Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Ding CKC, Wen KW. Adenoma overview. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/colontumoradenoma.html. Accessed September 22nd, 2025.
Definition / general
- Sometimes referred to as conventional adenoma to be distinguished from serrated lesions
- Serrated lesions are of different pathway and are not included in this topic
- Benign, premalignant neoplasm composed of dysplastic colorectal epithelium
Essential features
- Premalignant lesions
- At least low grade dysplasia; absence of true invasion
- Subtypes include tubular adenoma (most common), villous adenoma, tubulovillous adenoma and advanced adenoma
Terminology
- Conventional colorectal adenoma
ICD coding
- ICD-O:
- ICD-11: 2E92.4Y & XH7SY6 - other specified benign neoplasm of the large intestine & tubular adenoma, NOS
Epidemiology
- High incidence in populations with diets typical of high income countries with a sedentary lifestyle
- High risk population overlap with those of colorectal adenocarcinoma (see Etiology)
Sites
- Colon
Pathophysiology
- Adenoma - carcinoma sequence: genetic changes that occur before morphologically identifiable tumor formation, including a small set of driver genes (APC, CNNTB1, KRAS, SMAD4 and TP53) (Proc Natl Acad Sci U S A 2013;110:1999)
- APC genetic alteration results in reduced degradation of beta catenin and dysregulated WNT signaling (Science 1997;278:120)
- Inherited (constitutional) APC alterations lead to familial adenomatous polyposis
- Activating KRAS mutations leads to growth dysregulation through MAPK pathway (Br J Cancer 1997;75:341)
- SMAD deletion leads to disruption of TGFb growth inhibitory pathway
- Alteration of PTEN or activation of PIK3CA disrupts PI3K pathway, inhibits apoptosis and promotes neoplastic cell survival (Nat Commun 2016;7:11971, Nat Commun 2014;5:4961)
- Alteration of TP53 allows the cells to survive DNA damage and other cellular stresses (Int J Cancer 1995;64:47)
- APC genetic alteration results in reduced degradation of beta catenin and dysregulated WNT signaling (Science 1997;278:120)
- Small subset of adenoma acquires defect in DNA mismatch repair genes (predominantly hypermethylation of the MLH1 promoter) (Gastroenterol Hepatol Bed Bench 2017;10:S117)
Etiology
- Increased risk associated with consumption of processed and red meat, alcohol, excess body fat (Lancet Oncol 2015;16:1599, Ann Oncol 2017;28:1788, N Engl J Med 2016;375:794)
- Decreased risk associated with consumption of dietary fiber and dairy products, increased levels of physical activity (Ann Oncol 2017;28:1788, BMJ 2016;354:i3857)
Clinical features
- See Diagnosis
Diagnosis
Prognostic factors
