Table of Contents
Definition / general | Essential features | Terminology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Busca A, Parra-Herran C. Calcification. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/ovarynontumorcalcification.html. Accessed August 4th, 2025.
Definition / general
- Ovarian calcifications are commonly found in the context of a neoplasm (mature teratoma, mucinous cystadenoma, serous neoplasia, etc.) or as incidental findings in grossly normal ovaries
Essential features
- Ovarian calcifications can be idiopathic or associated with benign or malignant conditions (endometriosis, teratoma, mucinous lesions, serous neoplasms, etc.)
- Calcifications are divided into psammomatous (psammoma bodies) and nonpsammomatous
- Calcifications associated with a neoplasm do not need to be reported but identifying psammomatous calcifications in an otherwise normal ovarian specimen should prompt additional sampling to rule out the possibility of an underlying serous neoplasm
Terminology
- Calcifications, microcalcifications, osseous metaplasia
Sites
- Ovary
Pathophysiology
- Pathologic calcifications are metastatic (associated with hypercalcemia) or dystrophic (associated with normal calcemia); ovarian calcifications are considered dystrophic, due to calcium deposition in areas of cellular degeneration or necrosis
- Presence of stromal calcifications suggests a paracrine effect in the stromal cells in response to hormonal stimuli (Mod Pathol 2003;16:219)
- Gallstones spilled into the peritoneal cavity during laparoscopic cholecystectomy can lead to secondary cholelithiasis of the ovary (J Reprod Med 2007;52:968)
Etiology
- No known causes
Clinical features
- Calcifications are usually asymptomatic
Diagnosis
