Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Vithanage I, Haroon S. Erosive gastritis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/stomacherosive.html. Accessed September 24th, 2025.
Definition / general
- Erosive gastritis is loss of superficial epithelium of the gastric mucosa caused by impairment of mucosal defenses
Essential features
- Loss of superficial epithelium of the gastric mucosa, erosion (wearing away away) of the stomach lining, along with inflammation
- Common in the body of the stomach
- Usually an acute inflammatory process
- Diagnosis is mostly clinical and endoscopic
- References: Arq Gastroenterol 2022;59:275, Eur J Radiol 1982;2:205
Terminology
- Acute erosive gastritis
- Hemorrhagic gastritis
- Acute hemorrhagic gastritis
ICD coding
- ICD-10: К29.60 - other gastritis without bleeding
Epidemiology
- Both genders, at any age, can be affected when exposed to the causative agents of erosive gastritis
Sites
- Typically occurs in the gastric body but the antrum may also be involved
Pathophysiology
- Mucosal damage due to increased acid secretion, decreased bicarbonate buffer and reduced blood flow
- Increased acid production could be secondary to factors such as stressed state (due to various reasons such as, physiologic stress related to severe trauma, severe burns, ventilator dependency or intracranial trauma), elevated levels of ACH and histamine, resulting in increased acid production
- Stress results in the release of angiotensin II, which decreases blood flow to the mucosa, causing reactive oxygen species formation, resulting in oxidative stress on the mucosa