- Most adenomas do not progress through the adenoma carcinoma sequence
- Risk is associated with:
- Higher number of lesions
- Larger size
- Higher proportion of villous architecture
- Extent of high grade dysplasia
Case reports
- 61 year old man with rectal bleeding for 1 week (Medicine (Baltimore) 2020;99:e20985)
- 66 year old woman with homogeneous segmental bowel wall thickening (BJR Case Rep 2020;6:20200016)
- 76 year old man with positive fecal occult blood test (Tokai J Exp Clin Med 2016;41:22)
Treatment
- Major treatment: endoscopic biopsy or resection
- According to NCCN Guidelines for Colorectal Cancer Screening (version 2.2021), if pathology identified:
- Low risk adenoma: < 2 polyps and < 1 cm
- Repeat colonoscopy in 7 - 10 years
- High risk polyp:
- High grade dysplasia present
- Villous / tubulovillous histology
- 3 - 10 adenomatous polyps (serrated lesions are discussed in different section)
- Repeat colonoscopy in 3 years; if negative, repeat colonoscopy in 5 years
- If positive, treat according to the pathology finding
- Large colorectal polyps (> 1 cm in size) without invasion:
- If pedunculated, colonoscopy in 3 years
- Sessile morphology with no high risk endoscopic features for invasive cancer:
- If complete resection and no unfavorable risk factors, colonoscopy in 1 - 3 years
