Table of Contents
Definition / general | Essential features | Embryology | Anatomy | Physiology | Diagrams / tables | Clinical implications | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2 | Practice question #3 | Practice answer #3Cite this page: Lee JTH, Gupta R. Anatomy & histology. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/larynxanatomy.html. Accessed September 24th, 2025.
Definition / general
- Larynx is a complex tubular organ that extends from the tip of the epiglottis at the superior aspect to the inferior border of the cricoid cartilage
- Required for phonation and to prevent aspiration of ingested food or liquid
- Hypopharynx is the inferiormost part of the pharynx and plays an essential role in swallowing
- Trachea or the windpipe is the passage for air from the nose to the lung
Essential features
- Larynx is essential for phonation and to prevent aspiration of swallowed material
- Extends from the superior tip of the epiglottis to the inferior border of the cricoid cartilage
- Lined by pseudostratified ciliated respiratory mucosa in most parts except the vocal cords that are lined by squamous epithelium
- Submucosal tissues include minor salivary gland tissue and cartilage
- Hypopharynx is the inferiormost part of the pharynx and the point where the pharynx divides into the larynx anteriorly and the esophagus posteriorly
- Trachea allows passage of air from the nose to the lungs
Embryology
- Larynx develops from the endodermal lining and adjacent mesenchyme of the foregut
- Supraglottic region develops from the third and fourth brachial pouches
- Glottic and subglottic region develops from the sixth brachial pouch
- Larynx descends in the neck from the age of 18 - 24 months to achieve its adult position between the vertebrae C4 and C7 by the age of 6 years
- Pharynx develops from the branchial apparatus beginning at the fourth and fifth week of development
- Trachea develops from the foregut endoderm; the embryonic stage of the lower respiratory tract begins at approximately day 22, when the respiratory diverticulum forms on the ventral wall of the foregut endoderm
- Reference: Wenig: Atlas of Head and Neck Pathology, 3rd Edition, 2015
Anatomy
Larynx
Hypopharynx
Trachea
- Larynx is about 4 - 5 cm in length and 2 cm in diameter
- There is variation in size between genders and age; the larynx is smaller in women than men and larger in adults than children
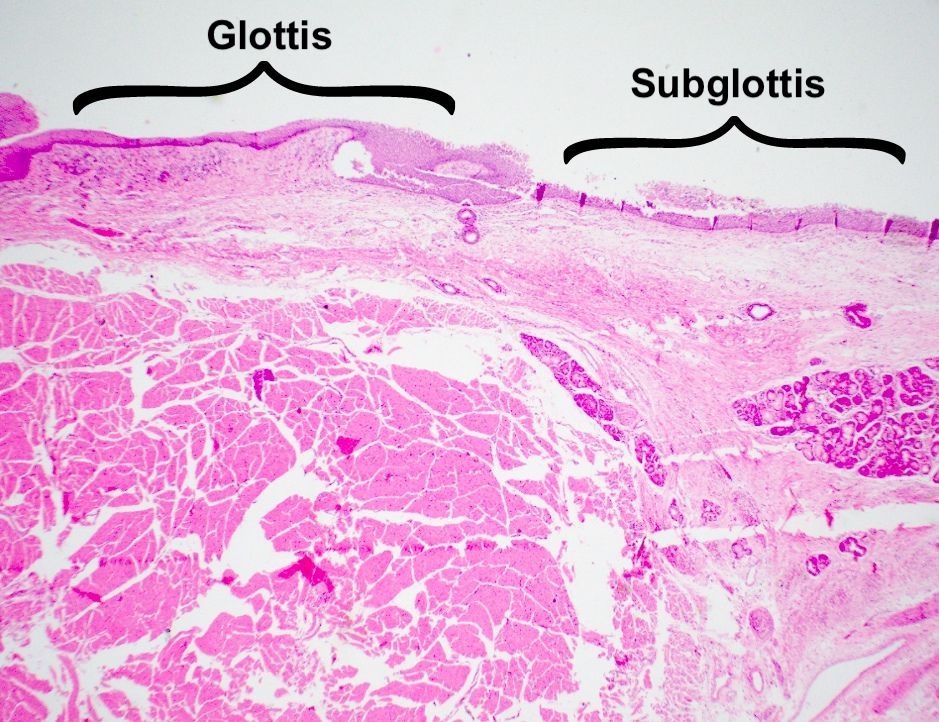
- Larynx is divided into 3 major regions: supraglottis, glottis and subglottis
- Supraglottis: region between the tip of epiglottis and true cord; it includes the aryepiglottic folds, false vocal cords and ventricles