- Prolonged exposure of gastric mucosa to acids also increases risk for development of erosive gastritis
- References: Histopathology 2007;50:15, J Gastroenterol 2010;45:131, Korean J Fam Med 2015;36:300
Etiology
- Common causes include nonsteroidal anti-inflammatory drugs (NSAIDs), alcohol and stress (burn, surgery, trauma)
- Other causes are cancer chemotherapy, uremia, ischemia and shock, acid / alkali ingestion, mechanical trauma (nasogastric tube), distal gastrectomy, Helicobacter infection, hemodialysis and peritoneal dialysis (Front Immunol 2022;13:840916)
Clinical features
- Usually due to acute inflammatory processes but may be subacute or chronic
- When acute, can present with GI bleeding (Front Immunol 2022;13:840916)
- When subacute or chronic, mild nonspecific symptoms (pain, nausea and vomiting) or no symptoms
- Lesions develop as soon as 12 hours after the insult
- Can complicate to ulceration or perforation in severe untreated cases
Diagnosis
- Diagnosis is clinical and endoscopic as well as histological diagnosis which is distinct and characteristic (Arq Gastroenterol 2022;59:275)
Case reports
- 46 year old woman with epigastric pain and anemia (Gastroenterology Res 2017;10:138)
- 52 year old woman with infection of non-Helicobacter pylori Helicobacter (Helicobacter 2021;26:e12814)
- 54 year old man with immune checkpoint inhibitor therapy (Front Immunol 2022;13:840916)
Treatment
- Treatment is supportive
- Includes acid suppressive therapy and removal of the inciting cause
Gross description
- Superficial erosions and punctate mucosal lesions (Arq Gastroenterol 2022;59:275)
