Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Videos | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Tran P, Occidental M. Warty dyskeratoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumornonmelanocyticwartydyskeratoma.html. Accessed August 20th, 2025.
Definition / general
- Warty dyskeratoma (WD) is an uncommon, benign follicular neoplasm characterized by acantholytic dyskeratosis
- Presents as a solitary papule or nodule with a central keratotic plug, commonly on the scalp, face or neck of adults
Essential features
- Well circumscribed, solitary papule or nodule lined by epithelial cells and filled with keratin debris
- Classic cupuliform (cup shaped) architecture with focal acantholysis / clefting and dyskeratosis with corps ronds and grains
- Histologically resembles but is not related to Darier disease
Terminology
- Follicular dyskeratoma
- Isolated dyskeratosis follicularis (AMA Arch Derm 1958;77:377)
- Isolated Darier disease (keratosis follicularis / follicular keratosis)
- Dyskeratoma segregans (J Am Acad Dermatol 2002;47:423)
- Acantholytic keratosis (Diagnostics (Basel) 2022;12:1273)
ICD coding
- ICD-10: D23.9 - other benign neoplasms of skin
Epidemiology
- Older adults (mean age: 47 - 60 years old) (J Am Acad Dermatol 2002;47:423, AMA Arch Derm 1958;77:377)
- Slight female predominance (~2:1) (J Am Acad Dermatol 2002;47:423)
Sites
- Most commonly on the scalp, face or neck
- Can also be found in the oral cavity or on the trunk, extremities or genitals
- Rare multiple lesions have only been reported on the scalp (Am J Dermatopathol 2018;40:e44, Ann Dermatol 2011;23:98, Ann Dermatol 2023;35:S345)
- Rarely affects the vulva (Int J Gynecol Pathol 1983;2:286)
Pathophysiology
- Unclear pathogenesis at this time; likely follicular differentiation in an adnexal neoplasm (J Am Acad Dermatol 2002;47:423, AMA Arch Derm 1958;77:377)
- Oral warty dyskeratoma has been suggested to be a separate entity (J Am Acad Dermatol 2002;47:423)
- Not related to nor a precursor to Darier disease (AMA Arch Derm 1958;77:377)
Etiology
- Unknown etiology at this time (J Am Acad Dermatol 2002;47:423, Am J Dermatopathol 2018;40:e44, Ann Dermatol 2011;23:98)
- Despite its name, warty dyskeratoma is not associated with human papillomavirus (HPV) infection (J Am Acad Dermatol 2002;47:423)