- Glottis: region between the top of true vocal cord and 1 cm below; it includes the true vocal cords and the anterior commissure
- Subglottis: region between the lower border of the glottis and the inferior border of the cricoid cartilage
- Laryngeal skeleton includes 9 cartilages; 3 unpaired and 3 paired
- 3 unpaired cartilages: epiglottis, thyroid and cricoid
- Epiglottic cartilage
- Leaf shaped elastic cartilage
- Main function is to close the laryngeal inlet during swallowing to prevent aspiration
- Connected to the arytenoids by the aryepiglottic folds
- Connected to the thyroid cartilage by the thyroepiglottic ligament
- Thyroid cartilage
- Largest of the laryngeal cartilages
- Shield / butterfly shaped hyaline cartilage
- Extends from the hyoid bone to the cricoid cartilage
- Supports and protects the vocal cords
- Attachment for several muscles of the larynx
- Participates in changing the pitch of the voice
- Forms the Adam's apple
- Cricoid cartilage
- Signet ring shaped hyaline cartilage
- Maintains the airway patency
- Forms the inferior border of the larynx and encircles the trachea
- Epiglottic cartilage
- 3 paired cartilages: arytenoid, corniculate and cuneiform
- Arytenoid cartilage
- Paired pyramid shaped hyaline cartilages
- Located superior to the cricoid cartilage and forms the cricoarytenoid joint
- Provide support to and control the tension of the vocal cords critical for phonation
- Cuneiform (Wrisberg cartilage) and corniculate cartilages (cartilages of Santorini)
- Tiny cartilages sitting on the apices of the arytenoid cartilages and are enclosed within the aryepiglottic folds
- Their main function is to stiffen the aryepiglottic fold to prevent aspiration during swallowing
- Arytenoid cartilage
- 3 unpaired cartilages: epiglottis, thyroid and cricoid
- Ligaments and membranes of the larynx hold the hyoid bone and the cartilages of the larynx to form 1 functional unit
- Intrinsic ligaments connect the laryngeal cartilages
- Cricothyroid, cricocorniculate, thyroepiglottic, thyroarytenoid and the arytenoidepiglottic ligaments
- Cricovocal membrane (conus elasticus) and vocal cord ligament form the true vocal cords when covered by mucosa
- Quadrangular membrane and the vestibular ligament form the false vocal cords when covered by mucosa
- Extrinsic ligaments attach the larynx to other structures, like the hyoid and trachea: the thyrohyoid, hyoepiglottic and cricotracheal ligaments
- Intrinsic ligaments connect the laryngeal cartilages
- Larynx also has intrinsic and extrinsic muscles
- Intrinsic muscles are required for voice production
- Attachments spanning the laryngeal cartilages bring about movement for phonation
