Table of Contents
Definition / general | Essential features | Terminology | Blood flow (or inflow - outflow) method | Short axis method | Base of the heart method | 4 chamber method | Coronary dissection methods | Gross images | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Thomas SC, Gitto L. Basic heart dissection techniques for forensic purposes. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/forensicsheartdissection.html. Accessed September 26th, 2025.
Definition / general
- Heart dissection is a medical procedure whereby a pathologist examines and dissects the heart of a deceased individual to determine the cause of death or any underlying heart conditions
Essential features
- Cardiovascular disease accounts for most natural deaths in the medical examiner / coroner's office
- Multiple heart dissection techniques exist
- Each dissection technique allows for examination of specific heart regions or disease
Terminology
- Short axis: the heart is dissected into thin slices perpendicular to its long axis, allowing for a detailed examination of the cross sectional anatomy of the heart
- Blood flow (or inflow - outflow): the heart is dissected following the path of blood
- 4 chambers: the heart is dissected to expose its 4 chambers
- Base of the heart: the heart is dissected to expose the valve plane
Blood flow (or inflow - outflow) method
- Initial dissection: separate the aorta and pulmonary artery from the other vessels at the base of the heart, cutting the intervening connective tissue
- Right atrium: cut anteriorly from the inferior vena cava (IVC) opening to the tip of the right atrial appendage
- Alternatively, dissect along the posterior atrial wall between the IVC and superior vena cava (SVC)
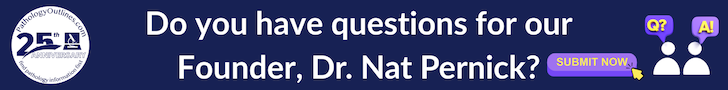
- Both methods will allow for preservation of the sinoatrial node that lies on the lateral margin of the junction of the SVC with the right atrium and the atrial appendage along the crista terminalis (sulcus terminalis - terminal groove) (see image 1)
