Table of Contents
Definition / general | Essential features | Terminology | Diagrams / tables | Critical reporting systems | Critical laboratory communications | Examples of critical values | Laboratory communications (noncritical) | Microscopic (histologic) images | Videos | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Christie-Nguyen PT, Hassell LA. Critical reporting systems and laboratory communications. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/labadminreportingandcomm.html. Accessed August 1st, 2025.
Definition / general
- Critical values (CVs): laboratory results that require prompt, appropriate intervention to avert potential serious outcomes
Essential features
- The process of establishing CVs that merit immediate notification should involve not only laboratory personnel but also clinical providers, clinical informaticists and hospital management
- CV communication should be done promptly, ideally within 30 minutes, for all chemistry, toxicology, hematology, therapeutic drugs, microbiology, anatomical pathology and cytopathology
- The advisable means of CV communication is internal phone calls; significant / unexpected diagnosis in anatomical pathology can be communicated by a secured messaging system if there is failure to initiate a phone call
Terminology
- Critical values
- Urgent actionable results
- Unexpected findings with potential urgent implications
- Rapid results
- Frozen section reporting
Diagrams / tables
Critical reporting systems
- The laboratory medical director develops the list of critical values based on CAP guidelines and the institution's patient population
- Establishes critical report procedure; lab technicians, clinical personnel, clinical informaticists and hospital management must be involved
- Categorizes the urgency level of critical values and expected turnaround time for each group (Jt Comm J Qual Patient Saf 2005;31:68):
- Red:
- Life threatening values
- Requires an immediate call, ideally within 30 minutes (Arch Pathol Lab Med 2012;136:148)
- Prompt clinical decision warranted
- Orange:
- Significantly abnormal results
- Requires quick calls but not immediate
- Clinical decision needed within hours
- Yellow:
- Abnormal results but not life threatening
- Can be sent passively
- Additional communication is necessary
- Clinical decisions are needed within days
- Red:
- Separate CVs list for anatomic pathology (including surgical pathology and cytopathology) with 2 categories (J Am Soc Cytopathol 2021;10:341):
- Red: time critical diagnoses that are medical emergencies or have infectious risks
