Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Negative stains | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Hall KC, Biernacka A. SMOLD. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/breastsmold.html. Accessed September 12th, 2025.
Definition / general
- Keratinizing squamous metaplasia of lactiferous ducts (SMOLD) in association with acute and chronic inflammation including foreign body giant cells
Essential features
- Retroareolar inflammatory lesion due to lactiferous duct blockage and rupture secondary to keratinizing squamous metaplasia
- Strong association with smoking
- Characteristic microscopic findings include a mixed inflammatory infiltrate including keratinaceous debris within giant cells and lactiferous ducts with squamous metaplasia or intraluminal keratin
- Recurrence is common without definitive treatment, including excision of the affected duct and smoking cessation
Terminology
- Zuska disease, recurrent subareolar abscess, periductal mastitis, subareolar fistula
ICD coding
- ICD-10: N61 - inflammatory disorders of breast
Epidemiology
- Uncommon, found in women and men
- Often fourth to fifth decade of life; range: 14 - 79 years old (Surg Clin North Am 2022;102:1103)
Sites
- Subareolar, breast (bilateral)
Pathophysiology
- Accumulation of keratin secondary to squamous metaplasia in deeper lactiferous ducts with subsequent blockage and rupture
- Rupture of duct with extrusion of keratinaceous debris incites a mixed inflammatory response