- Right ventricle: place the scissors or blade within the right atrial cavity and move through the tricuspid valve; keep the blade along the right ventricle's lateral margin (free wall) and make a single, continuous dissection to the cardiac apex (see image 2)
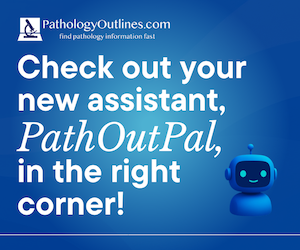
- Right ventricle outflow tract: once the right ventricular cavity is opened, extend the dissection from the apex upwards through the pulmonary outflow tract (pulmonary conus, valve and artery)
- Placing the scissors or the blade parallel to the interventricular (IV) septum will decrease the chance of cutting through one of the cusps of the pulmonary valve (see image 3)
- Left atrium: an easy way to open the left atrium is by dissecting between the pulmonary veins' orifices
- If the pulmonary veins need to be spared, make a hole in the left atrial appendage and extend the dissection to the orifice of the pulmonary veins (see image 4)
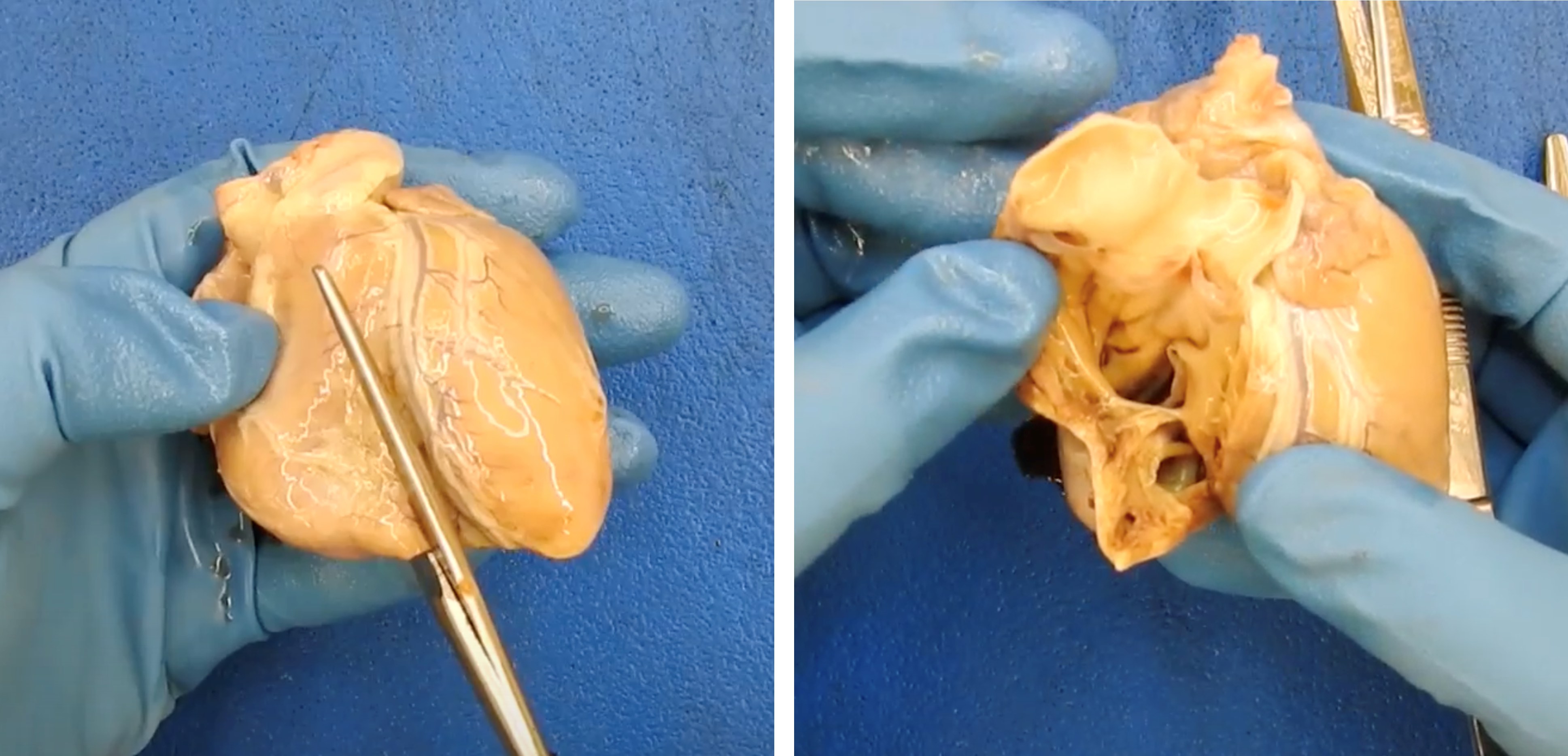
- Left ventricle: place the scissors or blade within the left atrial cavity and move through the mitral valve; keep the blade along the lateral margin of the left ventricle and make a single, continuous dissection to the cardiac apex (see image 5)
- Left ventricle outflow tract: once the left ventricular cavity is opened, the dissection needs to be extended along the IV septum between the apex and the aortic valve (AV)
- If the AV cusps are not relevant in the specific case, placing the scissors or the blade perpendicular to the IV septum will decrease the chance of cutting through one of the AV cusps
- If the AV cusps need to be spared, the safest way is to check them from the aortic root by cutting the aorta up to ~0.5 - 1 cm above the AV plane
- When the AV cusps are exposed, place the scissors between the cusps and make a dissection in the direction of the IV septum (see image 6)