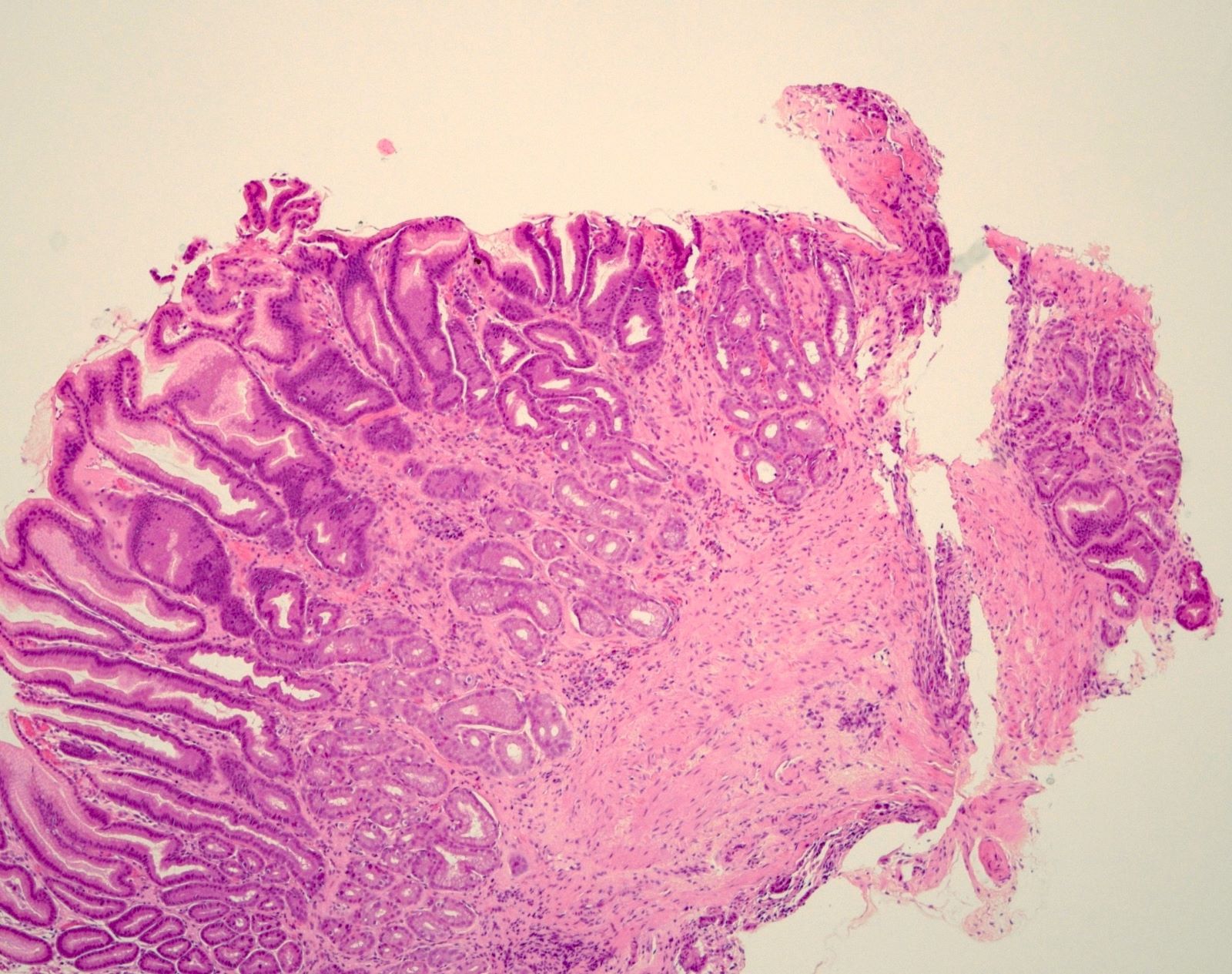
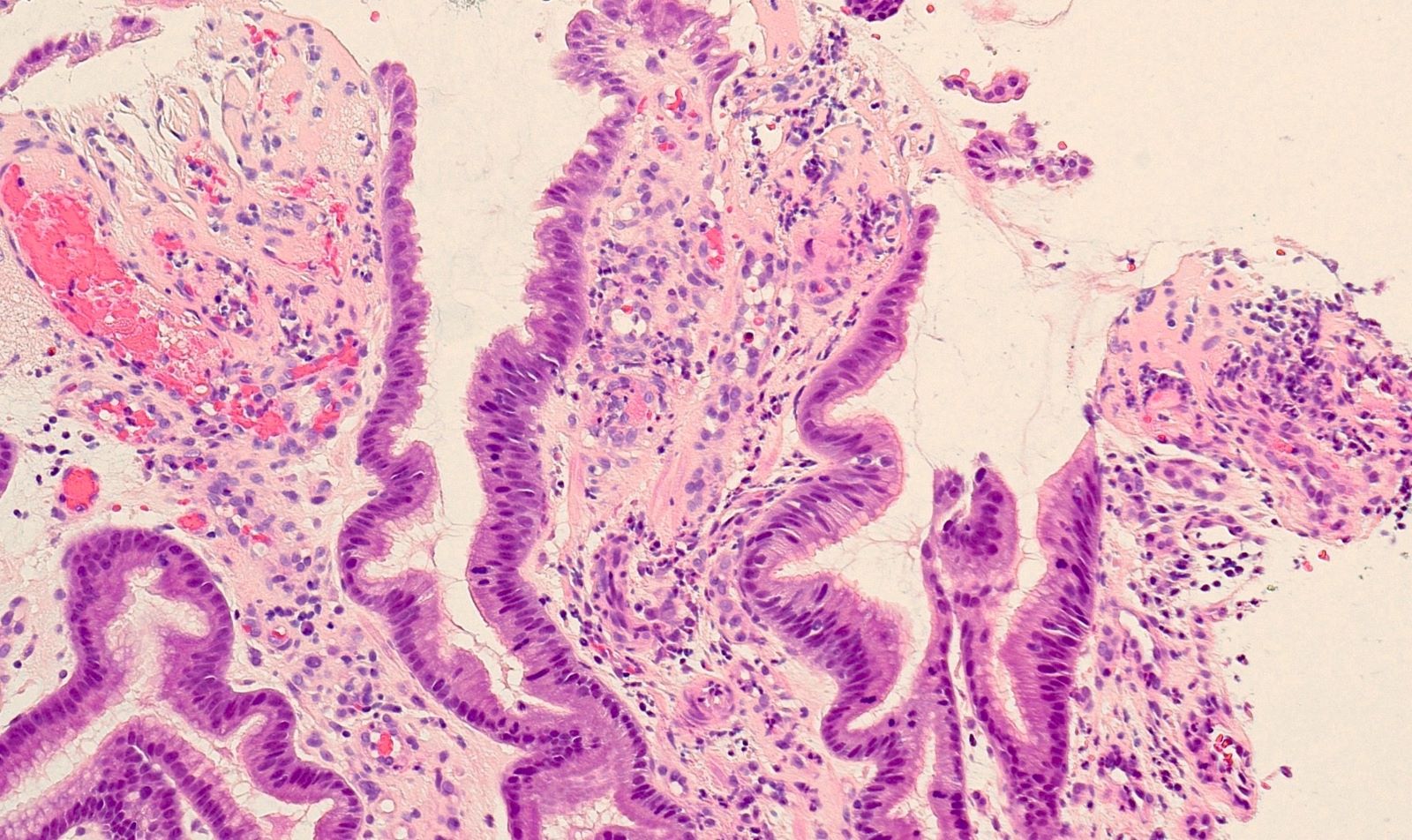
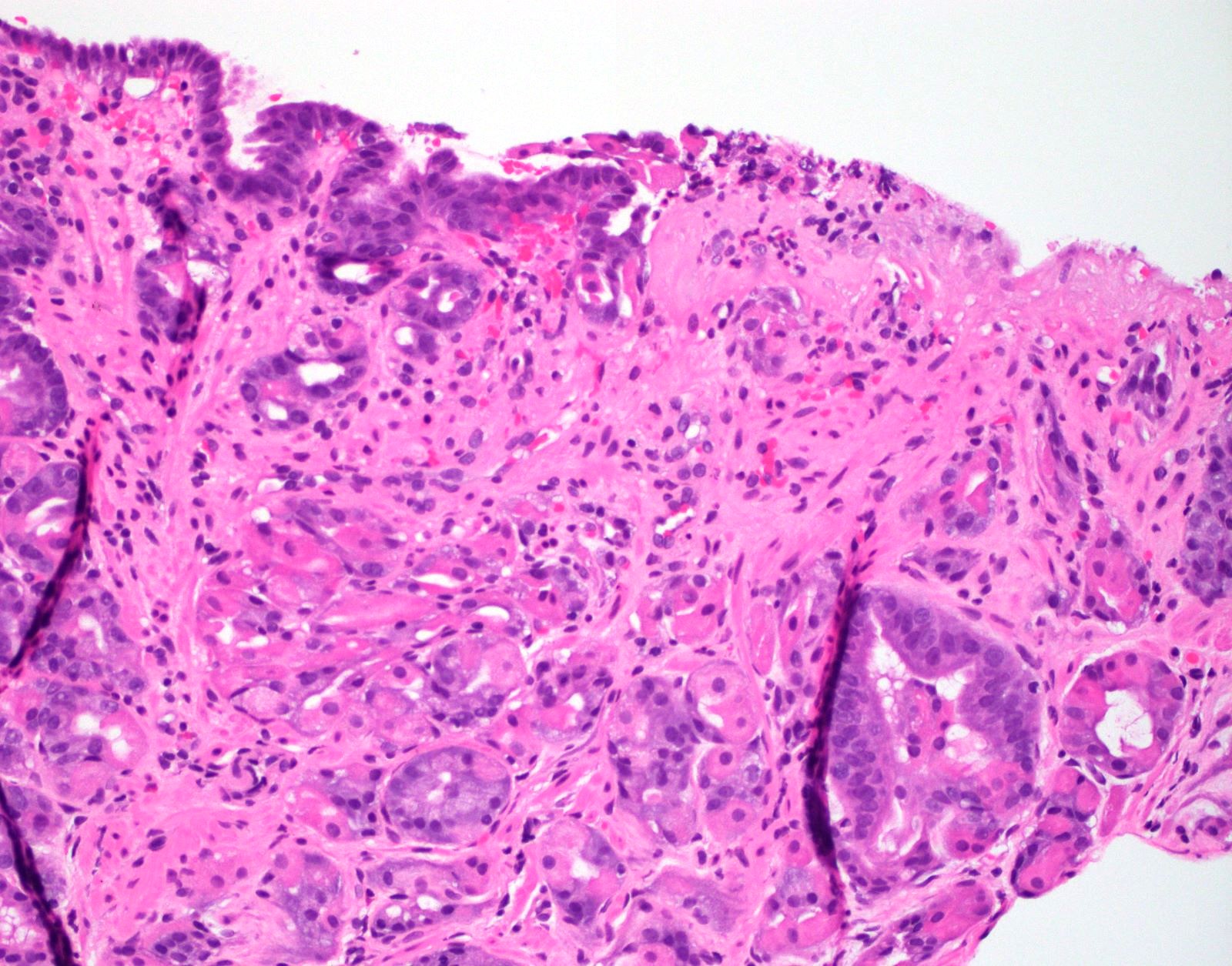
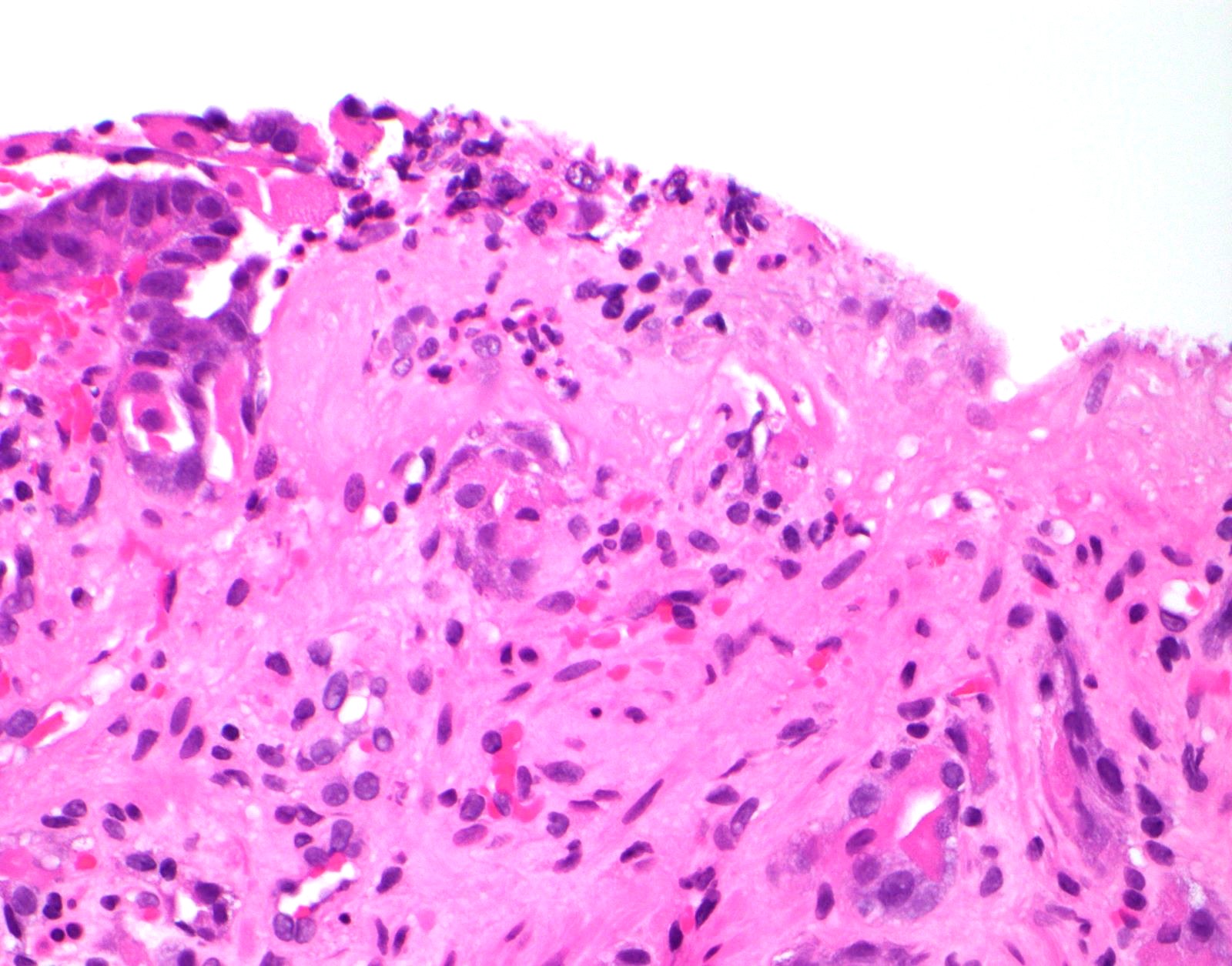
Microscopic (histologic) description
- Loss of superficial epithelium of the gastric mucosa
- Mild to moderate edema, congested vessels and scattered neutrophils in the lamina propria
- Ulceration, granulation tissue and hemorrhage in more severe disease
- Moderate to severe acute inflammatory infiltrate, fibrinopurulent exudate, mucosal sloughing, regenerative changes in the adjacent epithelium in late disease
- References: Arq Gastroenterol 2022;59:275, Korean J Gastroenterol 2017;69:278
Microscopic (histologic) images
Positive stains
- If Helicobacter pylori is the suspected cause, then immunohistochemistry and special stains can be used (see Helicobacter pylori)
Sample pathology report
- Stomach, body, biopsy:
- Erosive gastritis
- No Helicobacter-like organisms identified
- No intestinal metaplasia is seen
Differential diagnosis
- H. pylori gastritis:
- Can show surface erosions
- Chronic inflammation with plasma cells in the lamina propria
- Active (neutrophilic) inflammation in the lamina propria
- Organisms seen on H&E, special stain or immunostain
- Reactive (chemical) gastropathy:
- Lack of erosion or inflammation
- Foveolar hyperplasia
- Gastric antral vascular ectasia:
- Vascular ectasia, fibromuscular proliferation and fibrin thrombi in vessels are the characteristic features
- Portal hypertensive gastropathy:
- Clinical history (portal hypertension) and specific endoscopic findings
Additional references
Practice question #1