- Secondary infection or abscess may occur
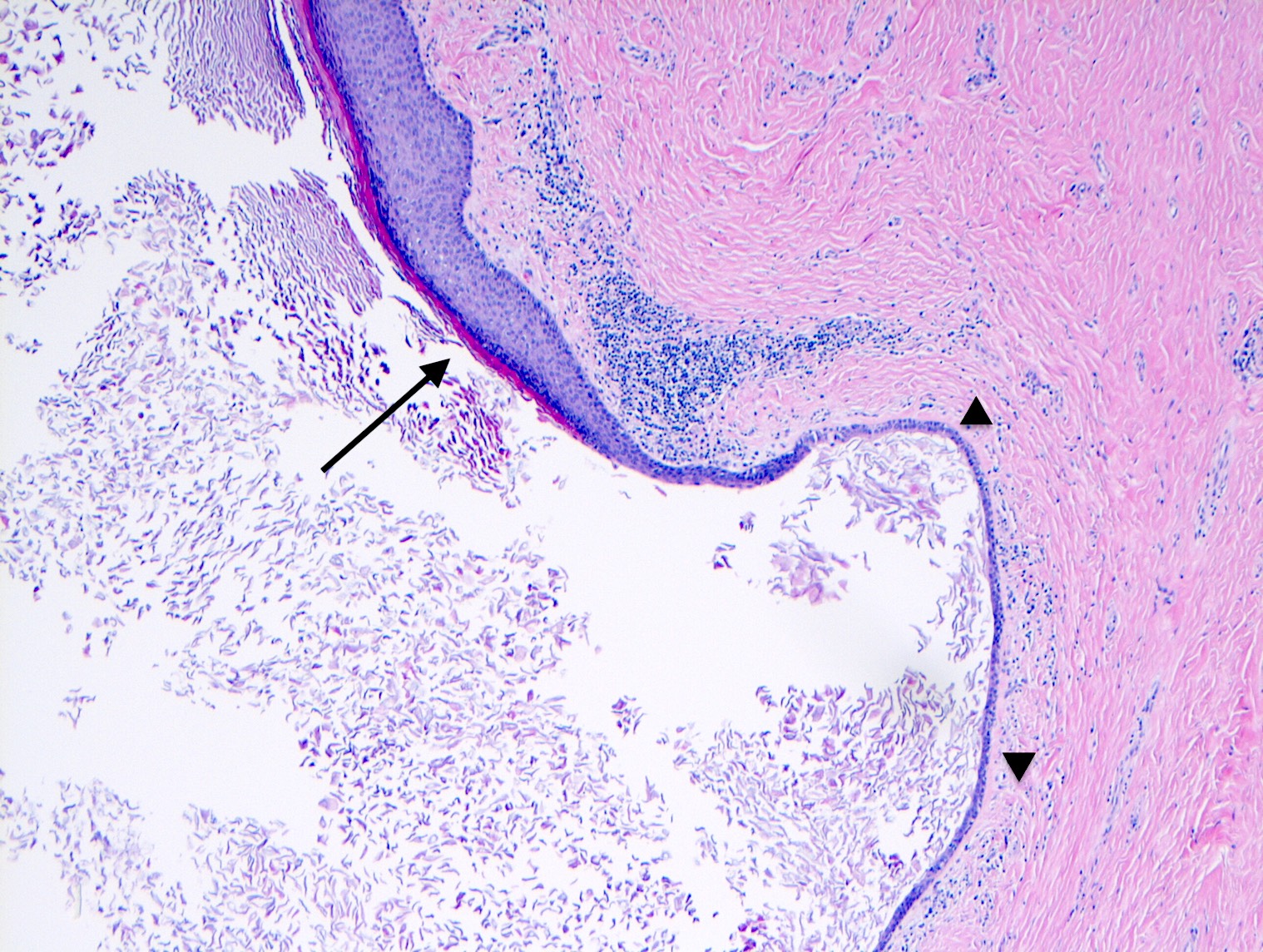
- Repeat recurrences may lead to fistula formation
- Fistula tract forms beneath smooth muscle of areola, which is a path of least resistance
- Reference: Schnitt: Biopsy Interpretation of the Breast, 3rd Edition, 2017
Etiology
- Strong correlation with smoking
- Relative vitamin A deficiency related to smoking may be a causative factor in squamous metaplasia
- Less common associations
- Congenital nipple cleft and nipple piercings (Surg Clin North Am 2022;102:1103)
Clinical features
- Painful, warm, erythematous swelling or mass near nipple
- Often misinterpreted as an abscess
