Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Genetics | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Davis D, Weins A. Acute tubular necrosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneyatn.html. Accessed May 14th, 2024.
Definition / general
- Sudden decline in renal function, secondary to ischemic or toxic damage to renal tubular epithelial cells
- More accurate term is acute tubular injury (ATI), as necrosis is not commonly seen
Essential features
- Secondary sudden decline in renal function from ischemic (50%) or toxic (25%) causes
- Acute tubular injury (ATI) is more accepted term, as necrosis is rarely seen in ischemic injury
- Acute tubular necrosis (ATN) is a subset of ATI (Kidney Int Rep 2020;5:1993)
- Clinically similar to acute interstitial nephritis (AIN); histopathology needed for diagnosis (Nephron 2019;143:211)
Terminology
- Acute tubular injury (ATI)
- Acute tubular damage
- Lower nephron nephrosis (Am J Surg Pathol 2018;42:625)
ICD coding
Epidemiology
- Most common cause of intrinsic AKI (~85%)
- True ATN presents in 1% of hospitalized patients and ~4/10,000 of the general population
- More likely to affect patients with comorbidities (e.g., diabetes mellitus, heart failure, cancer, atherosclerosis, chronic kidney disease [CKD]), undergoing high risk surgery or presenting with shock (StatPearls: Acute Renal Tubular Necrosis [Accessed 13 June 2022])
Sites
- Kidney: tubular disease
- Ischemia: patchy involvement of nephron; S3 of the proximal tubule and more distal tubules, including thick ascending limb, are usually affected
- Toxic: usually more proximal nephron affected, especially convoluted segment of proximal tubules (Semin Nephrol 2018;38:21)
Pathophysiology
- Ischemia leads to vasoconstriction and decreased renal perfusion, causing damage and dysfunction of renal tubular endothelial cells that in turn leads to damage and dysfunction of renal tubular epithelial cells
- Nephrotoxins are a direct cause of renal tubular epithelial cell damage and dysfunction
- Renal tubular epithelial cell injury can be seen as a loss of brush borders and cell adhesion
- Apoptotic sloughed off tubular cells, other cellular detritus and eosinophilic and granular casts, comprised mainly of Tamm-Horsfall protein, obstruct the lumen leading to a decrease in glomerular filtration rate (GFR) and oliguria