- Identified by ultrasound or at the time of histologic examination
Laboratory
- No specific laboratory findings
Radiology description
- Curvilinear or punctate echogenic foci, usually between 1 - 3 mm (Radiology 1996;198:415)
Prognostic factors
- In a study of 28 patients, the presence of large ovarian calcifications (> 5 mm) identified by imaging in otherwise normal ovaries remained stable and was not associated with ovarian neoplasms (Ultrasound Obstet Gynecol 2007;29:438)
Case reports
- 34 year old woman with ossification in the ovary associated with an old hemorrhagic cyst (Int J Clin Exp Pathol 2020;13:2356)
- 46 year old woman with ovarian ossification associated with endometriosis (Clin Exp Obstet Gynecol 2007;34:113)
- 65 year old woman with bilateral ovarian endometriotic cysts showing extensive ossification (Gynecological Surgery 2007;4:191)
Treatment
- Resection if symptomatic, rupture or suspicion for neoplastic process
Gross description
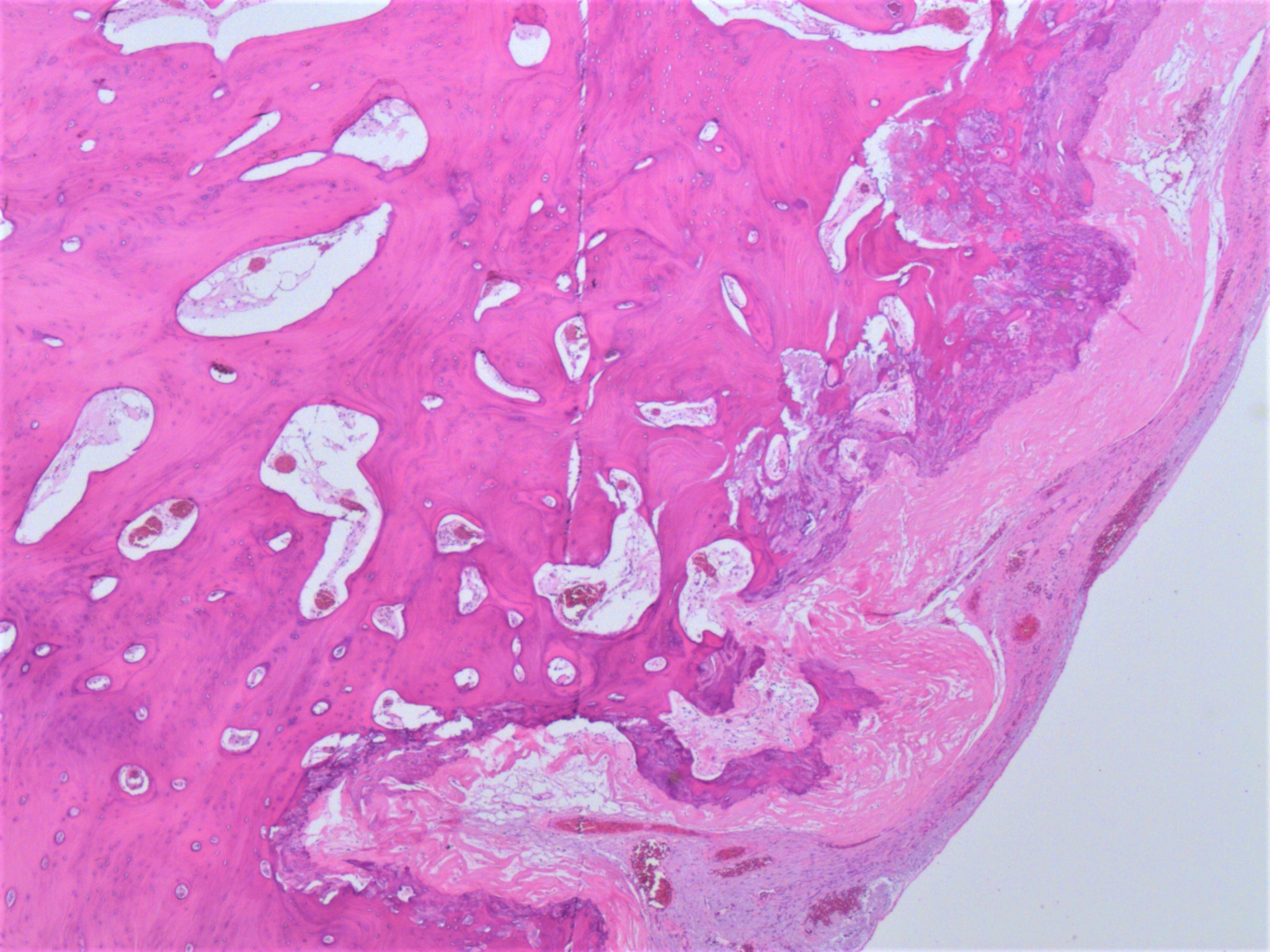
- Microcalcifications usually not apparent grossly
- Areas of bone formation are nodular and calcified
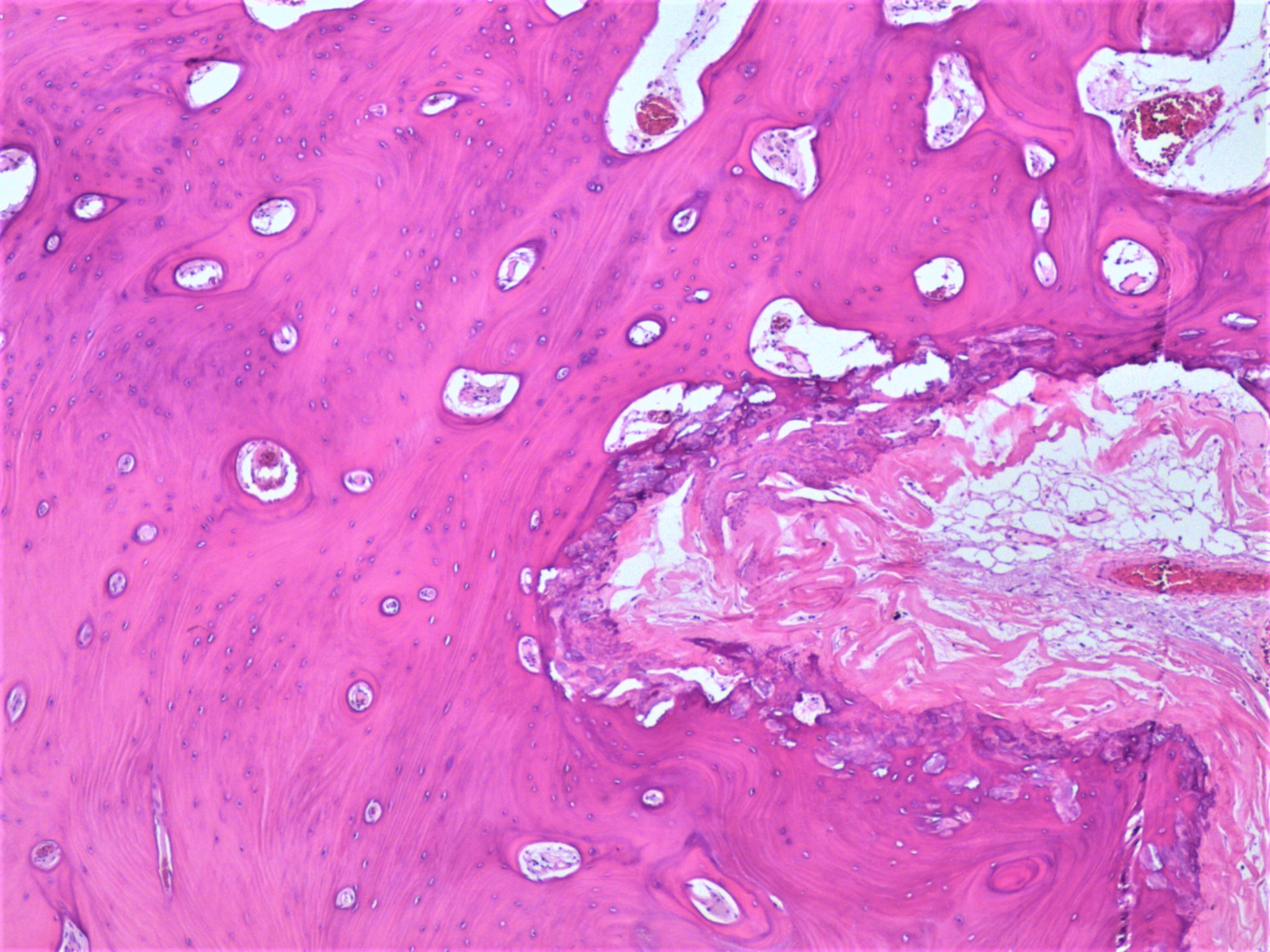
Microscopic (histologic) description
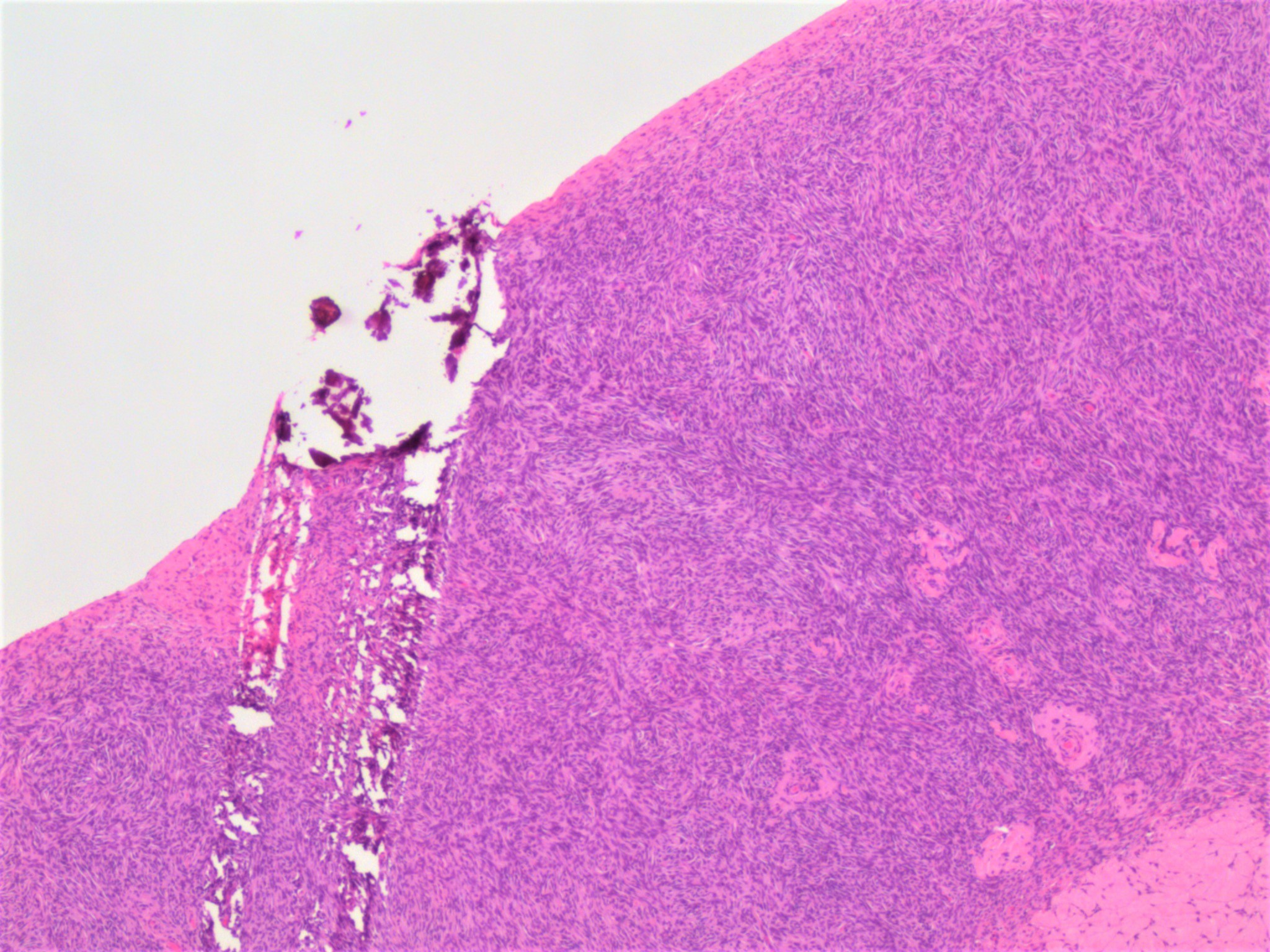
