Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Diez Freire C, Masood S. Duct ectasia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/breastductectasia.html. Accessed May 3rd, 2024.
Definition / general
- Mammary duct ectasia is a disorder of the extralobular ducts
- Is characterized by different degrees of periductal inflammation, periductal fibrosis and duct dilatation
- Foamy histiocytes are typically present within the luminal secretions and infiltrate the wall of the involved ducts
Essential features
- Foamy histiocytes within luminal secretions and within wall and epithelium of involved ducts
- Periductal inflammation, can be plasma cell heavy
- Periductal fibrosis in late stages
Terminology
- Also called mastitis obliterans and comedo mastitis, although these terms have not been as widely used as duct ectasia
ICD coding
- ICD-10: N60.49 - mammary duct ectasia of unspecified breast
Epidemiology
- Usually women in perimenopausal and postmenopausal age
- It can occur in neonates
Sites
- Extralobular ducts; retro areolar, can be bilateral
Etiology
- Not well known
- Some authors believe that involution seen in postmenopausal women is the primary pathologic process (gland atrophy → stasis of secretions → leakage of lipid rich material through duct wall → periductal inflammation)
- Other authors believe that periductal inflammation is the inciting process that is followed by duct sclerosis, obliteration and finally ectasia
- Stasis caused by duct obstruction is considered by some to be the inciting cause of duct inflammation with further obstruction, stasis and dilatation as observed in cases of squamous metaplasia of lactiferous ducts (SMOLD)