- Orange: significant / unexpected diagnoses that necessitate additional communication
- Often use a middleware flagging system to raise an alerting pop up when CVs emerge
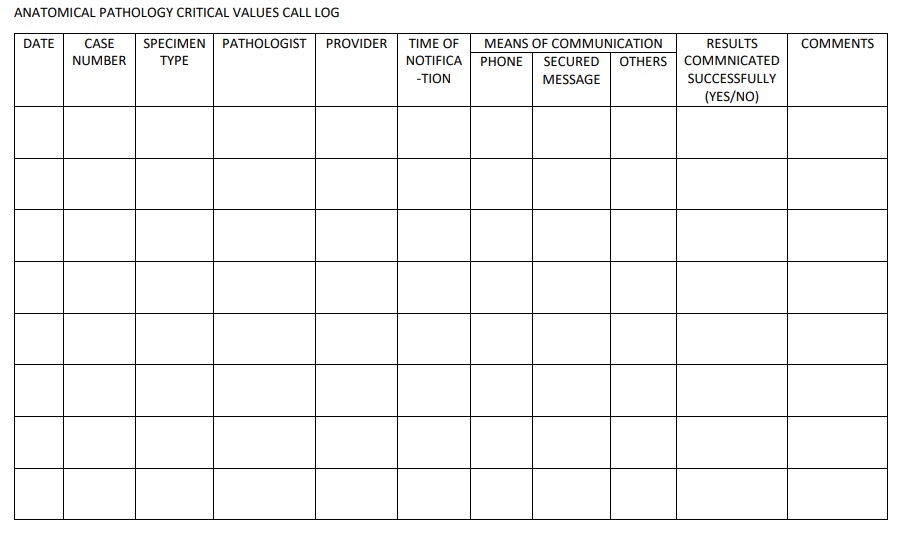
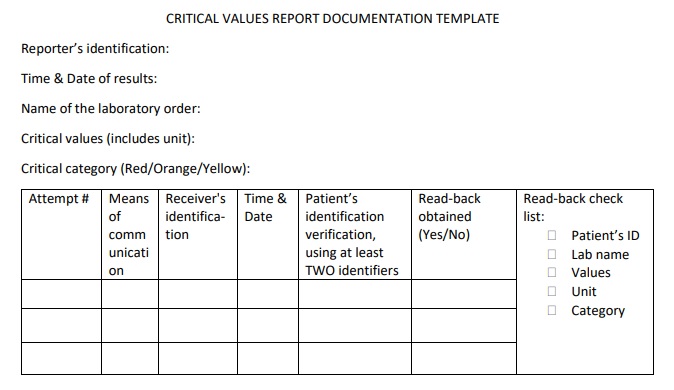
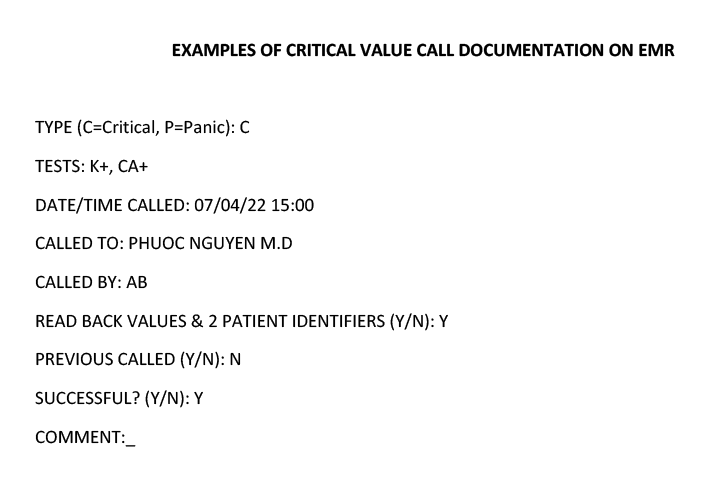
- Design a pop up with dropdowns on the electronic medical record to document when CVs emerge (example shown below); or a paper template to document the CVs calls log
- Include an on call roster so the lab staff can navigate to whom to report CVs, with a decision tree in the event of nonresponse
- Create an escalation policy, defining the order of receivers that the reporter should call when the ordering provider is not approachable
- Review / revise the critical value list periodically in consultation with medical providers
- Assess the effectiveness of the report critical system regularly
Critical laboratory communications
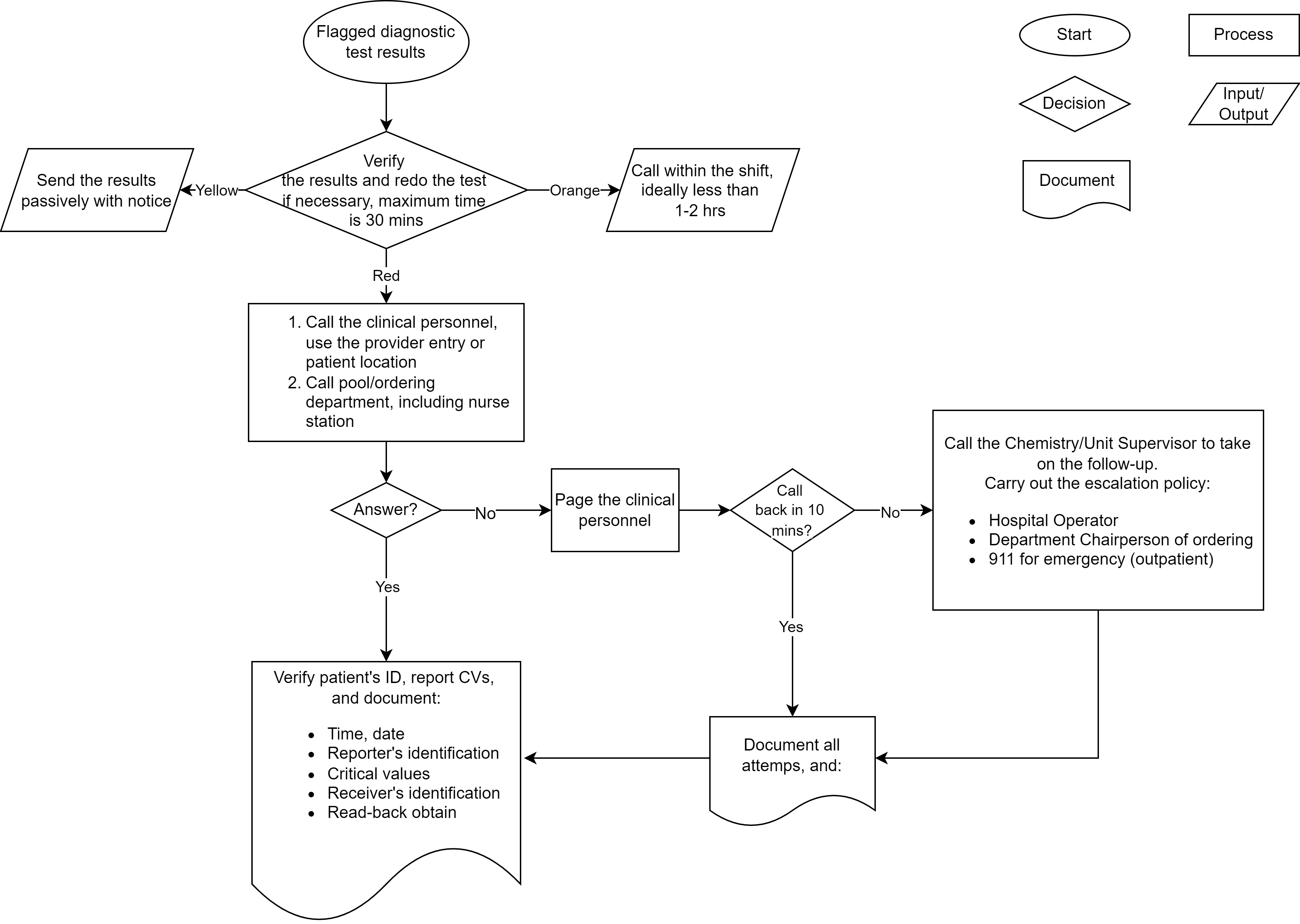
- Chemistry or microbiology critical values:
- Identify the reporter, usually the performing technologist
- Verify and repeat the test if needed; the maximum is 30 minutes
- Identify the receiver using the provider entry, the patient location and the on call roster
- Determine means of notification:
- Step 1: call the ordering physician (CAP recommended); call other extensions, including the nurse station, in the same department if there is no answer
- Verify the patient’s identification using 2 identifiers
- Test name
- Critical values (including unit and normal range), their category
- Read back for confirmation
- Verbally correct any errors and repeat the request for a read back if needed
- Document the notification process
- Step 2: page the clinical personnel if there’s no answer to the phone call; if the provider calls back in 10 minutes, conduct actions in Step 1
- Step 3: if there is no response after paging, call the chemistry / unit supervisor to take on the follow up
- That person initiates the escalation policy
- First task is to call the hospital operator for a medical alert call
- If there is still no response, call the department chairperson of ordering provider
- Step 1: call the ordering physician (CAP recommended); call other extensions, including the nurse station, in the same department if there is no answer
- The reporter must document all the calling attempts and notification details, including the reporter’s identification, time, date, critical values, category, receiver’s identification and whether a confirmation was provided (by a read back)
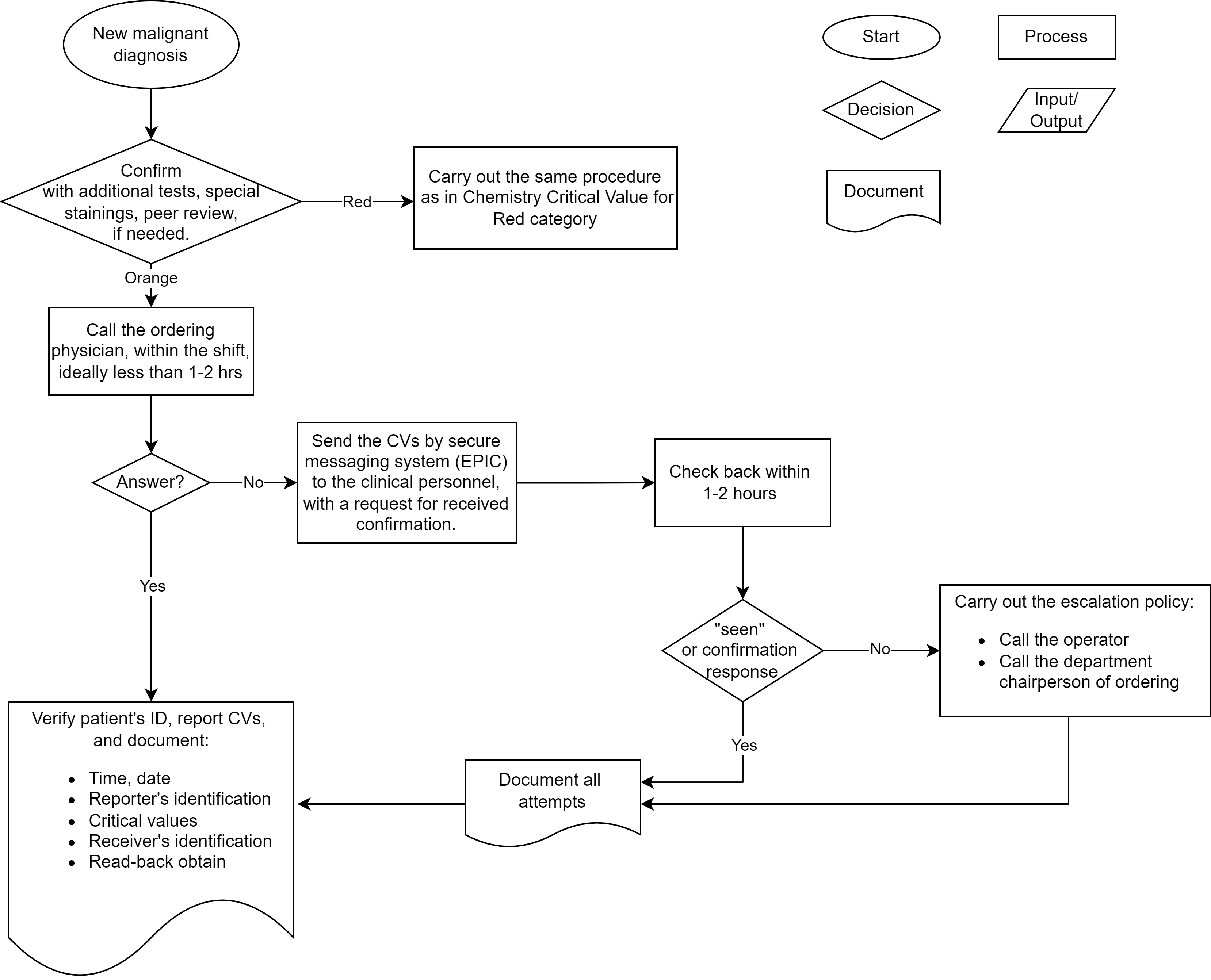
- Anatomical critical values:
- If needed, confirm the result with the additional tests, IHC staining and peer reviews
- Identify the reporter (usually the pathologist) who established the diagnosis
- Identify the receiver, usually the ordering provider or the physician who performed the biopsy / FNA / surgery
- Determine the category for the result
- If the result is in the red category, it needs immediate intervention; carry out the same procedure as in chemistry / microbiology CVs
- If the result falls in the orange category, carry out the following steps:
- Step 1: call the ordering physician (CAP recommended); call other extensions, including the nurse station, in the same department if there is no answer
- Verify the patient’s identification using 2 identifiers
- Specimen type
- Critical values, their category
- Request read back for confirmation
- Verbally correct any errors and repeat the request for a read back if needed
- Document the notification process
- Step 2: if there’s no answer to the phone call, send the critical values through a secure messaging system (i.e., EPIC) to the ordering physician and the patient’s provider; a confirmation of receipt should be requested (Lab Med 2020;51:e6)
- Step 3: check back within 1 - 2 hours; if there is no confirmation response, carry out the escalation policy; call the hospital operator for support; if there is still no response, call the department chairperson of ordering provider
- Step 1: call the ordering physician (CAP recommended); call other extensions, including the nurse station, in the same department if there is no answer
- The reporter must document all the call attempts and notification details, including the reporter’s identification, time, date, critical values, category, receiver’s identification and whether a confirmation is provided (by a read back)
- Critical values in outpatient settings:
- Step 1: verify the result and send the result to the ordering provider; call the patient’s primary care provider (PCP) clinic and report the result to the nurse / medical assistant / front desk personnel; carry out the same procedure as an inpatient critical values call:
- Verify the patient’s identification using 2 identifiers
- Test name
- Critical values (including unit and normal range), their category
- Read back for confirmation
- Verbally correct any errors and repeat the request for a read back if needed
- Document the notification process
- Step 2: if there is no answer from the primary care provider's clinic, call the lab supervisor / attending pathologist to take on the next steps