- If incomplete resection, referral for surgery evaluation or expertise in management of large colorectal polyps
- Sessile morphology with high risk endoscopic features, even if no invasive cancer identified by pathology - surgical evaluation or expertise in management of large colorectal polyps
- Low risk adenoma: < 2 polyps and < 1 cm
- Reference: National Comprehensive Cancer Network: NCCN Guidelines - Colorectal Cancer Screening [Accessed 18 October 2021]
Gross description
- Specimen is received in formalin, additionally labeled transverse colon polyps and consists of 2 soft, irregular, red-tan tissue fragments (0.5 x 0.3 x 0.2 cm in aggregate)
- Specimen is received in formalin, additionally labeled right colon and consists of multiple tan to white, soft, irregular mucosal tissue fragments (0.8 x 0.2 x 0.2 cm in aggregate)
Gross images
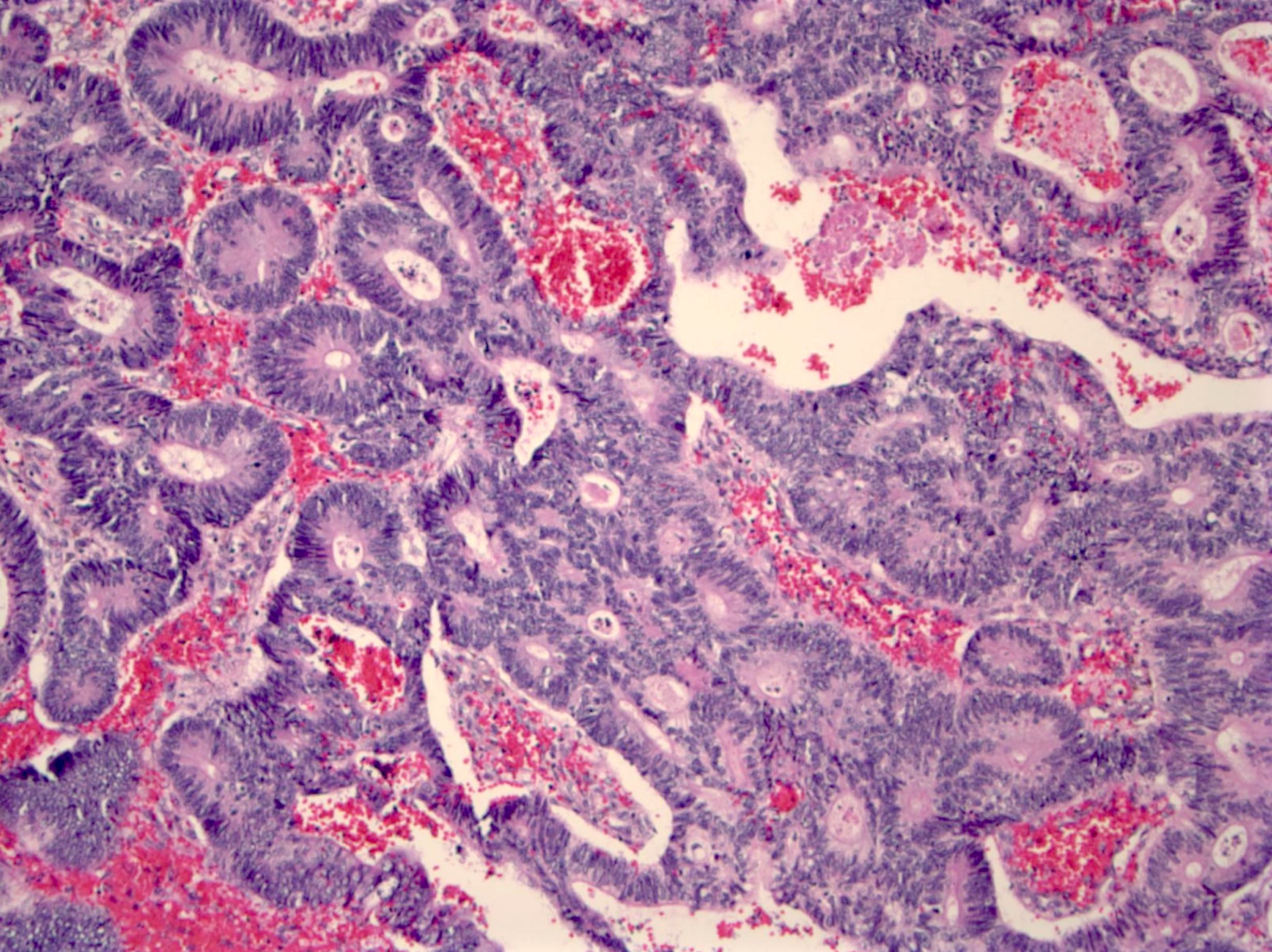
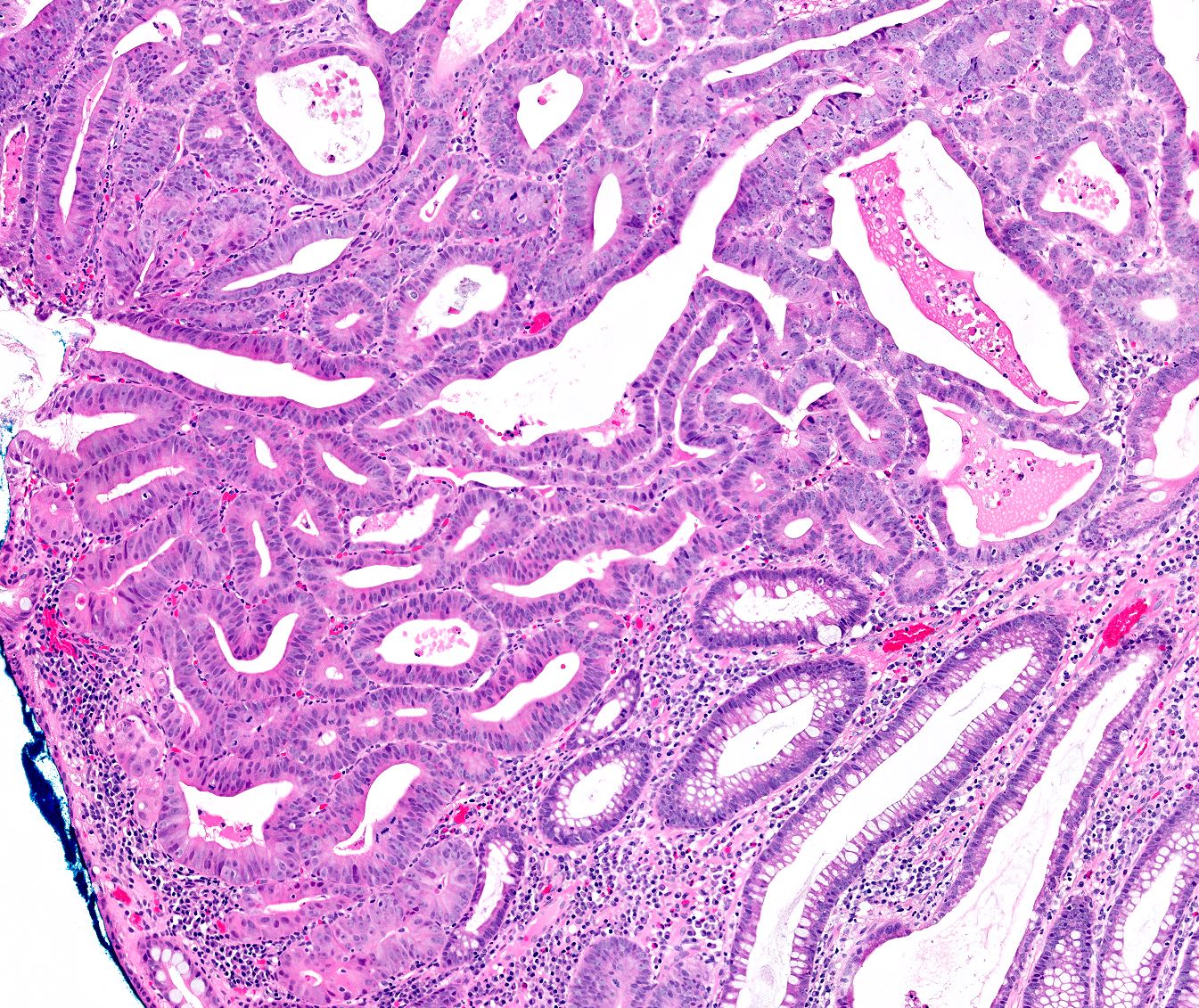
Microscopic (histologic) description
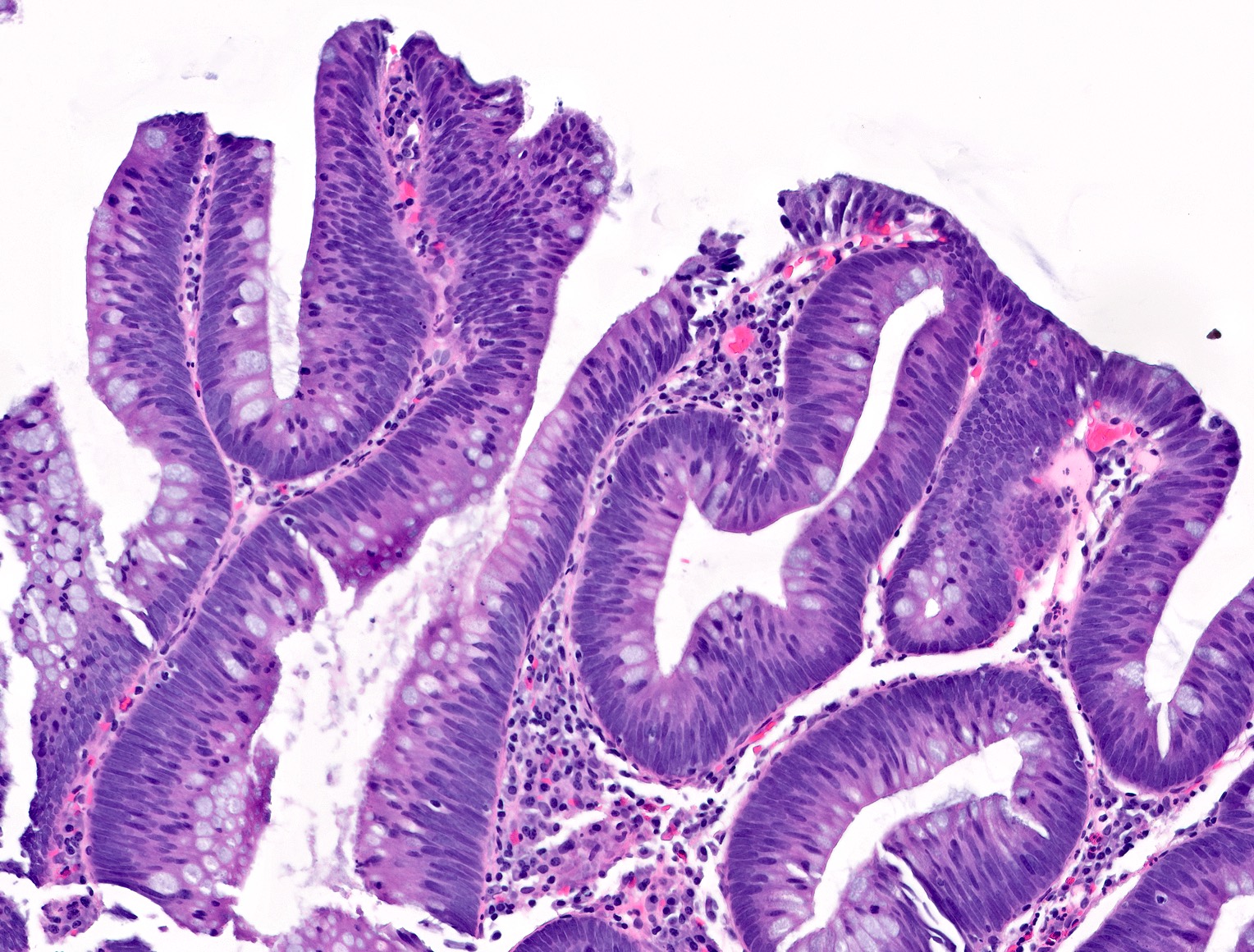
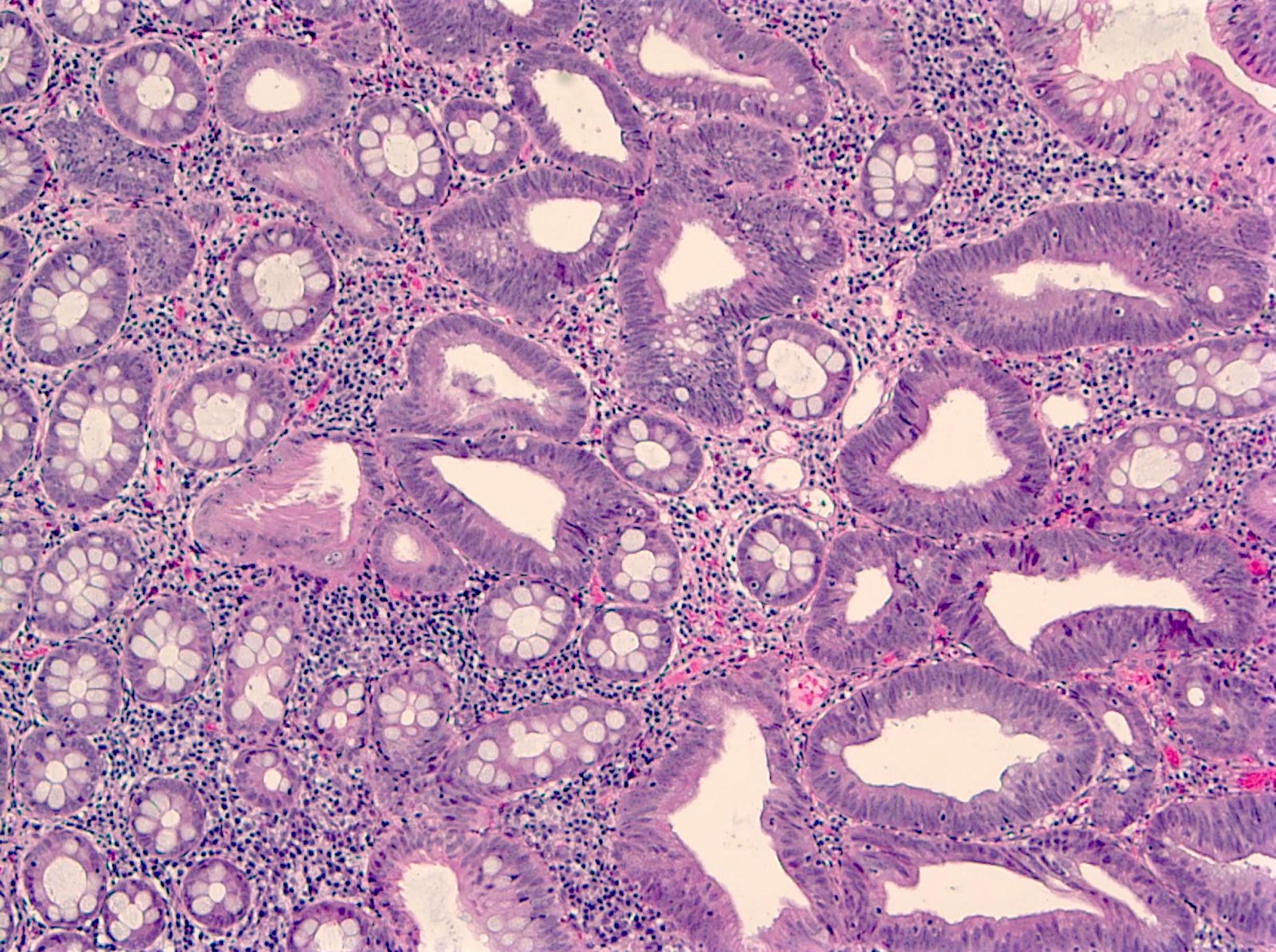
- Tubular adenomas:
- Conserved crypt architecture with variable elongation of the crypts and an increased number of glands
- At least low grade dysplasia: hyperchromatic nuclei, nuclear spindling and stratification, loss of cell polarity
- Decreased numbers of goblet cells and absorptive cells
- Small (< 25%) villous component is acceptable