A 58 year old man was admitted through the emergency department after suffering from polytrauma in a traffic accident. He becomes vitally stable after resuscitation, however, develops persistent nausea associated with epigastric pain. Gastroendoscopy shows small superficial mucosal erosions or erythematous lesions in the gastric body and fundus. Which of the following is true regarding the pathophysiology of development of this condition in this patient?
- Angiotensin II is released, which increases blood flow to the gastric mucosa
- Elevated levels of ACH and histamine in stress result in decreased acid production
- Increased acid secretion leads to the development of gastric erosions
- Naturally produced nitric oxide is an enhancing factor for gastric erosion
- There is no significant dysregulation of gastric pH during the process
Practice answer #1
C. Increased acid secretion leads to the development of gastric erosions. One of the most common causes of erosive gastritis is stress. In the stressed state (may be due to physiologic stress related to severe trauma, severe burns, ventilator dependency or intracranial trauma), elevated levels of ACH and histamine result in increased acid production, thus inducing erosive gastritis, which can later on lead to hemorrhage if left undiagnosed / untreated. Naturally produced nitric oxide is believed to be protective against stress gastritis, as it leads to vasodilation. Angiotensin II is released as a result of stress, which decreases blood flow to the gastric mucosa, resulting in formation of reactive oxygen species (StatPearls: Stress Induced Gastritis [Accessed 6 February 2023]).
