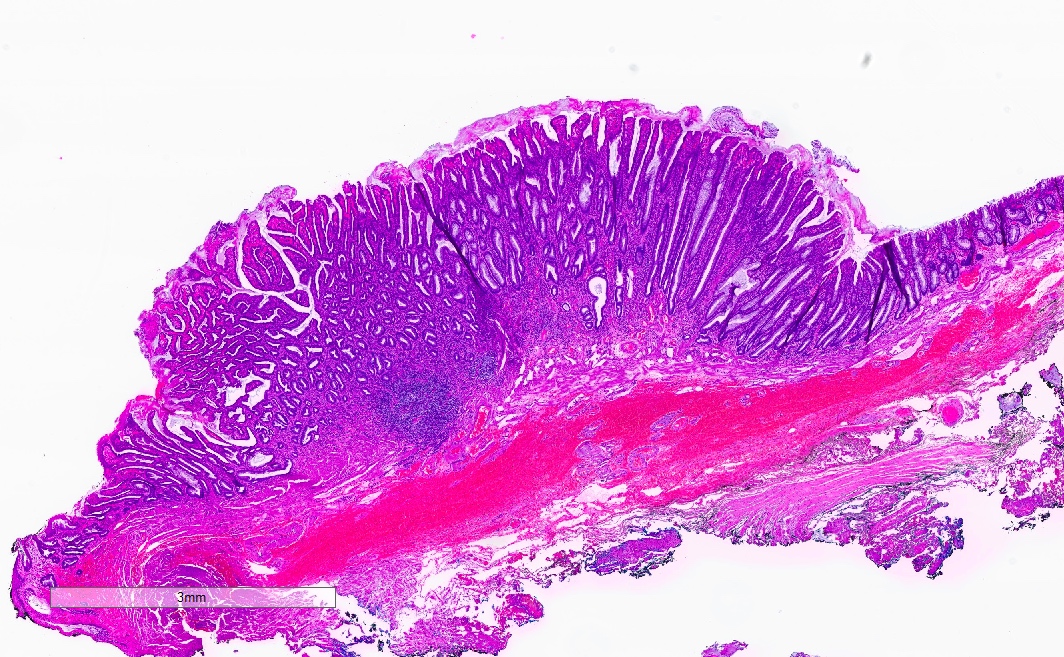
Gross description
- May be polypoid, flat, sessile or pedunculated
- Surface may appear hyperemic with petechiae or ulcerated
Gross images
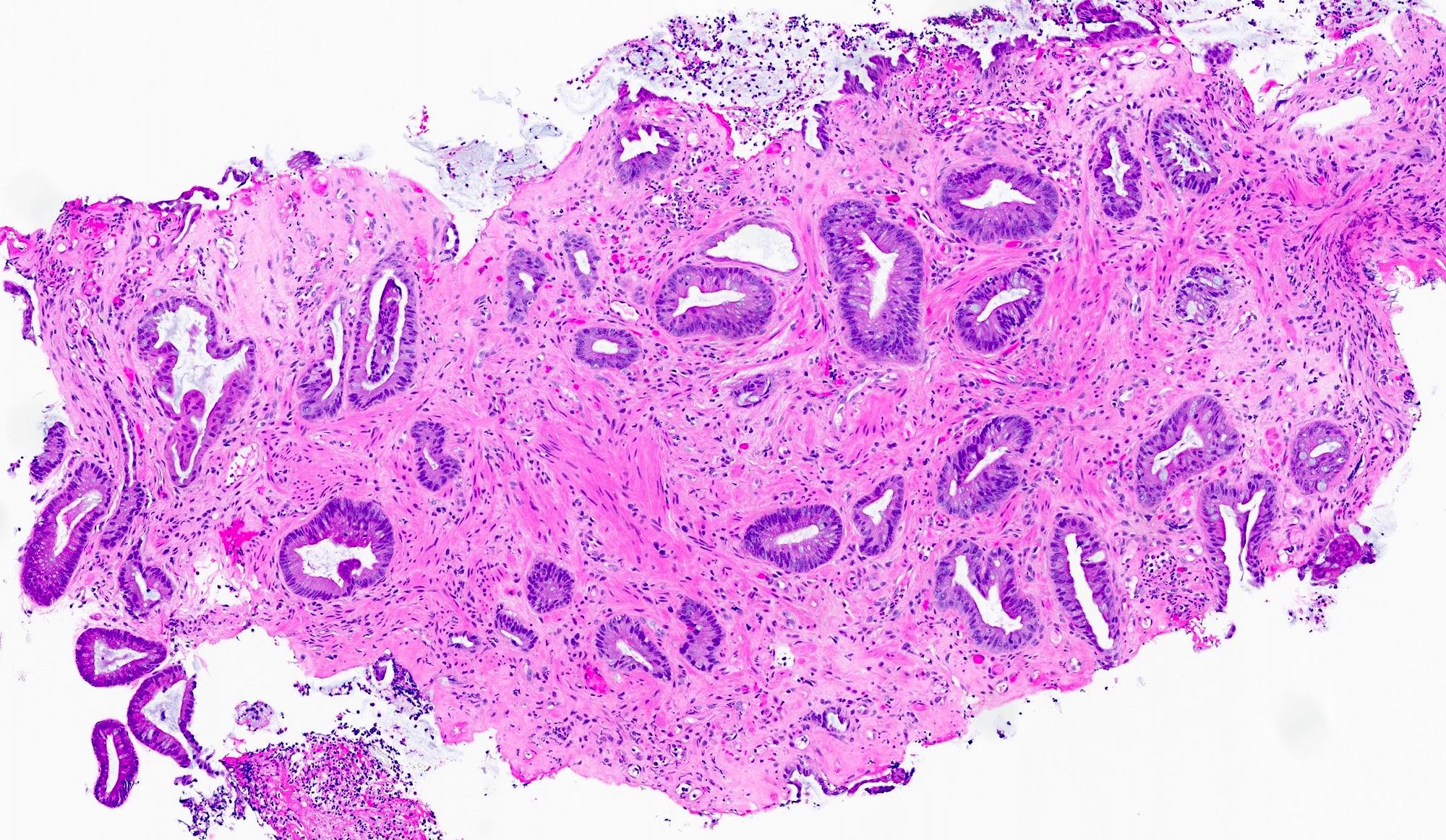
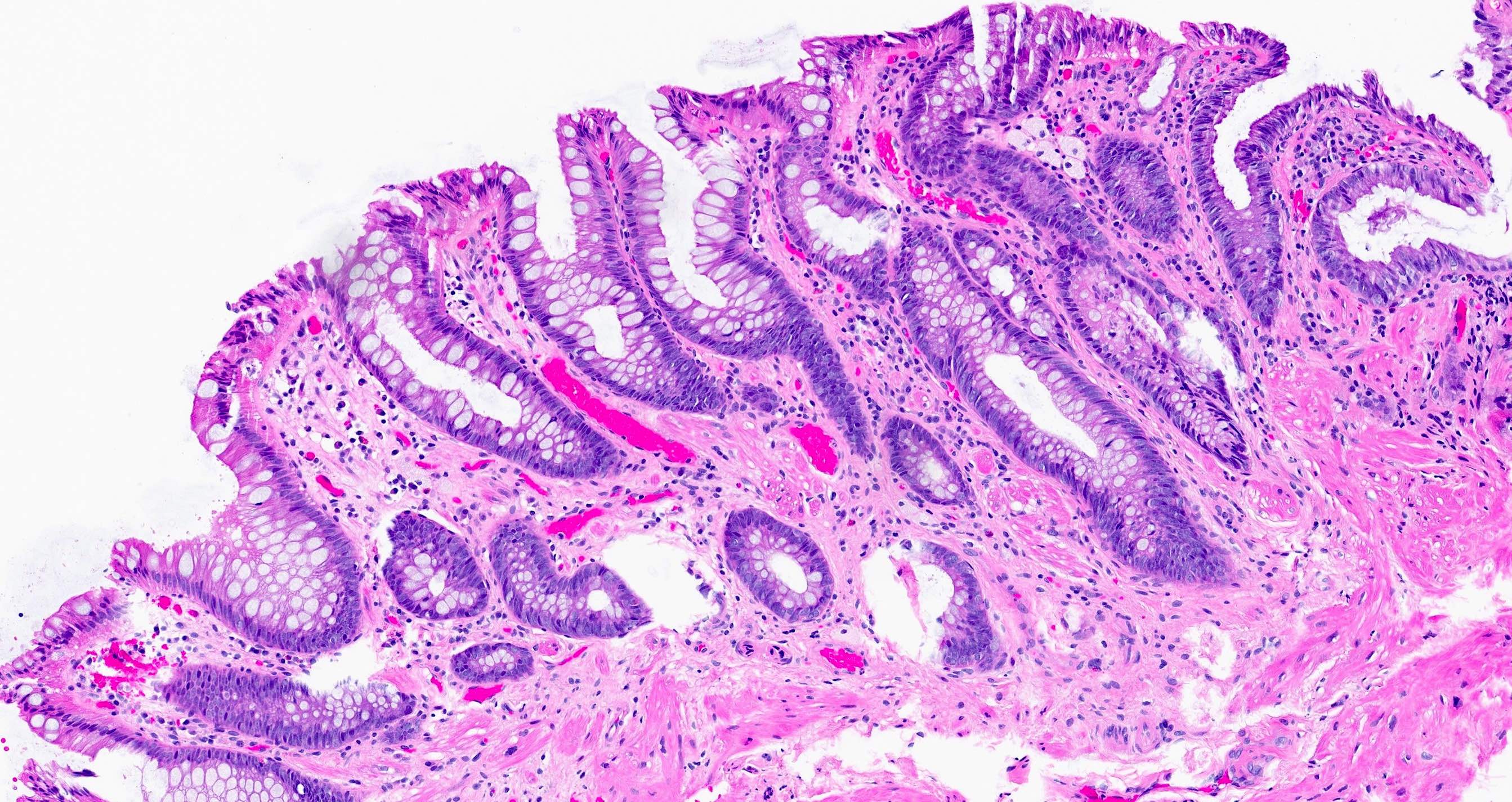
Microscopic (histologic) description
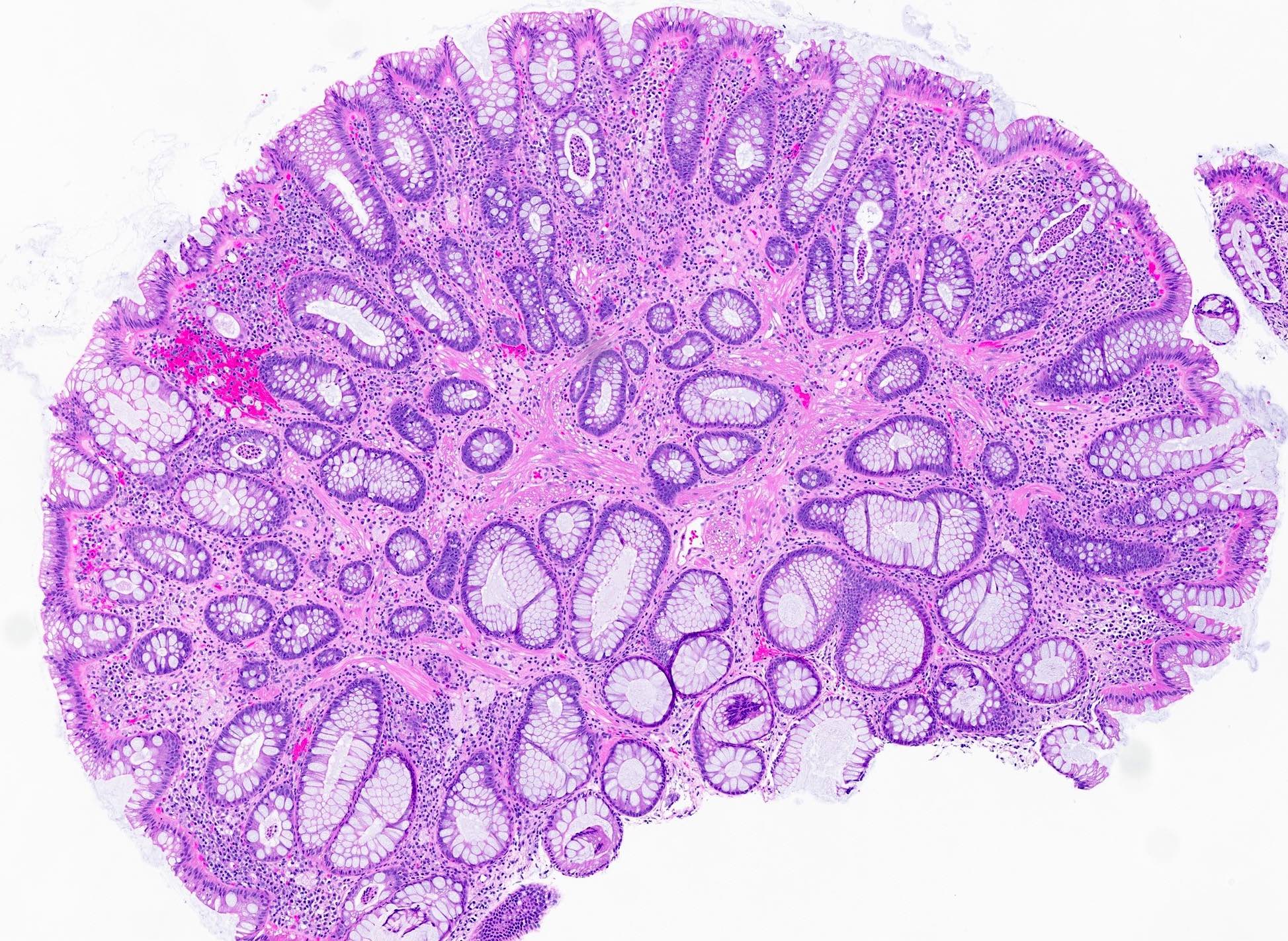
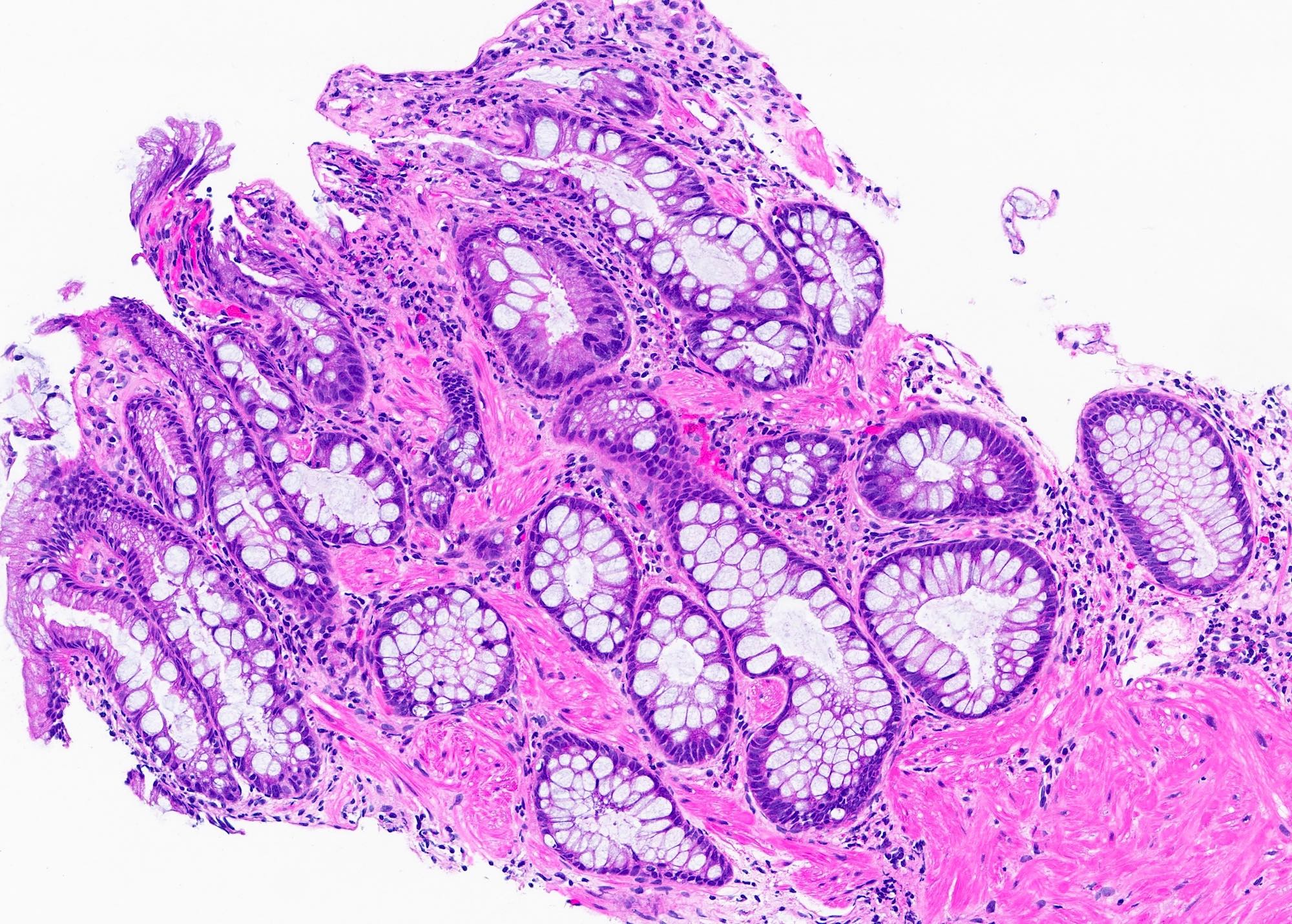
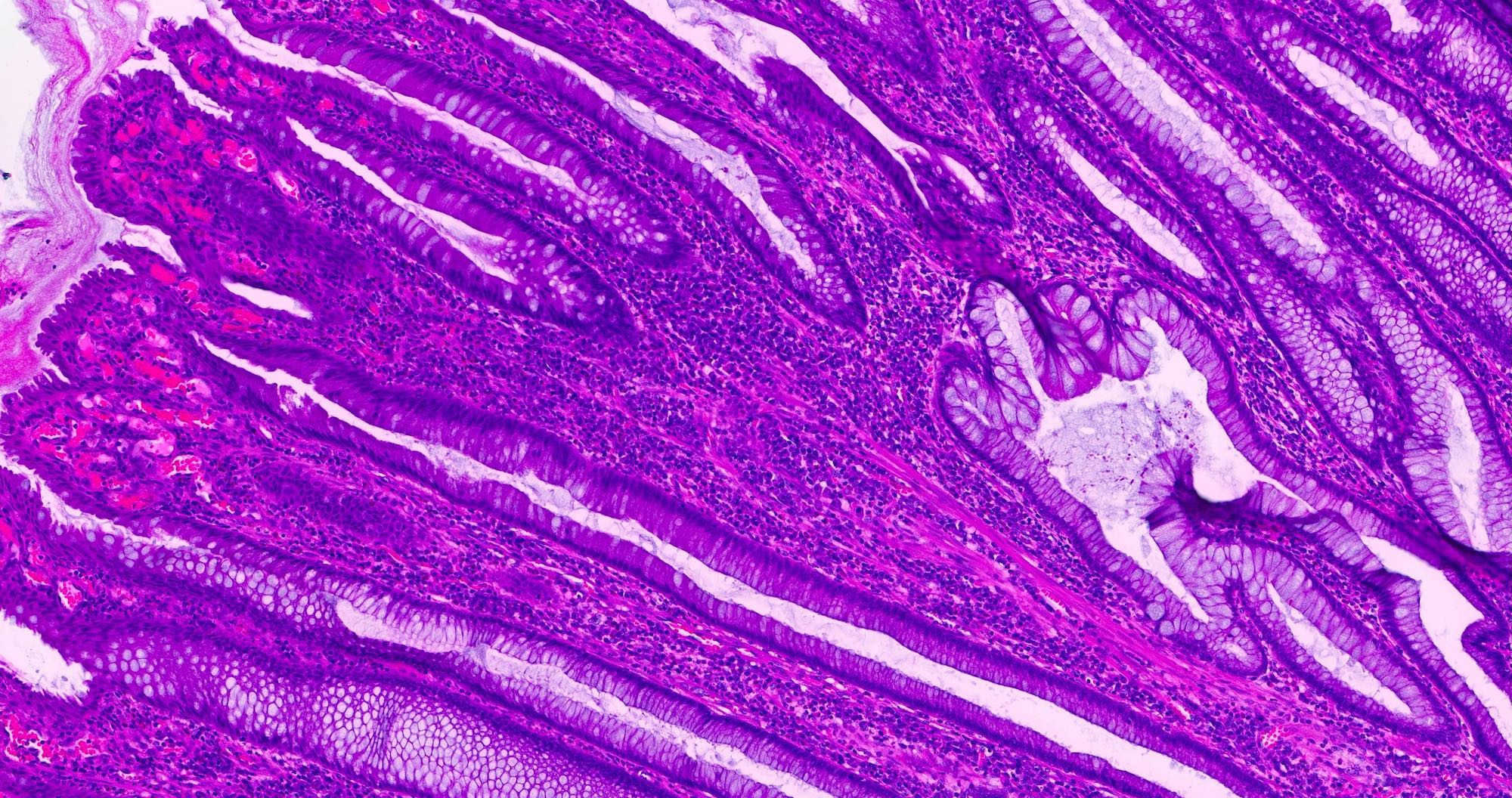
- Thickening and disruption of the muscularis mucosae and muscularization (splaying of muscularis propria between crypts) of the lamina propria
- Crypt elongation distortion and branching
