Table of Contents
Definition / general | Pathophysiology | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Differential diagnosisCite this page: Ehdaivand S, Gupta N. Gonadoblastoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/ovarytumorgonadoblastoma.html. Accessed May 12th, 2024.
Definition / general
- First described by Scully in 1953 (Cancer 1953;6:455)
- Also called dysgenetic gonadoma
- Mixture of germ cell tumor and sex-cord stromal tumor
- Usually occurs in individuals with abnormal sexual development and indeterminate gonads; usually gonadal dysgenesis with Y chromosome (i.e. XY gonadal dysgenesis, XO-XY mosaicism, not XX gonadal dysgenesis); 25% risk of neoplasia in these gonads
- Also present in phenotypically normal women, even during pregnancy, although ovary is never normal
- Y chromosome material appears to participate in gonadoblastoma tumorigenesis (Am J Clin Pathol 1997;108:197, Birth Defects Res C Embryo Today 2009;87:114)
- Associated with ataxia-telangiectasia
- 80% are phenotypic women, 20% are phenotypic men with undescended testicles and female internal secondary organs
- 50% have coexisting dysgerminoma
- Excellent prognosis if completely excised; almost never malignant
- Chromosomal analysis useful to diagnose androgen insensitivity / male pseudohermaphroditism (46,XY) and Turner syndrome (45,XO)
- Imaging:
- Imaging studies useful to diagnose intersexuality and identify patients at risk of developing gonadoblastoma
- Flat abdominal radiograph may reveal gonadal calcification, a classic pathologic finding in gonadoblastoma
Pathophysiology
- Gonadal differentiation starts after 5 weeks of gestation and depends on sex chromosome of fetus
- Errors in this complex multistep process of sexual differentiation may cause dysgenetic gonads
Case reports
- Two young patients with isochromosome 12p in dysgerminoma overgrowth component (Pathol Res Pract 2012;208:628)
- Patient with Denys-Drash syndrome and early presentation of bilateral gonadoblastoma (J Pediatr Endocrinol Metab 2013;26:971)
Treatment
- Pure Gonadoblastoma have excellent prognosis
- Local excision is adequate treatment if no frankly malignant are present
Gross description