- Loss of adhesion can cause backleak of glomerular filtrate into the interstitium, also leading to a decrease in GFR and oliguria (StatPearls: Acute Renal Tubular Necrosis [Accessed 13 June 2022])
Etiology
- Most cases are secondary to ischemia (50%), toxins (25%), sepsis (cytokine mediated injury) or obstruction
- Ischemia secondary to hypovolemia (blood loss, fluid loss or third spacing) or decreased perfusion pressure (systemic or local)
- Nephrotoxins include:
- Drugs
- Antibiotics (aminoglycosides, amphotericin, vancomycin)
- Antivirals (acyclovir, indinavir, tenofovir)
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Chemotherapy drugs (cisplatin, ifosfamide)
- Checkpoint inhibitors
- Calcineurin inhibitors (cyclosporine, tacrolimus)
- mTOR inhibitors
- Herbs
- IV contrast agents
- Anesthetics
- Heavy metals
- Lead
- Bismuth
- Mercury
- Uranium
- Platinum
- Organic toxins
- Ethylene glycol
- Carbon tetrachloride
- Fuel
- Printer ink
- Toluene
- Endogenous toxins
- Bile casts
- Hemoglobin
- Myoglobin
- Light chains
- Calcium oxalate
- Uric acid
- Drugs
- References: StatPearls: Acute Renal Tubular Necrosis [Accessed 13 June 2022], J Am Soc Nephrol 2020;31:1948