- Hyperplastic and serrated changes, including crypt branching, hypermucinous appearance of the epithelium (GE Port J Gastroenterol 2016;23:214)
- Secondary changes may include surface erosion, inflammation, hemorrhage, vascular congestion and ectasia (J Clin Pathol 2009;62:1034)
- Diamond shaped crypts and mucosal elastin (Histopathology 1990;17:129)
Microscopic (histologic) images
Videos
Mucosal prolapse polyp
Sample pathology report
- Sigmoid colon polyp, biopsy:
- Mucosal prolapse polyp
Differential diagnosis
- Hyperplastic polyp:
- Lack of splayed muscularis mucosae between crypts
- Serrated architecture with a sawtooth appearance, with serrations generally limited to the upper half of the crypts
- Neoplastic polyp:
- Presence of cytologic dysplasia
- Inflammatory polyp:
- Lacks thickening and splaying of muscularis propria between crypts
- Sessile serrated lesion / polyp / adenoma:
- Serrated crypts with dilatation or branching extending to crypt bases
- Peutz-Jeghers polyp:
- Peutz-Jeghers polyps contain large arborizing bundles of smooth muscle separating lobules of epithelium, whereas smooth muscle fibers in mucosal prolapse are thinner, more disorganized and separate individual crypts
Practice question #1