- All intrinsic muscles are paired except for the transverse arytenoid muscle
- Muscles causing adduction and closure of laryngeal inlet: oblique arytenoid muscle, aryepiglottic muscle, transverse arytenoid muscles
- Muscles causing abduction and widening of the laryngeal inlet: thyroepiglottic muscle
- Muscles modulating the tension in the vocal folds: thyroarytenoid (relax), lateral cricoarytenoid (adduct), posterior cricoarytenoid (abduct), cricothyroid (tense), vocalis (tense)
- Extrinsic muscles are required to move the larynx in its entirety; some extrinsic muscles attach directly to the larynx, while others are attached to the hyoid or the pharyngeal wall
- Extrinsic muscle attached directly to the larynx
- Cause laryngeal elevation: thyrohyoid and inferior pharyngeal constrictors
- Cause laryngeal depression: sternothyroid muscle
- Extrinsic muscles not attached directly to the larynx
- Cause laryngeal elevation: stylohyoid, hyoglossus, geniohyoid, mylohyoid, digastric
- Cause laryngeal depression: omohyoid, sternohyoid
- Elevates the pharyngeal wall: middle pharyngeal constrictor, stylopharyngeus, palatopharyngeus
- Extrinsic muscle attached directly to the larynx
- Intrinsic muscles are required for voice production
- Spaces associated with the larynx
- Pre-epiglottic space and paraglottic space
- These spaces contain adipose and connective tissues with lymphatics and blood vessels
- No lymph nodes are present in these spaces
- Reinke space
- Loose connective tissue within the lamina propria of the true vocal cord lying between the vocal cord ligament and surface squamous epithelium
- It is the common place for vocal cord polyp
- Pre-epiglottic space and paraglottic space
- Vascular supply and drainage of the larynx: superior and inferior laryngeal arteries with its parallel veins
- Larynx receives blood supply from both the external carotid artery and the subclavian artery
- Superior laryngeal arteries: external carotid artery gives rise to the superior thyroid artery that further branches into superior laryngeal arteries
- Inferior laryngeal arteries: subclavian artery gives rise to inferior thyroid artery that further branches to inferior laryngeal arteries
- Larynx drains into both the internal jugular and subclavian veins
- Superior and middle laryngeal vein drains into the internal jugular vein
- Inferior laryngeal vein drains into subclavian vein
- Larynx receives blood supply from both the external carotid artery and the subclavian artery
- Lymphatic system of larynx
- Superior half of the larynx above the vocal cords drains into jugulodigastric and midjugular nodes
- Inferior half of the larynx drains into pretracheal, paratracheal and inferior jugular nodes