- May be a side effect of BRAF inhibitor therapy (J Am Acad Dermatol 2012;67:1265)
- Oral lesions have associations with tobacco, alcohol and ill fitting dentures (Diagnostics (Basel) 2022;12:1273)
Clinical features
- Typically 3 - 4 mm in size (rarely 1 - 10 mm) (AMA Arch Derm 1958;77:377)
- Singular, brown or skin colored papule or nodule with smooth, rolled edge and central keratin plug or umbilication (J Am Acad Dermatol 2002;47:423)
- Typically asymptomatic but may be pruritic or present with foul smelling cheesy drainage, crusting or trauma associated central bleeding (Ann Dermatol 2011;23:98, AMA Arch Derm 1958;77:377, Am J Dermatopathol 2018;40:e44)
- Dermoscopic findings (cupuliform lesion)
- Glossy, smooth, well circumscribed dome shaped morphology
- Foveal and umbilicated center filled with white, keratinous debris with distinct border and no identifiable structure
- Skin colored with dark, dome-like pattern of the inner marginal area
- Collarette with white ring streaks, radial streaks and globules
- No prominent vasculature
- Clinical differential is broad, including but not limited to basal cell carcinoma, epidermal cyst, seborrheic keratosis, squamous cell carcinoma, keratoacanthoma, folliculitis, verruca vulgaris, comedo, condyloma (genital) (J Am Acad Dermatol 2002;47:423, Am J Dermatopathol 2018;40:e44, Int J Gynecol Pathol 2025;44:112)
Diagnosis
- Skin biopsy (excisional, shave, punch)
Prognostic factors
- No recurrence with excision (Diagnostics (Basel) 2022;12:1273)
Case reports
- 43 year old woman with exophytic nodule on the vulva (Dermatol Pract Concept 2024;14:e2024124)
- 47 year old man with a nodule on the scalp (Ann Dermatol 2011;23:98)
- 63 year old woman with severely pruritic keratotic papules of her scalp (Am J Dermatopathol 2018;40:e44)
- 71 year old man with papular lesion posterior to the right auricle (Clin Case Rep 2023;11:e7495)
- 78 year old man with ulcerated lesion of left retromolar trigone (JAAD Case Rep 2017;3:336)
Treatment
- Mainstay treatment is surgical excision (Am J Dermatopathol 2018;40:e44, Ann Dermatol 2011;23:98)
- Systemic isotretinoin with topical tretinoin and urea containing lotion have been reported with positive effects in rare cases of multiple lesions (Ann Dermatol 2023;35:S345)