- Tubulovillous adenoma:
- Similar to tubular adenoma but with 25 - 75% of villous component
- Villous component: architecture that resemble small intestinal villi
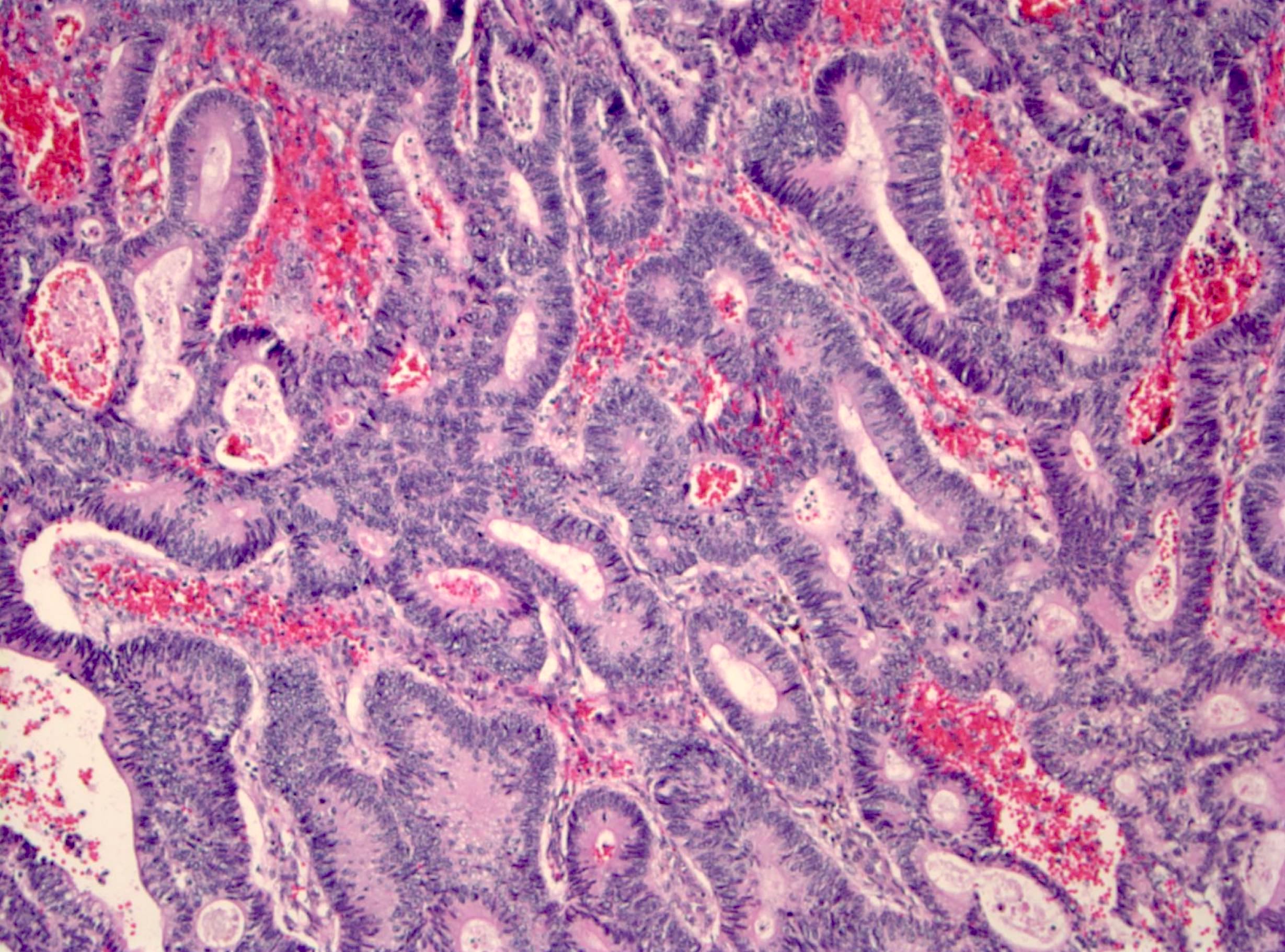
- Villous adenoma:
- > 75% of villous component
- Advanced adenoma:
- All adenomas with a size > 10 mm
- With tubulovillous or villous architecture
- With or without high grade dysplasia
- Highest risk of synchronous of metachronous adenomas
- Rare subtypes:
- Paneth cell rich subtype (more common in proximal colon or in younger patients) (Hum Pathol 2009;40:872, Sci Rep 2016;6:26129)
- Squamous components might be present as morules or squamous metaplasia (Pathobiology 2005;72:269)
- Other rare morphological findings (Histopathology 2021;78:348):
- Clear cell metaplasia or clear cell change
- Note the clear or vacuolated cytoplasm are not mucin
- Osseous metaplasia or heterotopic ossification
- Neuroendocrine differentiation
- Neuroendocrine hyperplasia
- Neuroendocrine metaplasia
- Neuroendocrine cell proliferation
- Composite intestinal adenoma microcarcinoid
- Mixed neuroendocrine - nonneuroendocrine neoplasm (MiNEN)
- Mixed adenoma - neuroendocrine tumor (MANET)
- Signet ring cell-like lesion
- Clear cell metaplasia or clear cell change
- Histology grading:
- 2 tiered system: low grade versus high grade