- This dissection can be extended from the AV plane to the apex
- Alternatively, after a dedicated dissection has secured the cusps, the left ventricle outflow tract can be opened by dissecting from the apex toward the AV, joining the previous AV dissection
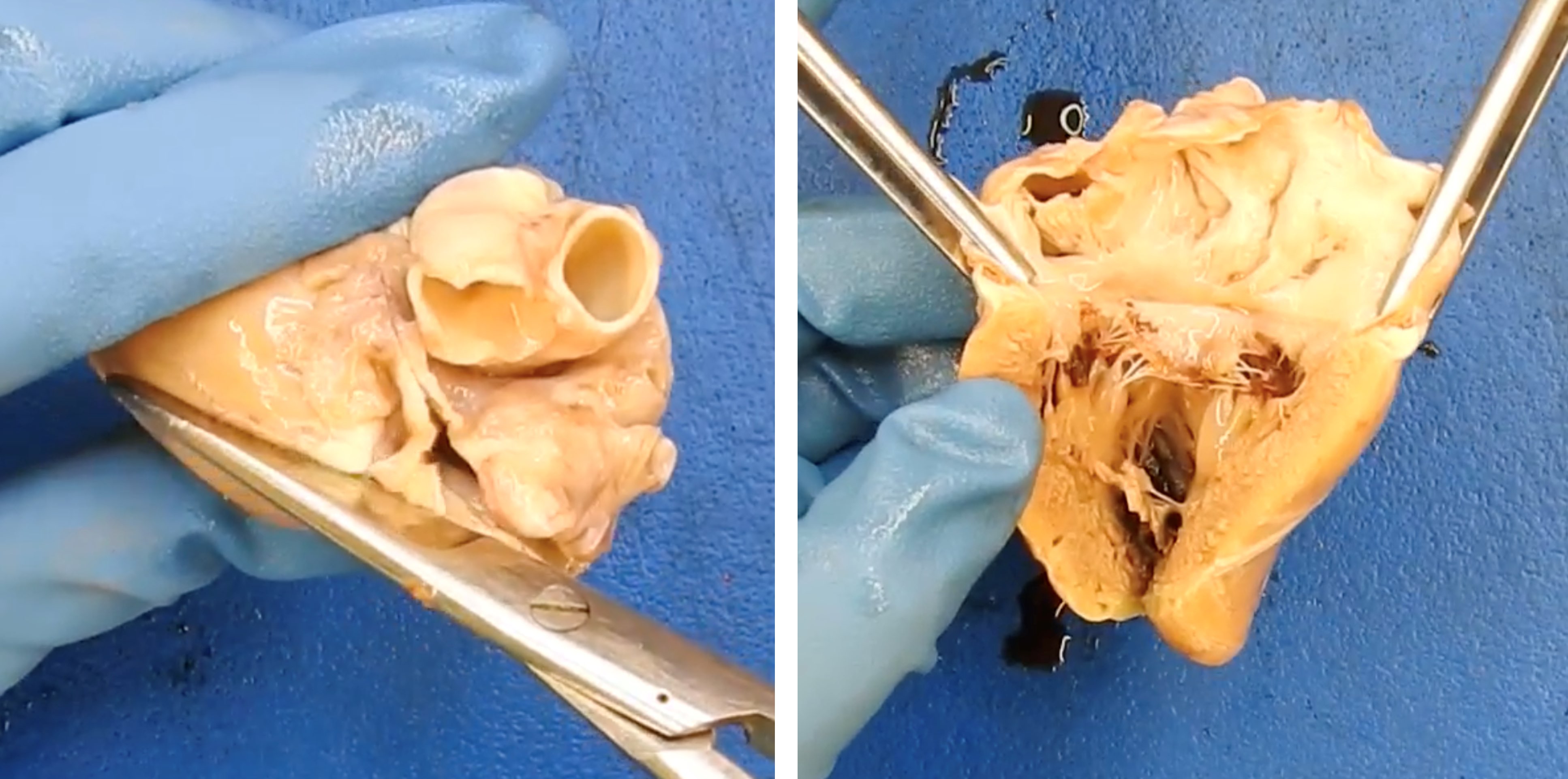
- Final dissections: once all chambers of the heart are opened, the right and left ventricles wall can be sliced by partial thickness sections from the endocardial surface, to allow examination of the myocardium
- Papillary muscle should be dissected to assess for any abnormalities
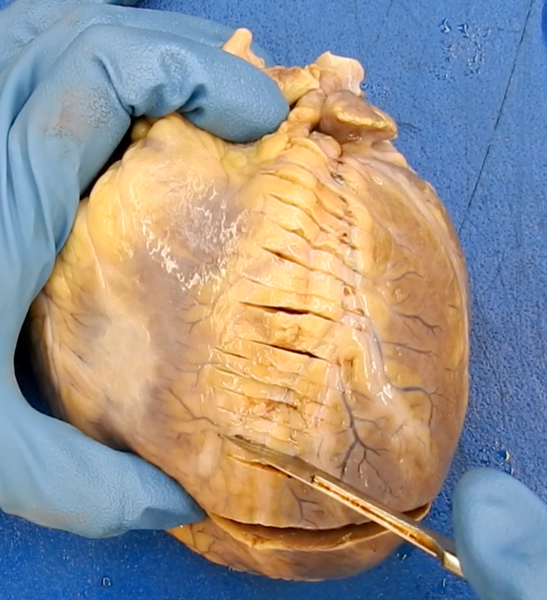
Short axis method
- Most common heart dissection technique used in forensic autopsies
- Initial dissection: multiple transverse cuts are performed, 0.8 - 1.5 cm thick from the cardiac apex to the base, parallel to the atrioventricular groove (which demarcates the borders of the underlying atria from the ventricles) (see image 1)
- Dissection should be stopped just below the apical papillary muscles to preserve the valve
- Heart should be kept as still as possible to avoid irregular sections or dissection artifacts; placing a paper towel beneath the organ may help
- Slices can then be placed on the board and examined (see image 2)
- Remaining specimen: once the transverse sections have been made, the heart can be dissected following the blood flow method described above
Base of the heart method
- Initial dissection: dissect the ventricles following the short axis method described above
- Right atrium: place the scissors into the IVC and dissect along the free wall of the right atrium to the tip of the right atrial appendage and the upper aspect of the atrial septum adjacent to the ascending aorta; leave ~1.0 cm distance from the tricuspid valve plane
- Left atrium: locate the coronary sinus ostium and dissect from the right atrium along the outer wall of the coronary sinus in the left atrioventricular groove
