Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Wu B, Shinohara M. Pyoderma gangrenosum. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorpyodermagangrenosum.html. Accessed May 1st, 2024.
Definition / general
- Noninfectious neutrophilic dermatosis with painful nodules / pustules that progress to necrotic ulcers with a characteristic violaceous edge
- Pyoderma gangrenosum is a diagnosis of exclusion based on clinical and histological findings
Essential features
- Painful ulcers
- Up to 50% associated with systemic disease, particularly inflammatory bowel disease
- Diagnosis of exclusion
- Early lesions show neutrophilic folliculitis / perfolliculitis with dermal abscess
- Later lesions are ulcerated with mixed dermal inflammation and neutrophilic abscess that undermines the ulcer edge
ICD coding
- ICD-10: L88 - pyoderma gangrenosum
Epidemiology
- Uncommon; ~3 - 10 cases per million people per year
- M = F
- Any age; most common between 20 - 50 years old
- Reference: J Eur Acad Dermatol Venereol 2009;23:1008
Sites
- Any site; most common lower legs, peristomal
Pathophysiology
- Likely multifactorial but poorly understood
- Neutrophil dysfunction: abnormal neutrophil trafficking possibly related to abnormal intracellular metabolic oscillations (J Invest Dermatol 1998;111:259)
- Genetic predisposition: mutations like in the PSTP1P1 / CD2BP1 gene identified for pyoderma gangrenosum associated syndromes, such as pyogenic arthritis, pyoderma gangrenosum and acne (PAPA) syndrome (Hum Mol Genet 2002;11:961)
- Immune system dysregulation / systemic inflammation: increased proinflammatory and neutrophil chemotactic factors (Lab Invest 2000;80:595, Arch Dermatol 2011;147:1203, Am J Clin Dermatol 2017;18:355)
Etiology
- Unknown etiology; 25 - 50% idiopathic