Diagrams / tables
Clinical features
- Events leading to renal hypoperfusion or use of nephrotoxic substances
- Physical exam: signs of volume depletion and hypotension (tachycardia, dry mucous membranes, decreased skin turgor, lethargy, nausea or vomiting), fever if septic, oliguria or anuria initially and possibly polyuria in recovering patients
- Underlying etiology is important for treatment
- References: Contrib Nephrol 2021;199:131, Ren Fail 2019;41:576, Nephron 2019;143:170
Diagnosis
- Clinically ATN and AIN are similar
- Acute tubular injury with or without tubular necrosis
- Biopsy needed for definitive diagnosis (Nephron 2019;143:211)
Laboratory
- Decreased GFR, elevated creatinine and blood urea nitrogen (BUN)
- Urinalysis: muddy brown casts, renal tubular epithelial cells
- Fractional excretion of sodium (FENa): usually > 2% while prerenal disease has a value < 1%, though not always the case
- Urine Na: usually > 40 - 50 mEq/L
- Azotemia
- Hyperkalemia
- Metabolic acidosis
- Possibly myoglobinuria or hemoglobinuria (StatPearls: Acute Renal Tubular Necrosis [Accessed 13 June 2022], Nat Rev Nephrol 2019;15:599, Curr Opin Nephrol Hypertens 2019;28:560)