- Step 3: the lab supervisor / attending pathologist attempts to call the patient’s home or mobile phone number; explain to the patient that they have a critical test result and need to contact their primary care provider and come to the nearest emergency department for immediate treatment
- Step 4: if the patient is unable to comprehend the results or there is no call answer, call 911 for support
- The reporter must document all call attempts and notification details, including the reporter’s identification, time, date, critical values, category, receiver’s identification and whether a confirmation is provided (by a read back)
- Step 1: verify the result and send the result to the ordering provider; call the patient’s primary care provider (PCP) clinic and report the result to the nurse / medical assistant / front desk personnel; carry out the same procedure as an inpatient critical values call:
Examples of critical values
A. Chemistry critical values:
| Test | Less than or equal to | Greater than or equal to |
| ALT neonate < 12 months | 100 U/L (UC Irvine: Critical Values for Infants (<12 Months) [Accessed 2 September 2022]) | |
| Bilirubin neonate 1D | ≥ 6 µg/mL (UC Irvine: Critical Values for Infants (<12 Months) [Accessed 2 September 2022]) | |
| Bilirubin neonate 2D | ≥ 10 µg/mL (UC Irvine: Critical Values for Infants (<12 Months) [Accessed 2 September 2022]) | |
| Bilirubin neonate 3D - 4D | ≥ 12 µg/mL | |
| Bilirubin neonate 5D - 12M | ≥ 15 µg/mL (UC Irvine: Critical Values for Infants (<12 Months) [Accessed 2 September 2022]) | |
| Calcium adults | 6 mg/dL, adult 6.5 mg/dL, pediatric (UC Irvine: Critical Values for Infants (<12 Months) [Accessed 2 September 2022]) | 13 mg/dL, adult 12 mg/dL, pediatric (UC Irvine: Critical Values for Infants (<12 Months) [Accessed 2 September 2022]) |
| CO2 | 10 mmol/L | 50 mmol/L |
| Ethanol | 300 mg/dL, adult 10 mg/dL, pediatric | |
| Ethanol glycol | 20 mg/dL | |
| Glucose adults | 450 mg/dL 300 mg/dL | |
| Isopropanol | 10 mg/dL | |
| Magnesium | 1.0 mg/dL | 4.7 mg/dL |
| Methanol | 10 mg/dL | |
| Potassium | 2.8 mmol/L, adult 3.0 mmol/L, pediatric | ≥ 6.2 mmol/L, adult 6.5 mmol/L, pediatric |
| Propylene glycol | 100 mg/dL | |
| Sodium | 120 mmol/L | 160 mmol/L |
| Troponin T | > 0.01 ng/mL | |
| Test | Greater than or equal to |
| Acetaminophen | 150 µg/mL: 4 hours post ingestion 40 µg/mL: 12 hours post ingestion (ARUP Lab: Critical Values List [Accessed 2 September 2022]) |
| Amikacin | 35 µg/mL |
| Carbamazepine | 12 µg/mL |
| Digoxin | 2.0 ng/mL |
| Everolimus | 30 ng/mL (University of Michigan: Everolimus [Accessed 2 September 2022]) |
| Gentamicin | 15 µg/mL |