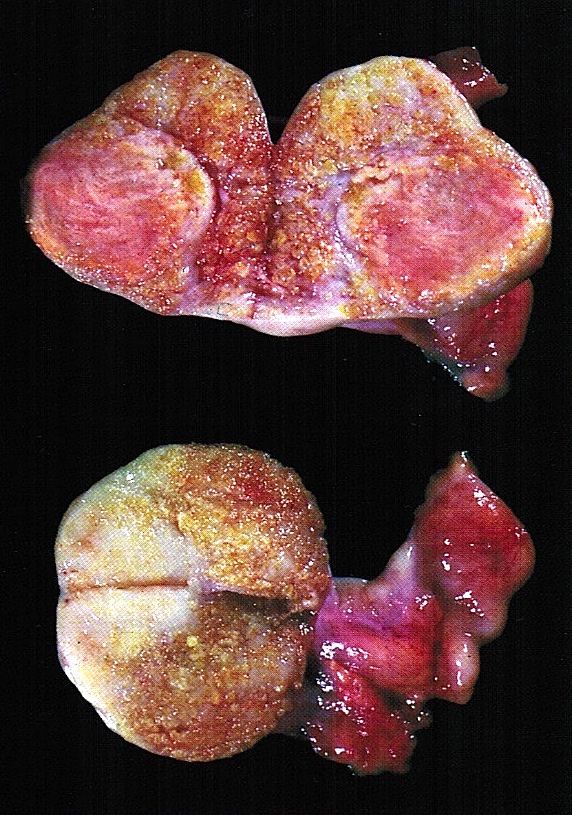
- 36% bilateral, tumors usually small and may be microscopic
Gross images
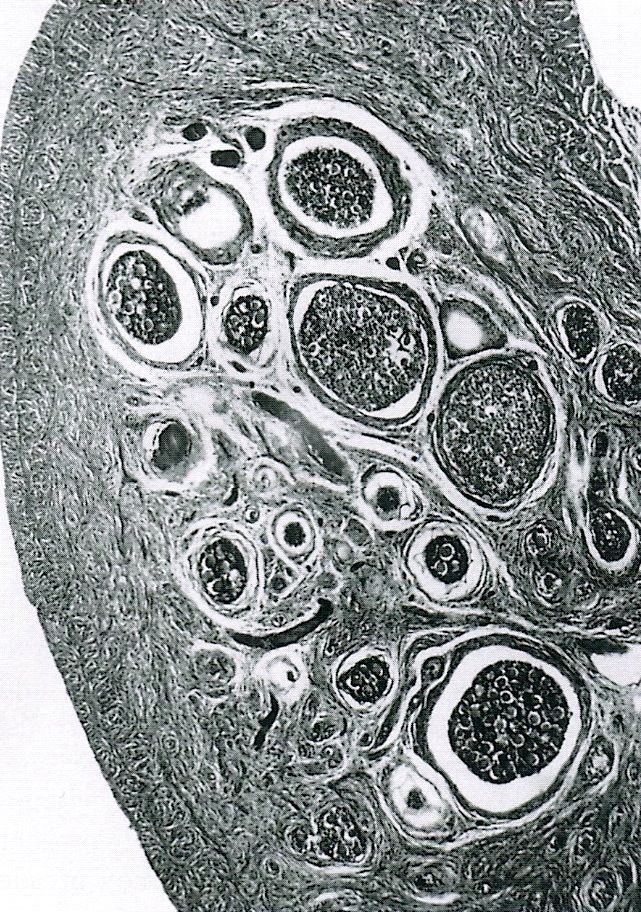
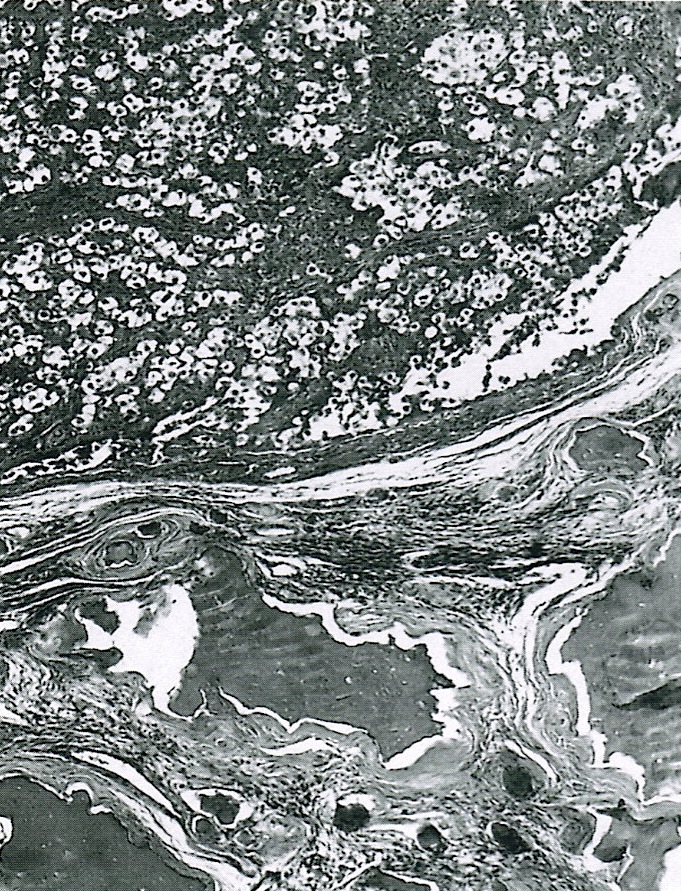
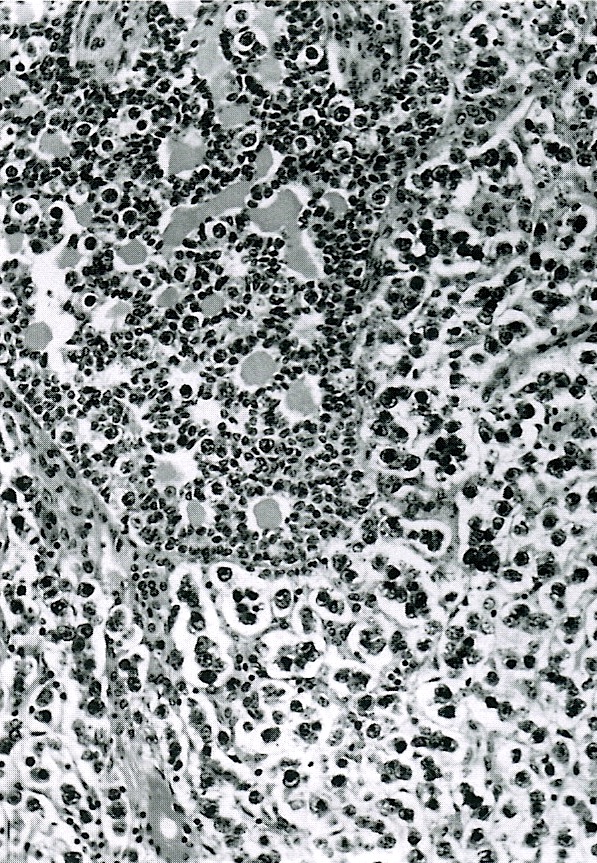
Microscopic (histologic) description
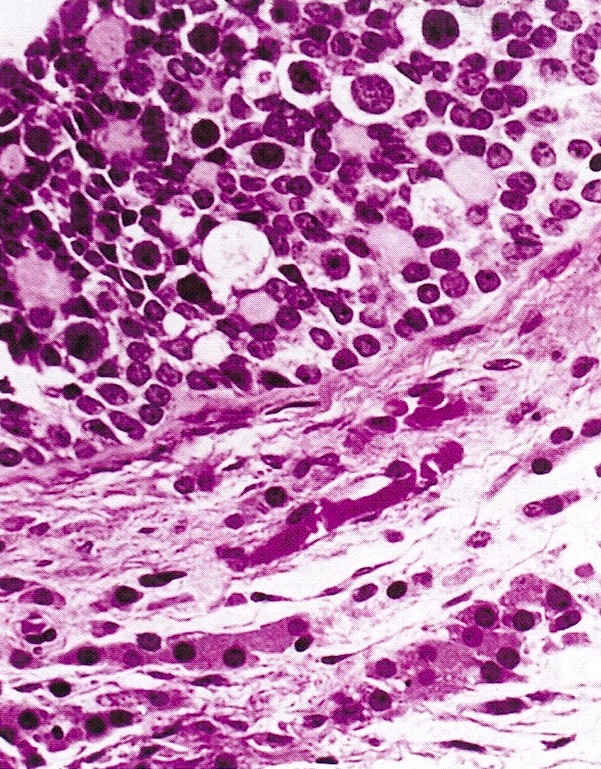
- Primitive germ cells and sex cord stromal cells surrounded by ovarian type stroma
- Nests of dysgerminoma-like germ cells and sex cord derivatives resemble immature Sertoli and granulosa cells
- Arranged in nests surrounded by ovarian stroma containing Leydig or lutein type cells
- Hyalinization and calcification are common
- May be dysgerminoma if overgrowth of this component (Am J Clin Pathol 1997;108:197)
Positive stains
- Anti-Müllerian hormone focally (Hum Pathol 2000;31:1202)
- SALL4 and SF1 (Int J Gynecol Pathol 2013;32:379)
- Occasional c-KIT mutations (PLoS One 2012;7:e43952)
Differential diagnosis
- Incidental finding in ovaries of normal infants / children: associated with follicular cysts, microscopic foci resembling gonadoblastoma or sex cord tumor with annular tubules