- Once the left atrium free wall is reached, extend the dissection from the lower aspect of the atrial septum to the level of the left atrial appendage and the upper border of the atrial septum, meeting the previous dissection from the right atrium
- Dissect through the atrial septum to remove both atria
- Aorta and pulmonary artery: transect the great vessels at the level of the valve commissures
- Trim the soft tissues as needed to expose the aortic and pulmonary valves
- If the left circumflex (LCX) and the right coronary arteries have not yet been examined, it is not possible to dissect them easily
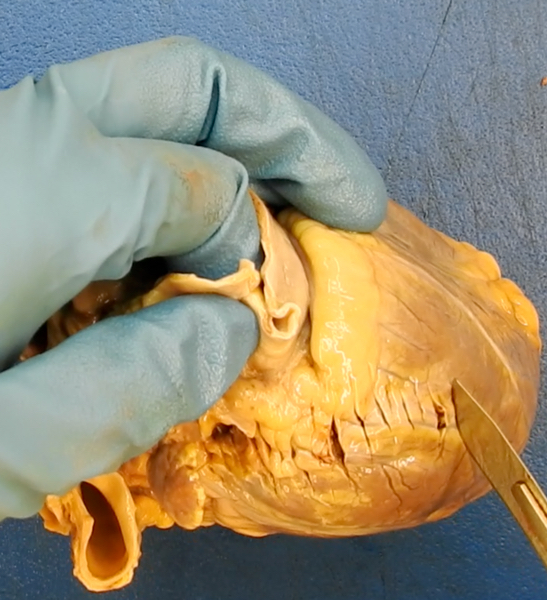
4 chamber method
- Initial dissection: the heart is placed with the anterior aspect facing the operator; the first cut can be done in 2 ways using a long blade sharp knife
- First way: dissect from the heart base to the apex
- Using the fingers through the atrial cavities and atrioventricular valves (mitral and tricuspid), to locate and palpate left and right free ventricular walls
- Superficial cuts can be made on the external aspect of the organ at the level of the left and right ventricular walls as a guide
- Place the blade between these 2 cuts (or approximately in the middle of the right and left ventricular walls)
- Place the free hand palm on the anterior aspect of the heart and make a single, continuous cut moving from the base to the apex, dissecting the right ventricle, the left ventricle and the IV septum
- Second way: dissect from the heart apex to the base
- Starting from the cardiac apex, the dissection is extended along the acute margin of the right ventricle, the obtuse margin of the right ventricle and the IV septum
- During the dissection, the operator can check if the cut is oriented in the right direction
- First way: dissect from the heart base to the apex
- Remaining specimen: once the heart is bisected into 2 halves, all 4 chambers should be visible; the remaining unopened portions (bilateral ventricular outflow tracts) can be opened following the blood flow method described above