- Tazarotenic acid, laser, 5-floxuridine, calamine reported with variable effectiveness (Am J Dermatopathol 2018;40:e44, Ann Dermatol 2023;35:S345)
- Electrodessication and irradiation appear ineffective (Ann Dermatol 2011;23:98)
Clinical images
Gross description
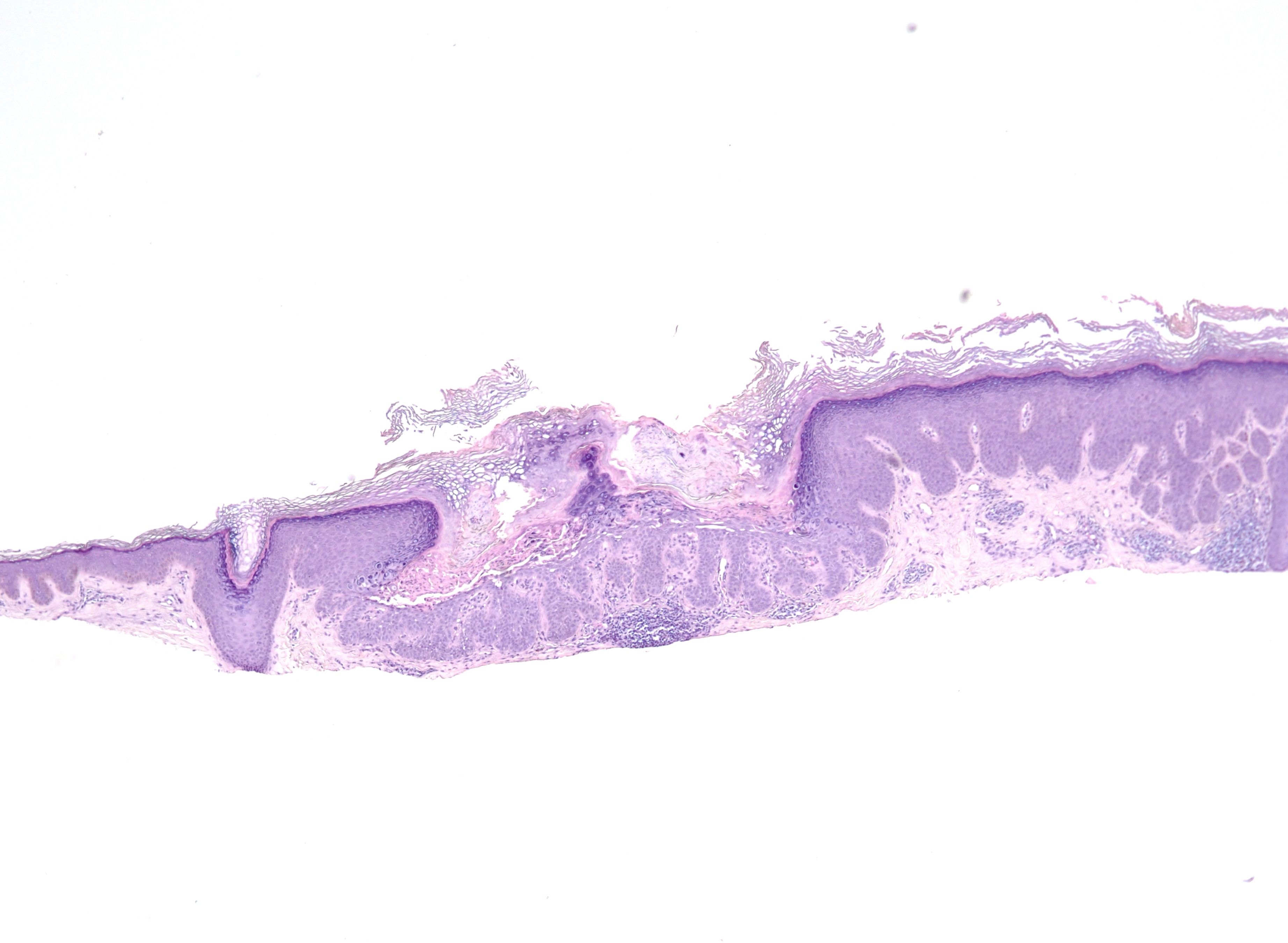
Microscopic (histologic) description
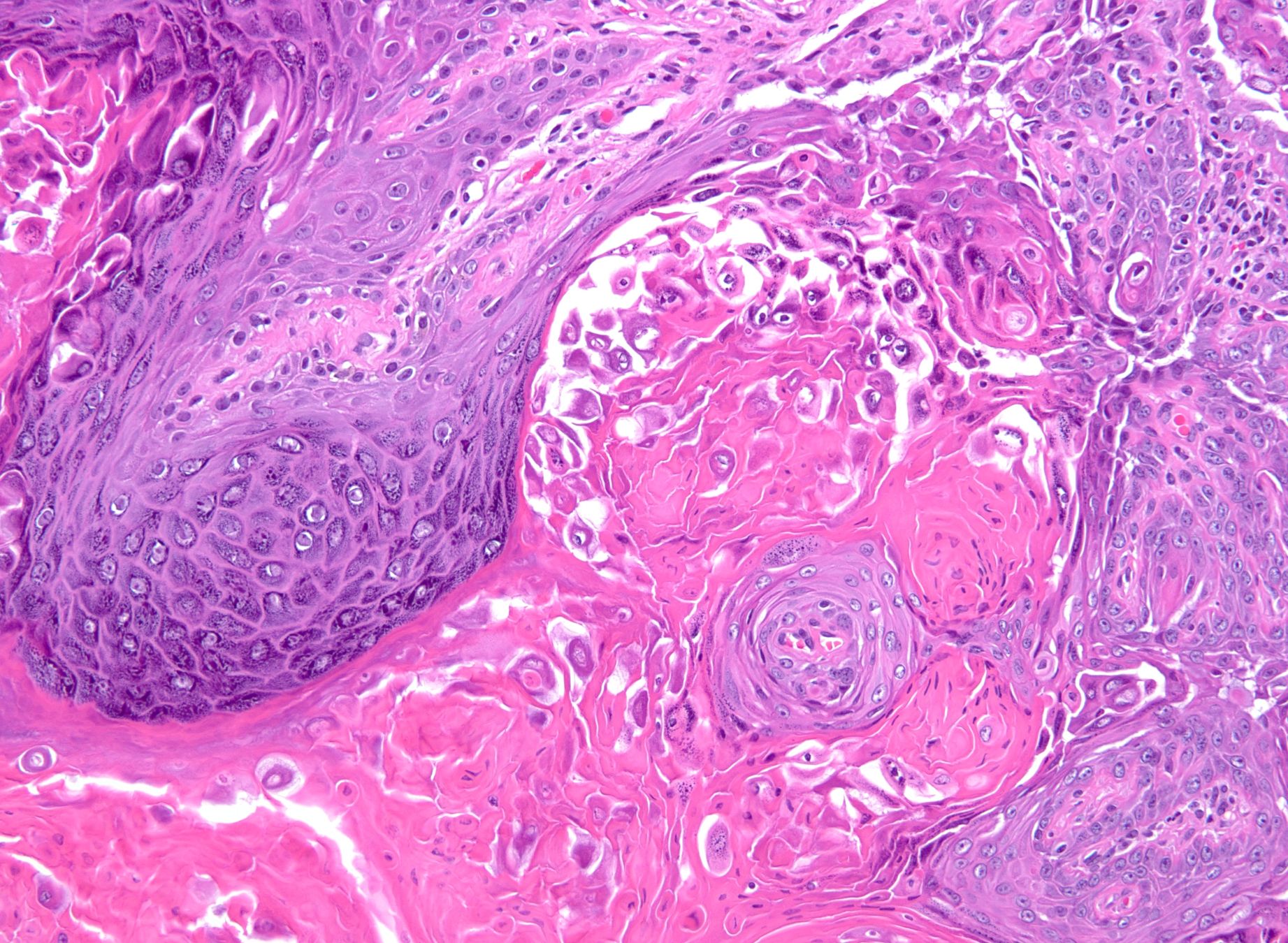
- Well circumscribed exoendophytic lesion filled with keratinous material and lined by proliferating epithelial cells with large nuclei, prominent nucleoli and variable amounts of cytoplasm
- Focal suprabasilar acantholysis with clefting and villi and dyskeratosis with corps ronds and grains
- Corps ronds: keratinocytes with small pyknotic nuclei and perinuclear halos
- Corps grains: compressed keratinocytes with elongated nuclei
- Often with hypergranulosis
- Cupuliform (cup shaped) architectural pattern: invagination in the epidermis lined by proliferating epithelial cells extending into the papillary dermis
- Classic pattern
- Parakeratotic plug
- Epidermal collarette
- Stroma with dense collagen, fibroblasts and intrastromal clefting with mild to moderate mixed inflammation, mainly lymphocytic and histiocytic
- Papillomatosis may be present
- Other patterns
- Cystic: 1 or more cystic structures lined by epithelial cells in the papillary and reticular dermis
- Connection to the epidermis may be seen focally
- Nodular: solid aggregates of epithelial cells in the papillary and reticular dermis underlying hyperplastic epidermis
- Least common pattern
- Connection to the epidermis may be seen focally
- Smaller and deeper than cupuliform and cystic lesions
- May represent an early stage in the development of warty dyskeratoma
- Combination of patterns may be seen
- Cystic: 1 or more cystic structures lined by epithelial cells in the papillary and reticular dermis
- Occasional mitoses, focal keratin pearls and vacuolated cells resembling koilocytes may be present
- Oral and vulvar lesions are histologically indistinguishable from head and neck lesions (Int J Gynecol Pathol 1983;2:286, Diagnostics (Basel) 2022;12:1273)
- References: J Am Acad Dermatol 2002;47:423, AMA Arch Derm 1958;77:377, AMA Arch Derm 1957;75:567, Am J Dermatopathol 2018;40:e44, Ann Dermatol 2011;23:98
Microscopic (histologic) images
Positive stains
- Not used for diagnosis
Videos
Warty dyskeratoma
by Jared Gardner, M.D.