- Up to 50% associated with systemic disease:
- Inflammatory bowel disease (e.g. ulcerative colitis)
- Arthritis
- Hematological malignancy or monoclonal gammopathies
- Other associated conditions: rheumatoid arthritis, seronegative arthritis, pregnancy, viral hepatitis, HIV, granulomatosis with polyangiitis
- Reference: Clin Med (Lond) 2019;19:224
Clinical features
- 4 major subtypes:
- Ulcerative / classic (most common): erythematous lesion that rapidly progresses to ulcer with undermined edge, violaceous border and purulent base
- Painful, with or without fever
- Possible pathergy (precipitated by minor trauma)
- Bullous: often associated with a hematological malignancy (Arch Dermatol 1972;106:901)
- Pustular: often associated with inflammatory bowel disease (Clin Exp Dermatol 2003;28:600)
- Vegetative / superficial granulomatous: mildly painful, verrucous quality, often without systemic condition (J Am Acad Dermatol 1988;18:511)
- Ulcerative / classic (most common): erythematous lesion that rapidly progresses to ulcer with undermined edge, violaceous border and purulent base
Diagnosis
- Nonspecific clinical and histologic findings; a diagnosis of exclusion
- Proposed diagnostic criteria by Delphi Consensus of International Experts (JAMA Dermatol 2018;154:461):
- Need major criteria + ≥ 4 minor criteria
- Major criteria: neutrophilic infiltrate on biopsy of ulcer edge
- Minor criteria:
- Exclude infection
- Pathergy
- History of inflammatory bowel disease or inflammatory arthritis
- History of papule, pustule, vesicle within 4 days of ulceration
- Peripheral erythema, undermining border and tenderness
- Multiple ulceration, at least 1 on anterior lower leg
- Healed ulcer site with wrinkled paper scar
- Decreased ulcer size upon initiating immunosuppressant