Prognostic factors
- Favorable unless sustained renal failure or combined with systemic issues or other underlying conditions
- Morbidity is associated with complications secondary to renal failure rather than intrinsic damage from ATI / ATN
- Possible association between biopsy proven ATN and progression to end stage renal disease (ESRD) (J Korean Med Sci 2020;35:e206)
Case reports
- 31 year old man with rhabdomyolysis and ATN (JBJS Case Connect 2019;9:e0318)
- 33 year old pregnant woman following SARS-CoV-2 infection (Respir Med Case Rep 2020;30:101090)
- 47 year old man with nausea, vomiting and reduced urine output secondary to povidone iodine ingestion (Medicine (Baltimore) 2017;96:e8879)
- 54 year old woman with hypokalemia and ATN secondary to acylovir use (BMC Nephrol 2018;19:324)
- 59 year old man with high serum levels of vancomycin and tobramycin and ATN (Am J Surg Pathol 2018;42:625)
Treatment
- Underlying cause will determine route of treatment
- Stop toxic insult or medication
- Prevent hypovolemia or hypotension if possible
- Replete volume status
- Avoid angiotensin converting enzyme inhibitors (ACEs), angiotensin receptor blockers (ARBs), NSAIDs, aminoglycosides, IV contrast media and other known renally toxic drugs