- Less common features include purulent nipple discharge, skin thickening or ipsilateral axillary lymphadenopathy
- Inverted nipple can be seen
- Fistula tract opening at the edge of the areola is characteristic
- Reference: Schnitt: Biopsy Interpretation of the Breast, 3rd Edition, 2017
Diagnosis
- Integrative diagnosis utilizing clinical findings, radiology and pathology
Radiology description
- Mammogram: retroareolar localized increased stroma / asymmetric density; less common findings include stromal distortion, solitary mass or normal imaging (Clin Radiol 2012;67:e42)
- Ultrasound: medial periareolar hypoechoic lesion, possibly with discreet sinus or abscess with adjacent dilated ducts (Clin Radiol 2012;67:e42)
Case reports
- 29 year old woman with 8 month history of nipple cellulitis and inversion (BMJ Case Rep 2020;13:e237568)
- 56 year old woman with recurrent left subareolar breast abscesses and fistula associated with Prevotella bivia infection (Cureus 2022;14:e28904)
- 82 year old woman with diagnosis of SMOLD in association with primary squamous cell carcinoma (Breast Cancer 2018;25:365)
Treatment
- Excision of affected duct is most effective
- Antibiotics or incision and drainage procedures result in recurrence
- Ultrasound guided percutaneous needle electrolysis (PNE) was effective treatment in a small series (J Clin Med 2020;9:649)
- Smoking cessation is recommended
- Reference: BMJ Case Rep 2020;13:e237568