- Smoking, phenothiazine treatment and hyperprolactinemia have been postulated as possible causes (Hoda: Rosen's Breast Pathology, 4th Edition, 2014)
Clinical features
- Typically, the age of presentation can range from 40 - 70 years old although it has been described in children and is rarely seen in men (Hoda: Rosen's Breast Pathology, 4th Edition, 2014)
- Pain, nipple discharge (can be clear, cloudy or bloody), nipple retraction or a mass (worm-like doughy palpable mass beneath the nipple) can be the clinical presentation (Hoda: Rosen's Breast Pathology, 4th Edition, 2014)
- By mammography can resemble DCIS due to the ductal pattern of calcifications that can be present (Schnitt: Biopsy Interpretation of the Breast, 3rd Edition, 2017, O'Malley: Breast Pathology, A Volume in the Series, Foundations in Diagnostic Pathology, 2nd Edition, 2011)
Case reports
- 14 month old boy with nipple discharge (Ann Surg Treat Res 2014;86:165)
- 42 year old woman with galactorrhea (Endocrine Abstracts 2017;49:EP1053)
Treatment
- Circumareolar incision and removal of the affected duct and fistula tract, if present, is the treatment of choice
Gross description
- Firm fibrotic breast tissue with prominent dilated and thick walled ducts filled with a tan-white, creamy to brown colored pasty or granular secretions (Schnitt: Biopsy Interpretation of the Breast, 3rd Edition, 2017, O'Malley: Breast Pathology, A Volume in the Series, Foundations in Diagnostic Pathology, 2nd Edition, 2011)
- Calcifications with abscess formation can also be seen (Hoda: Rosen's Breast Pathology, 4th Edition, 2014)
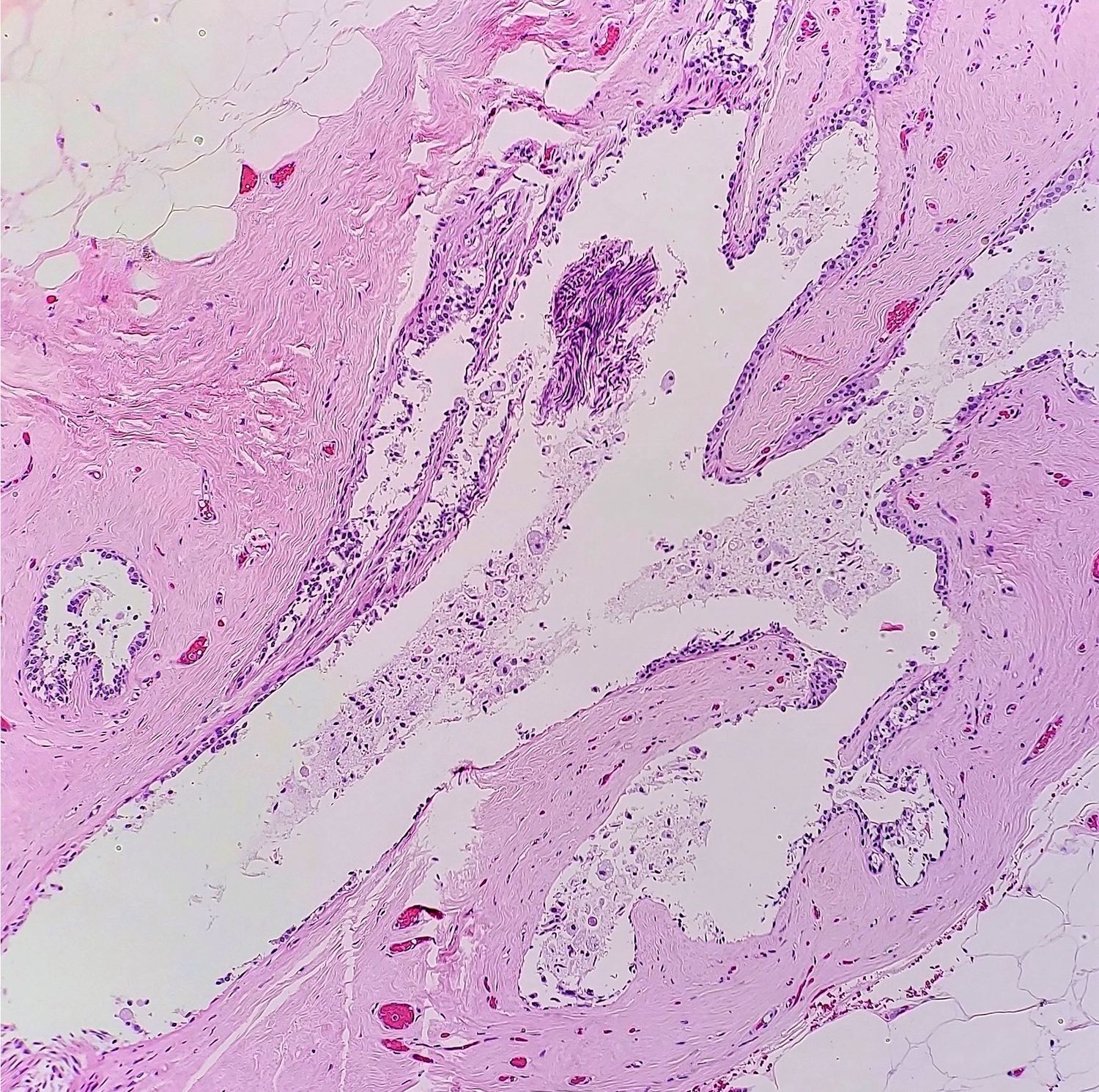
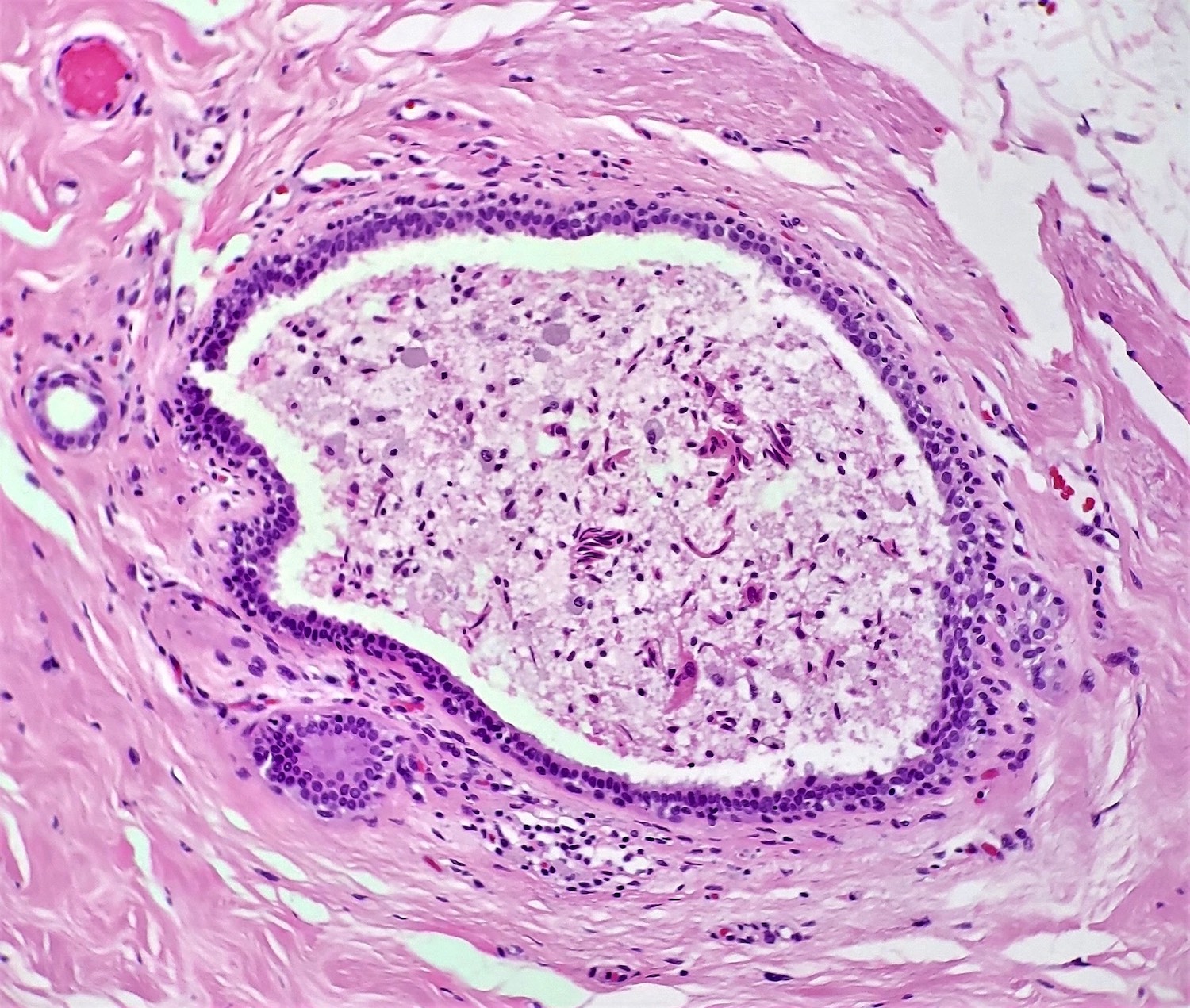