| Lead | 10 µg/dL (for < 16 years old) 20 µg/dL (for ≥ 16 years old) |
| Lidocaine | 5 µg/mL |
| Lithium | 1.5 mEq/L (University of Michigan: Lithium [Accessed 2 September 2022]) |
| Phenobarbital | 60 µg/mL, adult 50 µg/mL, neonate < 12 months (UC Irvine: Critical Values for Infants (<12 Months) [Accessed 2 September 2022]) |
| Phenytoin | 30 µg/mL |
| Procainamide | 16 µg/mL |
| Salicylate | 30 mg/dL (University of Michigan: Salicylate [Accessed 2 September 2022]) |
| Sirolimus | 25 ng/mL: liver transplantation 15 ng/mL: renal transplantation (UC Irvine: Critical Values for Adults and Pediatrics (≥ 12 Month) [Accessed 2 September 2022]) |
| Tacrolimus | 20 ng/mL (UC Irvine: Critical Values for Adults and Pediatrics (≥ 12 Month) [Accessed 2 September 2022]) |
| Theophylline | 20 µg/mL |
| Tobramycin | 10.5 µg/mL (University of Michigan: Tobramycin [Accessed 2 September 2022]) |
| Valproic acid | 150 µg/mL |
| Vancomycin peak / random | 60 µg/mL (University of Michigan: Vancomycin [Accessed 2 September 2022]) |
| Test | Less than or equal to | Greater than or equal to |
| Fibrinogen | 80 mg/dL | |
| Hematocrit, adult | 18% | 55% |
| Hemoglobin, adult | 6 g/dL (< 7 outpatient) | 22 g/dL |
| HIT (heparin dependent antibody) | Positive | |
| INR (venous) | 5.0 (University of Michigan: PT (Prothrombin Time) and INR [Accessed 2 September 2022]) | |
| Platelet count | 10.0 k/mm3 | 1,000 k/mm3 |
| PTT (outpatient only) | 50 seconds | |
| White blood count | 1.0 k/mm3 | 50.0 k/mm3 |
B. Microbiology critical values:
|
C. Anatomical pathology critical values:
or "orange" category |
|
or "red" category | ||
Site specific CVs | Pap smear |
|
| CSF |
| |
| BAL |
| |
Site agnostic CVs |
| |
or "red" category |
|
Laboratory communications (noncritical)
- Changes in methodology, reference ranges, availability, specimen requirements or other matters should be communicated to laboratory users in a timely manner
- Laboratory user manuals (specimen requirements, ordering, expected turn around times, etc.) should be available to all lab users
- Quality improvement effort results and feedback should be regularly provided to lab users as part of the laboratory quality plan
- Communication channels could include email, posters, newsletters, texts
- Incentive measures can improve user's awareness of laboratory policies and issues and improve quality; examples:
- Small gifts (lab trinkets, etc.)
- Recognition ("stars of the month" bulletin boards, newsletter mentions, etc.)
- Discounts on other services
- Contact information, for questions and interpretation, should be provided along with reported results