Comment Here
Reference: Erosive gastritis
Comment Here
Reference: Erosive gastritis
Practice question #2
A 42 year old woman with rheumatoid arthritis presents with dyspepsia and bloating. Gastroendoscopy shows small erythematous lesions in the gastric body. On histopathology, there are surface erosions with ectatic superficial capillaries and mild edema in the lamina propria (see image above). Intestinal metaplasia is not seen. What is the diagnosis?
- Erosive gastritis
- Gastric antral vascular ectasia (GAVE)
- H. pylori gastritis
- Low grade dysplasia
- Reactive gastropathy
Practice answer #2
A. Erosive gastritis. Longstanding NSAID use (in this case, for rheumatoid arthritis) predisposes a patient to erosive gastritis. In this patient, there were small erythematous lesions in the gastric body and histology is compatible erosive gastritis. GAVE usually shows watermelon stomach; endoscopically and histologically there is increase in blood vessel number and diameter with fibrin thrombi and fibromuscular hyperplasia. H. pylori gastritis will show active chronic gastritis with organisms which can be seen on H&E, special stain or immunostain. Low grade dysplasia will show hyperchromatic and pleomorphic nuclei within tall columnar epithelium. There will be abrupt transition from benign to dysplastic epithelium.
Reactive gastropathy is characterized by foveolar hyperplasia, mucin depletion in surface epithelial cells and lamina propria expansion by fibromuscular and capillary hyperplasia (Cureus 2020;12:e10873).
Comment Here
Reference: Erosive gastritis
Comment Here
Reference: Erosive gastritis