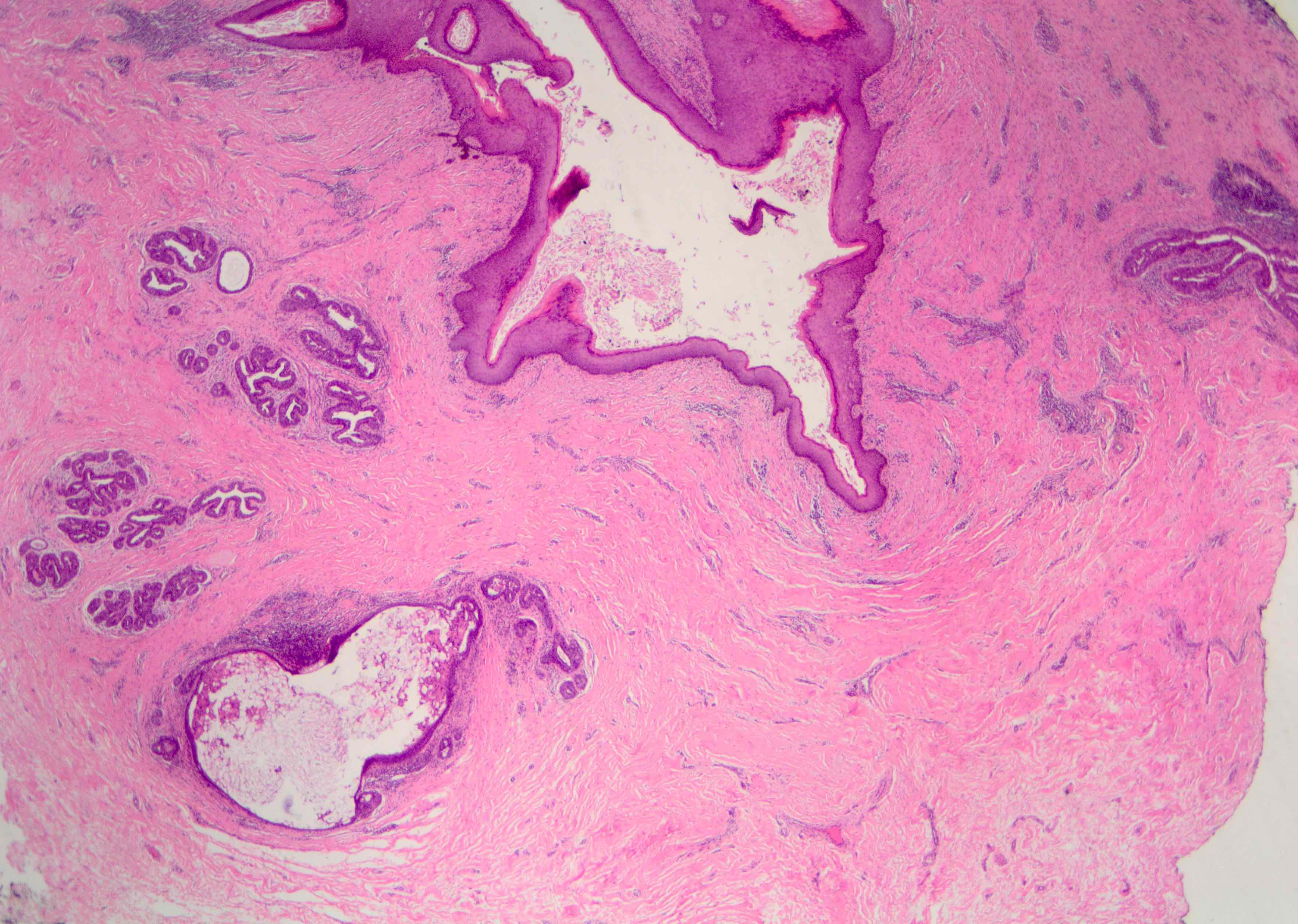
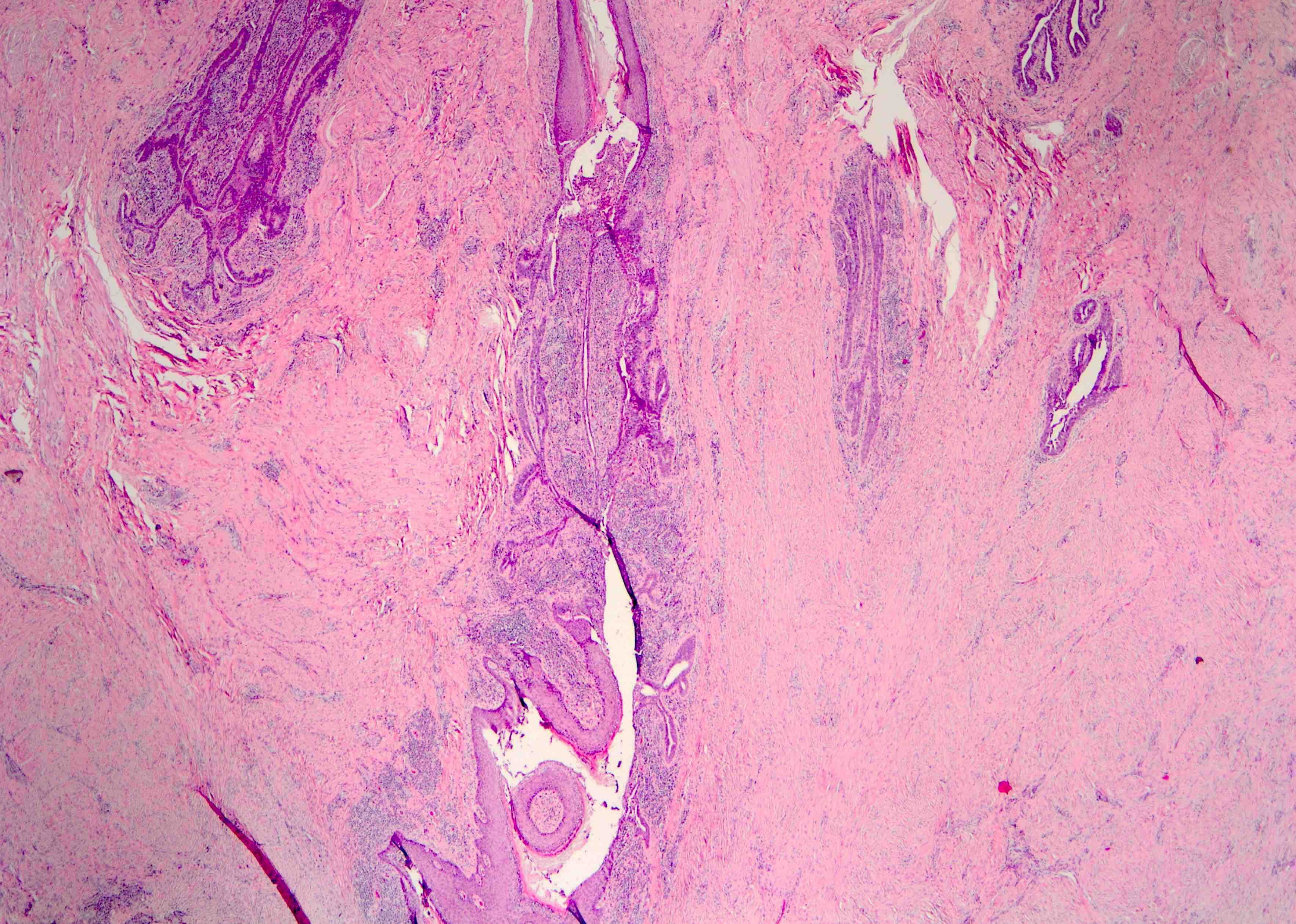
Gross description
- Portion (or entire) nipple - areola complex and underlying breast tissue containing possible fistula tract or abscess
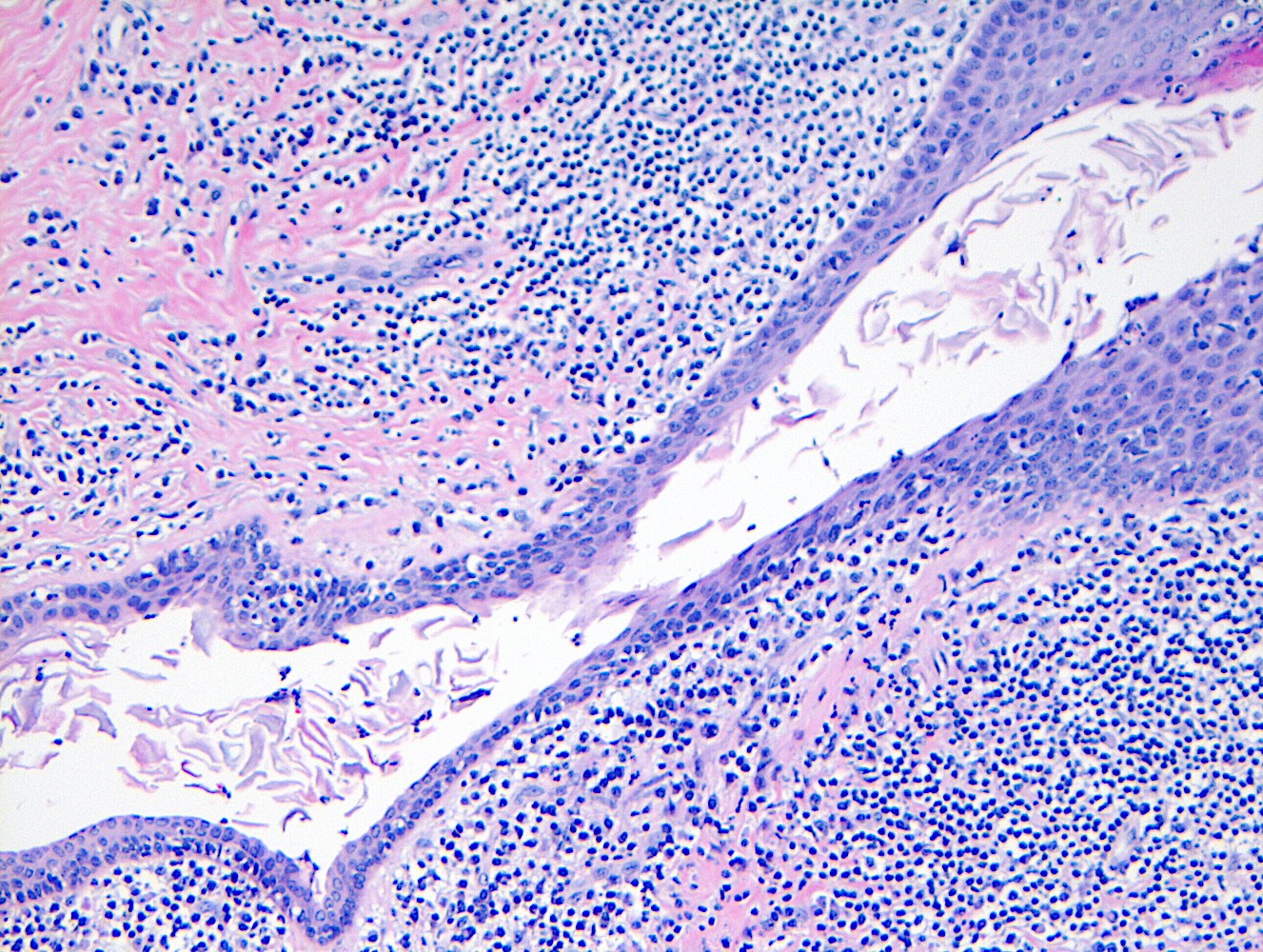
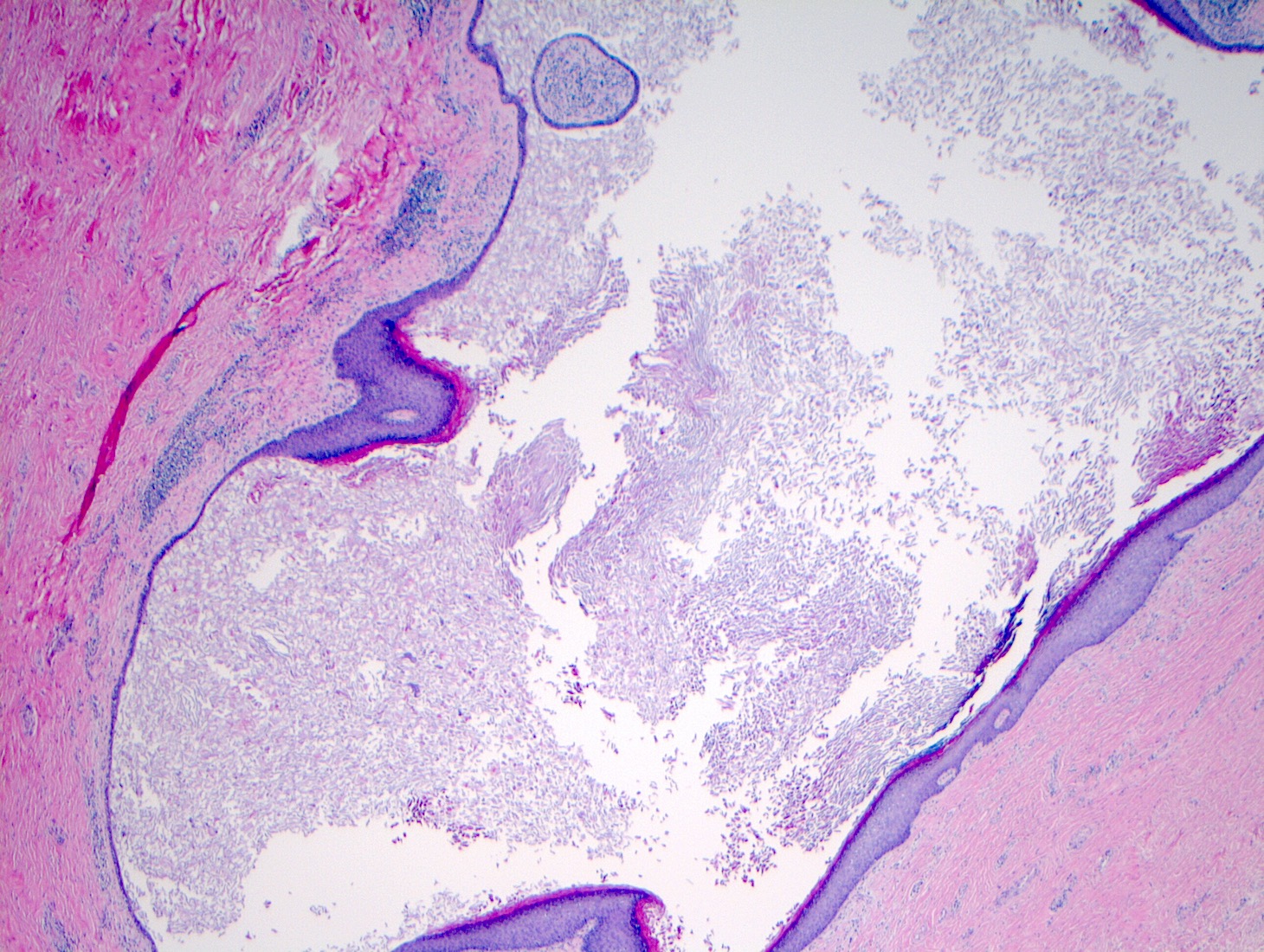
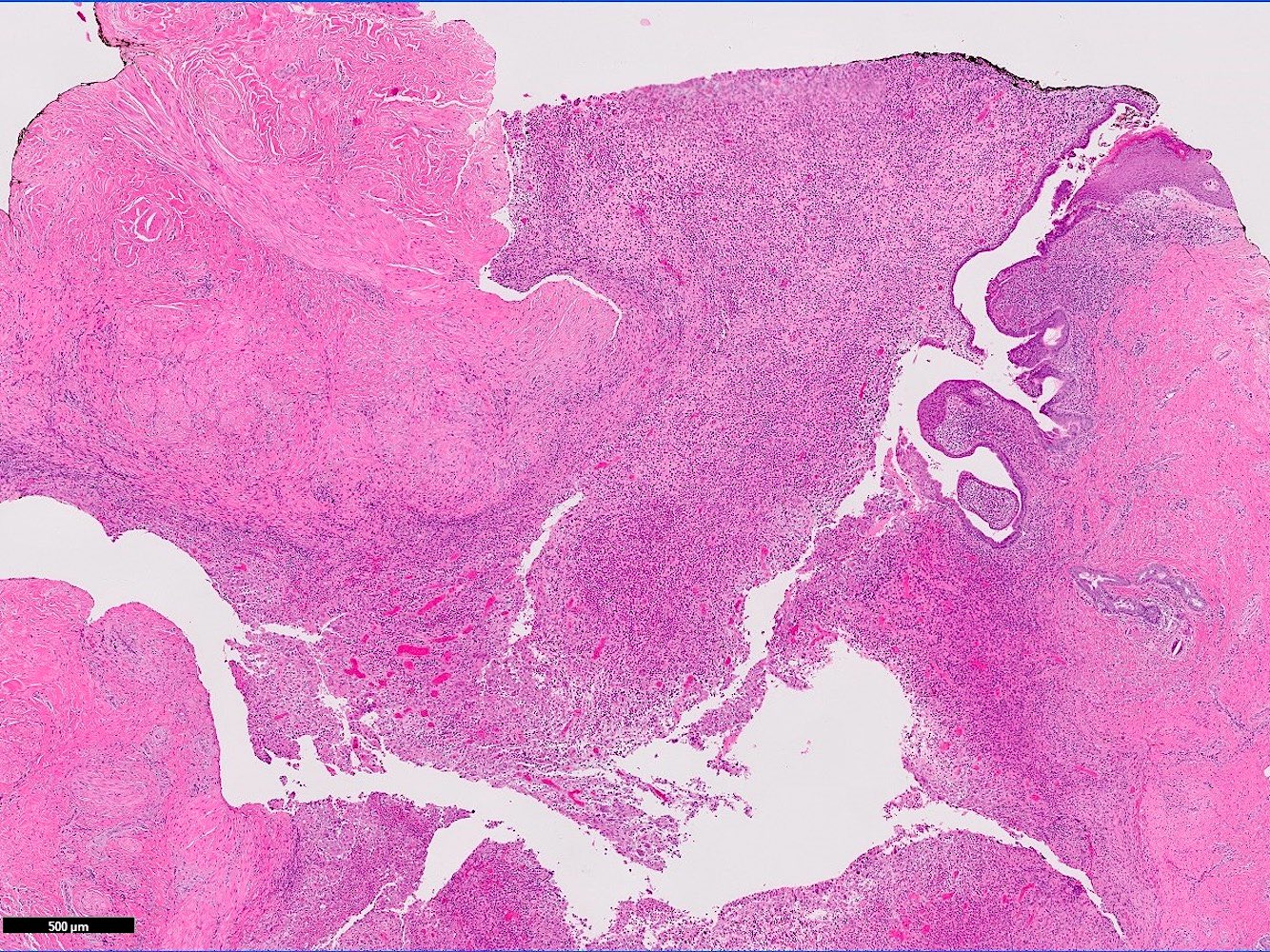
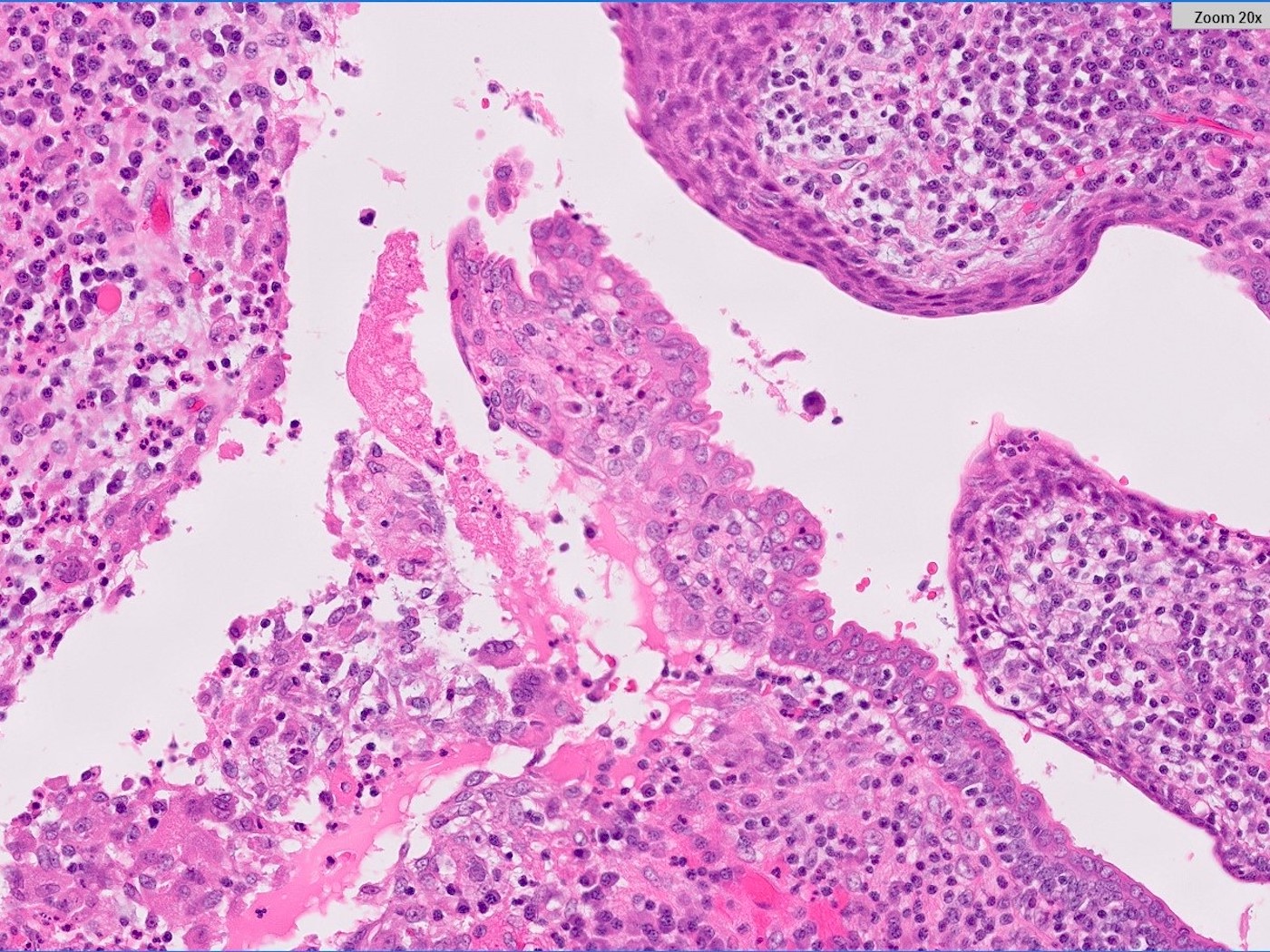
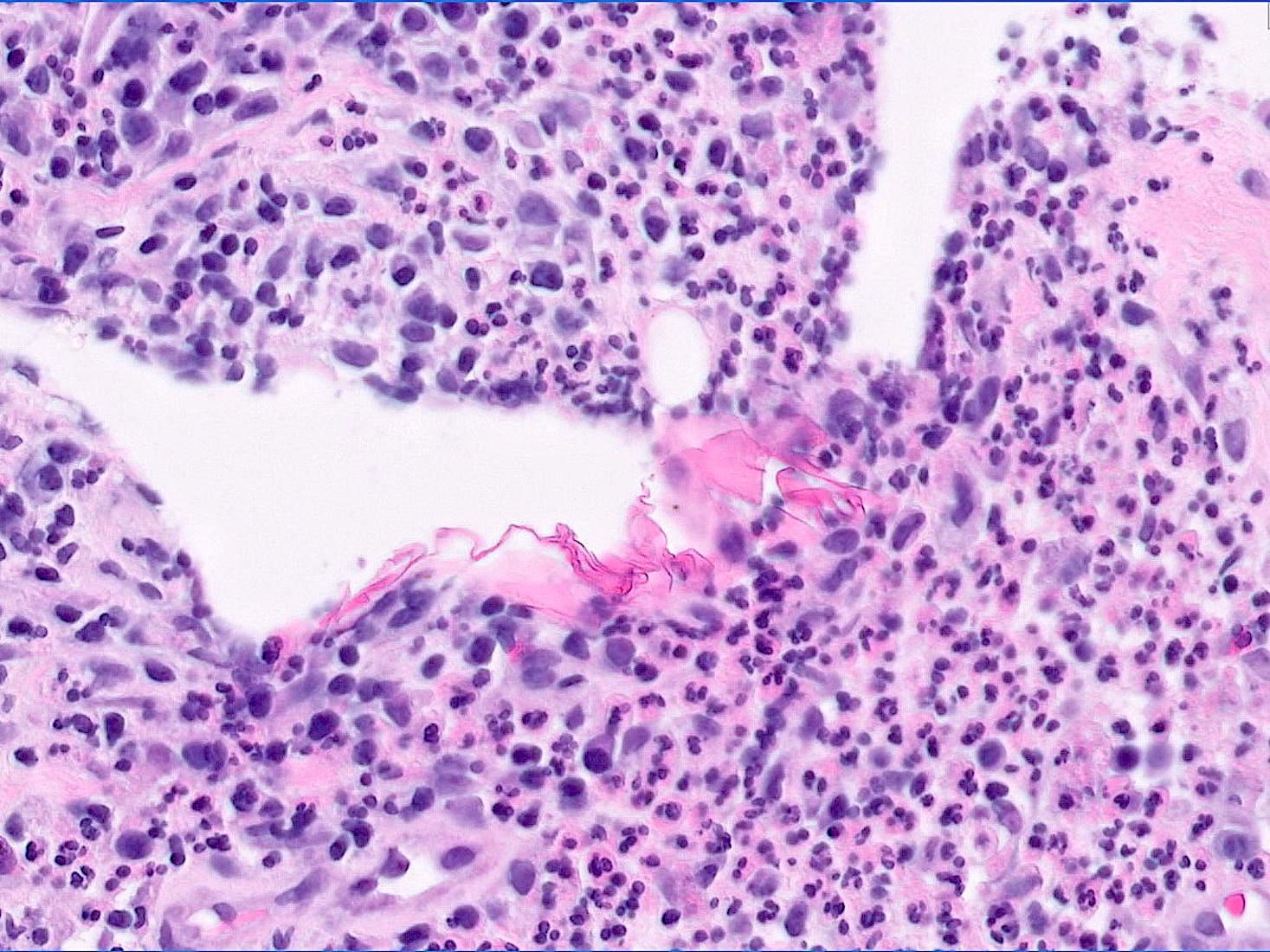
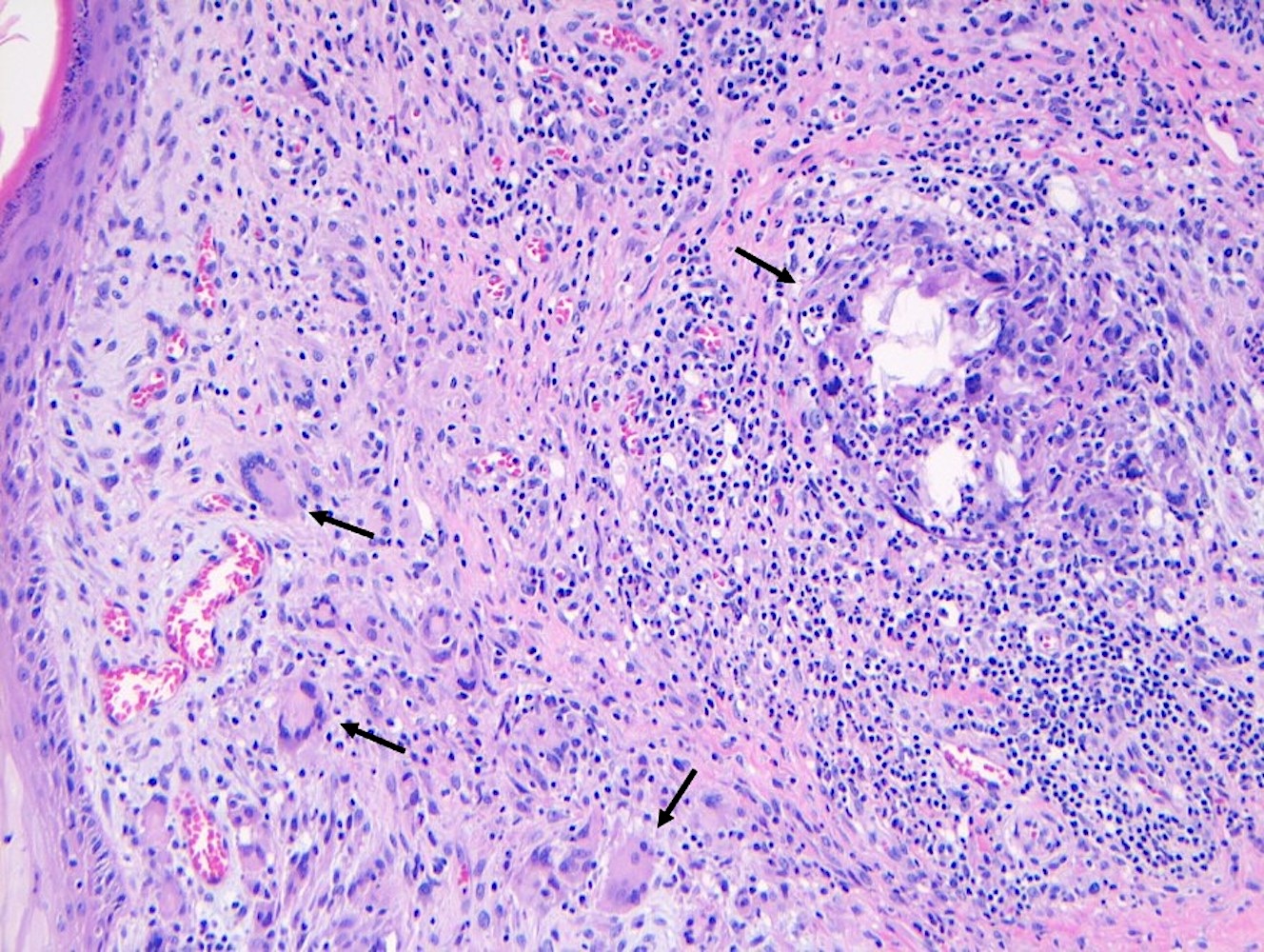
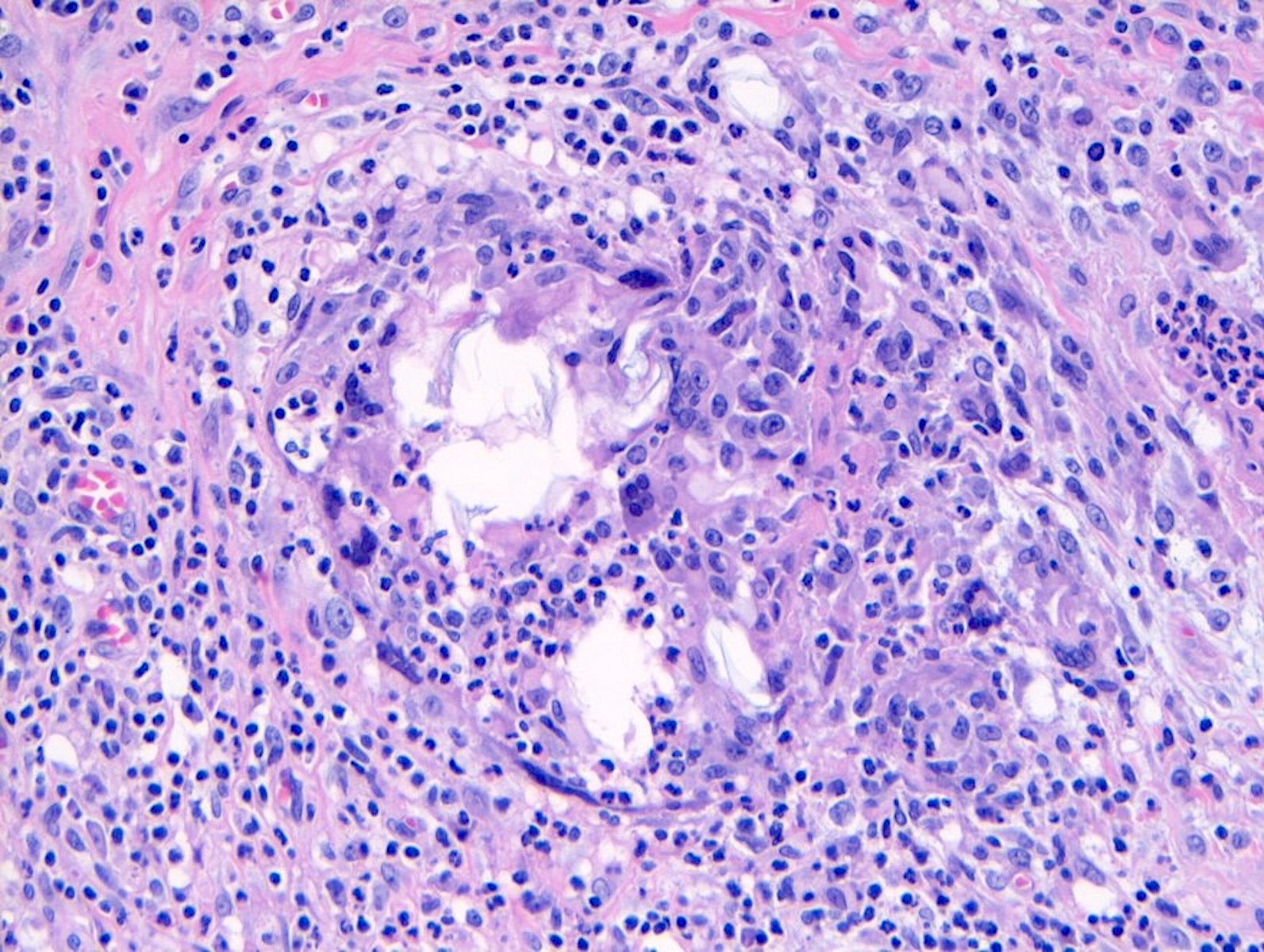
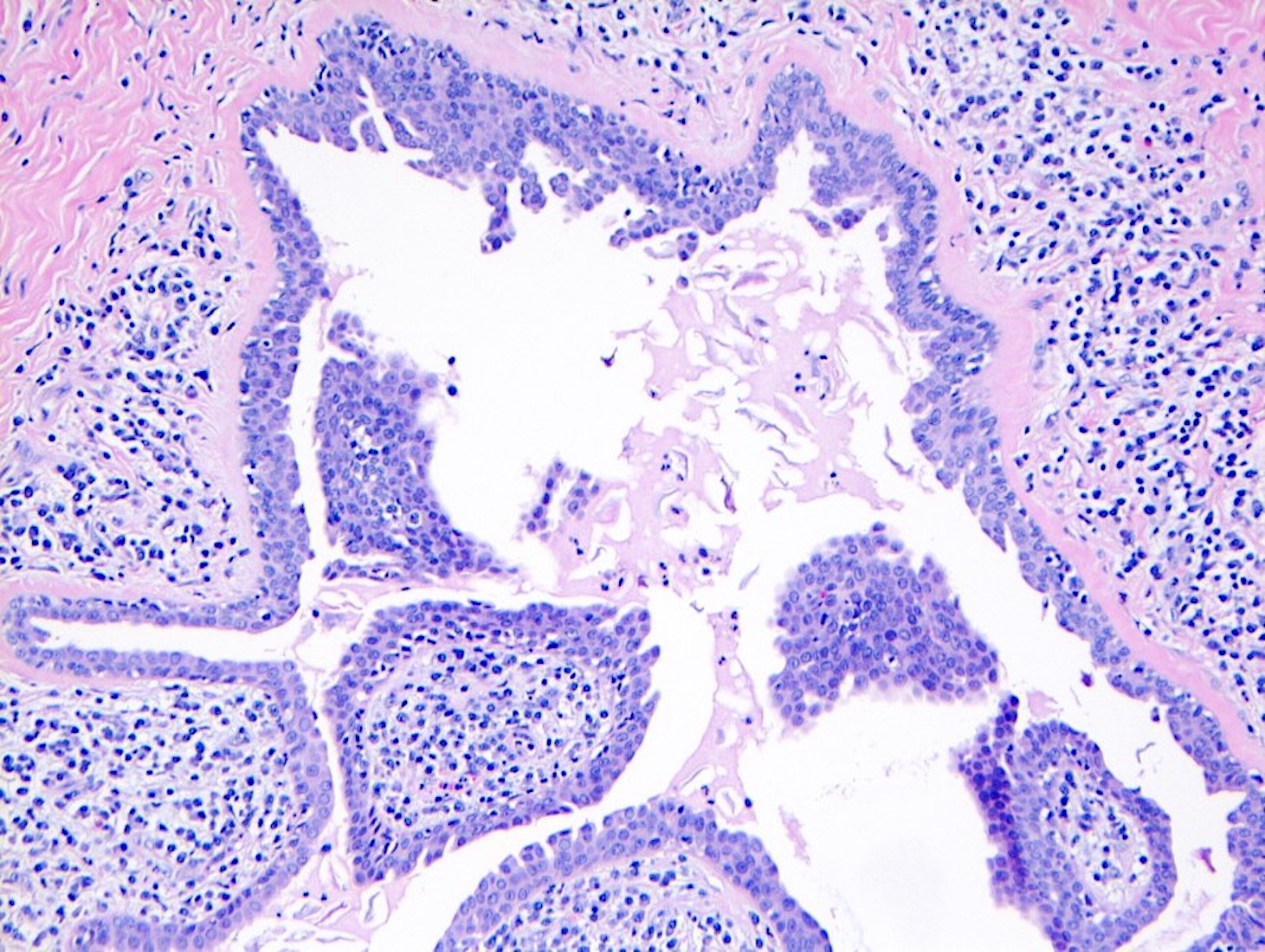
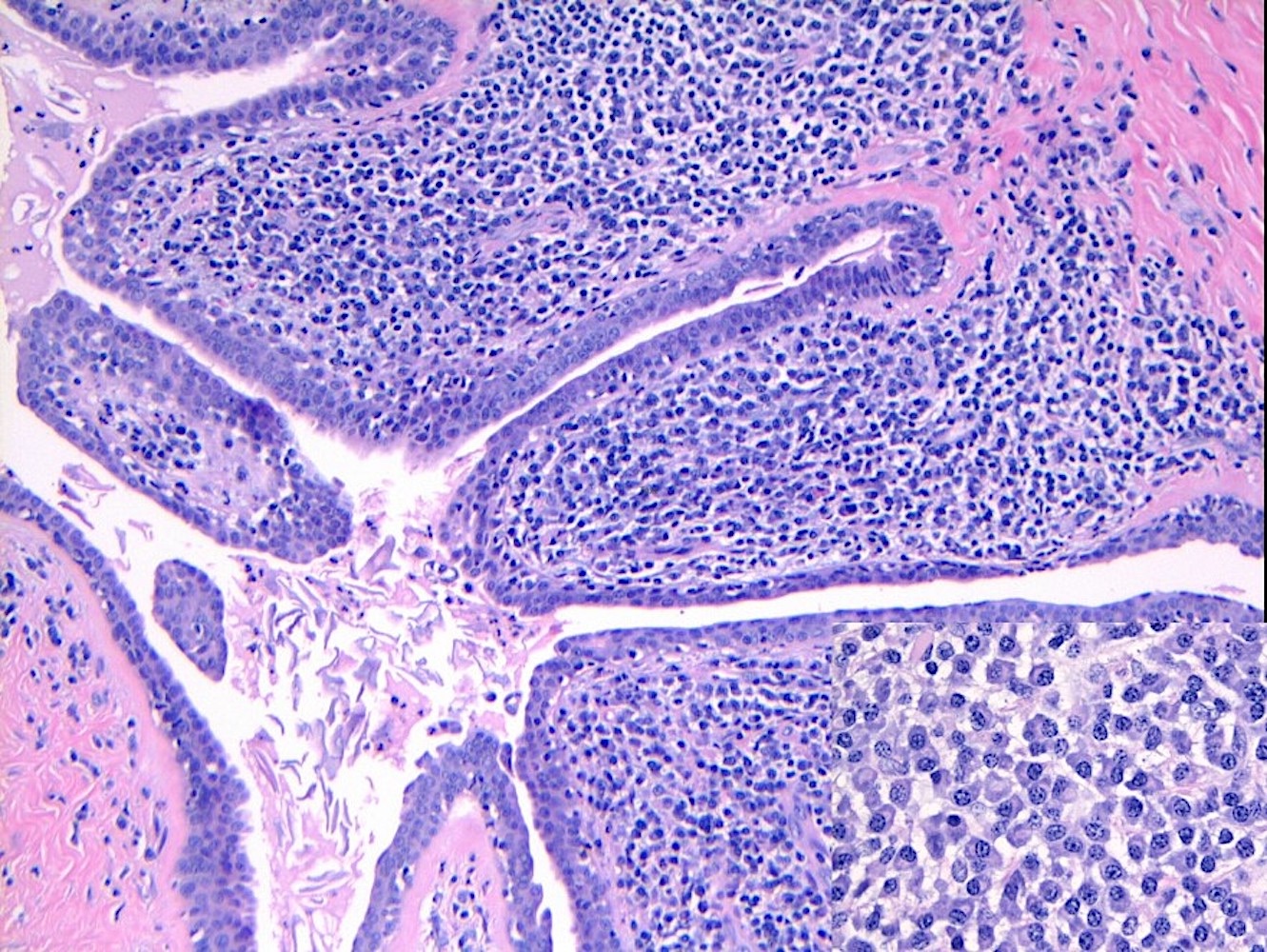
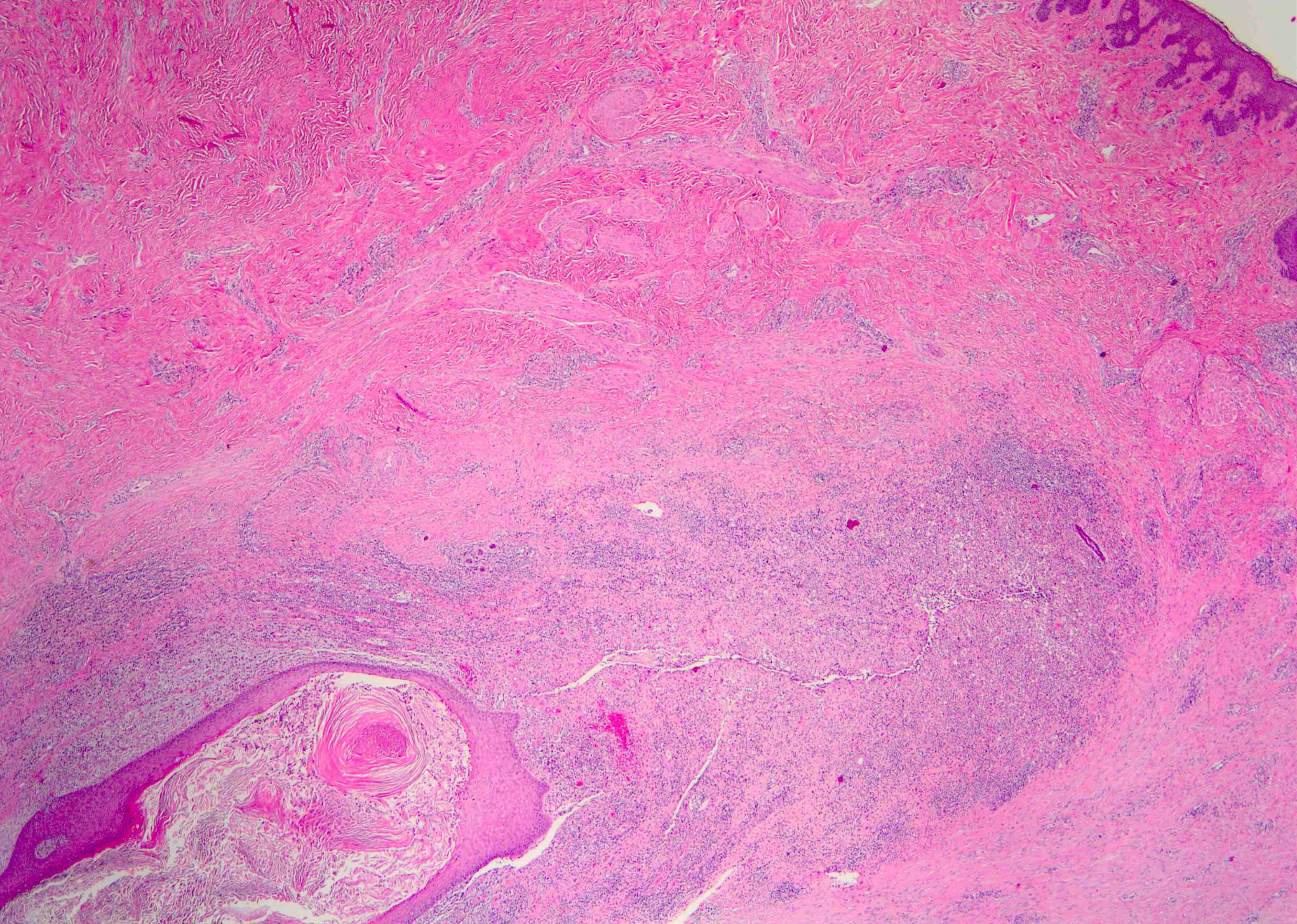
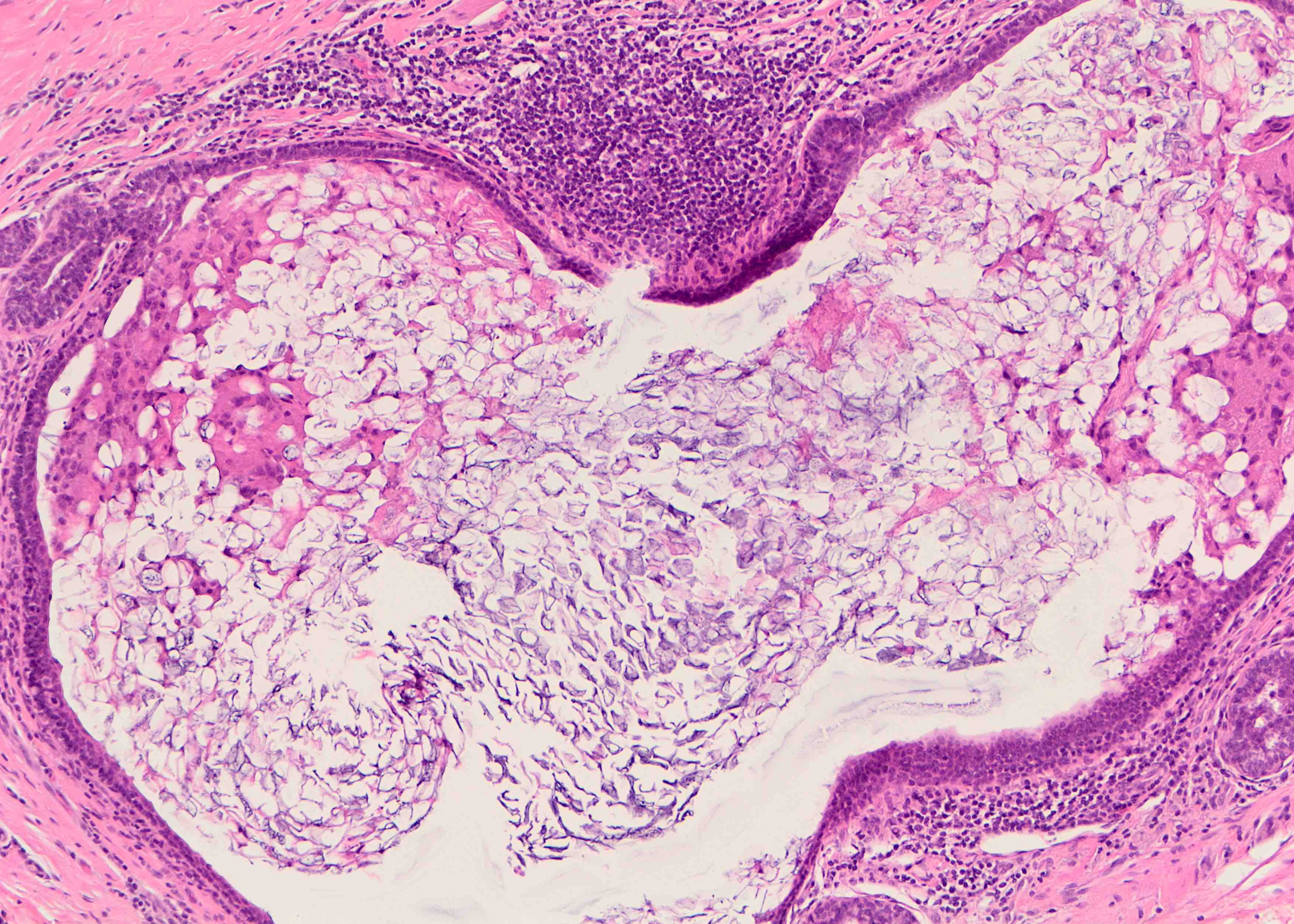
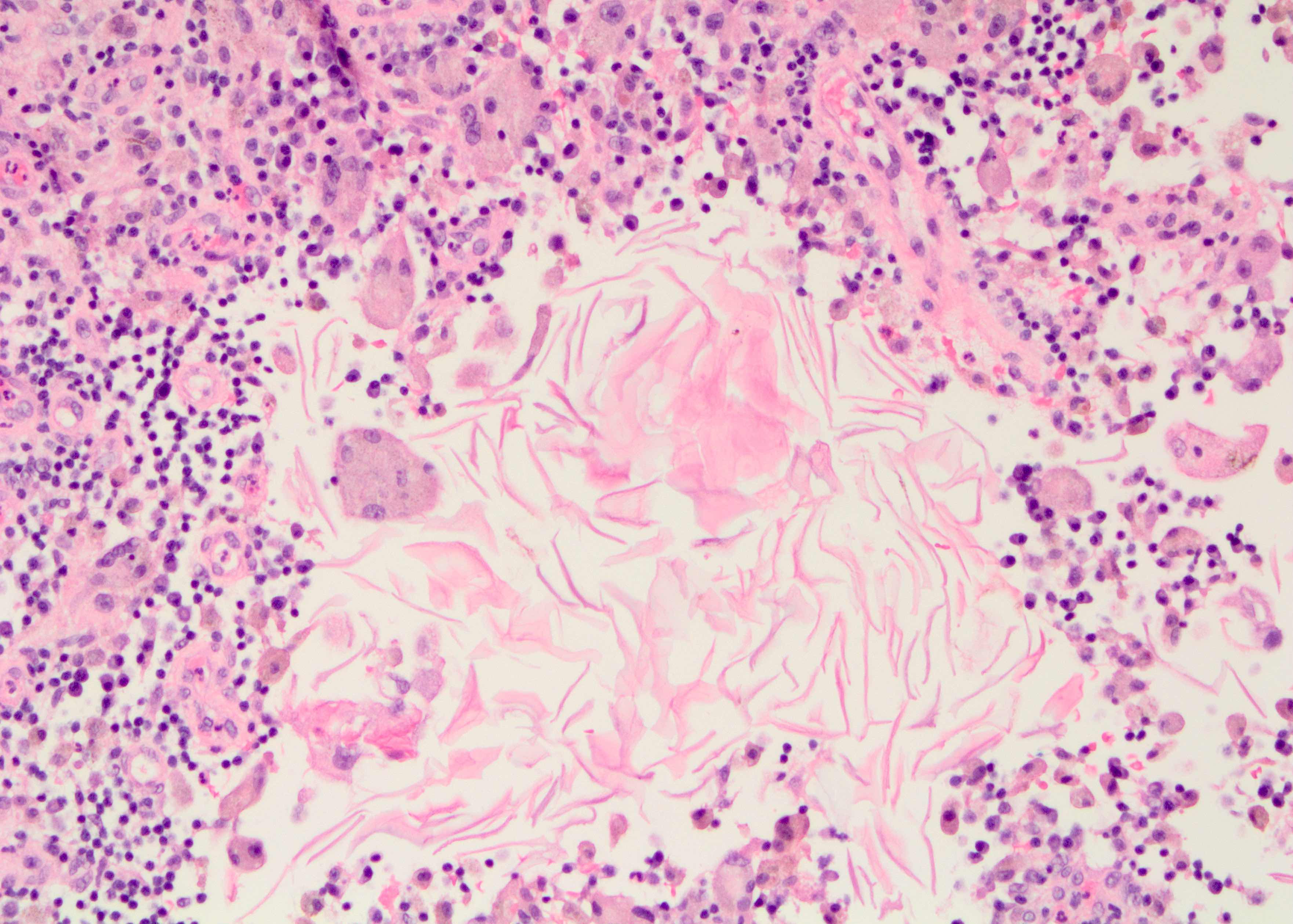
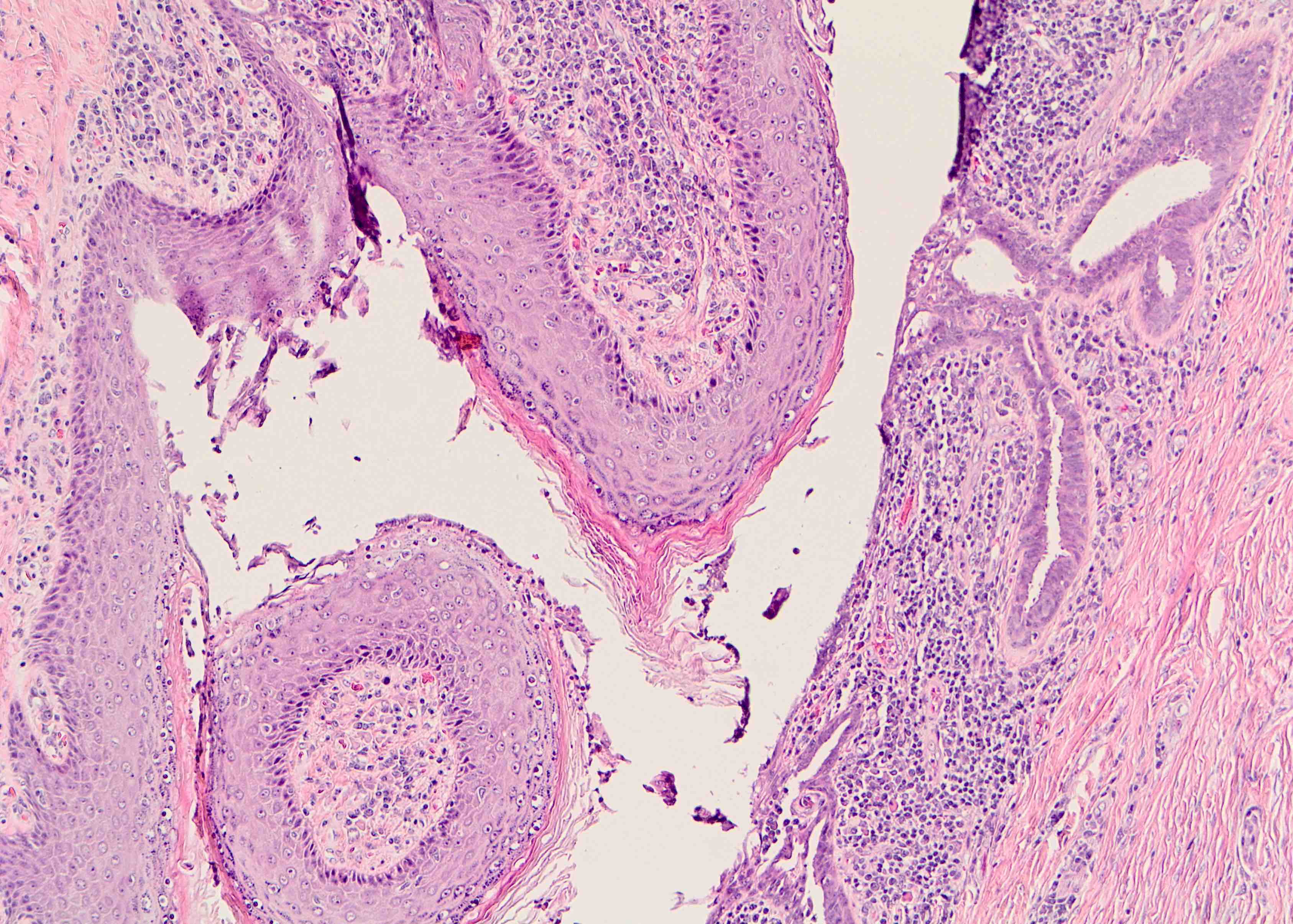