Coronary dissection methods
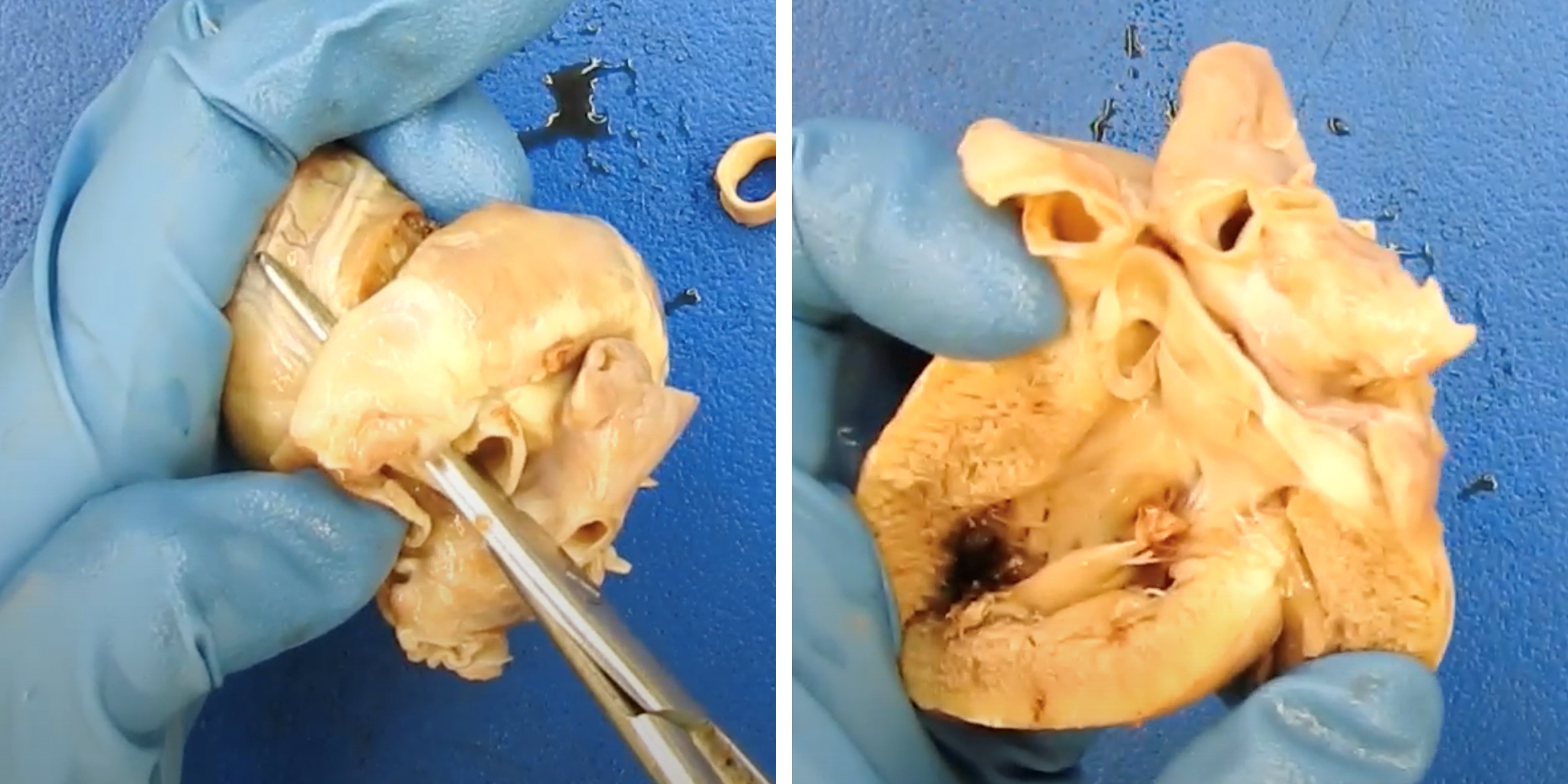
Serial sectioning
Longitudinal dissection
Removal of the coronary arteries from the heart
- Most common coronary dissection technique
- Locate the coronary arteries on the epicardial surface
- Separate the aorta and pulmonary artery from the other vessels at the base of the heart, cutting the intervening connective tissue to locate the left common coronary artery (see image 1)
- Make an initial transverse section at the left common coronary origin level
- Then move distally to find the vessel bifurcation
- Follow the left anterior descending (LAD) coronary artery path, making serial 0.3 cm thick cuts perpendicular to the main axis of the vessels, up to the most distal part (see image 2)
- After examining the LAD coronary artery, move back to the left common coronary artery bifurcation and follow the LCX coronary artery, which travels laterally just below the left atrial appendage
- If needed, the soft tissue below the left atrial appendage can be superficially trimmed to allow a more accessible examination of the LCX coronary artery
- Follow the LCX coronary artery path, making serial 0.3 cm thick cuts perpendicular to the main axis of the vessels, up to the most distal part (see image 3)
- Place the heart with the anterior aspect facing the operator and the apex facing inferiorly
- Rotate the heart ~45 degrees counterclockwise and make a straight cut at the level of the adipose tissue surrounding the lateral ascending aorta
- This should expose the right coronary artery, which travels just below the right atrial appendage
- Follow the right coronary artery path, making serial 0.3 cm thick cuts perpendicular to the main axis of the vessels, up to the most distal part (see image 4)
Longitudinal dissection
- Can be done in young subjects when there are no concerns for coronary diseases
- Serial sectioning is still the preferred method