- Innervation of the larynx is from 2 sets of nerves from the vagus nerve (tenth cranial nerve)
- Superior laryngeal nerve
- Internal branch provides sensory and autonomic innervation to the mucosa superior to the glottis; visceral afferents to the epiglottis also assist in taste
- External branch supplies motor innervation and visceral efferent to the cricothyroid and inferior pharyngeal constrictor muscles
- Recurrent laryngeal nerve (StatPearls: Anatomy, Head and Neck, Larynx Recurrent Laryngeal Nerve [Accessed 18 July 2024])
- Provides motor innervation to all intrinsic muscles of the larynx except the cricothyroid muscle; hence, critical for phonation
- Provides sensory innervation inferior to the glottis and motor innervation to intrinsic muscles of the larynx
- Superior laryngeal nerve
- Reference: StatPearls: Anatomy, Head and Neck - Larynx [Accessed 18 July 2024]
Hypopharynx
- Also known as laryngopharynx
- Most caudal portion of the pharynx
- Point at which the pharynx divides anteriorly into the larynx and posteriorly into the esophagus
- Located inferior to the epiglottis and is bordered by the pharyngoepiglottic fold superiorly and the upper esophageal sphincter inferiorly
- 3 main structures in the hypopharynx include the posterior pharyngeal wall, the right and left pyriform sinuses and the postcricoid area
- Reference: StatPearls: Anatomy, Head and Neck: Laryngopharynx [Accessed 24 September 2024]
Trachea
- Most proximal portion of tracheobronchial tree; it originates at the inferior edge of the larynx and connects to the main stem bronchus and the left bronchus via carina
- Tracheal diameter is ~24 - 26 mm in adult men and 22 - 24 mm in women
- Trachea is broader in the proximal region as compared to the distal segment
- Has 16 - 20 C shaped cartilage rings with a narrow thin membrane connecting each of the tracheal rings; the posterior aspect of the trachea is adjacent to the anterior esophagus
- Arterial supply of the proximal trachea consists of the tracheoesophageal branches of the inferior thyroid artery and small branches from the subclavian, internal mammary and innominate artery; the distal trachea, with carina and bronchi, are supplied by the bronchial arteries, which usually originate from the proximal descending aorta
- Reference: StatPearls: Anatomy, Thorax, Tracheobronchial Tree [Accessed 24 September 2024]
Physiology
Larynx
Hypopharynx
Trachea
- Main functions of larynx include phonation, facilitation of respiration and protection of the lower airways
- Respiratory and phonatory functions are initiated voluntarily but regulated involuntarily
- Protective function is entirely reflexive and involuntary