Which of the following histological features is characteristic of a mucosal prolapse polyp of the colon?
- Colonic crypts separated by splayed hypertrophic muscularis mucosae
- Cytologic dysplasia
- Hyperchromatic, elongated, penicillate nuclei
- Sawtooth pattern glands limited to the upper half of the crypts
- Serrated crypts with dilatation and branching extending to crypt bases
Practice answer #1
A. Colonic crypts separated by splayed hypertrophic muscularis mucosae are a characteristic feature of mucosal prolapse polyp. Answer E is incorrect because serrated crypts with dilatation and branching extending to crypt bases is a feature of sessile serrated lesion / polyp / adenoma. Answer B is incorrect because mucosal prolapse polyp is a nonneoplastic lesion that lacks cytologic dysplasia. Answer C is incorrect because hyperchromatic, elongated, penicillate nuclei are a feature of low grade adenomatous dysplasia. Answer D is incorrect because sawtooth pattern glands limited to the upper half of the crypts is a feature associated with hyperplastic polyps.
Comment Here
Reference: Mucosal prolapse polyp
Comment Here
Reference: Mucosal prolapse polyp
Practice question #2
Practice answer #2
C. Mucosal prolapse polyp. This image shows elongated crypts, surface congestion and erosion and splaying of the muscularis mucosae between individual crypts consistent with mucosal prolapse polyp. Answer D is incorrect because Peutz-Jeghers polyps typically contain larger smooth muscle bundles, which separate epithelium into lobules. Answer B is incorrect because inflammatory polyps lack splaying of muscularis mucosae between crypts. Answer A is incorrect because hyperplastic polyps, microvesicular type show serrated architecture with a sawtooth appearance in the upper half of the crypts.
Comment Here
Reference: Mucosal prolapse polyp
Comment Here
Reference: Mucosal prolapse polyp