- References: Ren Fail 2019;41:576, Nephron 2019;143:170, Am Fam Physician 2019;100:687
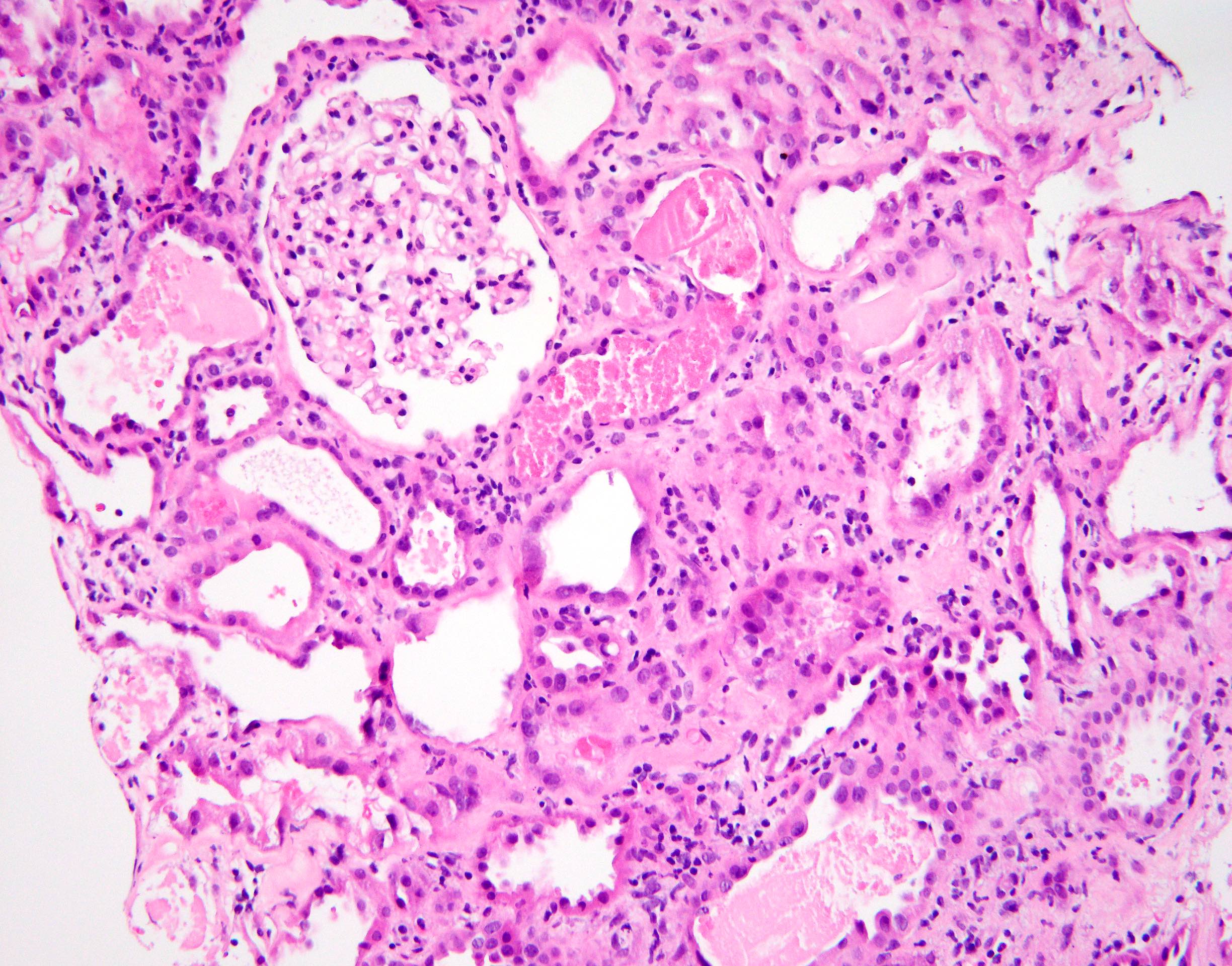
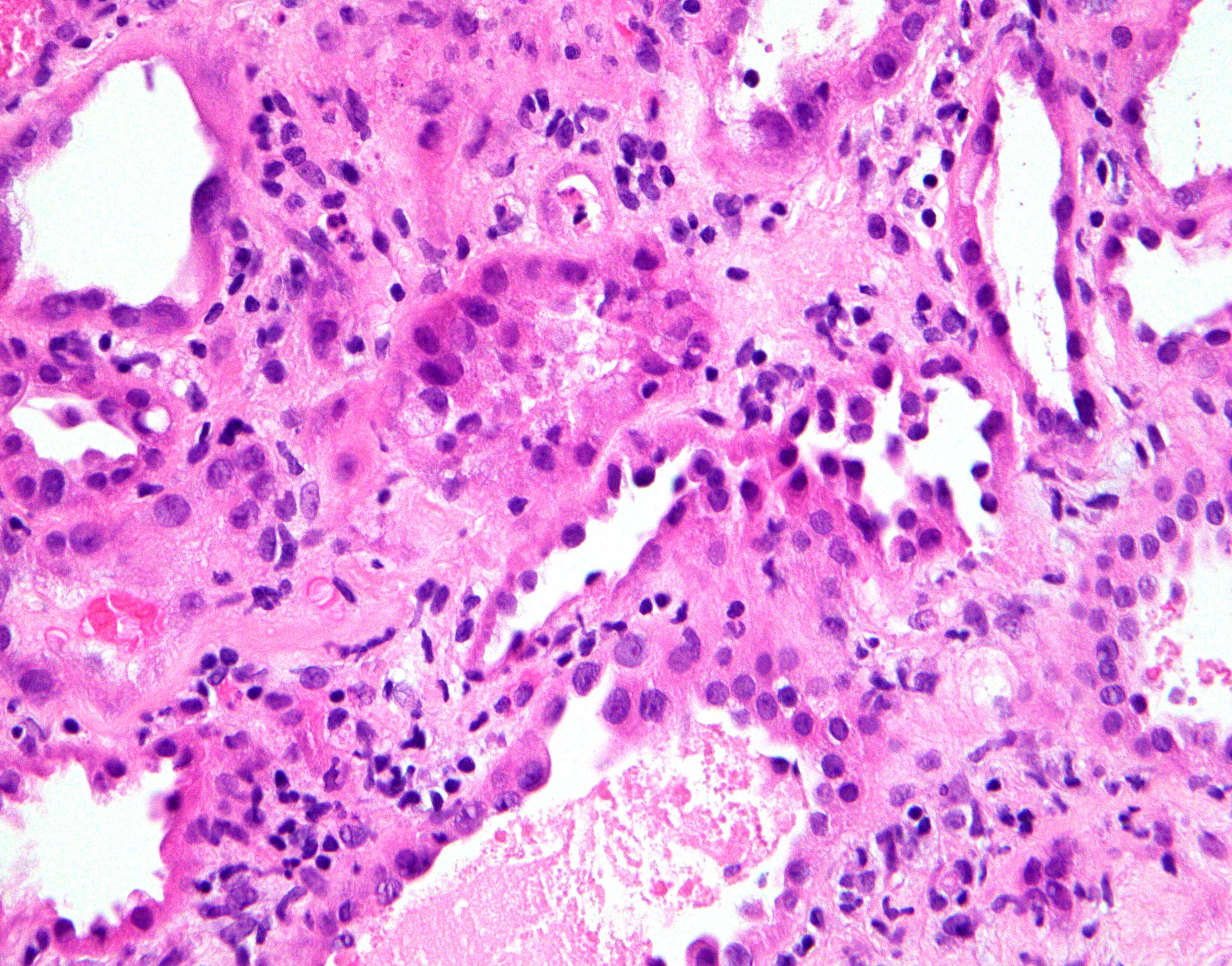
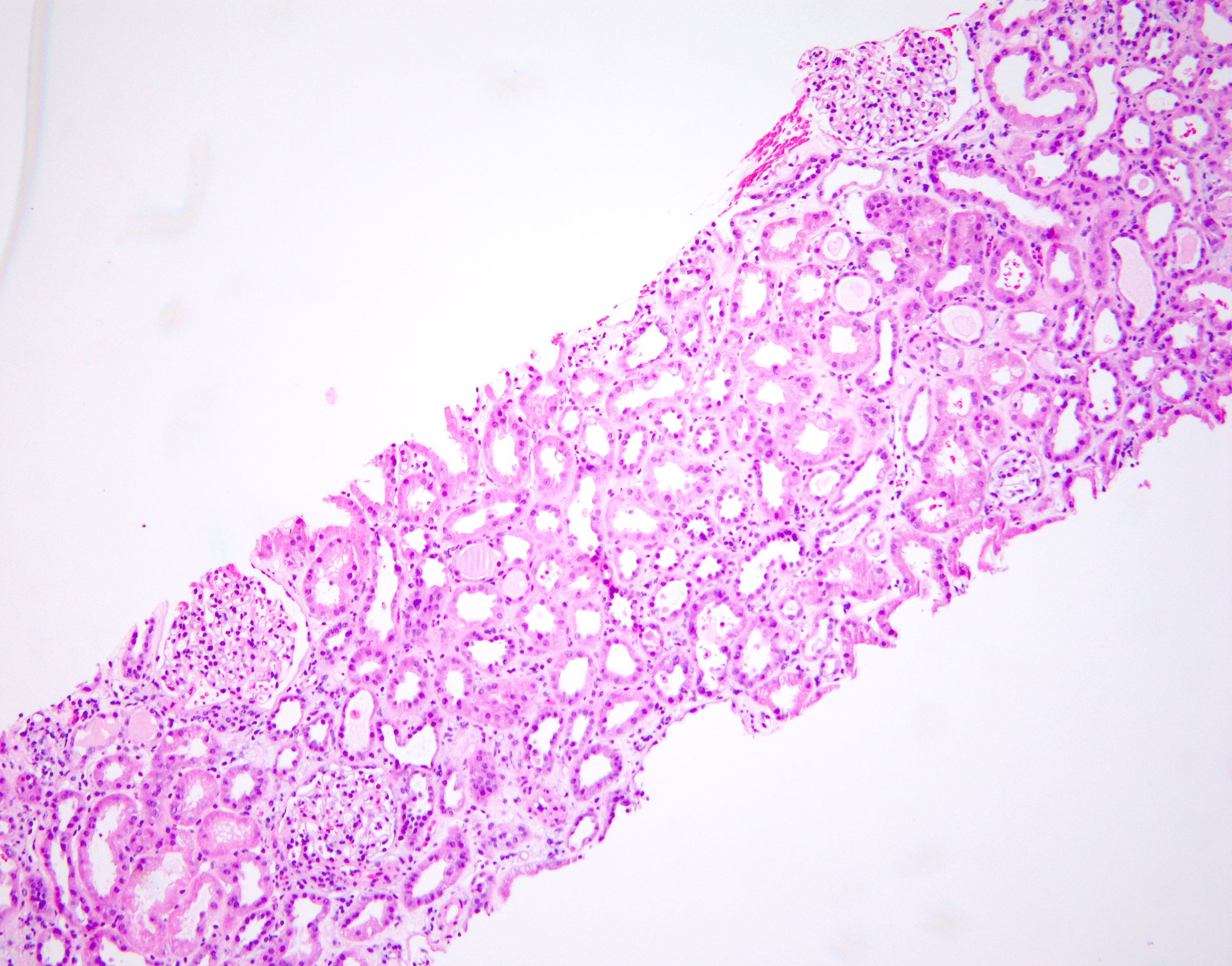
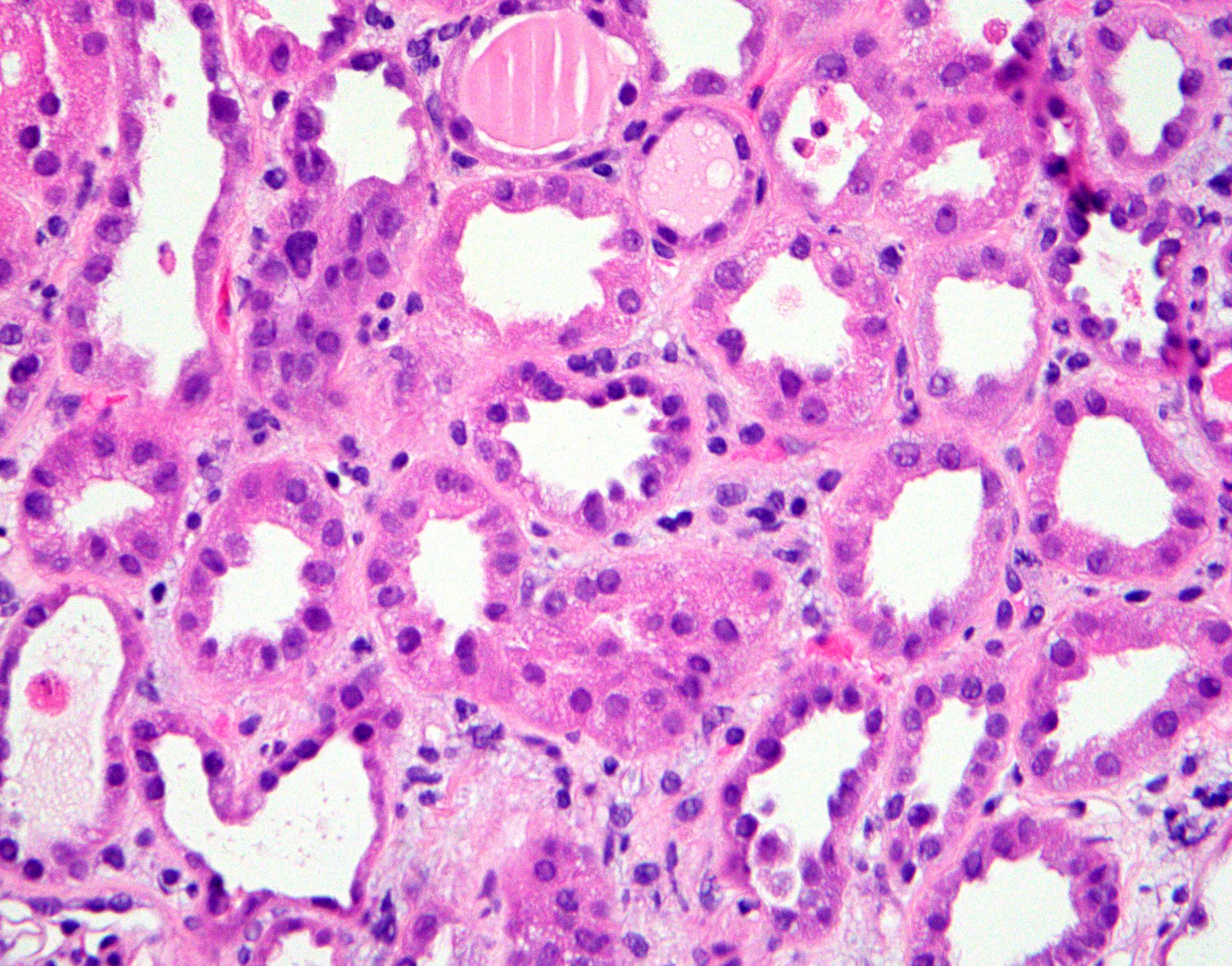
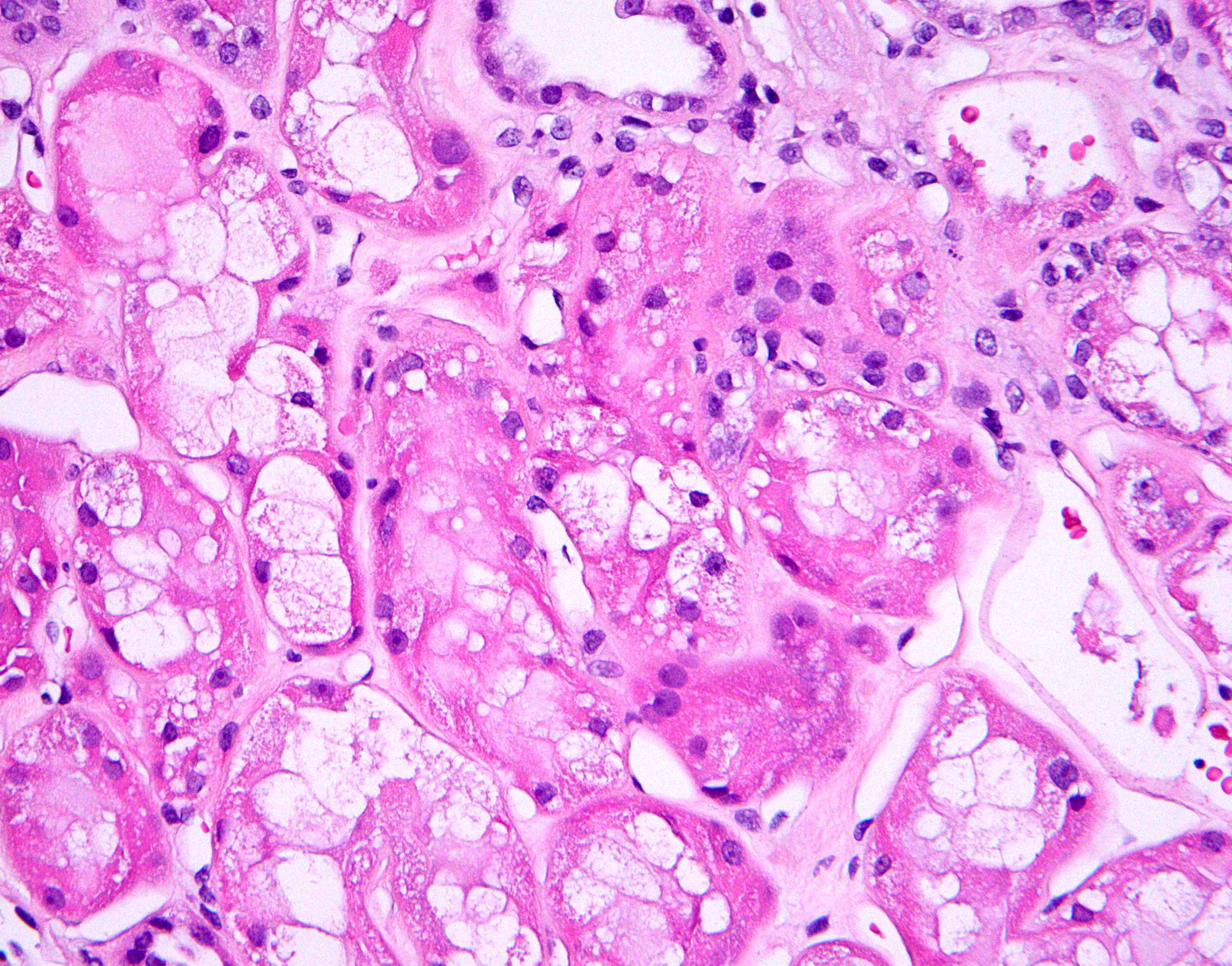
Microscopic (histologic) description
- Attenuation or simplification of tubular epithelium with loss of brush border and blebbing of apical cytoplasm with increased eosinophilic staining
- Tubular epithelial nuclei with condensed chromatin, increased in basophilic staining or loss of distinct nuclear contour
- Tubular lumens filled with sloughed off necrotic tubular epithelial cells, fibrin debris or hyaline casts
- Note: toxic damage more associated with necrosis than ischemic damage (Kidney Int Rep 2020;5:1993, Am J Surg Pathol 2018;42:625)
Microscopic (histologic) images
Positive stains
Negative stains
- Ki67 (low)
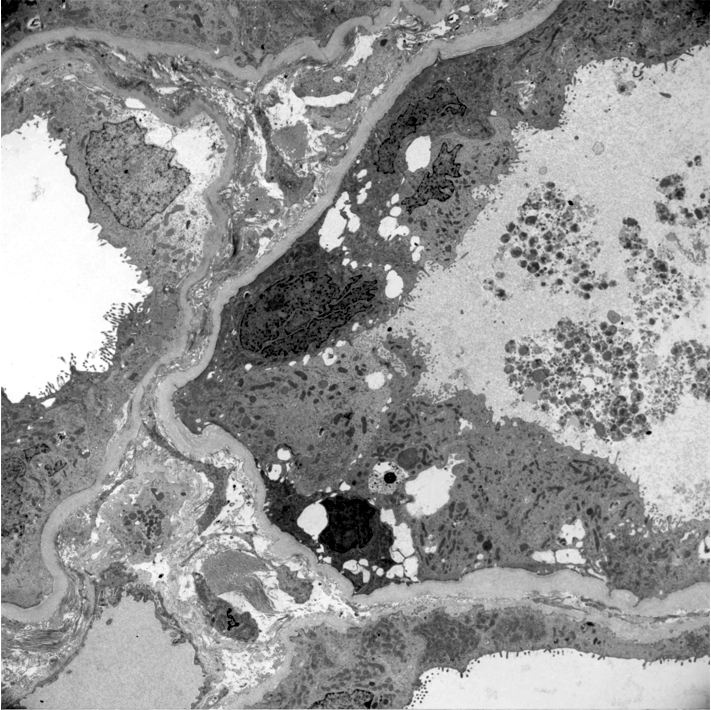
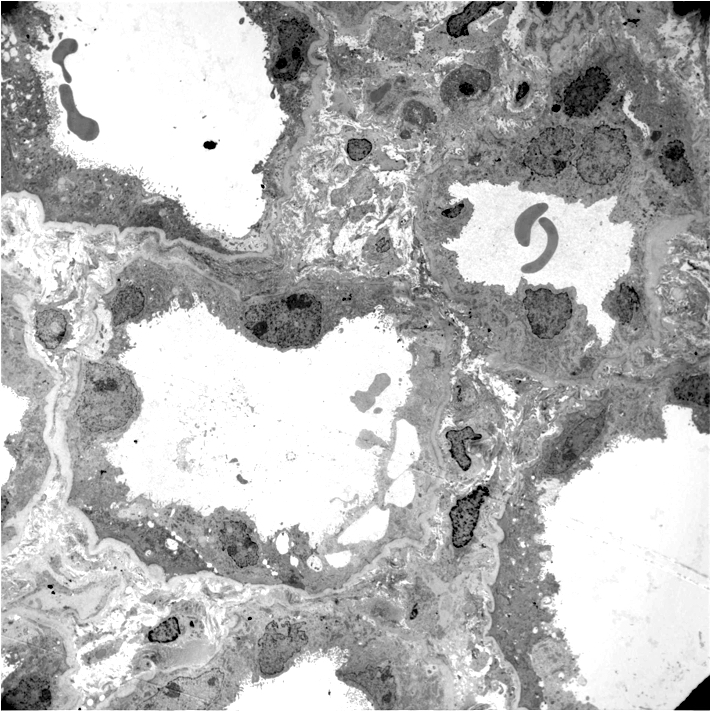
Electron microscopy description