- Phonation
- Air passed from the lungs to the closed vocal folds during exhalation causes the folds to vibrate and produce sound
- Length and tightness of the folds affect the pitch and voice
- Longer folds are seen in a larger larynx and produce lower pitch and deeper voice (e.g., as seen in most men)
- Protection of airway
- Larynx closes and moves upwards during swallowing, causing the epiglottis to close off the trachea
- This helps prevent aspiration of food and water into the lungs or choking from obstruction in the trachea
- Respiration
- Vocal folds remain open during breathing
- Larynx can be signaled to open wider to increase airflow during heavy breathing
- Reference: Am J Med 1997;103:9S
Hypopharynx
- Main function of the hypopharynx is to ensure the appropriate passage of food, liquids and air
- Action of swallowing is essential for the food and liquids to pass into the stomach and avoid aspiration into the lungs
- Reference: StatPearls: Anatomy, Head and Neck: Laryngopharynx [Accessed 24 September 2024]
Trachea
- Primary function of the trachea is to allow passage of inspired and expired air into and out of the lung (StatPearls: Anatomy, Thorax, Tracheobronchial Tree [Accessed 24 September 2024])
Diagrams / tables
Images hosted on other servers:
Clinical implications
- Every cell layer of the larynx can give rise to or can be affected by a variety of nonneoplastic and neoplastic diseases
- Symptoms are usually voice changes / hoarseness and dysphagia if there is obstruction
Nonneoplastic lesions of larynx (Wenig: Atlas of Head and Neck Pathology, 3rd Edition, 2015)
- Vocal cord nodule / polyp or singer nodule
- Common reactive stromal lesion related to inflammation or trauma from voice abuse, alcohol and smoking
- Often involves the anterior or middle third of the vocal cord and Reinke space
- Histologic subtypes include edematous myxoid, fibrous, vascular, hyaline and mixed
- Prone to recur
- Laryngocele
- Sac-like dilatation at the ventricle that contains air and maintains open communication with the laryngeal lumen
- Association with occupation involving excessive increased intralaryngeal pressure, such as musician, glassblower and weightlifters
- Laryngeal cyst
- Caused by accumulation of secretion associated with obstruction of mucous gland ducts in the saccule
- Single or multiple lesions involving the supraglottis
- Contact ulcer
- Nodular lesion with surface ulceration
- Generally secondary to chronic diseases (such as gastroesophageal reflux), shouting, persistent cough and postintubational trauma
- Shows granulation tissue and fibrinoid necrosis
- Laryngeal amyloidosis
- Extracellular accumulation of amyloid, either localized or associated with systemic disease