- Locate the coronary arteries' ostia at the level of the aortic valve
- Using dedicated vascular coronary scissors, place the blunt tip within the ostium and the sharp tip outside the vessel and extend the dissection as distally as possible
- If stenosis or atherosclerotic plaques are encountered during the dissection, do not push the blunt tip forward to avoid creating artifacts or removing potential plaques or thrombi
- Instead, stop the longitudinal dissection and perform a local serial section to evaluate the grade of lumen stenosis
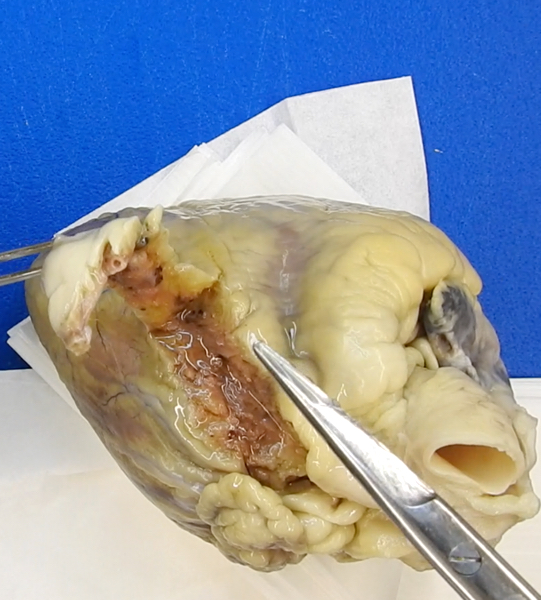
Removal of the coronary arteries from the heart
- Useful in case of severely atherosclerotic and calcified vessels
- Rarely necessary in the forensic setting
- This method will produce artifacts to the epicardial surface of the heart, which are expected and cannot be avoided
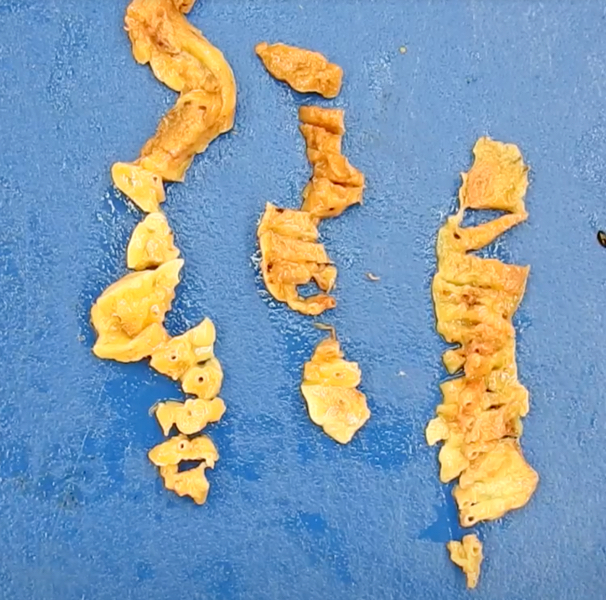
- Using scissors with blunt tips, make a small cut just beneath the origin of the left anterior coronary artery (see image 1)
- From there, dissect along the posterior aspect of the vessel, following its pathway up to the most distal part (see image 2)
- If a tract of the coronary artery is accidentally transected, proceed with an extra deeper cut along the posterior aspect of the vessel
- Use the same technique to remove the LCX and the right coronary arteries (see images 3 - 4)
- Once the coronary arteries have been removed, they can be placed on the board (see image 5)
- Serial transverse sections at 2 - 3 mm intervals are made to evaluate for lumen stenosis, thrombosis or other abnormalities (see image 6)
Gross images
Additional references
Practice question #1
A 16 year old athlete dies suddenly while playing soccer. At autopsy, there is no evidence of injury to the body. Toxicology is positive for tetrahydrocannabinol (THC) but is otherwise noncontributory. The forensic pathologist is going to examine the heart. What is the best next step?