Prognostic factors
- > 50% achieve complete wound healing in 1 year (Australas J Dermatol 2011;52:218)
- Unfavorable prognostic factors: male, old age onset, bullous pyoderma gangrenosum associated with hematologic malignancy
- Favorable prognostic factors: no underlying disease
Case reports
- 11 month old girl with papular, erythematous eruption on her legs, buttock, torso and oral mucosa (Pediatr Dermatol 2018;35:e257)
- 36 year old woman with extensive pyoderma gangrenosum after caesarean section (Int J Surg Case Rep 2021;81:105697)
- 67 year old woman and 87 year old woman with rheumatoid arthritis on rituximab that developed vulvovaginal pyoderma gangrenosum (JAAD Case Rep 2021;10:75)
- 68 year old man with history of ulcerative rectocolitis and erythematous and painful lesion on his leg (Dermatol Ther 2019;32:e12928)
Treatment
- General measures: control underlying disease, manage pain, wound care, avoid trauma
- For limited disease: topical therapy with corticosteroid and calcineurin inhibitors
- For extensive or advanced disease: first line therapy with systemic glucocorticoids or cyclosporine; second line / adjunctive therapy with tumor necrosis factor alpha (TNF alpha) inhibitors and anti-interleukin therapy
- Reference: Am J Clin Dermatol 2017;18:355
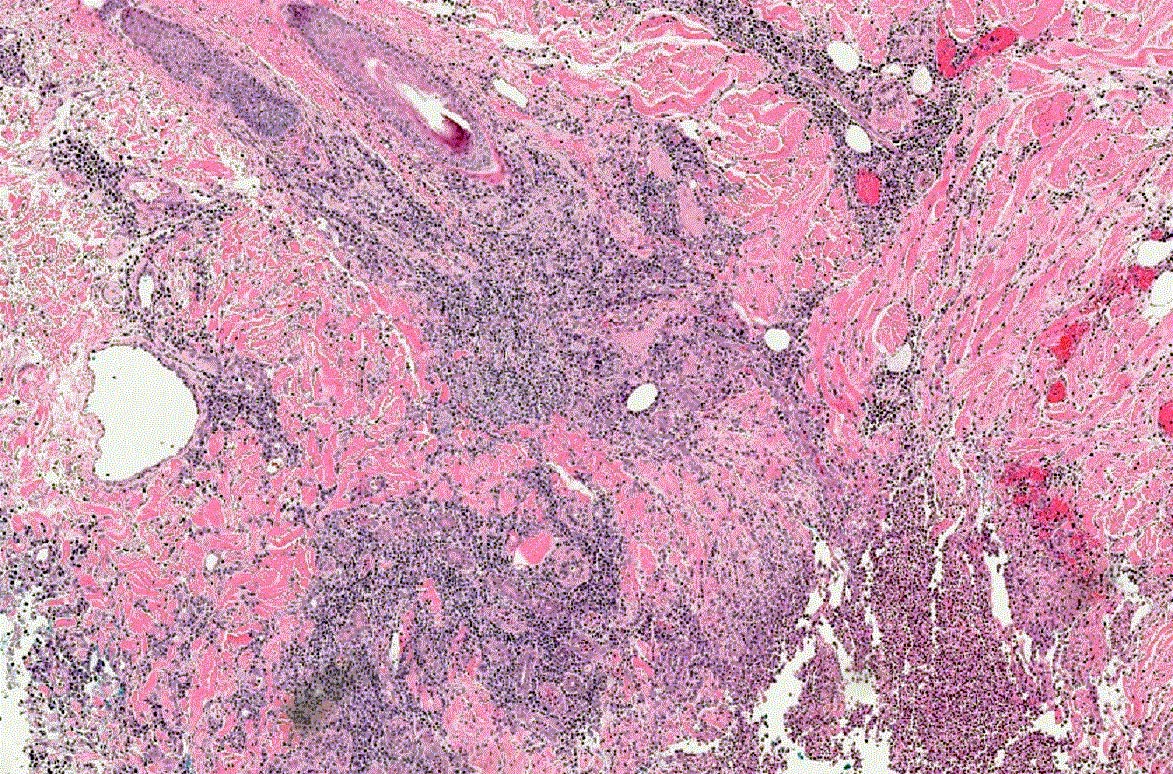
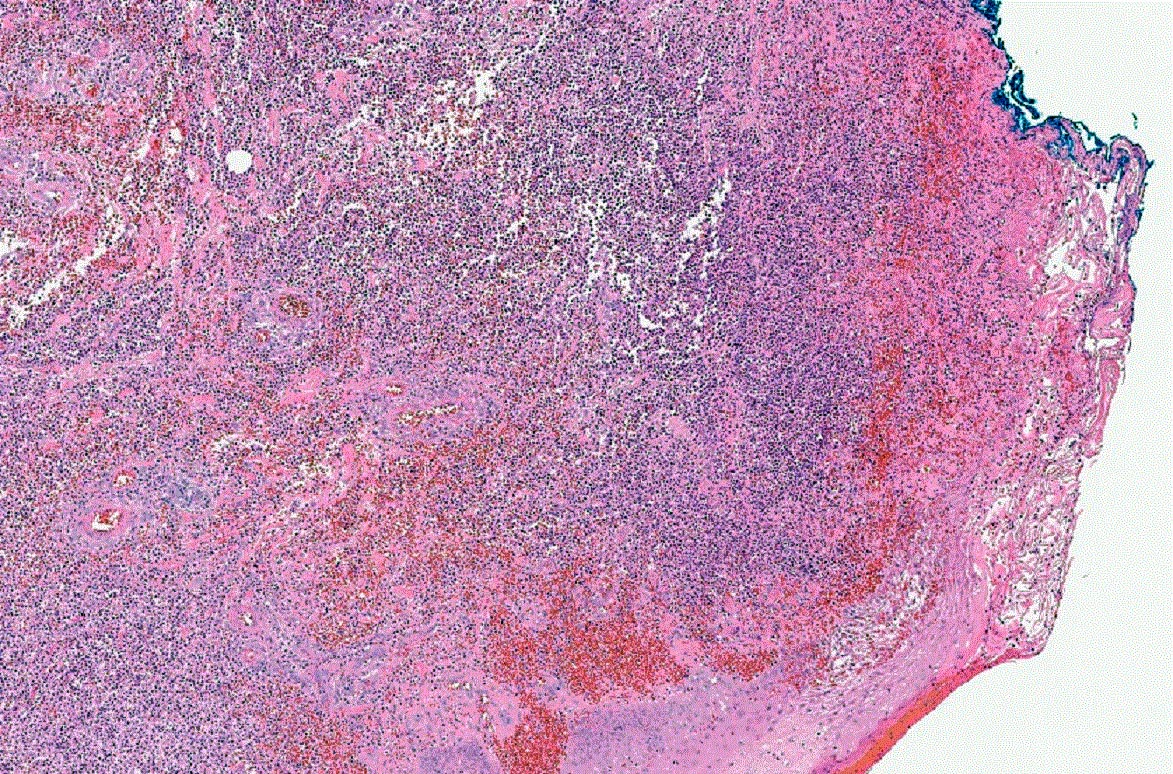
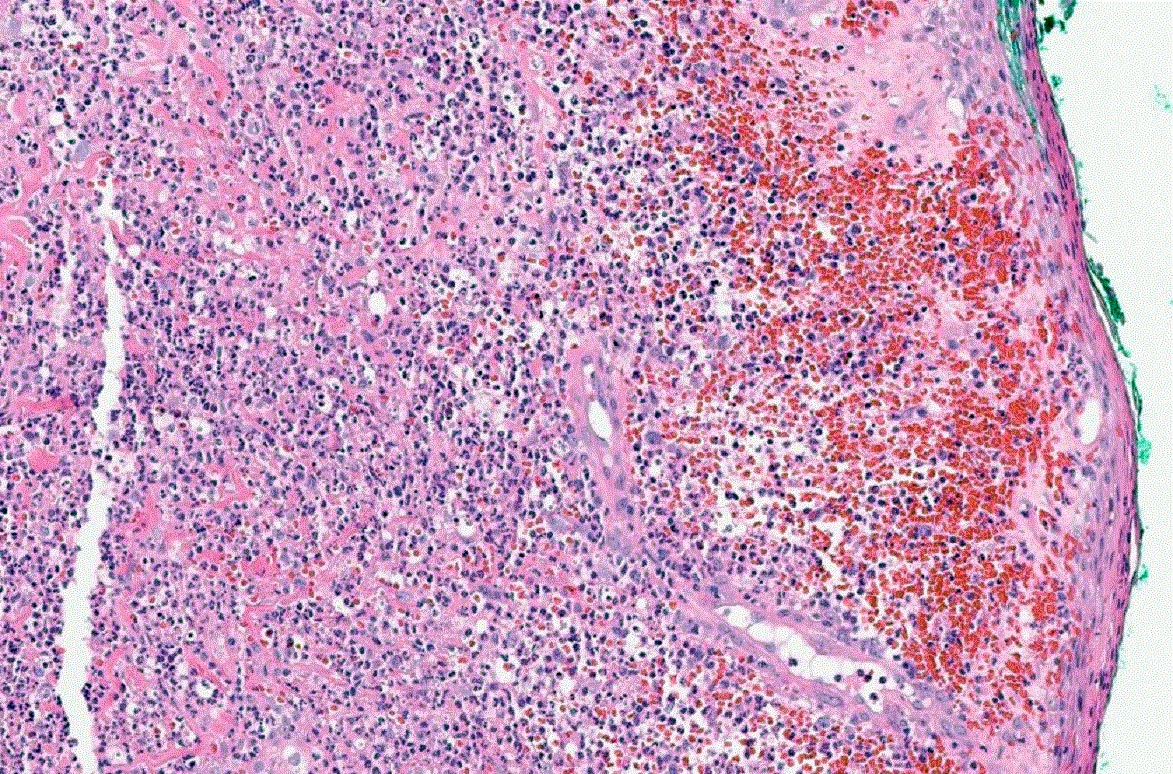
Microscopic (histologic) description
- Variable, dependent on the lesion age and site
- Early lesion:
- Neutrophilic folliculitis and perifolliculitis
- Intradermal neutrophilic abscess formation
- Later lesions:
- Epidermal ulceration
- Superficial dermal necrosis
- Mixed inflammation with undermining at ulcer edge (characteristic) and abscess