- Appears macroscopically as a gray-white nodule
- Histologically demonstrates amorphous eosinophilic material
- Congophilic with apple green birefringence
- May show associated multinucleate foreign body type giant cell response
- Infectious disease of larynx
- Viral infections such as respiratory viruses and herpes simplex virus
- Acute epiglottitis by Haemophilus influenzae can cause airway compromise in the pediatric age group due to edema of the vallecula and extending to the posterior pharyngeal wall
- Autoimmune diseases such as systemic lupus erythematosus (SLE), rheumatoid arthritis, Sjögren syndrome and granulomatosis with polyangiitis, Crohn's disease and IgG4 related disease involving the submucosal minor salivary glands, soft tissues and vessels
- Laryngeal benign epithelial changes such as hyperplasia, parakeratosis and ulceration
- Clinical appearance as leukoplakia
- Requires histologic examination to exclude dysplasia and malignancy
- Requires histologic examination to exclude submucosal lesions inciting a reaction
Neoplasms of larynx, hypopharynx and trachea (Wenig: Atlas of Head and Neck Pathology, 3rd Edition, 2015)
- Larynx is affected most commonly by the neoplasms seen in this region; neoplasms of the trachea are rare
- Benign epithelial neoplasms
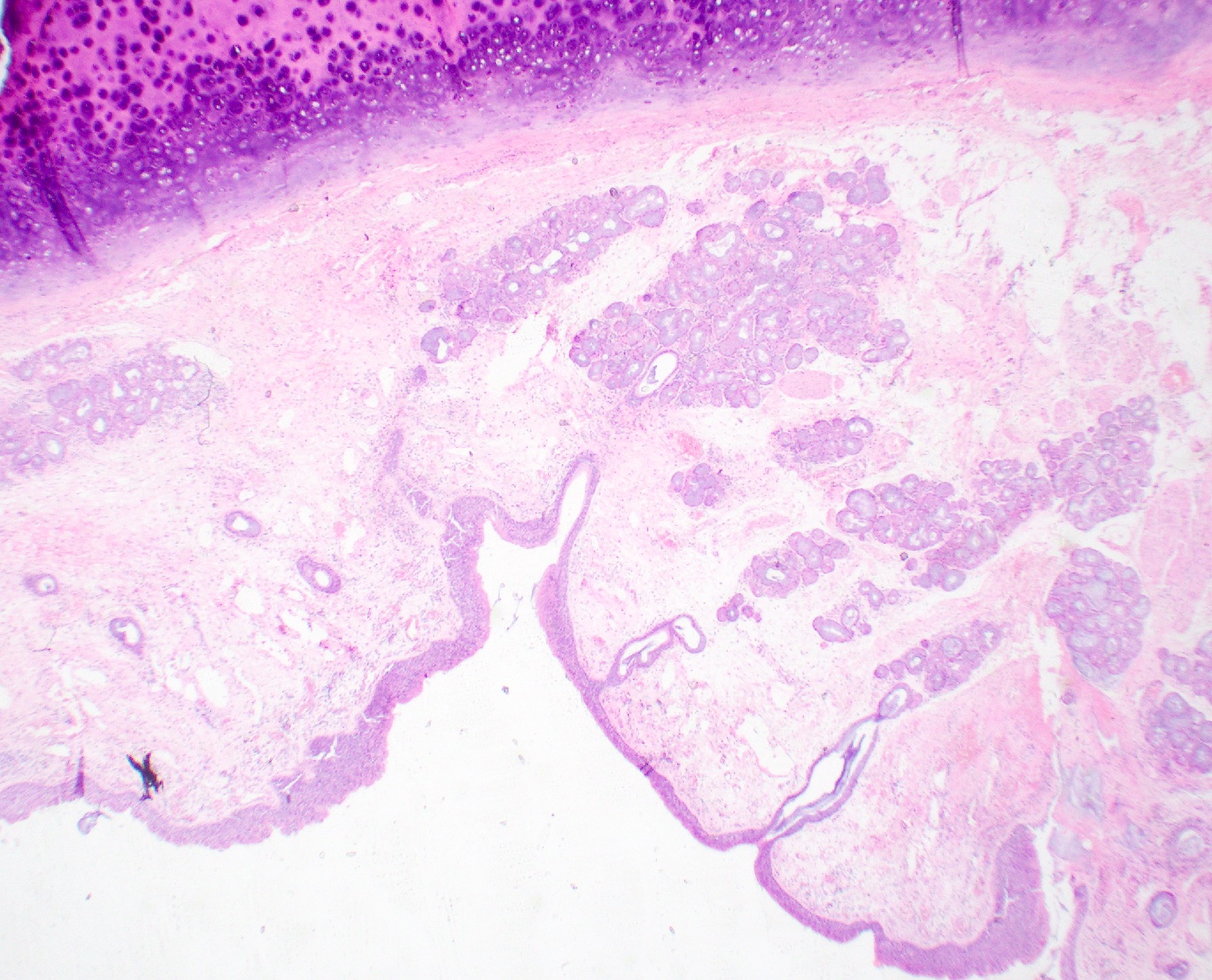
- Squamous papilloma (nonkeratinizing) / papillomatosis
- Most common benign warty neoplasm in larynx, caused by low risk human papillomavirus infection (HPV) (HPV 6 and 11)
- Junction between supraglottis - glottis and glottis - subglottis
- Juvenile onset (< 20 years) and adult onset
- Multiple recurrences and complications such as asphyxia, infection and transformation to carcinoma
- Keratinizing papilloma occurs in adults and is associated with smoking
- Histologically shows papillary fronds with fibrovascular cores lined by hyperplastic benign squamous epithelium
- Histologic examination is essential to exclude this lesion from verrucous carcinoma and exophytic squamous cell carcinoma
- Squamous papilloma (nonkeratinizing) / papillomatosis
- Benign salivary gland neoplasms
- Pleomorphic adenoma
- Oncocytic cyst
- Warthin tumors
- Benign mesenchymal neoplasms
- Hemangioma
- Chondroma
- Neurofibroma
- Inflammatory myofibroblastic tumor
- Granular cell tumor
- Premalignant
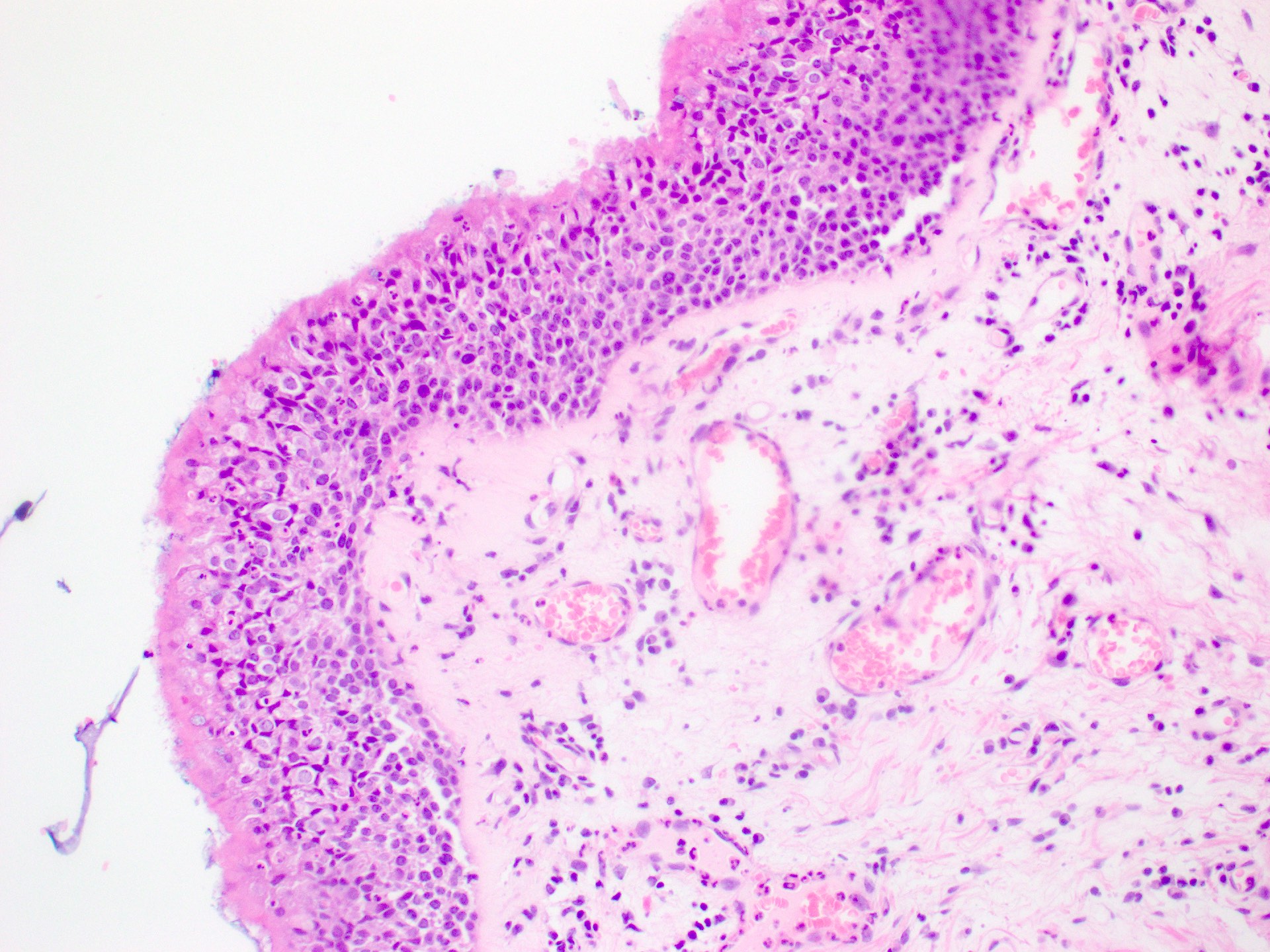
- Laryngeal epithelial dysplasia
- Accumulation of genetic alteration and may progress into invasive squamous cell carcinoma
- Caused by smoking and alcohol
- Vocal cords are often affected and produce a hot potato voice
- May be asymptomatic if supraglottis or subglottis are involved