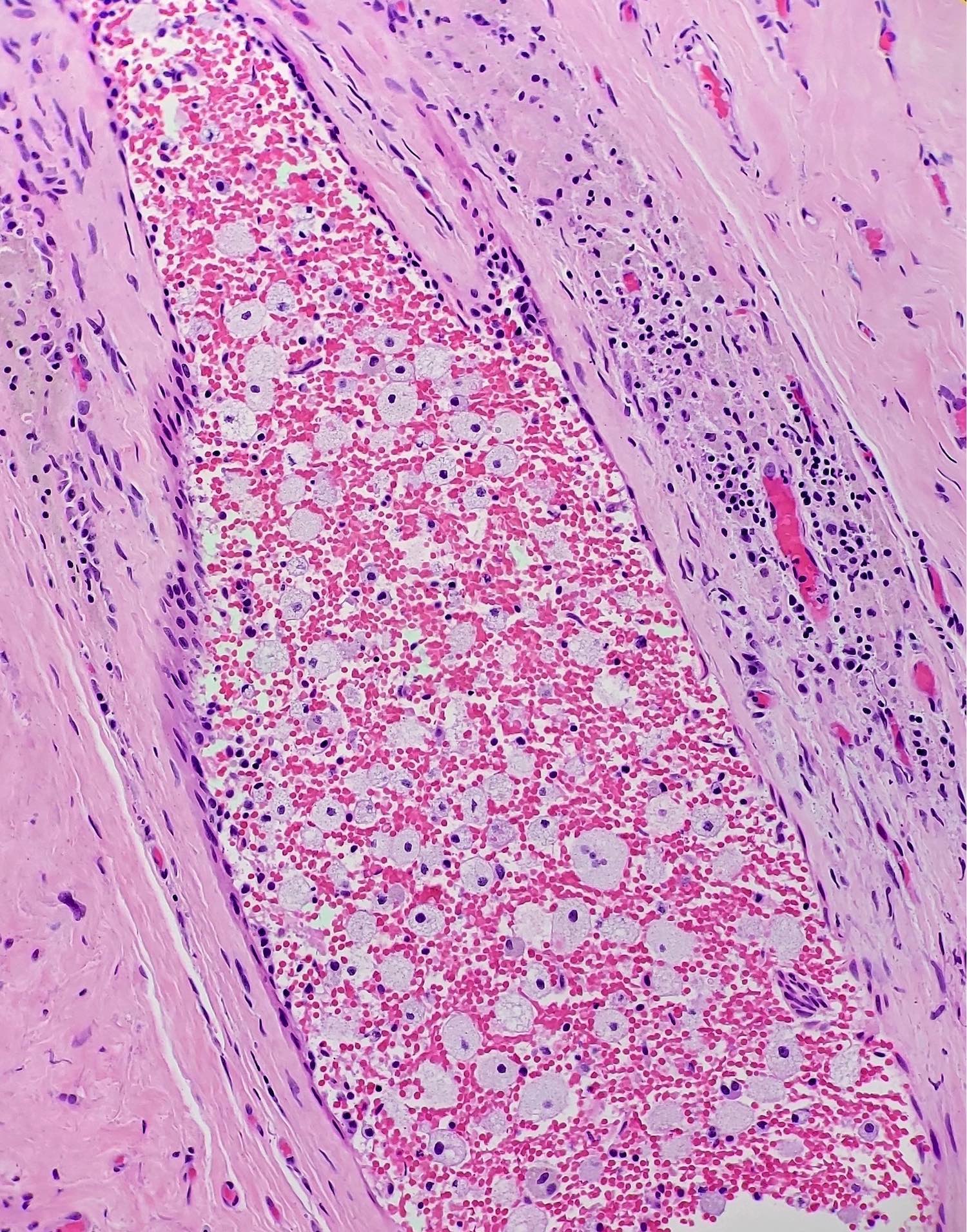
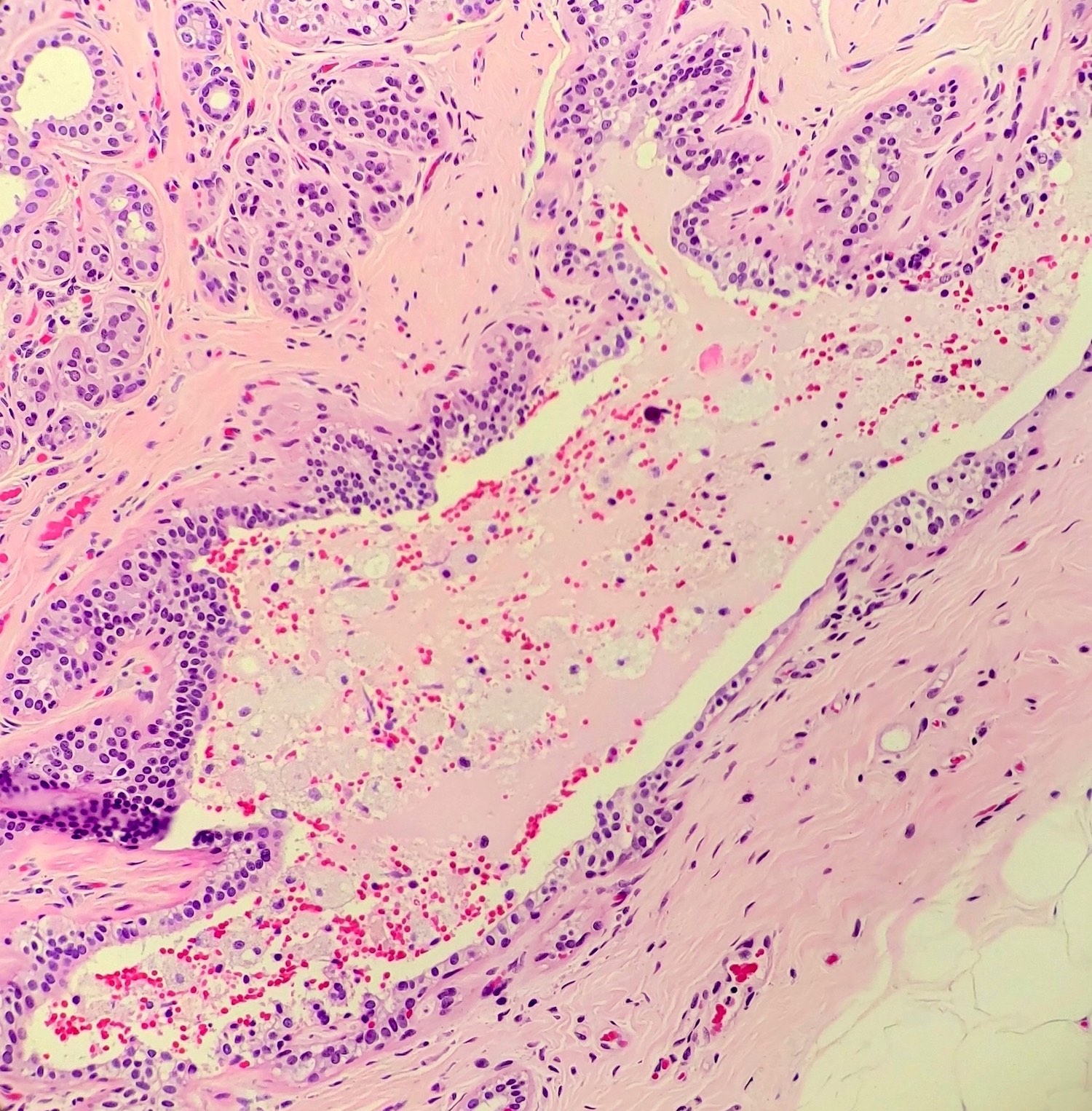
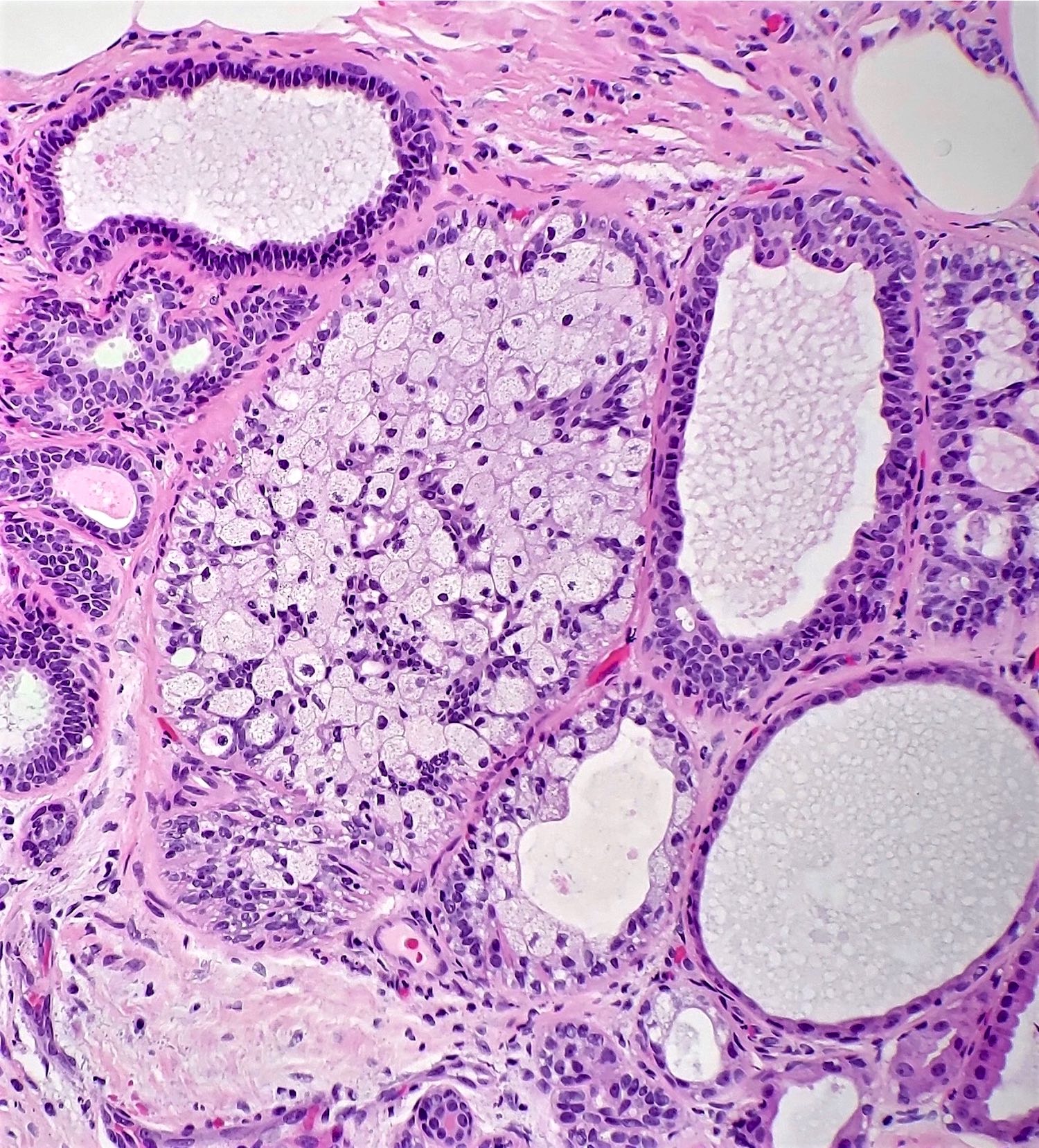
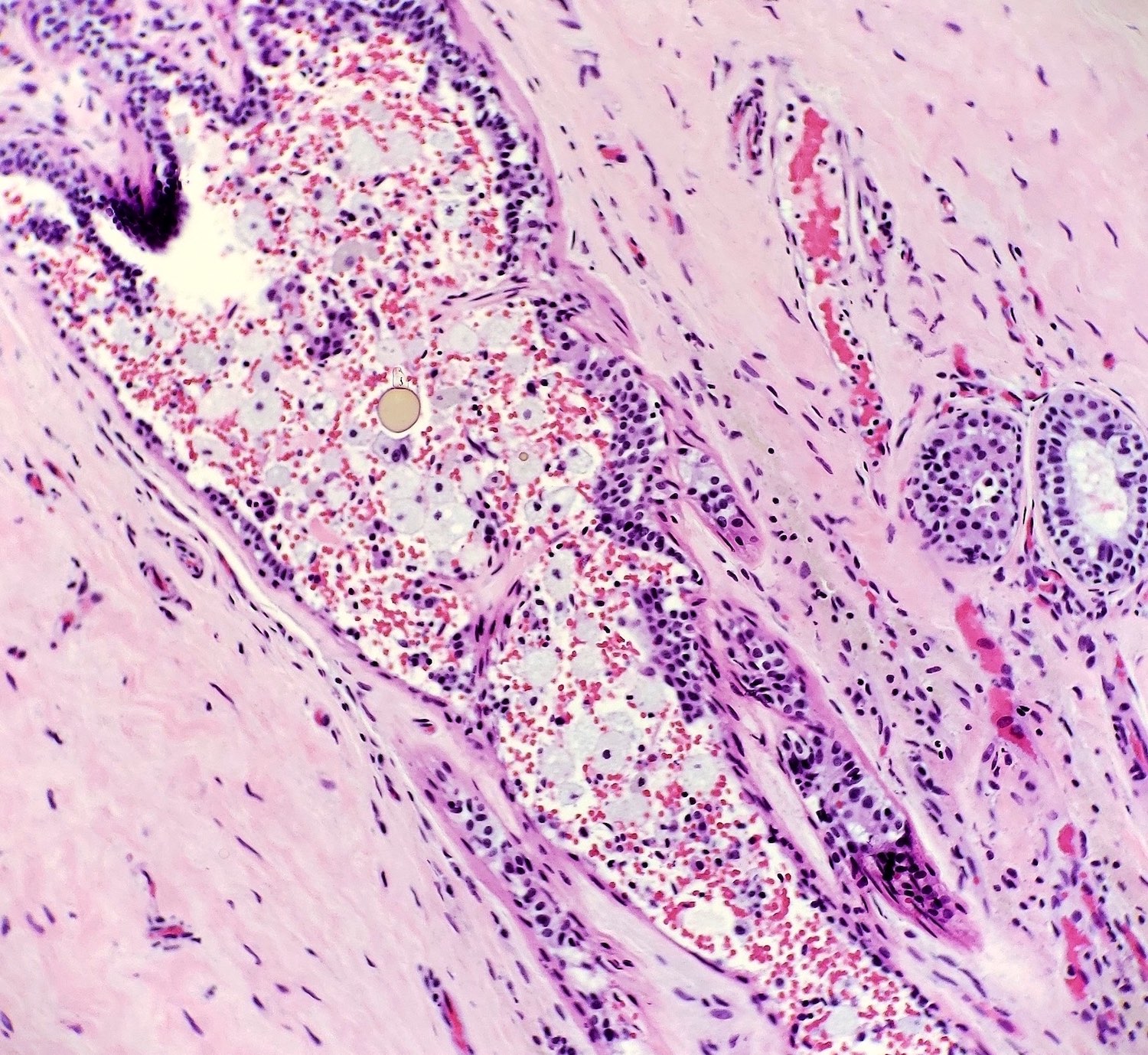
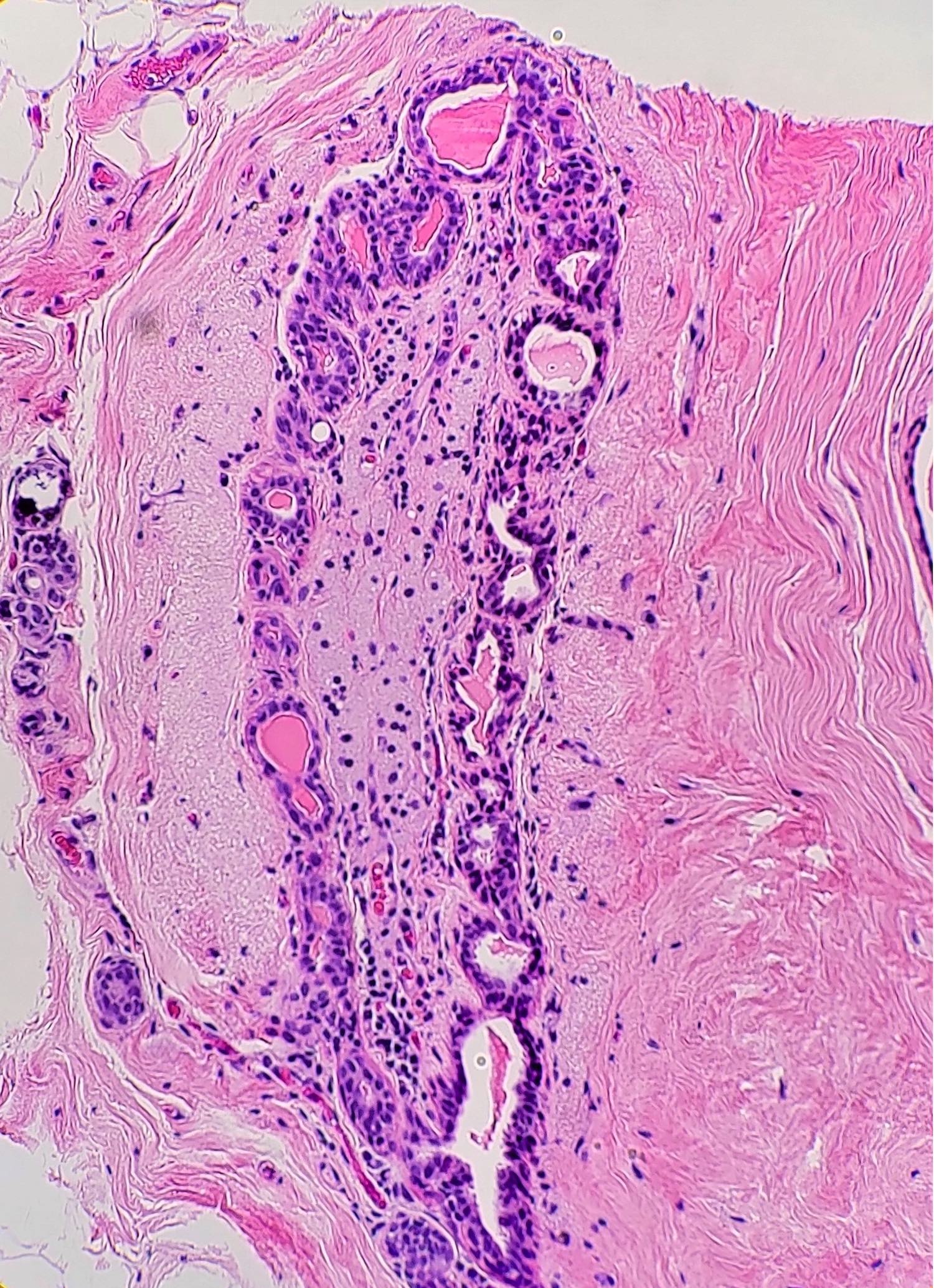
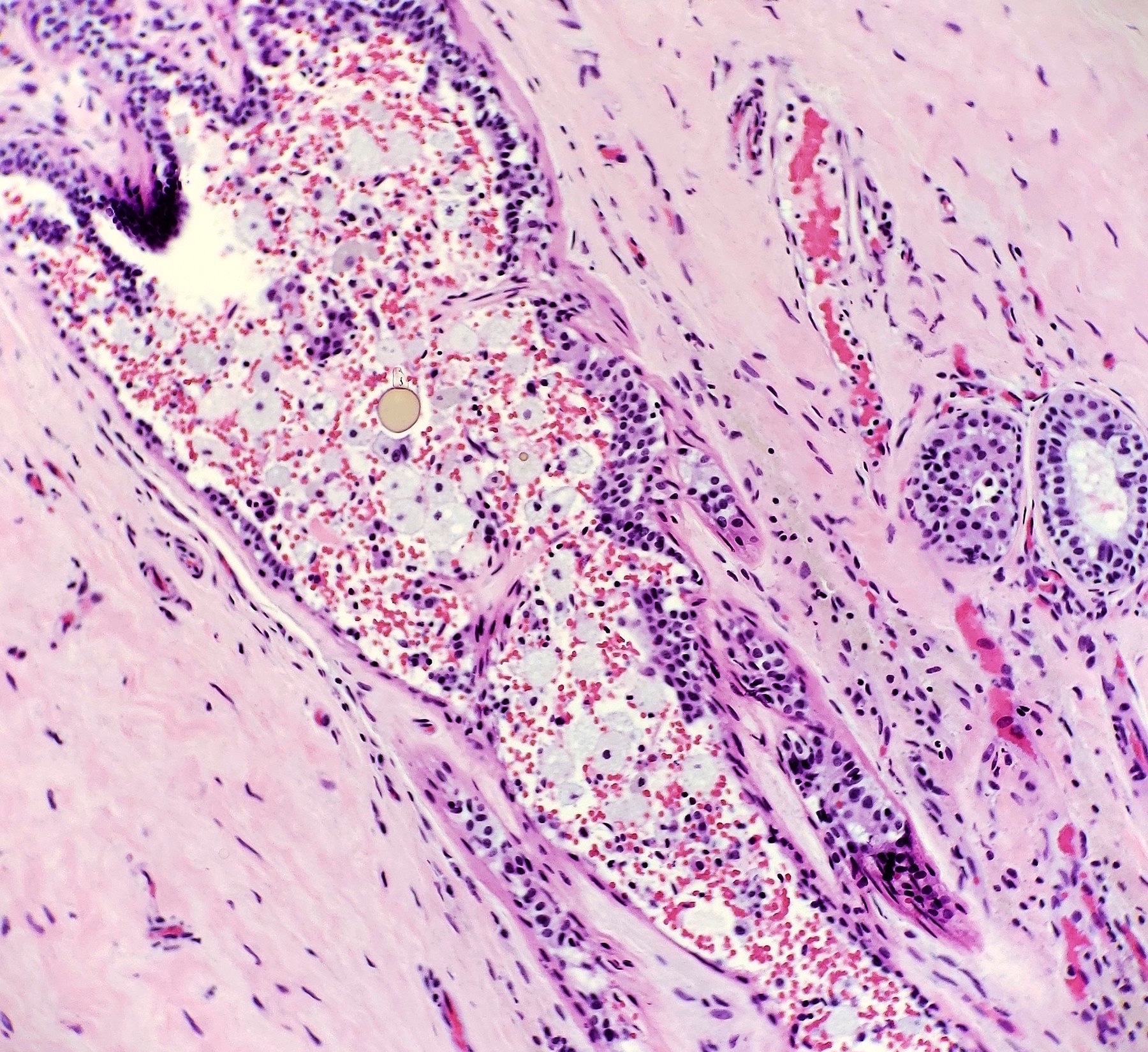
Microscopic (histologic) description
- Dilation of ducts with foamy histiocytes within the luminal secretions and infiltrating the wall of the involved ducts
- Periductal inflammation with lymphocytes, plasma cells, neutrophils and histiocytes; these can become multinucleated in cases of duct rupture due to reaction to spilled secretions in the stroma
- Periductal fibrosis with obliteration of the duct’s lumen can also be seen (garland sign)
Microscopic (histologic) images
Cytology description
- Thick cheesy secretion composed of amorphous material and cellular debris that resembles necrosis