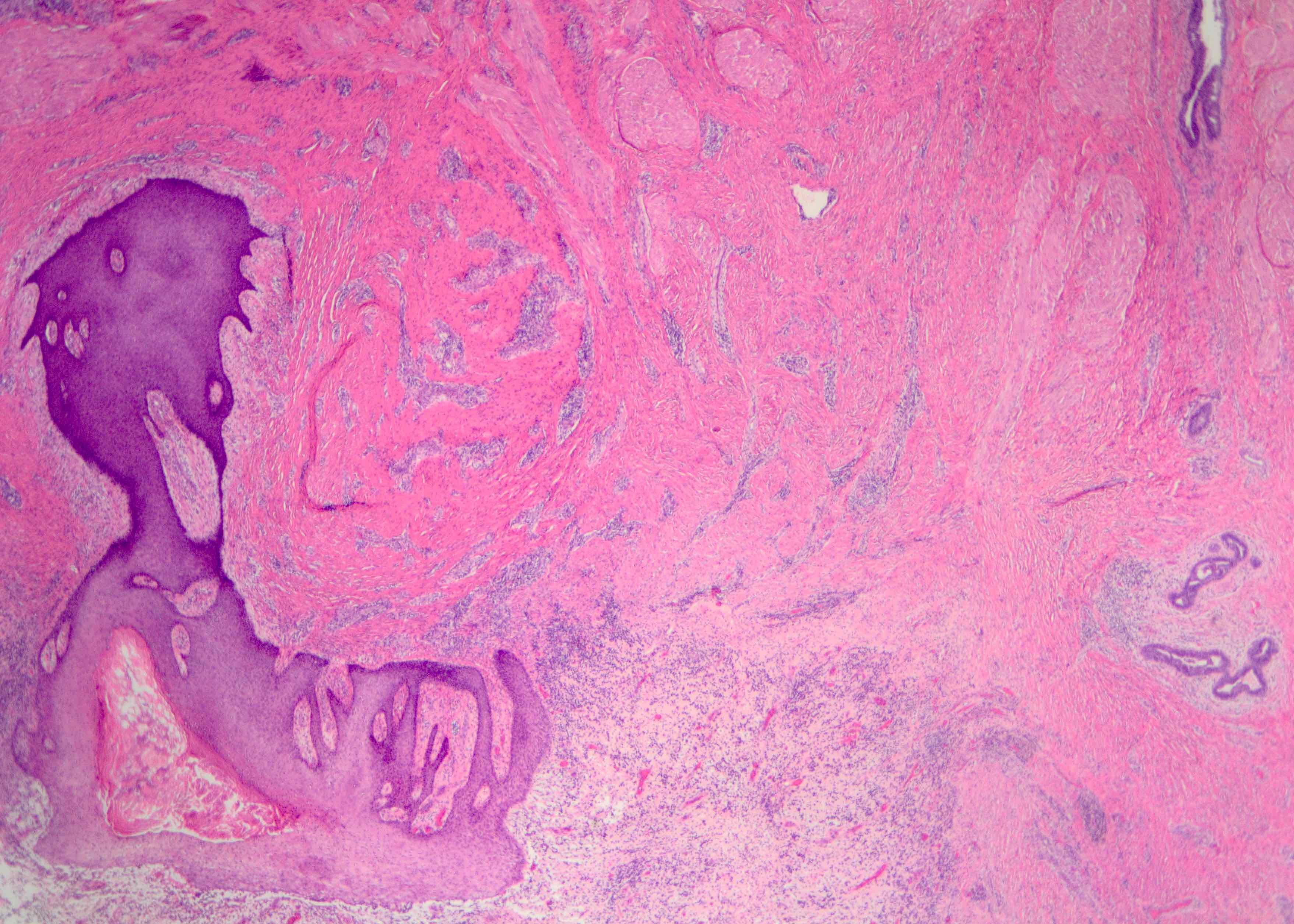
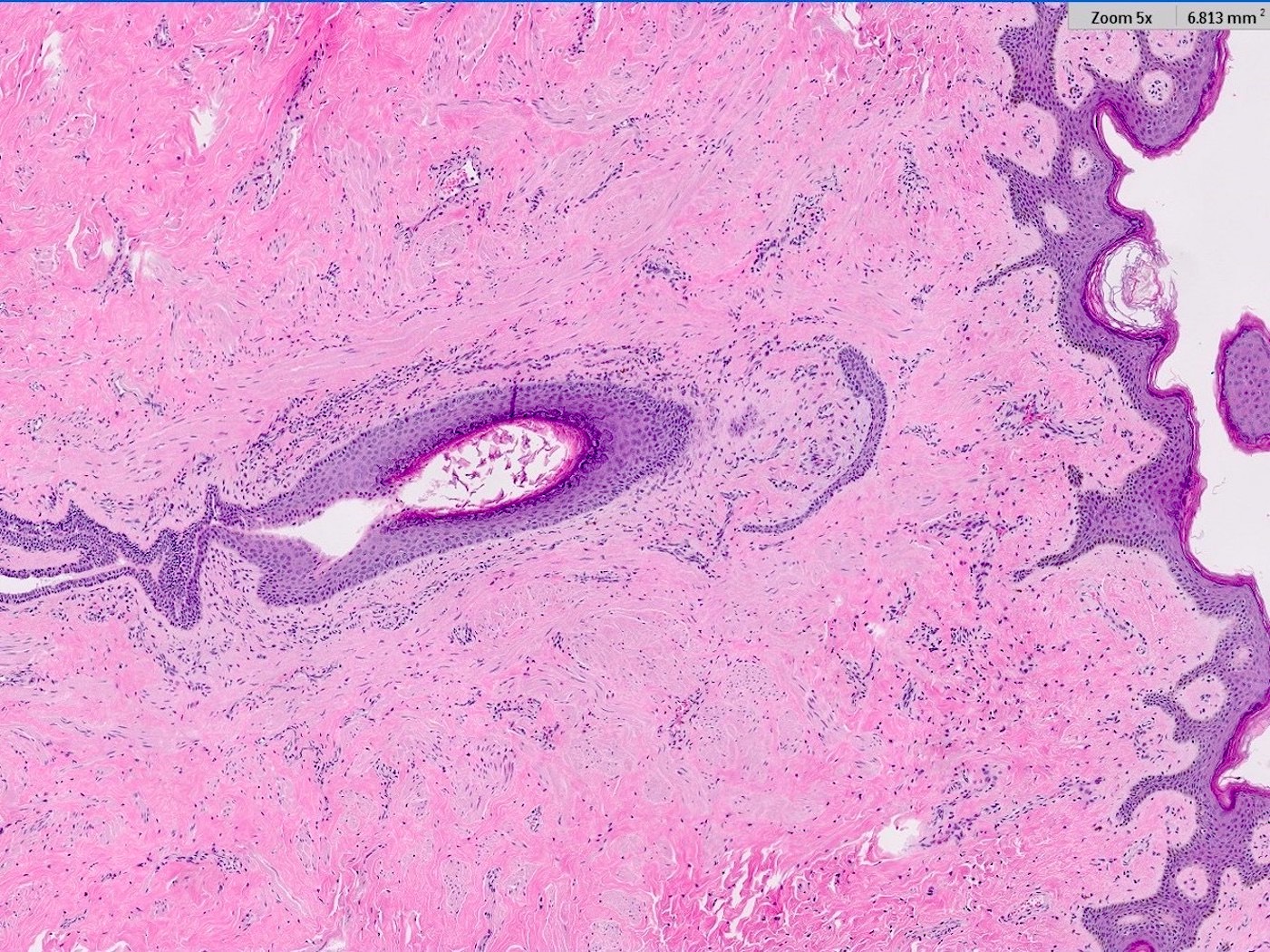
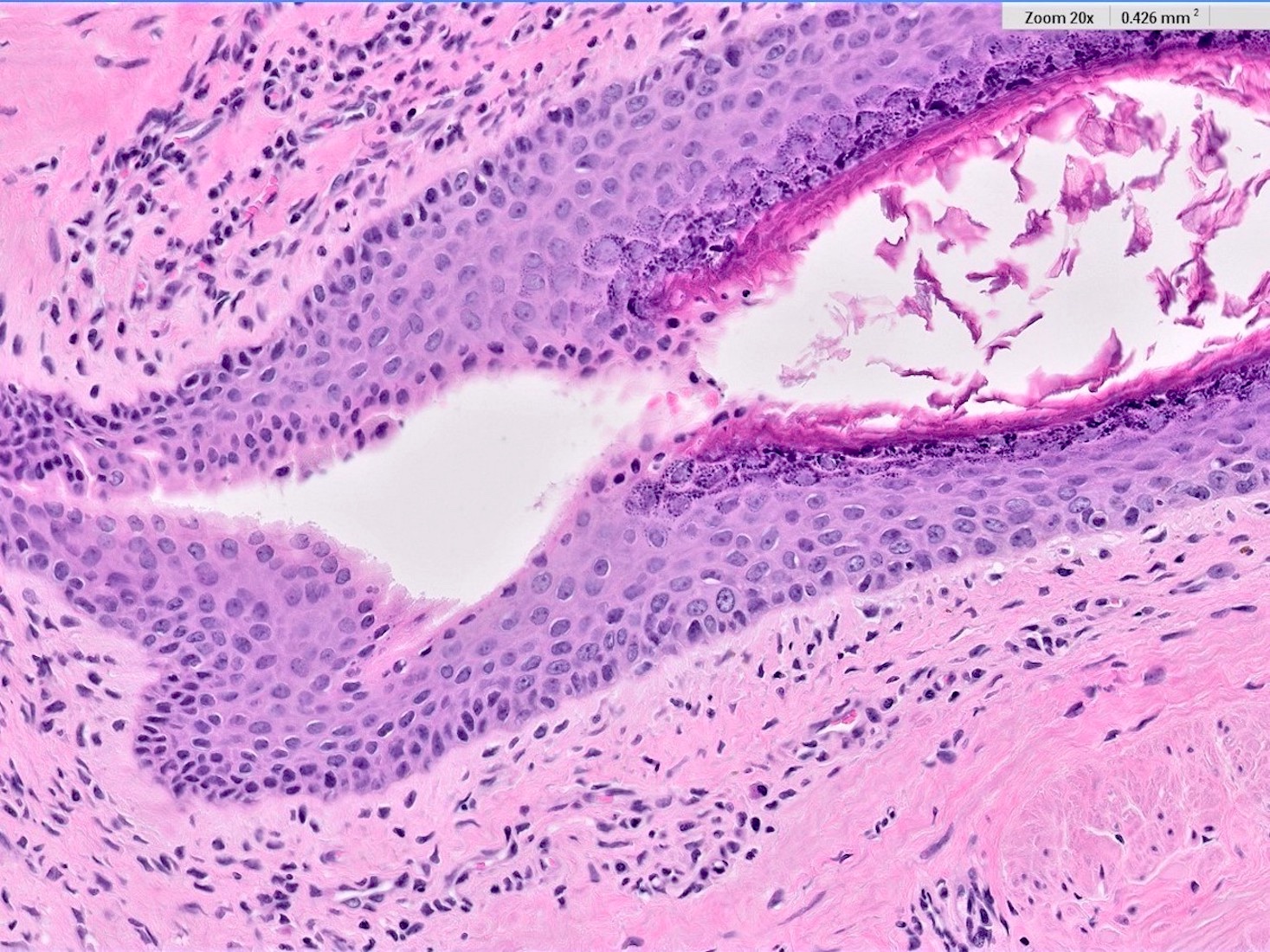
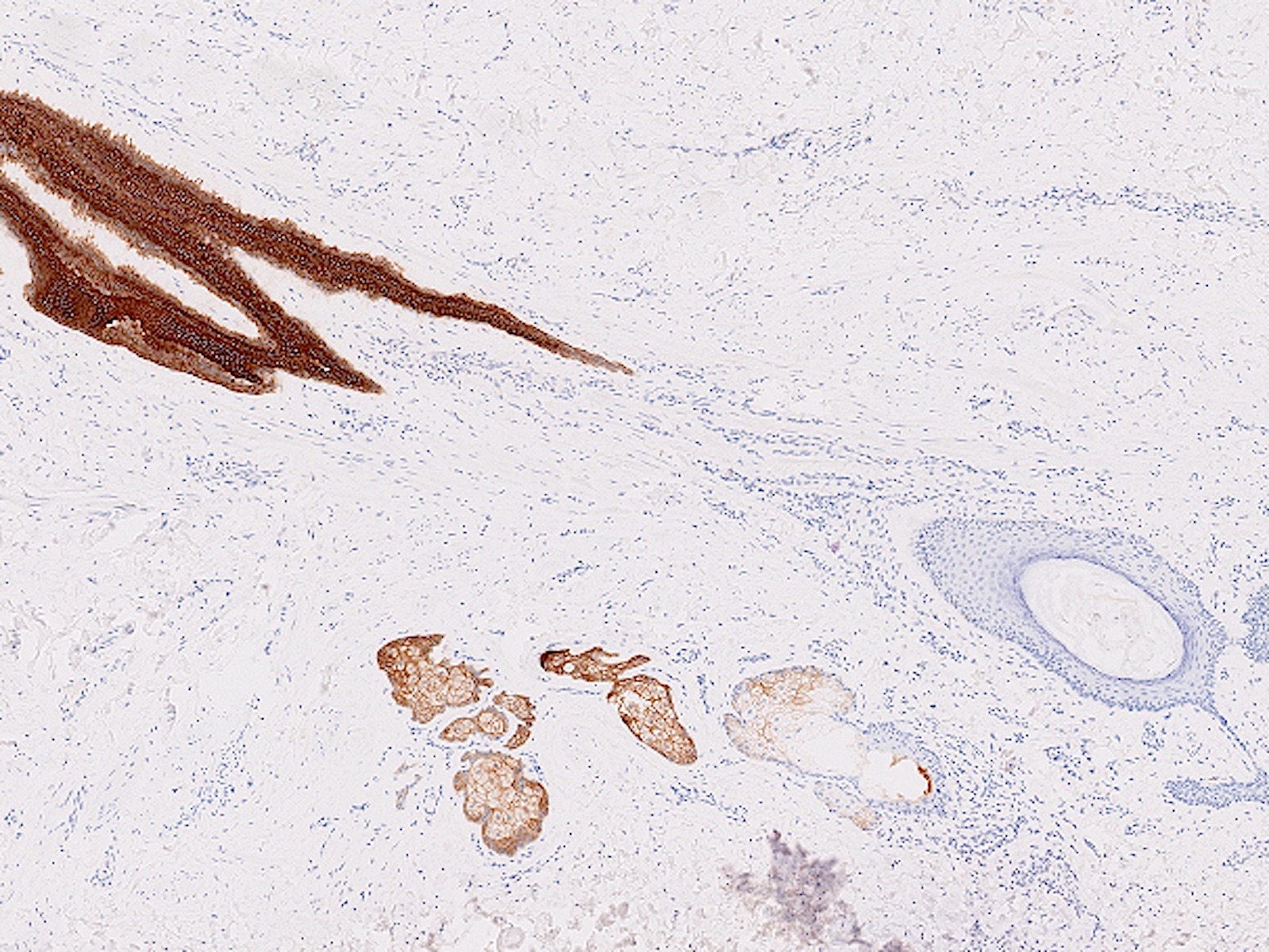
Microscopic (histologic) description
- Squamous metaplasia past the normal transition point to ductal epithelium, which is 1 - 2 mm beneath the skin surface
- Ducts filled or expanded by keratin debris
- Duct rupture with keratin debris inciting acute and chronic inflammatory reaction
- Keratin debris within giant cells is characteristic
- Reference: Schnitt: Biopsy Interpretation of the Breast, 3rd Edition, 2017
Microscopic (histologic) images
Contributed by Katie C. Hall, M.D., Anna Biernacka, M.D., Ph.D. and Mary Ann Gimenez Sanders, M.D., Ph.D.