- Occasional giant cells (associated with inflammatory bowel disease)
- Advancing edge often has subepidermal edema
- Leukocytoclastic vasculitis and lymphocytic vasculitis may be present (J Cutan Pathol 2003;30:97)
- Acanthosis in perilesional zone
- Variants:
- Ulcerative / classic variant: central neutrophilic abscess and peripheral angiocentric lymphocytic infiltrates
- Bullous variant: subepidermal bullae and dermal neutrophilic infiltrates
- Pustular variant: subcorneal pustules, subepidermal edema, dense dermal neutrophilic infiltrates
- Vegetative / superficial granulomatous variant: reactive epidermal proliferation, dermal abscess, sinus tracts and palisading granulomas
Videos
Pyoderma gangrenosum versus nonspecific chronic ulcer changes
Sample pathology report
- Skin, leg, punch biopsy:
- Ulcer with mixed dermal inflammation (see comment)
- Comment: The findings are nonspecific but could be compatible with pyoderma gangrenosum. Pyoderma gangrenosum is a diagnosis of exclusion and other causes of ulceration, including infection, must be ruled out.
Differential diagnosis
- Sweet syndrome:
- Not typically associated with ulcer, prominent karyorrhexis and deeper / more extensive inflammation
- Infection or necrotizing fasciitis:
- Involves deeper subcutaneous tissue; presence of microorganisms
- Arthropod bite reaction:
- Numerous eosinophils
- Venous stasis ulceration:
- Can show identical findings, usually without prominent neutrophils
- Can show identical findings
Additional references
Board review style question #1
Board review style answer #1
Board review style question #2
Which of the following is a feature of early pyoderma gangrenosum biopsies?
- Eosinophilic pustulosis
- Epidermal ulceration
- Neutrophilic folliculitis
- Subepidermal bullae
Board review style answer #2