- Amorphous material may have a crack artifact as seen in watery thyroid colloid
- Small crowded groups or sheets of ductal cells with reactive atypia may be present
- The inflammatory component has plasma cells (can be abundant), neutrophils and foamy macrophages that can have pigment
- Giant cells, calcifications and cholesterol clefts can also be present (DeMay: Art and Science of Cytopathology, Volume 2, Superficial Aspiration Cytology, 2nd Edition, 2012)
Positive stains
- CD68 highlights luminal and subepithelial histiocytes
Sample pathology report
- Left breast, 2 o’clock, 5 cm from nipple, ultrasound guided core biopsy:
- Duct ectasia
Differential diagnosis
- Breast abscess:
- Presence of severe acute inflammatory infiltrate
- Often associated with lactation
- Ductal carcinoma in situ:
- Neoplastic epithelial cells confined to the mammary ductal lobular unit
- Can have expansive comedo type necrosis
Board review style question #1
Board review style answer #1
C. Most commonly affects the extralobular ducts in the retroareolar region. The photo depicts duct ectasia. Answer A is incorrect because a history of duct ecstasia does not increase risk for breast carcinoma. Answer B is incorrect because duct ecstasia can be bilateral. Answer D is incorrect because duct ecstasia is most common in perimenopausal and postmenopausal women.
Comment Here
Reference: Duct ectasia of breast
Comment Here
Reference: Duct ectasia of breast
Board review style question #2
Mammary duct ectasia is characterized by which of the following microscopic findings?
- Epithelial proliferation that fills and distends the terminal duct lobular units
- Infiltrating ductal proliferation with desmoplastic stromal response
- Periductal inflammation and dilation of ducts, with foamy histiocytes within the luminal secretions and infiltrating the wall of ducts
- Proliferation of both stromal and glandular elements
Board review style answer #2
C. Periductal inflammation and dilation of ducts, with foamy histiocytes within the luminal secretions and infiltrating the wall of ducts with periductal inflammation. Duct estasia is characterized by different degrees of periductal inflammation, periductal fibrosis and duct dilation, as well as the presence of foamy histiocytes within luminal secretions and the periductal epithelium. Answers A, B and D are incorrect because duct ectasia is a benign nonproliferative disease.
Comment Here
Reference: Duct ectasia of breast
Comment Here
Reference: Duct ectasia of breast