- Training should be provided to lab personnel to improve external communications
- To inform lab users of pertinent changes or issues, information flow within the laboratory should include appropriate branch points
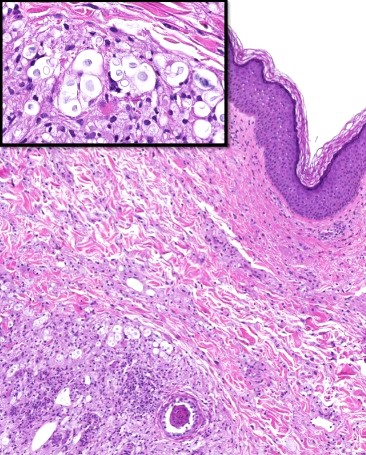
Microscopic (histologic) images
Videos
Critical values in clinical chemistry
Critical communications in healthcare
Communication in customer service
Practice question #1
A 56 year old woman was hospitalized due to a closed hip fracture. The patient has a 15 year history of diabetes mellitus type II and atrial fibrillation. She has been on insulin and warfarin to manage her conditions. Partial thromboplastin time (PTT) is in the normal range but prothrombin time (PT) and international normalized ration (INR) are increased at 43 seconds and 5.2, respectively. What is the best next step the performing lab technician should take?
- Call the lab director
- Call the ordering physician (or nurse)
- Call the pathology resident / attending
- Send the results to the ordering physician (or nurse)
- Verify or repeat the test
Practice answer #1
E. Verify or repeat the test. The first step is to verify and repeat the test if necessary. Nowadays, the results are usually sent automatically after being confirmed. Thus, after verification, calling the ordering physician would be the next step.
Comment Here
Reference: Critical reporting systems and laboratory communications
Comment Here
Reference: Critical reporting systems and laboratory communications
Practice question #2
A basic metabolic panel (BMP) from a 40 year old outpatient male with unclear medical history includes a serum sodium of 119 mmol/L. After verifying the result, the lab technician attempted to call the clinic from which the sample was sent but there was no answer. What is the next step that the technician should take?
- Call 911
- Call the lab supervisor / attending pathologist
- Call the patient’s emergency contact
- Call the patient’s family phone number
- Call the patient’s phone number
Practice answer #2
B. Call the lab supervisor / attending pathologist. After failing to reach the patient’s provider clinic, a lab technician's next step is to notify the lab supervisor / attending pathologist to take on the follow up. Since calling the patient may be needed, personnel with expertise in clinical medicine should undertake this responsibility in order to explain the results to the patient.
Comment Here
Reference: Critical reporting systems and laboratory communications
Comment Here
Reference: Critical reporting systems and laboratory communications