- Criteria for high grade dysplasia:
- Architecture: marked complex glandular crowding with glandular irregularity; cribriform architecture; intraluminal necrosis; can be observed at low power
- Cytology: substantial loss of cell polarity, marked enlarged nuclei with prominent nucleoli, dispersed chromatin pattern, atypical mitotic figures (Eur J Gastroenterol Hepatol 2002;14:183, Colorectal Dis 2015;17:682)
- Should be no evidence for invasion, however, pseudoinvasion (epithelial misplacement) could sometimes be seen due to prolapse (Mod Pathol 2015;28:S88)
- Features favoring pseudoinvasion / epithelial misplacement:
- Signs suggestive of previous epithelial trauma (extracellular mucin, hemorrhage or hemosiderin)
- Focus appears to be continuous with the surface epithelium with similar cytology
- Signs of mucosal prolapse such as muscular proliferation
- Acute necrosis of the surface
- Features favoring adenocarcinoma:
- Isolated glands without accompanying lamina propria
- Budding
- Vascular invasion
- Poor differentiation in morphology
- Concurrent review by more than 1 GI pathologist is suggested if high grade dysplasia is present
- Features favoring pseudoinvasion / epithelial misplacement:
Microscopic (histologic) images
Molecular / cytogenetics description
- Not routinely performed, although majority of cases will have chromosomal instability; a subset (~25%) of cases will show TP53 mutations
Videos
Tubular adenoma
Colon dysplasia
Villous adenoma
Sample pathology report
- Colon, hepatic flexure polyp, biopsy:
- Tubular adenoma with focal high grade dysplasia
- Ascending colon, polyp, endoscopic mucosal resection:
- Fragments of tubulovillous adenoma (see comment)
- Comment: No high grade dysplasia is identified. Specimen fragmentation precludes assessment of specimen margins.
Differential diagnosis
- Reactive colonic mucosa:
- Smaller nuclei with basal orientation
- No or less significant hyperchromasia or pseudostratification
- More abundant cytoplasm and mucin
- Invasive adenocarcinoma:
- At least invasion through muscularis mucosa into the submucosa
- Desmoplasia, single cells
- Traditional serrated adenoma:
- Sawtooth luminal / surface contour
- Ectopic crypts characterized by aberrant budding crypts
Practice question #1
Practice answer #1
D. TP53. Alteration of TP53 allows cells to survive DNA damage and other cellular changes. It is found in ~25% of adenomas.
Comment Here
Reference: Adenoma overview
Comment Here
Reference: Adenoma overview
Practice question #2
Practice answer #2
A. The number of adenomatous polyps considered to be a low risk feature is < 3.
Comment Here
Reference: Adenoma overview
Comment Here
Reference: Adenoma overview