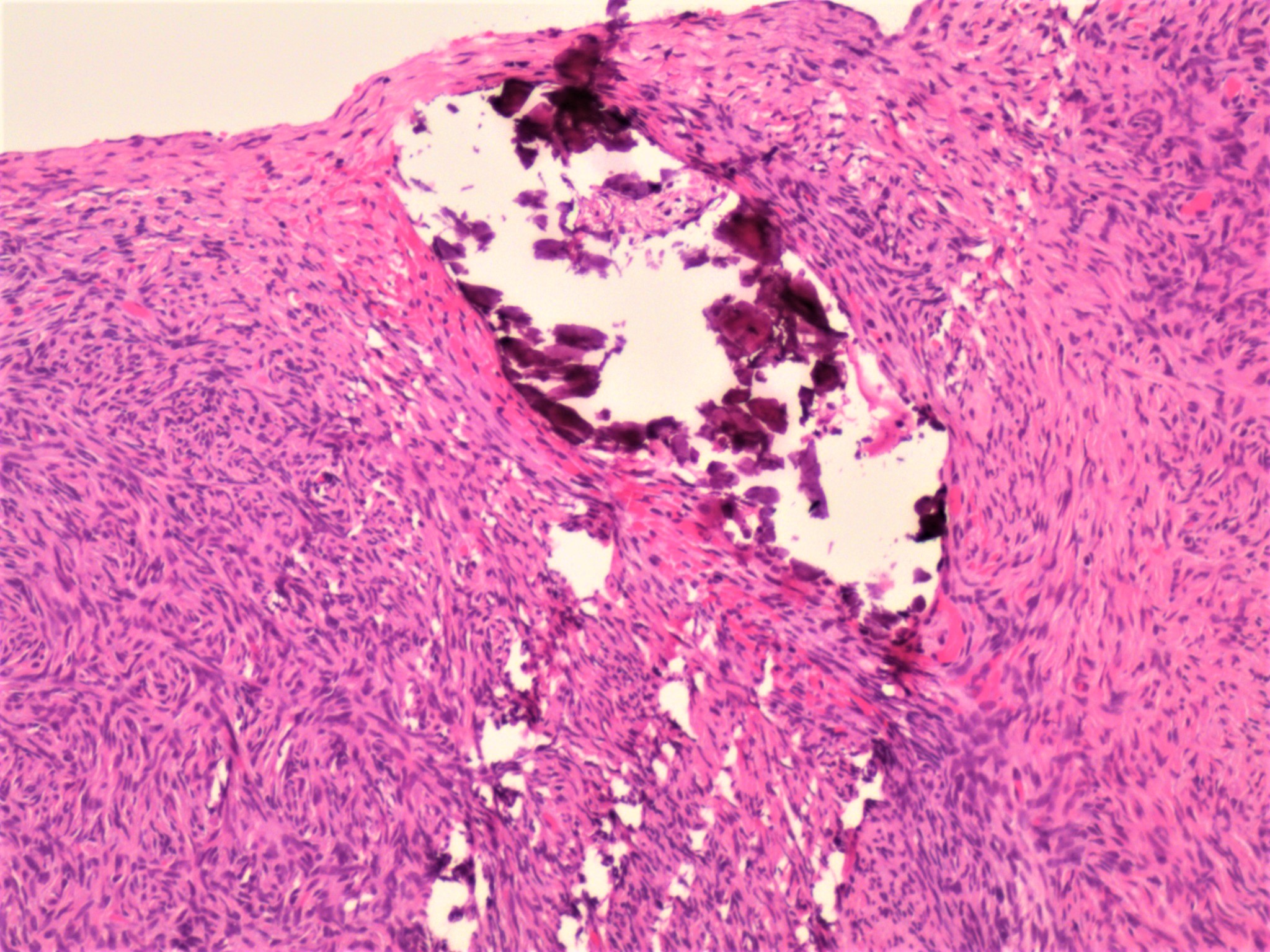
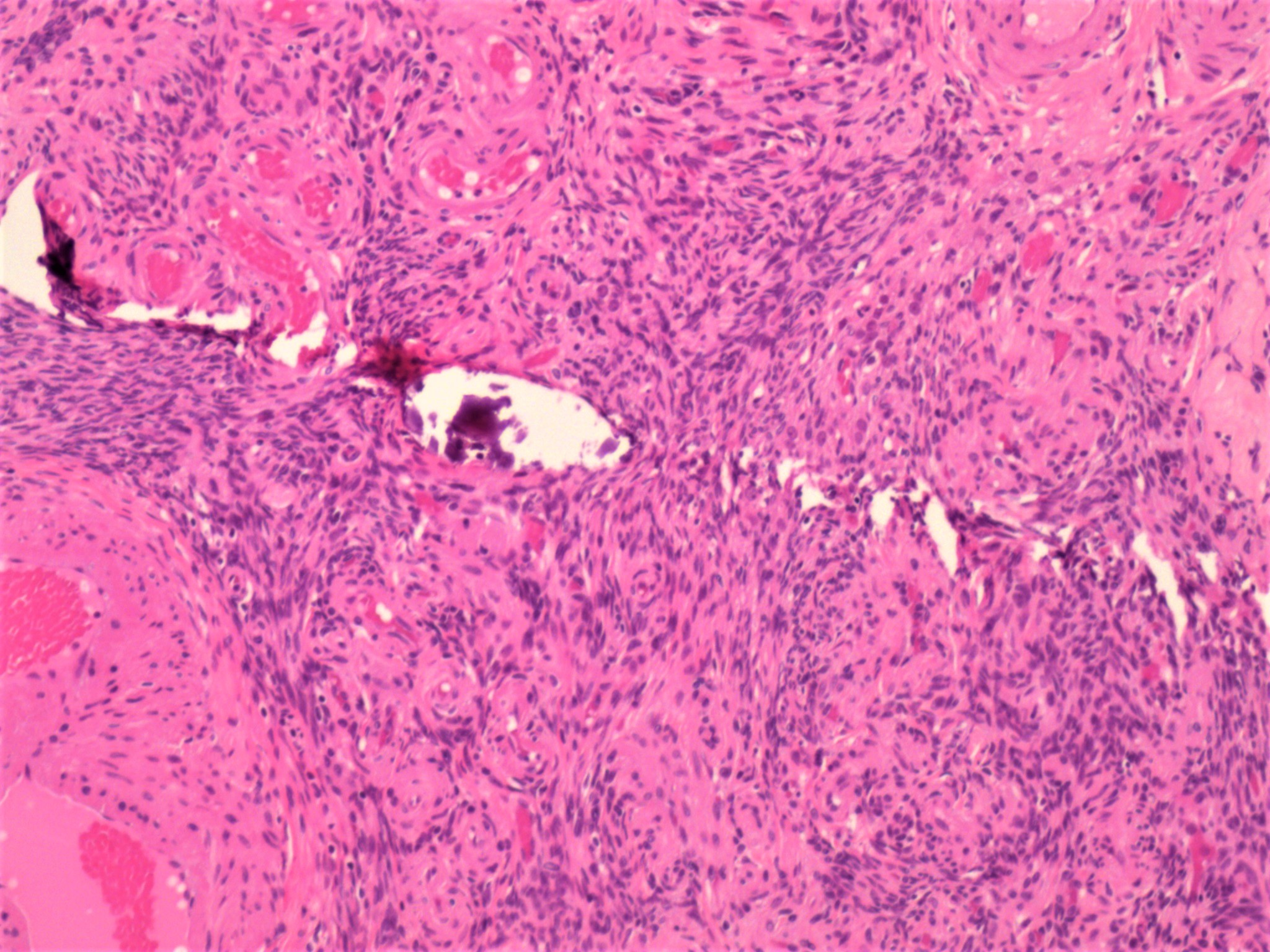
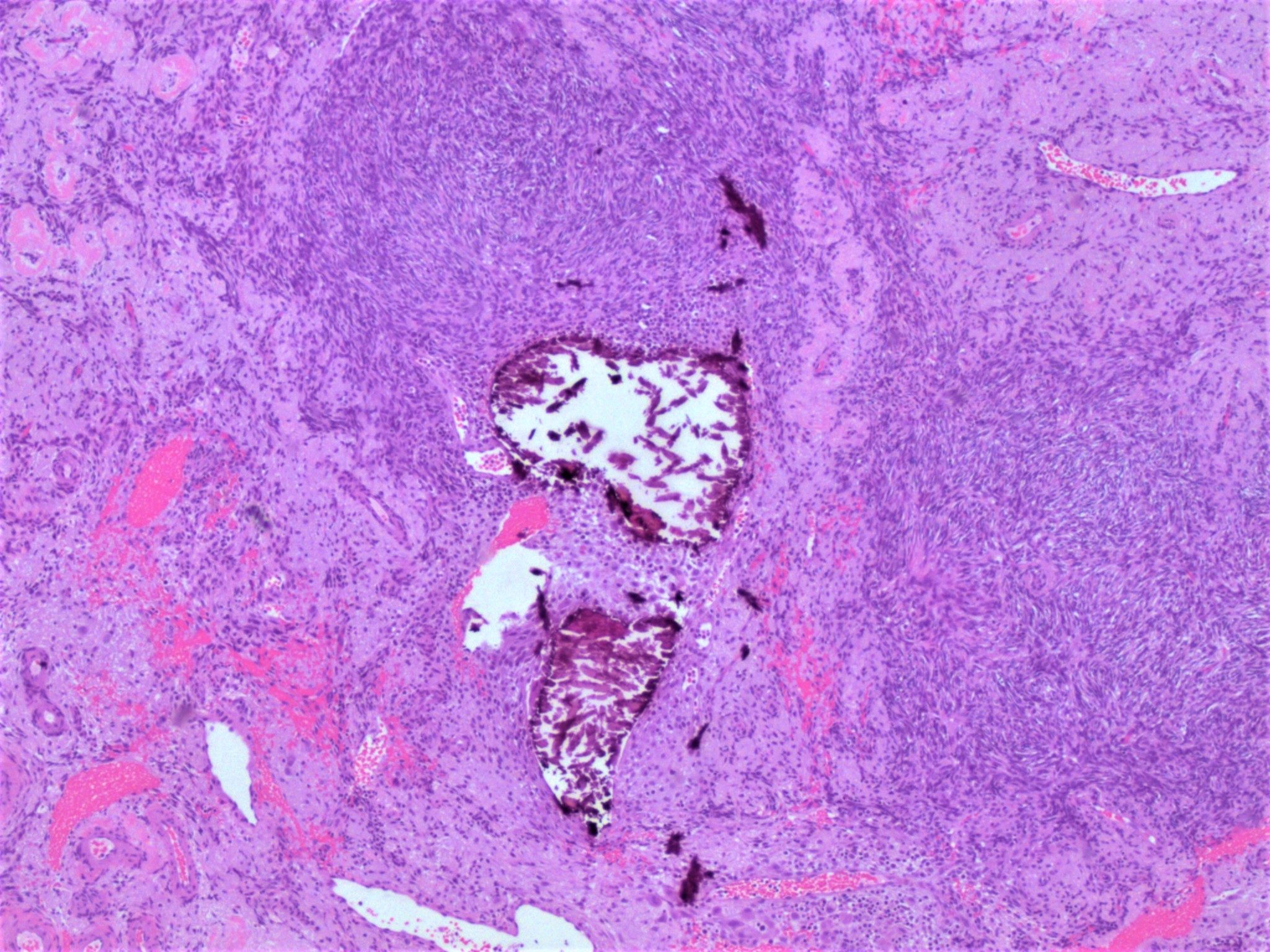
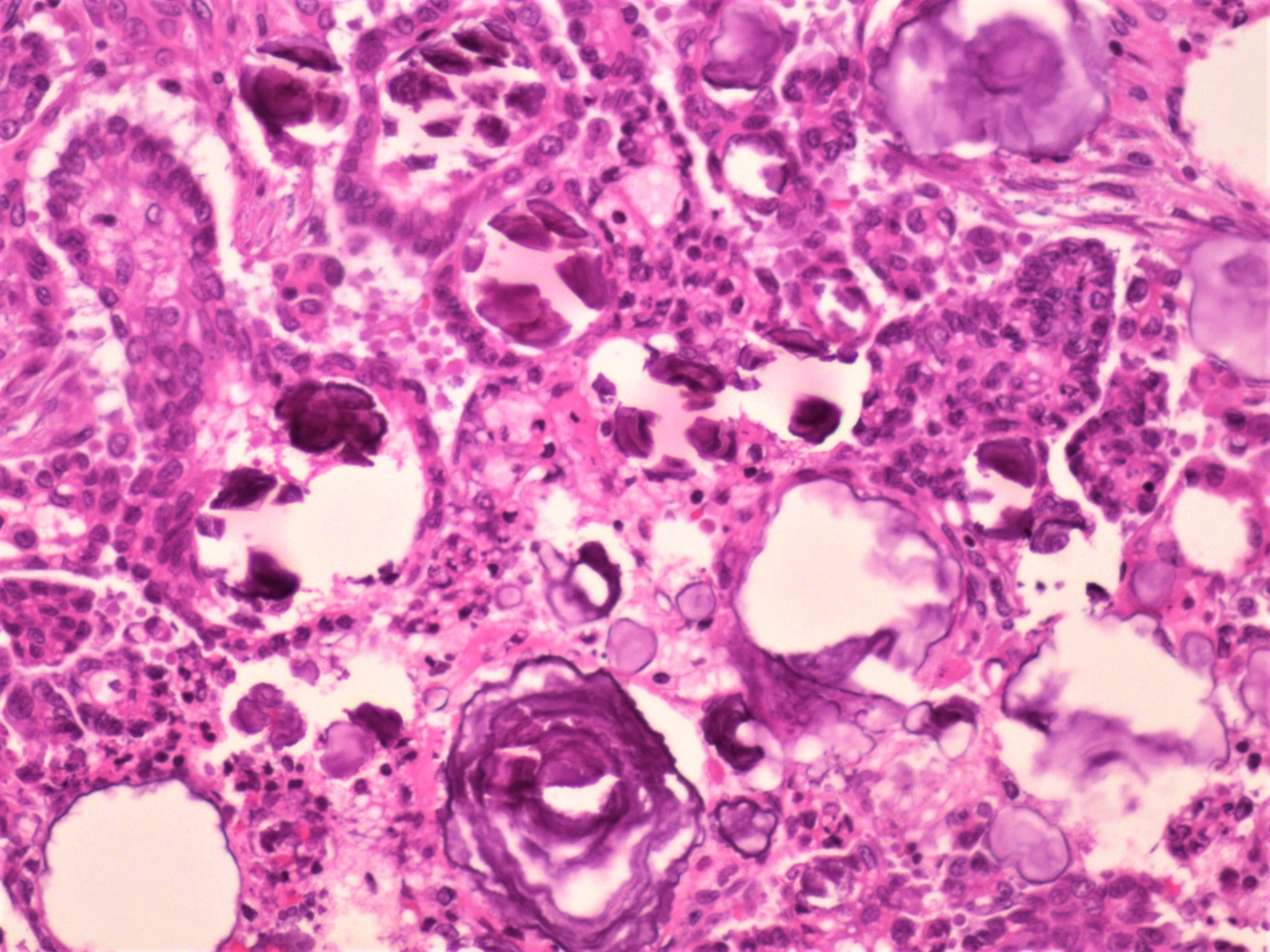
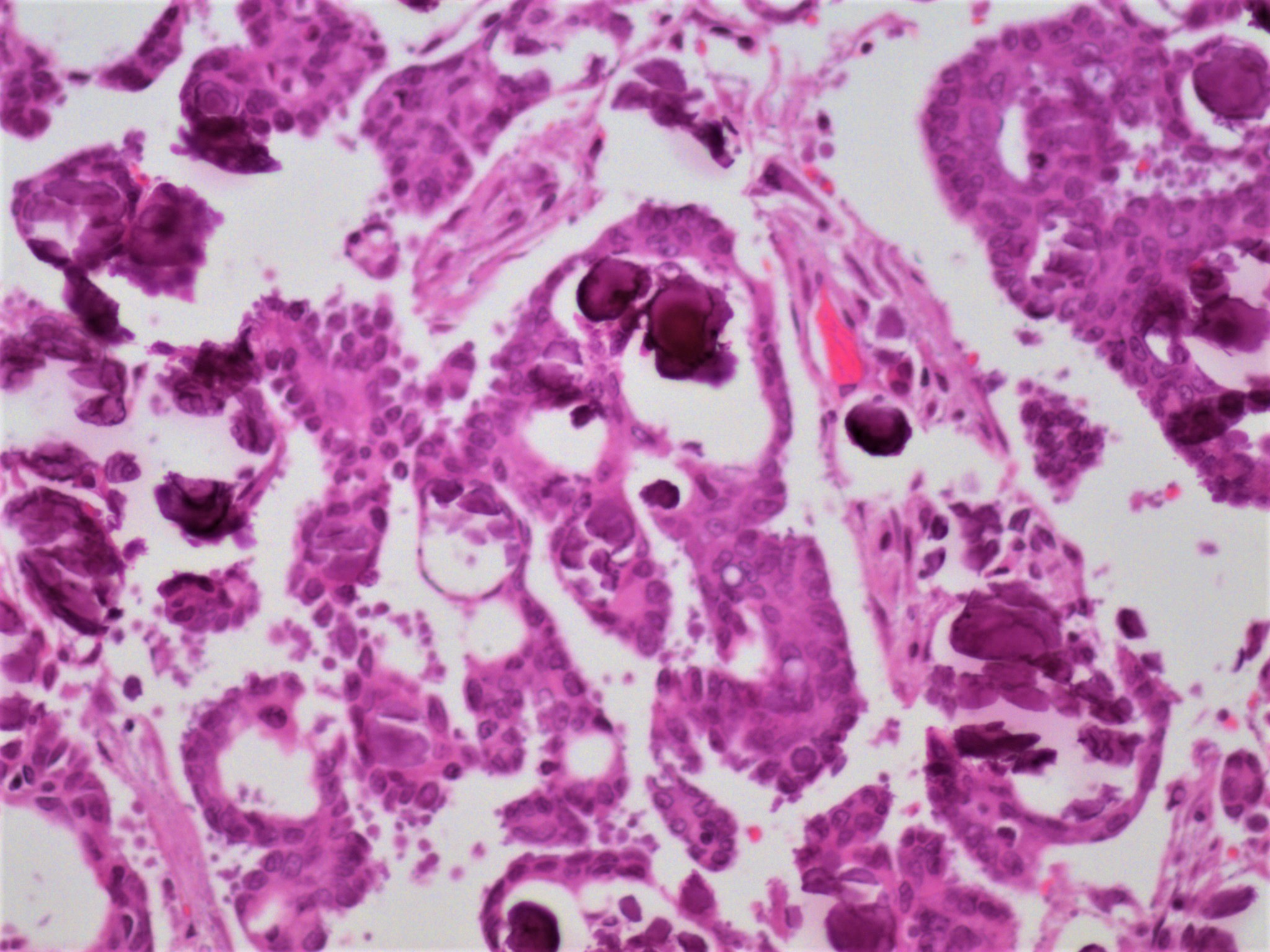
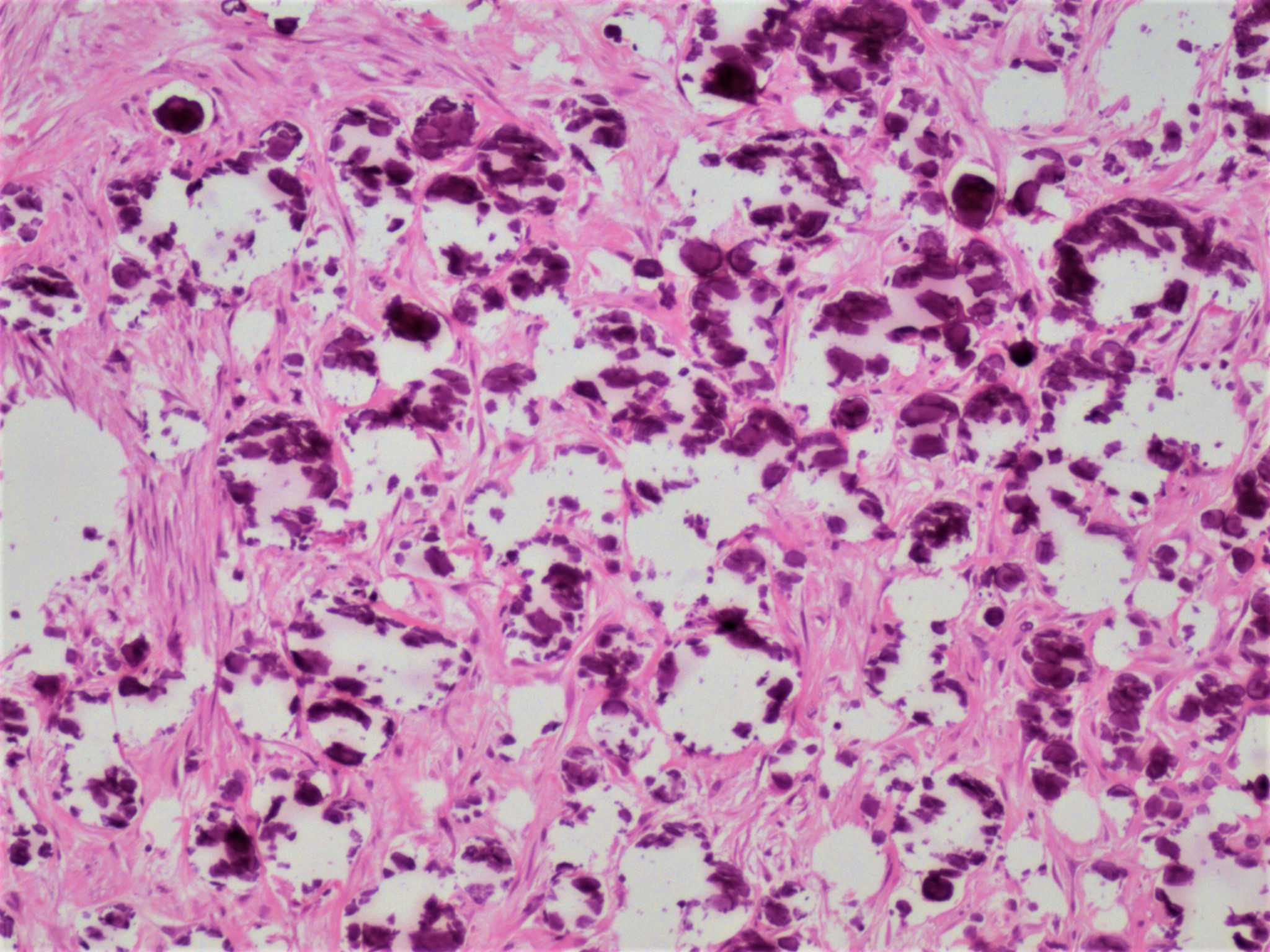
- Most ovarian calcifications consist of calcium phosphate, which stains dark purple on H&E sections
- Psammomatous calcifications: round with concentric laminations (onion-like appearance)
- Nonpsammomatous: irregular shape, dense, nonlaminated
- Bone formation shows well developed bone trabeculae
- Background ovary can be otherwise normal or show other associated pathology, such as endometriosis, teratoma, mucinous lesions, serous lesions; calcifications can be stromal or associated with the epithelial component (Mod Pathol 2003;16:219, J Nippon Med Sch 2005;72:29)
- Psammomatous calcifications in the absence of a serous neoplasm should prompt additional sampling to rule out a neoplastic process; their presence should be mentioned in the report if a serous tumor cannot be identified
Microscopic (histologic) images
Sample pathology report
- Ovary, right, oophorectomy:
- Benign ovary with surface adhesions and focal stromal psamommatous calcifications (see comment)
- Comment: The ovary has been extensively sampled, without evidence of a neoplastic process.
Differential diagnosis
- Teratoma:
- Osseous metaplasia versus teratoma: teratoma will have other components apart from bone
Practice question #1
Practice answer #1
Practice question #2
Which of the following is true about calcifications of the ovary?
- Are often symptomatic
- Can be associated with a neoplastic process
- Often arise in the context of hypercalcemia
- Their presence on imaging studies prompts a resection
Practice answer #2