- Histologically, the squamous cells show a lack of maturation, altered N:C ratio with nuclear enlargement and hyperchromasia, nuclear pleomorphism and mitoses
- Laryngeal epithelial dysplasia
- Malignant
- Squamous cell carcinoma is the most common epithelial malignancy
- Similar etiologic and histologic features as observed in the oral cavity
- Most common sites include the vocal cords and pyriform sinuses
- Adenoid cystic carcinoma and mucoepidermoid carcinoma are the most common minor salivary gland carcinomas
- Neuroendocrine tumors may be rarely seen
- Chondrosarcoma arises from the laryngeal cartilage
- Rhabdomyosarcoma, angiosarcoma and liposarcoma can arise from the soft tissues
- Squamous cell carcinoma is the most common epithelial malignancy
Gross description
- See Anatomy
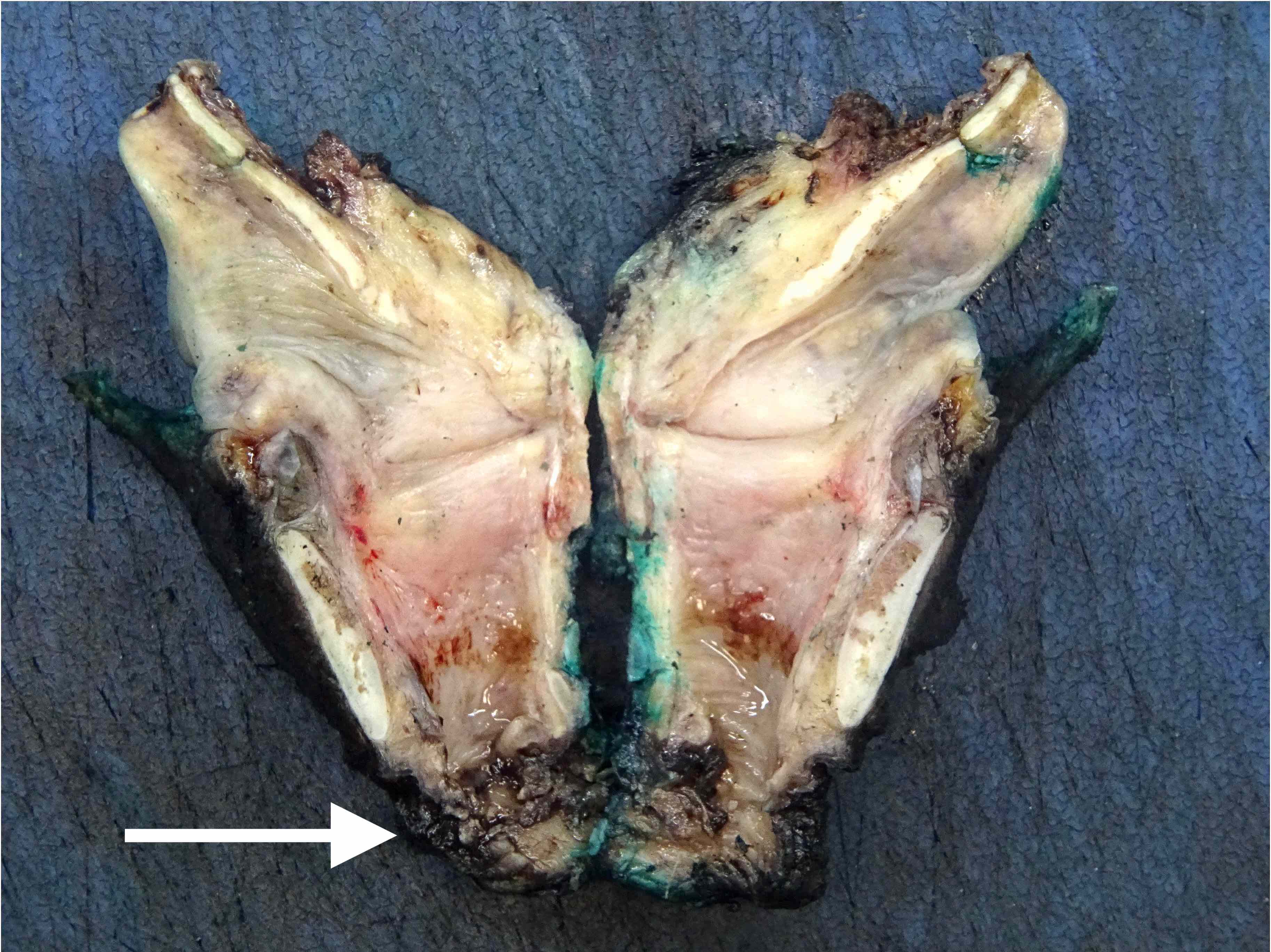
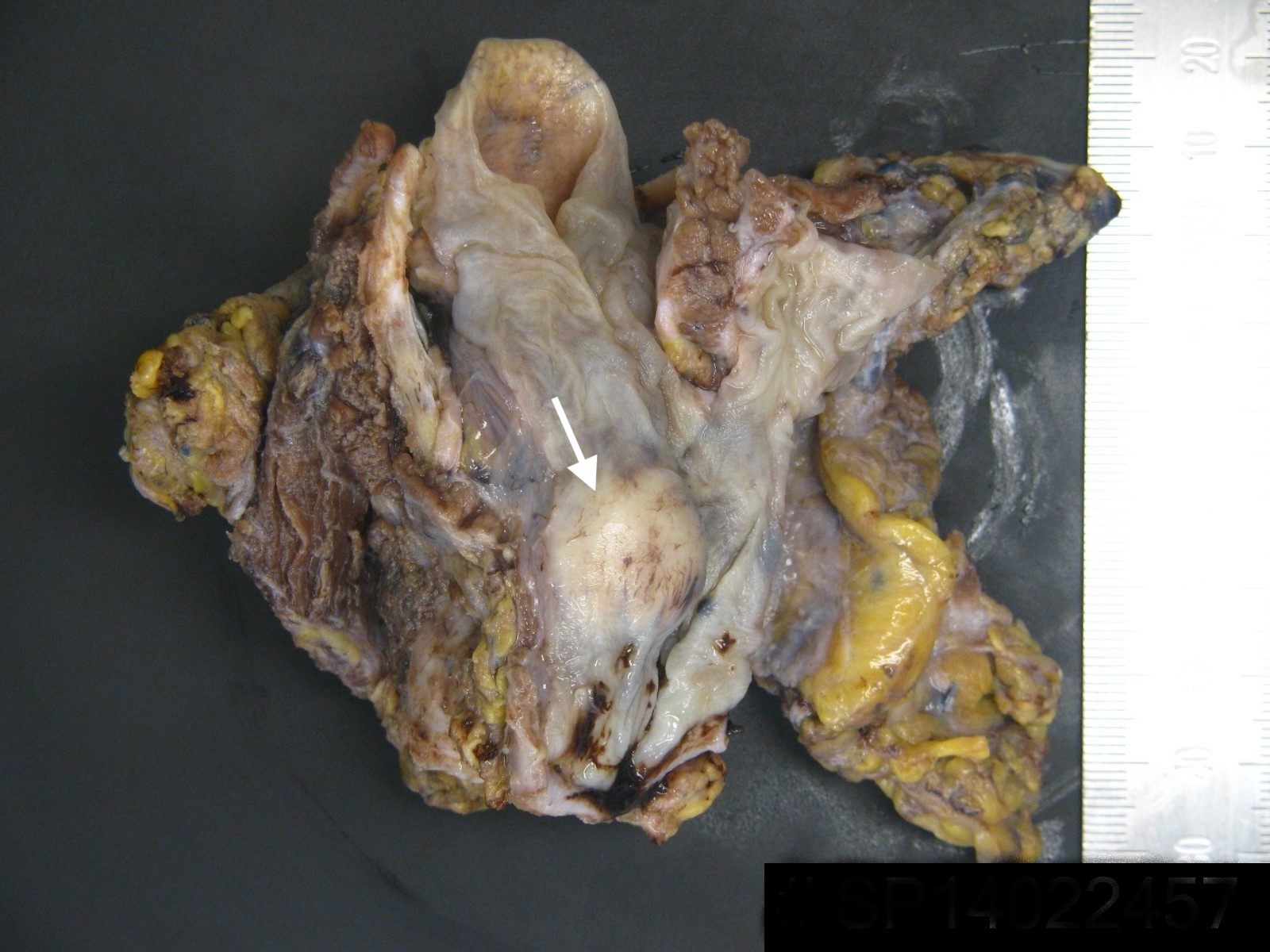
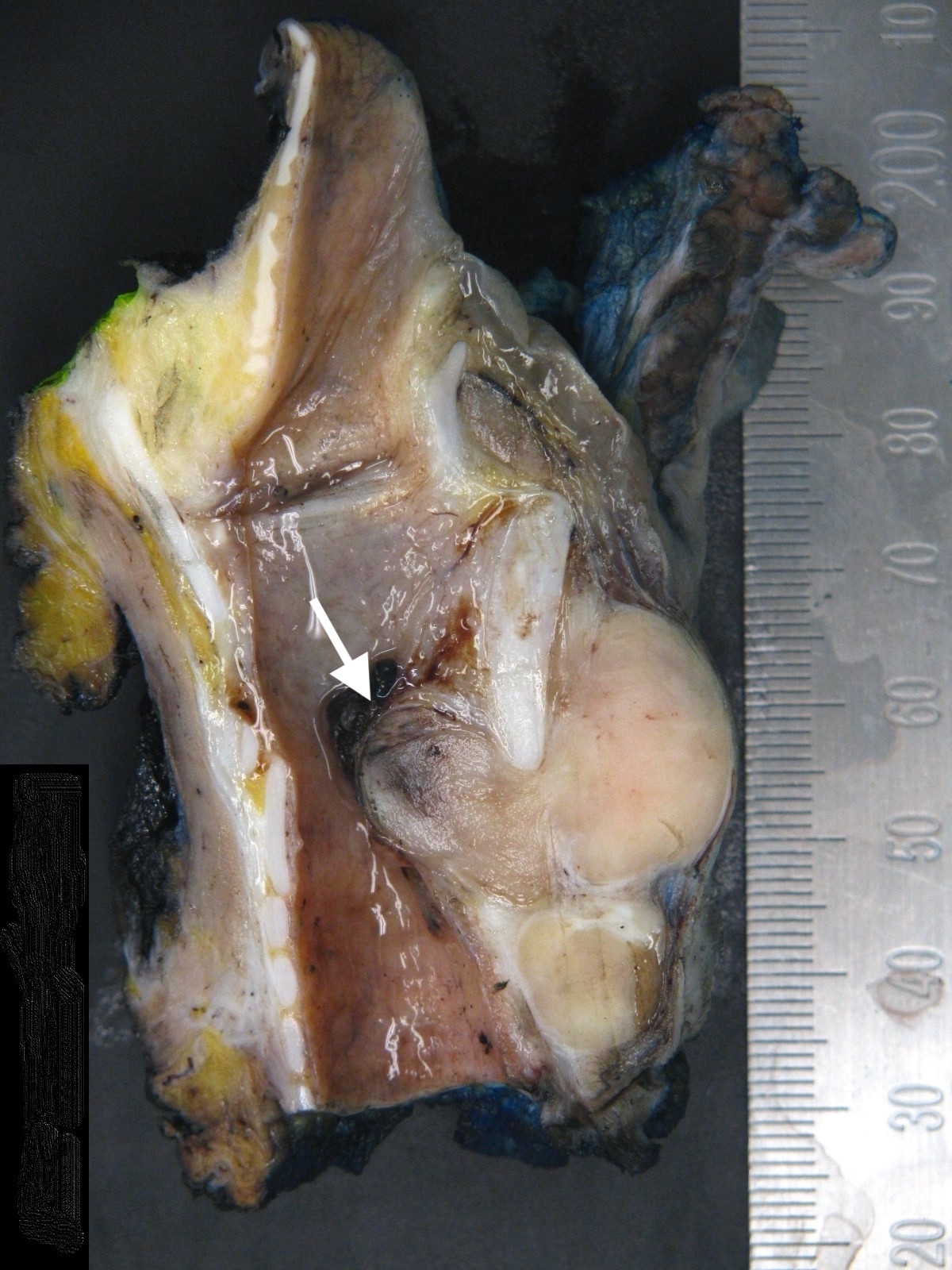
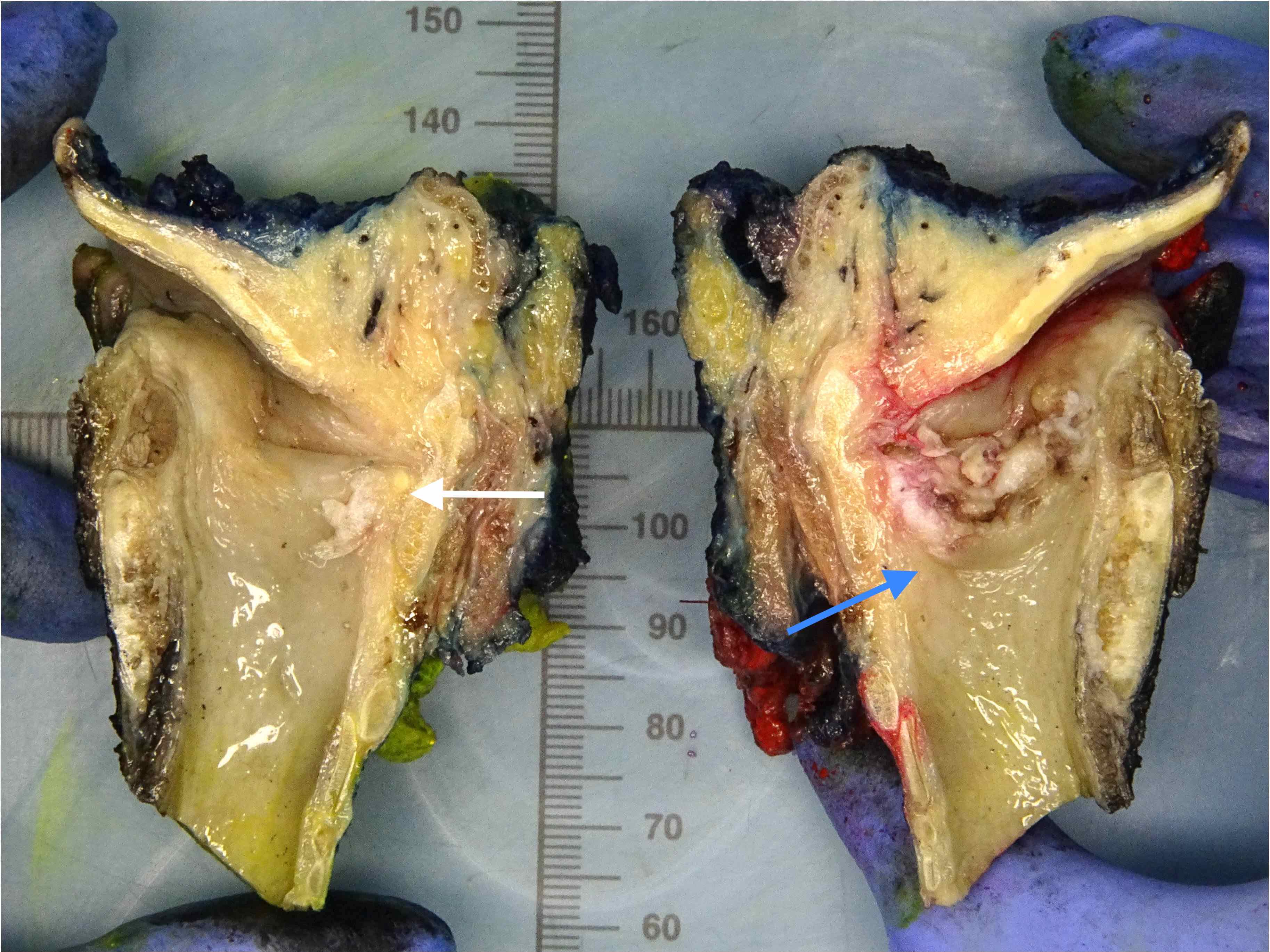
Gross images
Microscopic (histologic) description
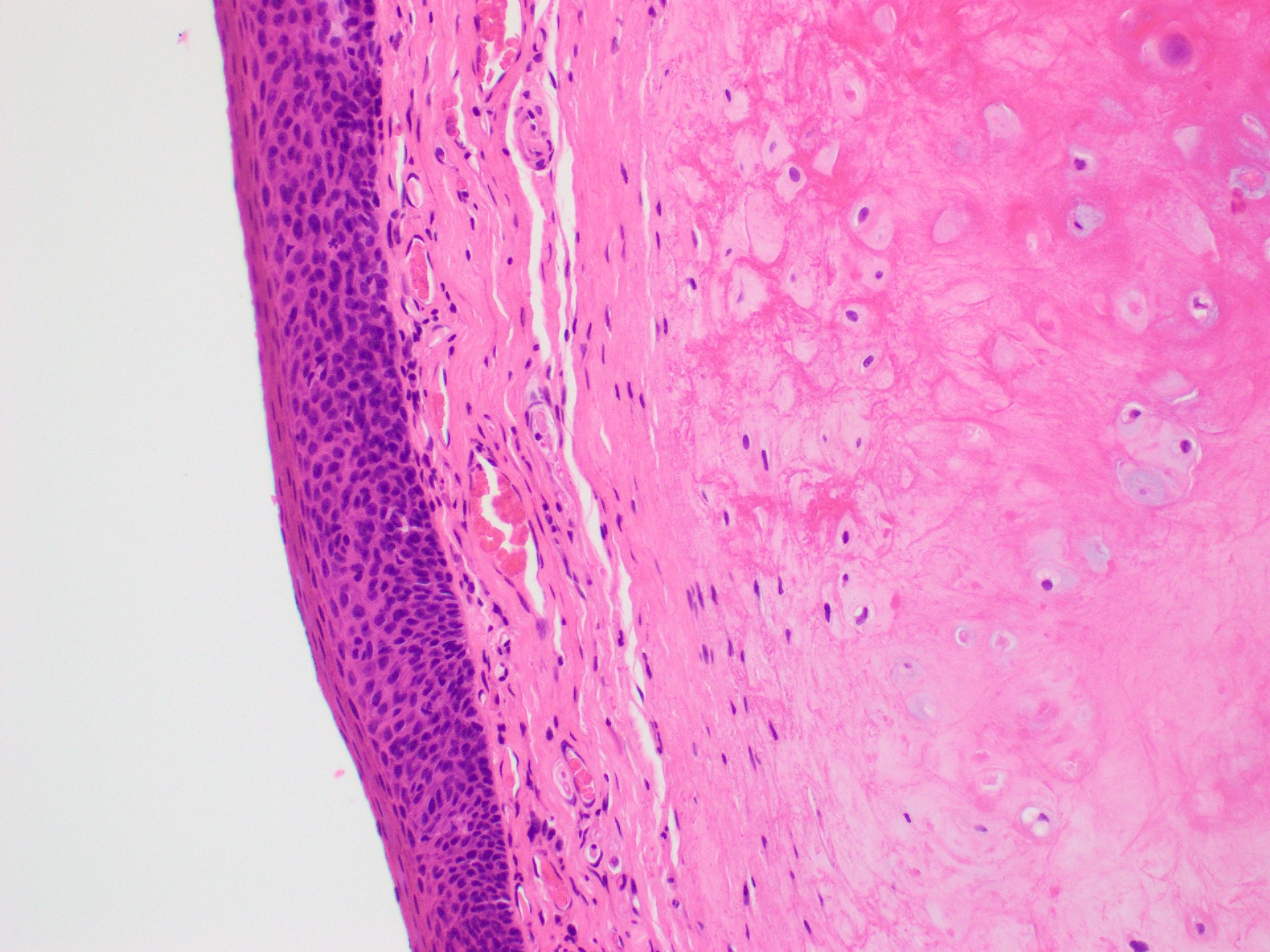
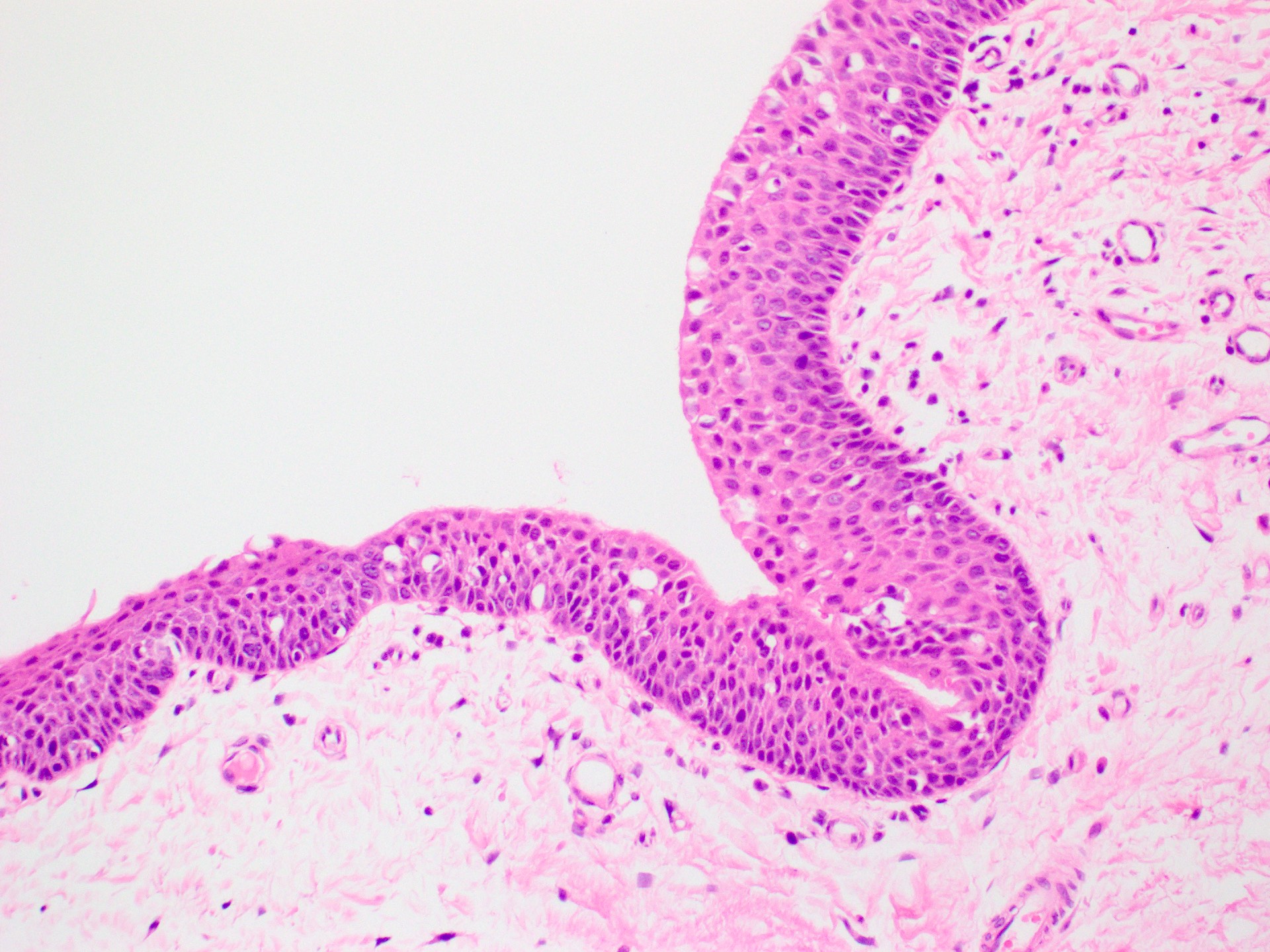
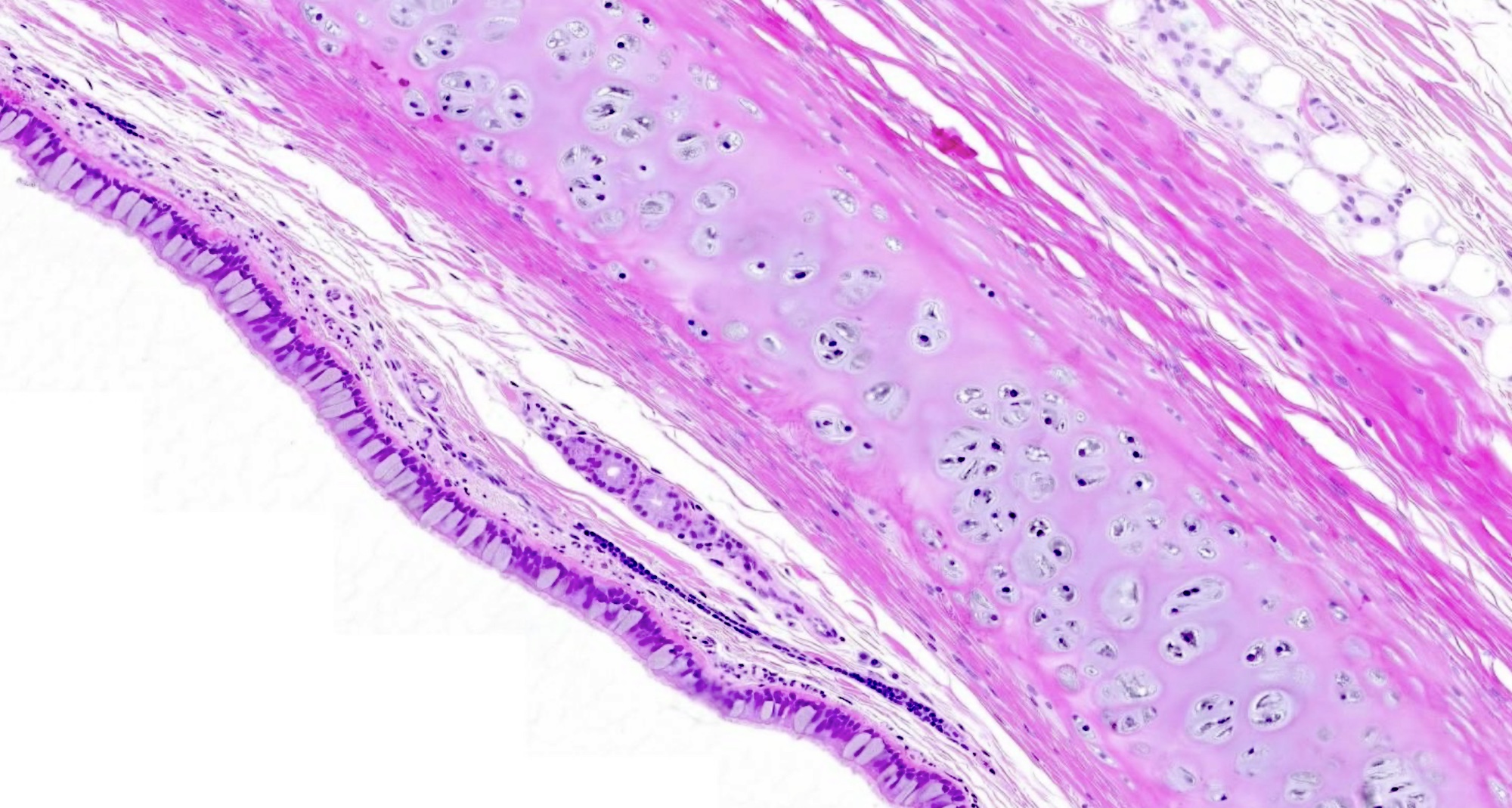
- Histological layers of the larynx include mucosa (epithelium and lamina propria), submucosa, cartilage and adventitia (StatPearls: Anatomy, Head and Neck, Larynx Vocal Cords [Accessed 24 September 2024])
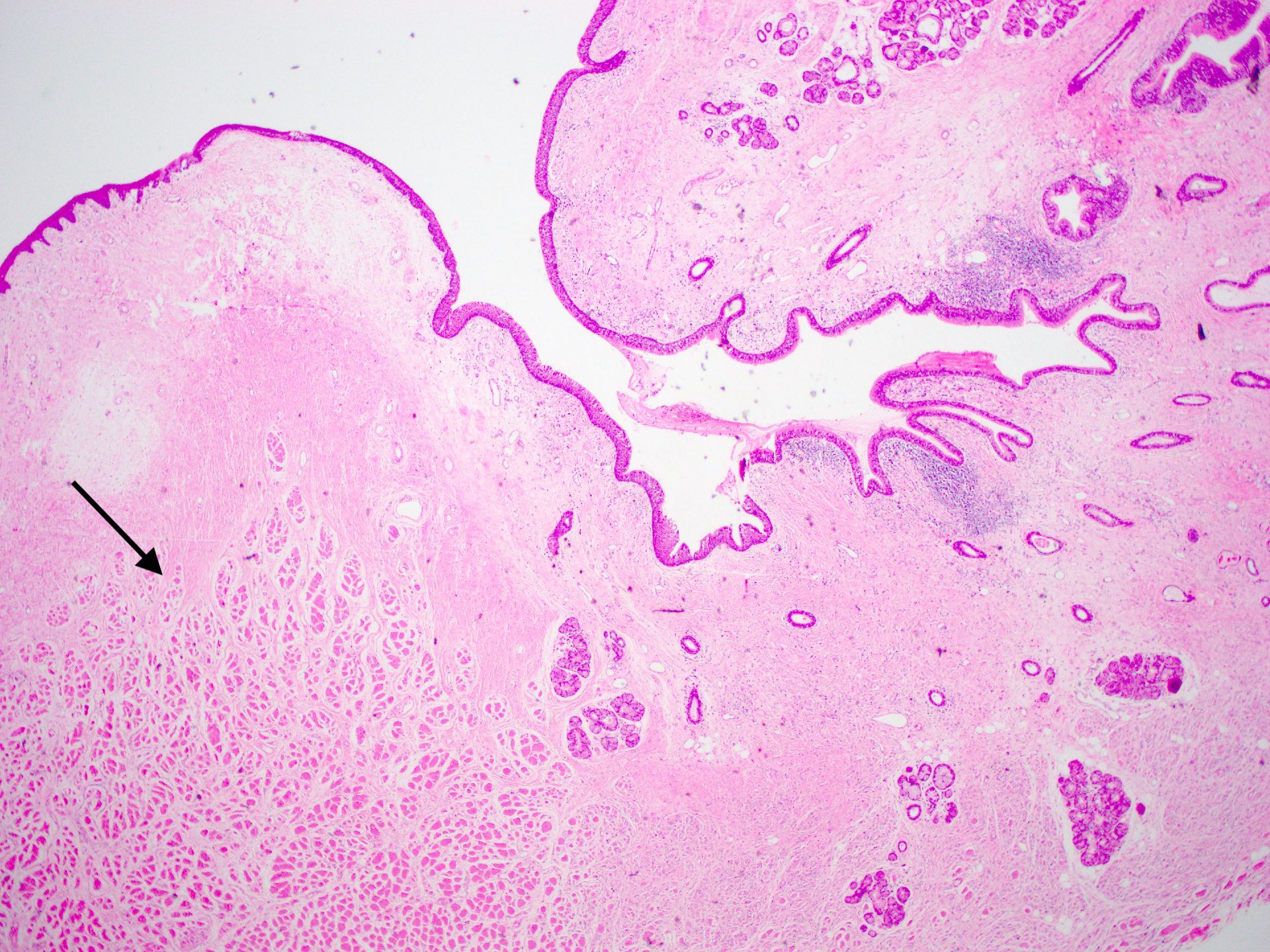
- Mucosa
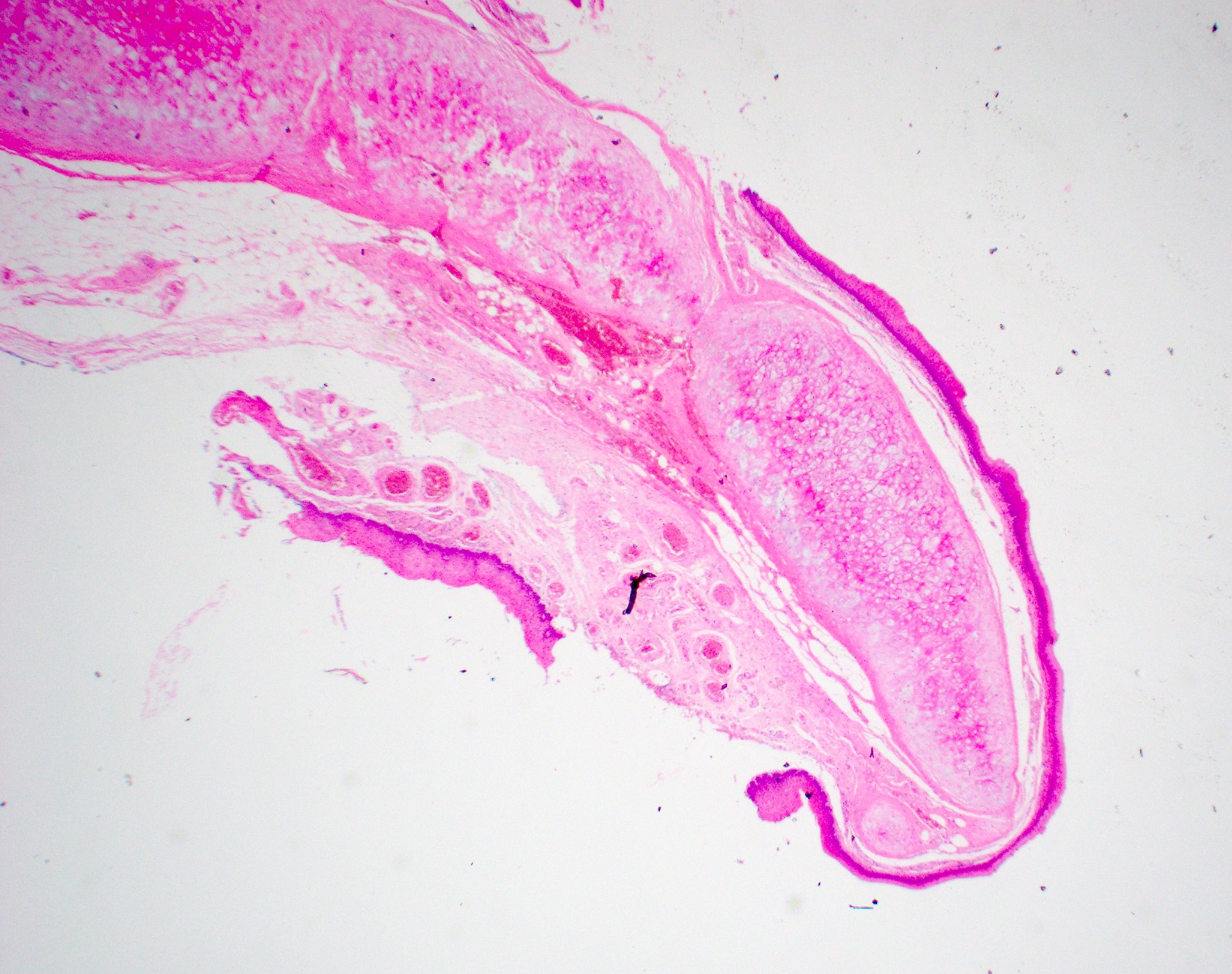
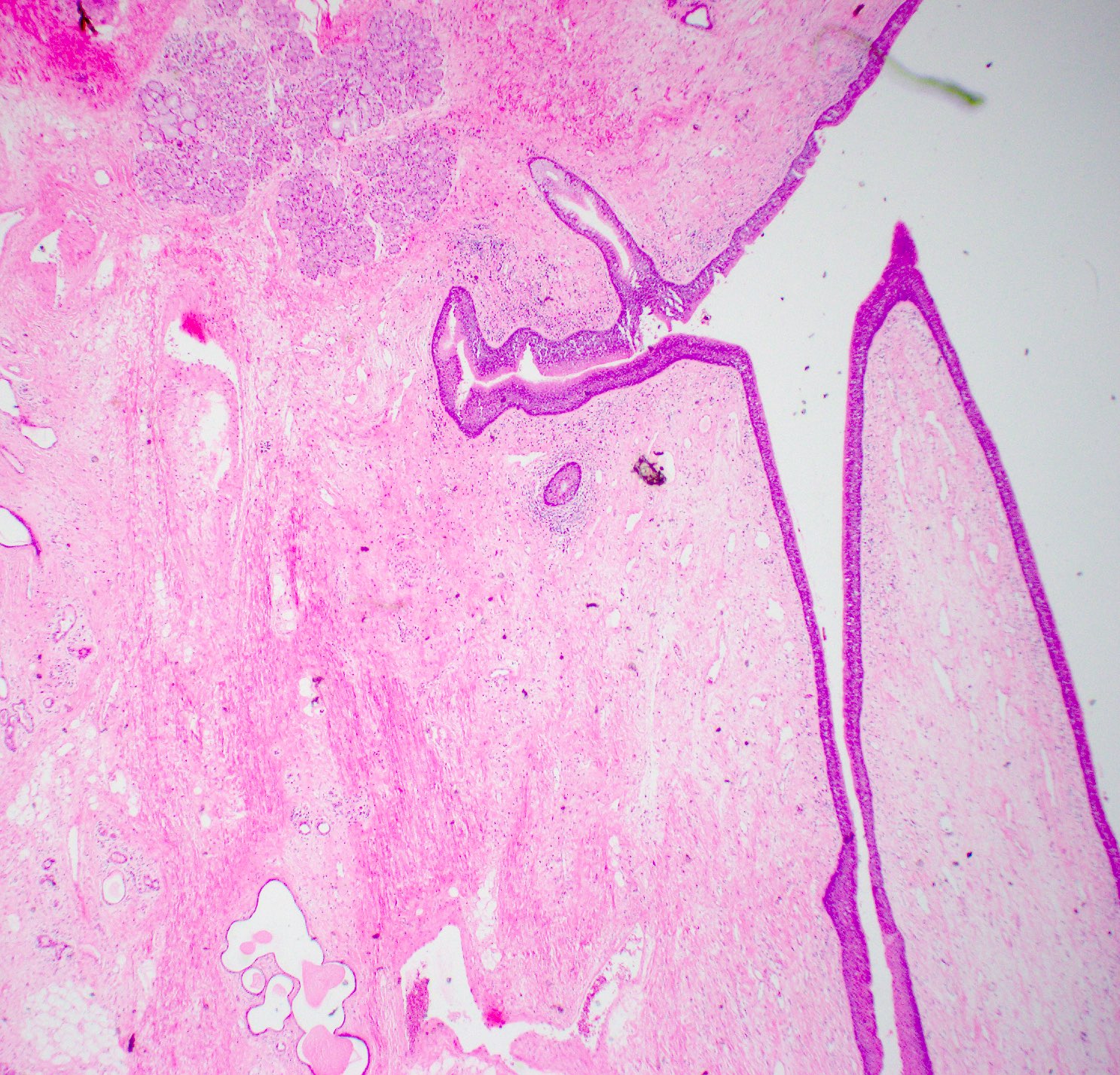
- Nonkeratinized stratified squamous epithelium: lines the epiglottis and true vocal cord
- Pseudostratified ciliated respiratory epithelium: lines the false cord, ventricle and subglottis
- Transitional type epithelium is present in between the ciliated respiratory mucosa of supraglottis or subglottis and the squamous epithelium of the true vocal cord
- Mucosa
- Lamina propria is composed of loose stromal tissue with numerous small vessels, lymphatic channels and nerves
- Seromucinous glands are present immediately beneath the epithelium except in true vocal cord region
- Vocal cord has less vessels and mostly lymphatic channels; thick vocalis muscle is present in the submucosa
- Adipose tissue can be seen intermingling with lamina propria and skeletal muscle of the larynx
- Laryngeal cartilage: hyaline cartilage and elastic cartilage
- Cartilage undergoes ossification with aging
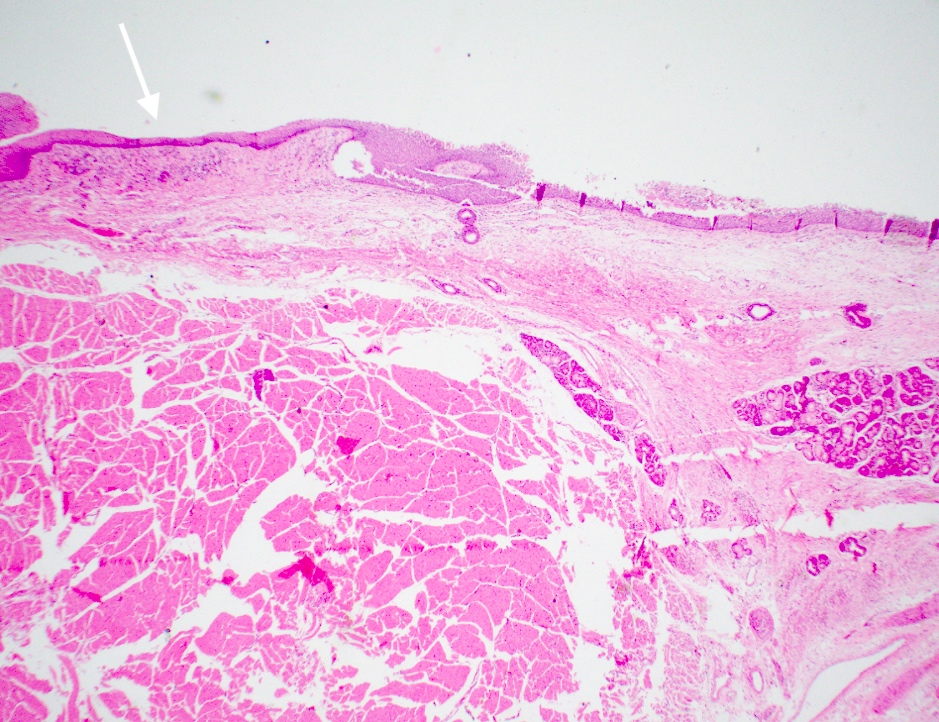
- Histologic layers of the hypopharynx include
- Squamous mucosa
- Skeletal muscle for voluntary deglutition
- Histologic layers of the trachea include
- Mucosa with suedostratified ciliated columnar epithelium
- Submucosal seromucinous glands
- Hyaline cartilage in the tracheal rings