- Dissect the heart after formalin fixation using the 4 chamber technique; in case of pathologic findings, consider further testing
- Dissect the heart after formalin fixation using the base of the heart method technique; in case of pathologic findings, consider further testing
- Dissect the heart after formalin fixation using the short axis technique; no other tests are needed
- Dissect the heart fresh following the blood flow; no other tests are needed
- Dissect the heart fresh using the 4 chamber technique; in case of pathologic findings, consider further testing
Practice answer #1
A. Dissect the heart after formalin fixation using the 4 chamber technique; in case of pathologic findings, consider further testing. Among the options, this answer gives the best combination. The clinical scenario suggests a sudden cardiac death, which in the young during sports activities is suspicious for hypertrophic cardiomyopathy. The 4 chamber dissection technique allows for a detailed evaluation of the myocardial wall thicknesses and will highlight the presence of interventricular septum hypertrophy and asymmetry. Genetic testing is recommended to family members if pathological findings are seen. The blood flow method (answer D) will not show evidence of septum asymmetry. The base of the heart method (answer B) is useful for examining the heart valves. It is not used for hypertrophic cardiomyopathy. While the short axis method (answer C) can be used, the 4 chamber method is recommended in case of possible hypertrophic cardiomyopathy since it will show the pathologic findings better. If a hypertrophic cardiomyopathy is suspected based on the clinical scenario and the heart external morphology, it is recommended to retain the heart and wait for formalin fixation. Attempting to cut the heart while it is fresh (answer E) can be difficult and may lead to artifacts that could hinder the ability to recognize the distinctive morphology associated with this condition.
Comment Here
Reference: Forensic heart dissection
Comment Here
Reference: Forensic heart dissection
Practice question #2
A 28 year old man was found unresponsive in his secured apartment. He was brought to the hospital, where he was pronounced dead. There was no evidence of trauma or foul play. He had no history of cardiovascular disease but complained of unspecific chest pain the day before, lasting 45 minutes. Urine drug screening performed at the hospital is positive for cocaine and amphetamine. What is the best next step?
- Do not perform an autopsy, collect blood samples during the external examination and run an expanded toxicology panel; once you get the results, you can sign out the case accordingly
- Perform the autopsy and save the heart in formalin for examination once fixed; run genetic tests and expanded toxicology
- Perform the autopsy, dissect the coronary arteries using the serial sectioning method and run expanded toxicology
- Perform the autopsy; since he is young and has no history of coronary disease, dissect the coronary artery using the longitudinal dissection method and run expanded toxicology
- Sign out the case as probably cocaine and amphetamine toxicity and accident
Practice answer #2
C. Perform the autopsy, dissect the coronary arteries using the serial sectioning method and run expanded toxicology. A history of recent chest pain in a young adult with no cardiovascular diseases and with urine screening tests positive for stimulants should raise the concern of possible coronary artery thrombosis. Serial sectioning of the coronary arteries allows for precise localization and measurement of the coronary thrombus. Full toxicology must still be requested since the urine drug screen is only qualitative. The subject is young with a history of chest pain and positive urine screen; thus, an autopsy is necessary to determine the cause and manner of death (answer A). There is no need to save the heart in formalin (answer B) unless there is a substantial concern for cardiomyopathy. The longitudinal dissection (answer D) should never be used when there is suspicion for coronary thrombosis since the tip of the scissors may move the thrombus from its original location, creating artifacts and possibly masking the pathologic finding.
Comment Here
Reference: Forensic heart dissection
Comment Here
Reference: Forensic heart dissection