Warty dyskeratoma: 5 minute pathology pearls
Sample pathology report
- Skin, left posterior scalp, shave biopsy:
- Warty dyskeratoma (see comment)
- Comment: There is a solitary, cup shaped lesion filled with keratin debris and lined by proliferating keratinocytes featuring suprabasal acantholysis and dyskeratosis with corps ronds and grains.
Differential diagnosis
- Darier disease (keratosis follicularis) (An Bras Dermatol 2019;94:630, J Dermatol 2017;44:232, AMA Arch Derm 1958;77:377):
- Multiple lesions
- Inheritable ATP2A2 mutation
- Lacks cup shaped architecture
- Extensive extrafollicular involvement
- Affects the nails
- Grover disease (transient acantholytic dermatosis) (An Bras Dermatol 2019;94:630):
- Multiple lesions
- Less prominent acantholysis and dyskeratosis
- Intraepidermal clefting
- May feature vesicles
- Hailey-Hailey disease (benign familial pemphigus) (An Bras Dermatol 2019;94:630, AMA Arch Derm 1958;77:377):
- Multiple lesions
- Lacks dyskeratosis
- Inheritable ATPC1 mutation
- More extensive epidermal lacunae
- Keratoacanthoma (J Am Acad Dermatol 2002;47:423):
- Typically lacks acantholysis with dyskeratosis
- More likely to feature atypia and mitotic activity
- Acantholytic dyskeratotic acanthoma (Int J Gynecol Pathol 2025;44:112):
- Lacks cupuliform architecture and follicular involvement
- May present as a plaque
- Papular acantholytic dyskeratosis of the genitocrural area (Int J Gynecol Pathol 2025;44:112, J Dermatol 2017;44:232):
- Multiple lesions
- Primarily affects the genital region
- Both ATP2A2 and ATP2C1 mutations
Practice question #1
Practice answer #1
E. Warty dyskeratoma histologically shows a solitary, cup shaped lesion filled with keratin debris with acantholysis and dyskeratosis.
Answer C is incorrect because keratoacanthoma features a crateriform shape with atypical keratinocytes and typically lacks acantholysis and dyskeratosis.
Answer D is incorrect because verruca vulgaris features an exophytic shape with inward rete cupping, hyperkeratosis, hypergranulosis and koilocytes.
Answer A is incorrect because acantholytic squamous cell carcinoma features atypical keratinocytes with or without keratinization and mitotic activity.
Answer B is incorrect because epidermoid inclusion cyst features lining with stratified squamous epithelium and lacks acantholysis and dyskeratosis.
Comment Here
Reference: Warty dyskeratoma
Comment Here
Reference: Warty dyskeratoma
Practice question #2
Practice answer #2
E. Warty dyskeratoma. The main histologic features of warty dyskeratoma are acantholysis and dyskeratosis with corps ronds and grains in a solitary, cup shaped lesion.
Answer B is incorrect because leukocytoclastic vasculitis features vascular involvement with neutrophil infiltration, neutrophilic dust, fibrinoid necrosis and extravasated erythrocytes.
Answer C is incorrect because lupus erythematosus features vacuolar interface dermatitis changes, rete effacement, hyperkeratosis with parakeratosis and follicular plugging.
Answer D is incorrect because pityriasis rosea features spongiotic dermatitis changes and perivascular lymphocytes.
Answer A is incorrect because bullous pemphigoid features subepidermal blistering, spongiosis with eosinophils and mixed perivascular inflammation.
Comment Here
Reference: Warty dyskeratoma
Comment Here
Reference: Warty dyskeratoma