- Proximal tubules show loss of brush border, apical blebs and shedding, cell swelling with mitochondrial condensation, nuclear fragmentation and cell detachment
- Lumen with cellular debris
- Peritubular capillaries with vacuolar degeneration of endothelial cells as well as thickened or multilayered basement membrane
- In ischemic injury, more likely to see autophagy and increased phagolysosomes
- In toxic injury, more likely to see cell contraction and necrosis, dilation of endoplasmic reticulum and mitochondrial swelling with inclusions (Semin Nephrol 2018;38:21)
Electron microscopy images
Genetics
- IL18 gene, particularly at rs1946518 and rs187238 polymorphisms, may lead to aberrant levels of IL18, which has been linked to pathogenesis of ATN and AKI (J Clin Med 2021;10:3039)
Videos
Overview of intrarenal acute kidney injury
Sample pathology report
- Left kidney, needle core biopsy:
- Acute tubular injury with acute tubular necrosis, widespread and severe, most likely ischemic (see comment)
- There is no evidence of an immune complex mediated disease, a paraprotein deposition disease or a diffuse podocyte disease; there are no signs of active glomerulitis or acute interstitial nephritis
- Minimal chronic changes of the parenchyma, including:
- Focal global glomerulosclerosis (2% of glomeruli)
- Minimal tubular atrophy and interstitial fibrosis (< 5% of the cortex)
- Moderate arterial sclerosis
- Comment: The biopsy reveals widespread tubular injury with severe acute tubular necrosis superimposed on advanced chronic changes of the parenchyma as summarized in the diagnosis above. The process is most likely ischemic.
Differential diagnosis
- Tubulointerstitial nephritis:
- Will show interstitial inflammation and tubulitis
- Cortical necrosis:
- Glomeruli and vessels also affected
- Autolysis:
Additional references
Board review style question #1
Board review style answer #1
Board review style question #2
Typical laboratory findings of acute tubular injury are
- Decreased GFR, increased Cr, FENa < 1%, urine Na > 40 mEq/L
- Decreased GFR, increased Cr, FENa > 2%, urine Na > 40 mEq/L
- Decreased GFR, increased Cr, FENa > 2%, urine Na < 40 mEq/L
- Increased GFR, decreased Cr, FENa < 1%, urine Na < 40 mEq/L
Board review style answer #2
B. Decreased GFR, increased Cr, FENa > 2%, urine Na > 40 mEq/L
Comment Here
Reference: Acute tubular necrosis
Comment Here
Reference: Acute tubular necrosis