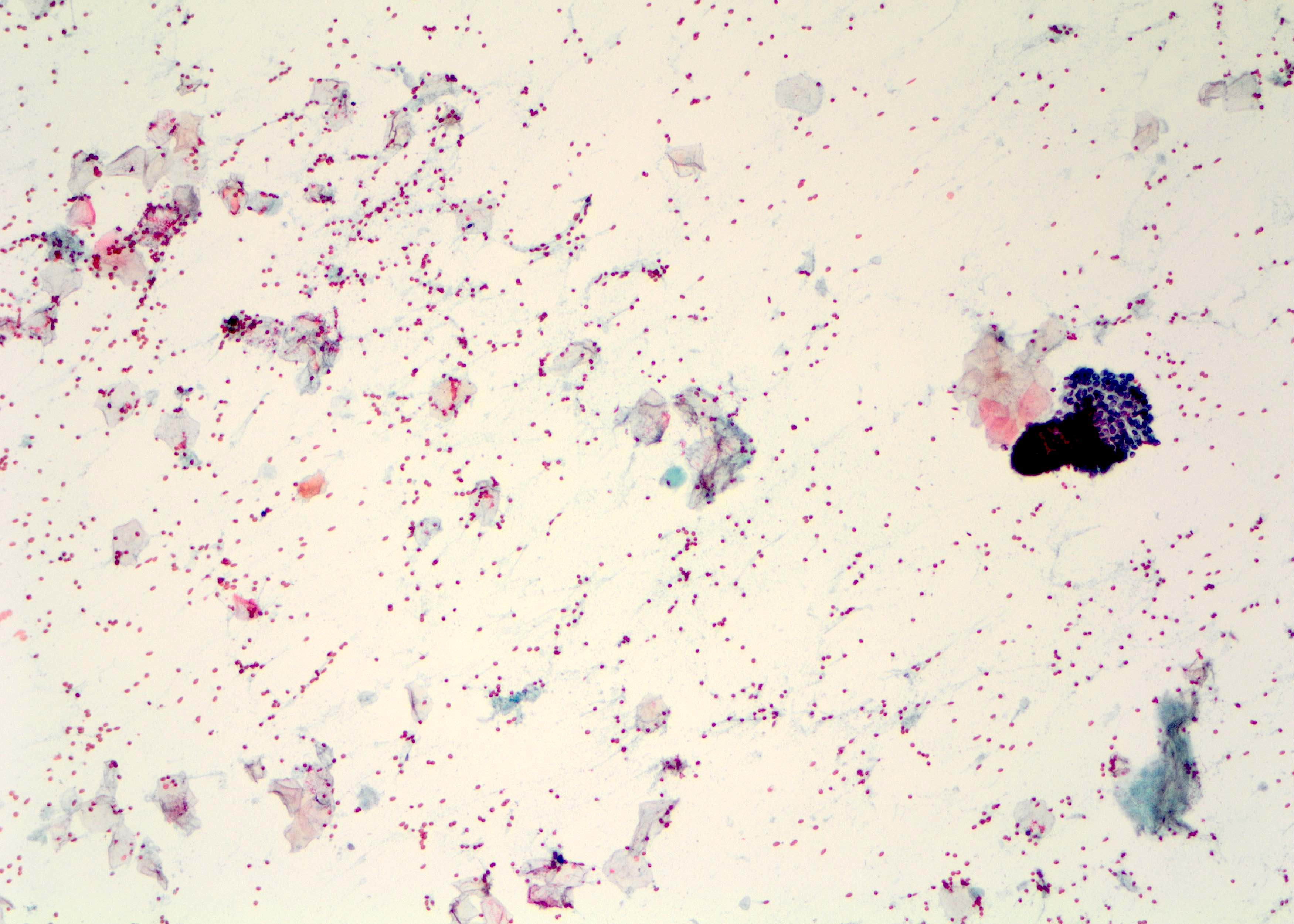
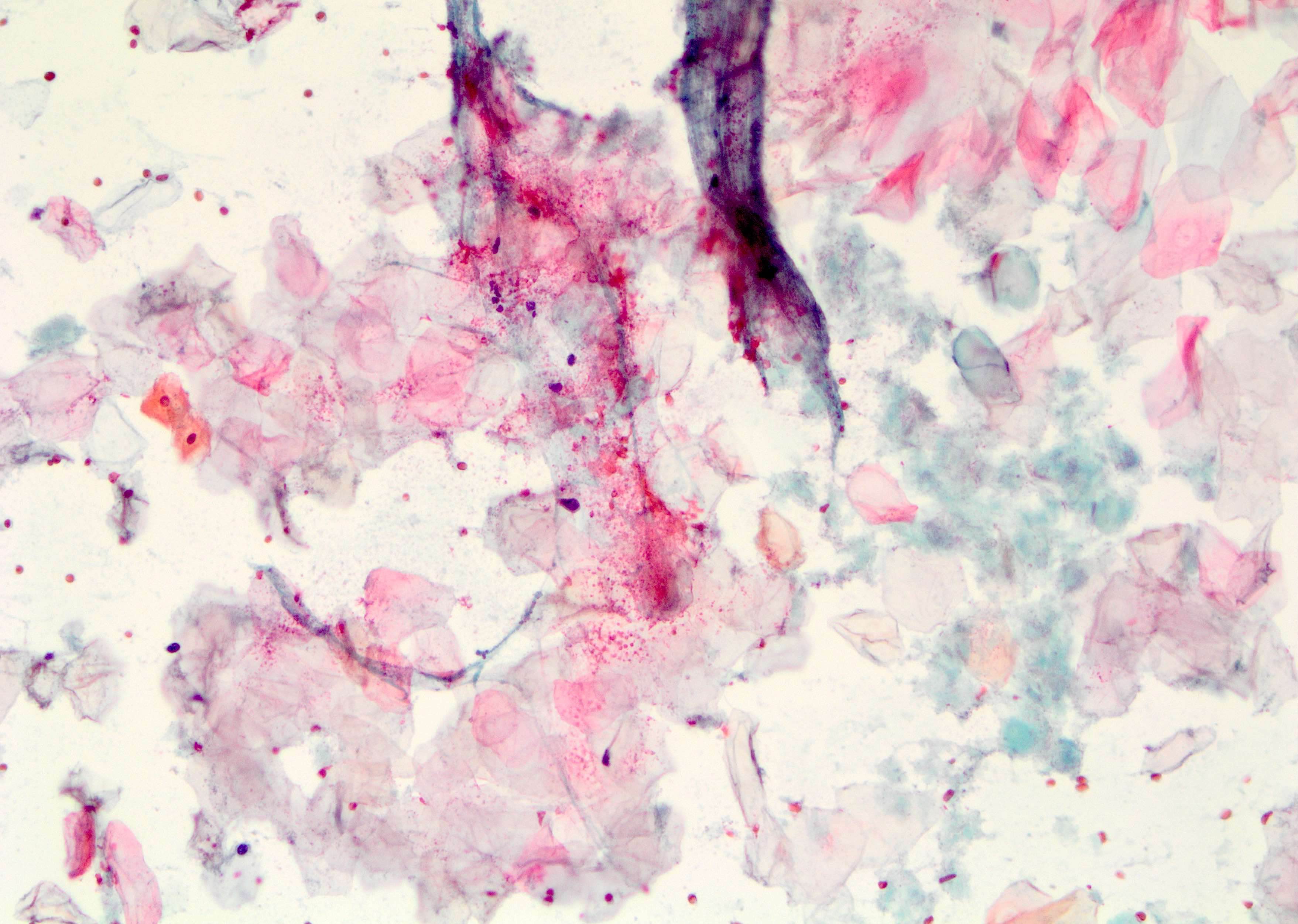
Cytology description
- Metaplastic squamous cells, anucleated squamous cells and mixed inflammation including macrophages and giant cells (Clin Radiol 2012;67:e42)
Sample pathology report
- Breast, left, retroareolar, ultrasound guided biopsy:
- Skin and breast parenchyma with chronic active inflammation including foreign body giant cells (see comment)
- Comment: There are rare keratin flakes associated with the inflammatory infiltrate. Given the patient's history of recurrent painful subareolar abscesses and chronic tobacco use, these findings could be compatible with squamous metaplasia of lactiferous ducts (SMOLD). Clinical correlation is recommended.
Differential diagnosis
- Mammary duct ectasia:
- Major and minor ducts affected with lymphocyte predominant inflammatory reaction
- Histiocytes within and surrounding duct wall in response to lipid or secretory material, not keratin
- Periductal fibrosis may be present
- Retroareolar abscess secondary to infection:
- Specific microorganism(s) identified via special stains or culture
- Squamous metaplasia or keratin debris not present in stroma
- Epidermal inclusion cyst:
- Present within superficial dermis and not continuous with lactiferous duct
- Cystic neutrophilic granulomatous mastitis or idiopathic granulomatous mastitis:
- Lobulocentric granulomatous inflammation
- Peripheral location
- Sinus tracts may open to skin surface without associated squamous metaplasia or central location
Practice question #1
A 39 year old woman presents with a retroareolar mass. She has a history of recurrent retroareolar abscesses previously treated with antibiotics and incision / drainage. An ultrasound guided biopsy of the mass shows similar findings to those in the photo. What is the definitive treatment?
- Central excision to include entire nipple
- Excision of affected duct
- Incision / draining and antibiotics
- Smoking cessation
Practice answer #1
B. Excision of affected duct. This is the correct answer and definitive treatment; squamous metaplasia of lactiferous ducts (SMOLD) is likely to recur without excision of the affected duct. Answer D is incorrect because while smoking cessation is suggested, it is not the definitive treatment.
Answer A is incorrect because excision is the definitive treatment; however, the entire nipple does not necessarily need to be included.
Answer C is incorrect because antibiotics and incision / drainage is the treatment for an abscess.
Comment Here
Reference: SMOLD
Comment Here
Reference: SMOLD
Practice question #2
What finding differentiates squamous metaplasia of lactiferous ducts (SMOLD) from other inflammatory breast conditions?
- Duct rupture with associated acute and chronic inflammation
- Lack of microorganisms on special stains and culture
- Lobulocentric granulomatous inflammation with neutrophils
- Squamous metaplasia with keratinaceous debris, possibly with foreign body giant cells
Practice answer #2
D. Squamous metaplasia with keratinaceous debris, possibly with foreign body giant cells. These findings in the appropriate clinical context and location are diagnostic for SMOLD.
Answer B is incorrect because this is not the only inflammatory breast disease that can lack microorganisms on special stains or culture.
Answer C is incorrect because a lobulocentric pattern of inflammation would not be expected in SMOLD. This is pattern of inflammation can be seen in cystic neutrophilic granulomatous mastitis and idiopathic granulomatous mastitis.
Answer A is incorrect because duct rupture can be seen in SMOLD as well as mammary duct ectasia.
Comment Here
Reference: SMOLD
Comment Here
Reference: SMOLD