Microscopic (histologic) images
Practice question #1
Practice answer #1
C. True vocal cord. The true vocal cord is lined by stratified squamous epithelium and shows thick vocalis muscle in the submucosa. Answer A is incorrect because there would not be thick vocalis muscle in the submucosa of the epiglottis. Answers B and D are incorrect because both the subglottis and the ventricle are lined by ciliated pseudostratified squamous epithelium.
Comment Here
Reference: Larynx, hypopharynx & trachea - Anatomy & histology
Comment Here
Reference: Larynx, hypopharynx & trachea - Anatomy & histology
Practice question #2
What tissue types are characteristically found in the trachea?
- Respiratory mucosa, seromucinous glands and elastic cartilage
- Respiratory mucosa, seromucinous glands and hyaline cartilage
- Squamous mucosa, seromucinous glands and elastic cartilage
- Squamous mucosa, seromucinous glands and hyaline cartilage
Practice answer #2
B. Respiratory mucosa, seromucinous glands and hyaline cartilage. The trachea is lined by pseudostratified ciliated columnar epithelium or respiratory mucosa with hyaline cartilage to facilitate respiration. Answer A is incorrect because elastic cartilage is not found in the trachea. Answers C and D are incorrect because, in addition to the lack of elastic cartilage in the trachea, it is lined by respiratory mucosa, not squamous mucosa.
Comment Here
Reference: Larynx, hypopharynx & trachea - Anatomy & histology
Comment Here
Reference: Larynx, hypopharynx & trachea - Anatomy & histology
Practice question #3
Which statement is true about Reinke space?
- It contains sparsely vascular submucosal stromal tissue
- It is an empty space in between the vocal cord ligament and epithelium
- Reinke space edema is not associated with smoking, phonotrauma or laryngopharyngeal reflux
- Vocal cord polyp that arises in this area is always malignant
Practice answer #3
A. It contains sparsely vascular submucosal stromal tissue. Reinke space is not an empty space; it contains loose stromal tissue with vascular supply. Answer B is incorrect because it is not an empty space. Answer C is incorrect because smoking, phonotrauma and laryngopharyngeal reflux are potential etiologies of Reinke space edema. Answer D is incorrect because a vocal cord polyp is not a malignant neoplasm; rather, it can arise from severe edema in this space that causes a polyp resulting from balloon-like swelling of the vocal folds secondary to subepithelial expansion of the superficial layer of the lamina propria.
Comment Here
Reference: Larynx, hypopharynx & trachea - Anatomy & histology
Comment Here
Reference: Larynx, hypopharynx & trachea - Anatomy & histology