Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Gonzalez R. Primary biliary cholangitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/liverPBC.html. Accessed May 10th, 2024.
Definition / general
- Primary biliary cholangitis (PBC) is a chronic, progressive cholestatic liver disease with granulomatous destruction of interlobular bile ducts, leading to fibrosis and ultimately cirrhosis
Essential features
- Typically occurs in middle aged women; extremely rare in children
- Labs include elevated alkaline phosphatase, elevated IgM and the classic antimitochondrial antibody (AMA)
- Histologic changes, including the pathognomonic florid duct lesions, can be patchy
Terminology
- Previously called primary biliary cirrhosis; renamed because not all patients progress to cirrhosis (Clin Res Hepatol Gastroenterol 2015;39:e57)
ICD coding
- ICD-10: K74.3 - primary biliary cirrhosis
Epidemiology
- Reported prevalence of 65.4 women per 100,000 in U.S.; incidence appears to be increasing (Clin Liver Dis 2003;7:795)
Sites
- Involves the most proximal portion of biliary tree, namely the interlobular bile ducts and canals of Hering; larger bile ducts are not typically affected (Hum Pathol 2002;33:983)
Etiology
- Likely autoimmune; associated with Sjögren syndrome, scleroderma, thyroiditis, rheumatoid arthritis, Raynaud phenomenon, membranous glomerulonephritis, systemic lupus erythematosus, celiac disease
Clinical features
- 85% are women, usually ages 40 - 60
- Symptoms include insidious onset of pruritis, malaise, dark urine, light stools, hepatomegaly, xanthomas, and xanthelasma
- Can develop cirrhosis and die from liver failure
- Some patients have overlap disease with autoimmune hepatitis; much more rarely, patients may have overlap with primary sclerosing cholangitis (PSC); in overlap, strict criteria for both diseases must be met (ACG Case Rep J 2018;5:e54)
- Increased risk of hepatocellular carcinoma once cirrhotic but there does not appear to be significant increased risk of cholangiocarcinoma (unlike in primary sclerosing cholangitis)
Diagnosis
- 2 out of 3 of the following criteria are required:
- Serum alkaline phosphatase > 1.5 times the upper limit of normal, antimitochondrial antibody, liver sample showing nonsuppurative destructive cholangitis and destruction of interlobular bile ducts (Autoimmun Rev 2014;13:441)
- Other characteristic clinical features include disease-specific antinuclear antibodies (sp100 and gp210), elevated serum IgM, hypercholesterolemia, xanthomas, Sicca syndrome, pruritus, and fatigue (Autoimmun Rev 2014;13:441)
- Patients who appear to have primary biliary cholangitis except for negative antimitochondrial antibody are said to have AMA-negative primary biliary cholangitis, also called autoimmune cholangitis
Laboratory
- Elevated serum alkaline phosphatase and IgM, AMA in 95%, elevated conjugated bilirubin (late)
- M2 form of AMA, present in 90%, is against E2 subunit of pyruvate dehydrogenase complex
Radiology description
- Parenchymal lace-like fibrosis and periportal halo sign on T2-weighted MRI in some patients (Eur J Radiol 2009;69:523)
Case reports
- 32 year old woman with hypokalemia (Medicine (Baltimore) 2018;97:e13172)
- 51 year old woman treated with sulfasalazine and abatacept (BMJ Case Rep 2018)
- 56 year old woman with rheumatoid arthritis (Cureus 2017;9:e1562)
- 62 year old man with dermatitis herpetiformis (Cureus 2017;9:e1247)
- 74 year old woman with multiple hepatic malignancies (World J Hepatol 2017;9:1378)
Treatment
- Ursodeoxycholic acid and obeticholic acid improve liver function and symptoms but may not halt progression of disease
- Liver transplant for advanced / cirrhotic cases; may eventually recur in the graft
Gross description
- Hepatomegaly early; cirrhosis late
Microscopic (histologic) description
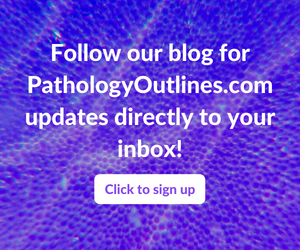
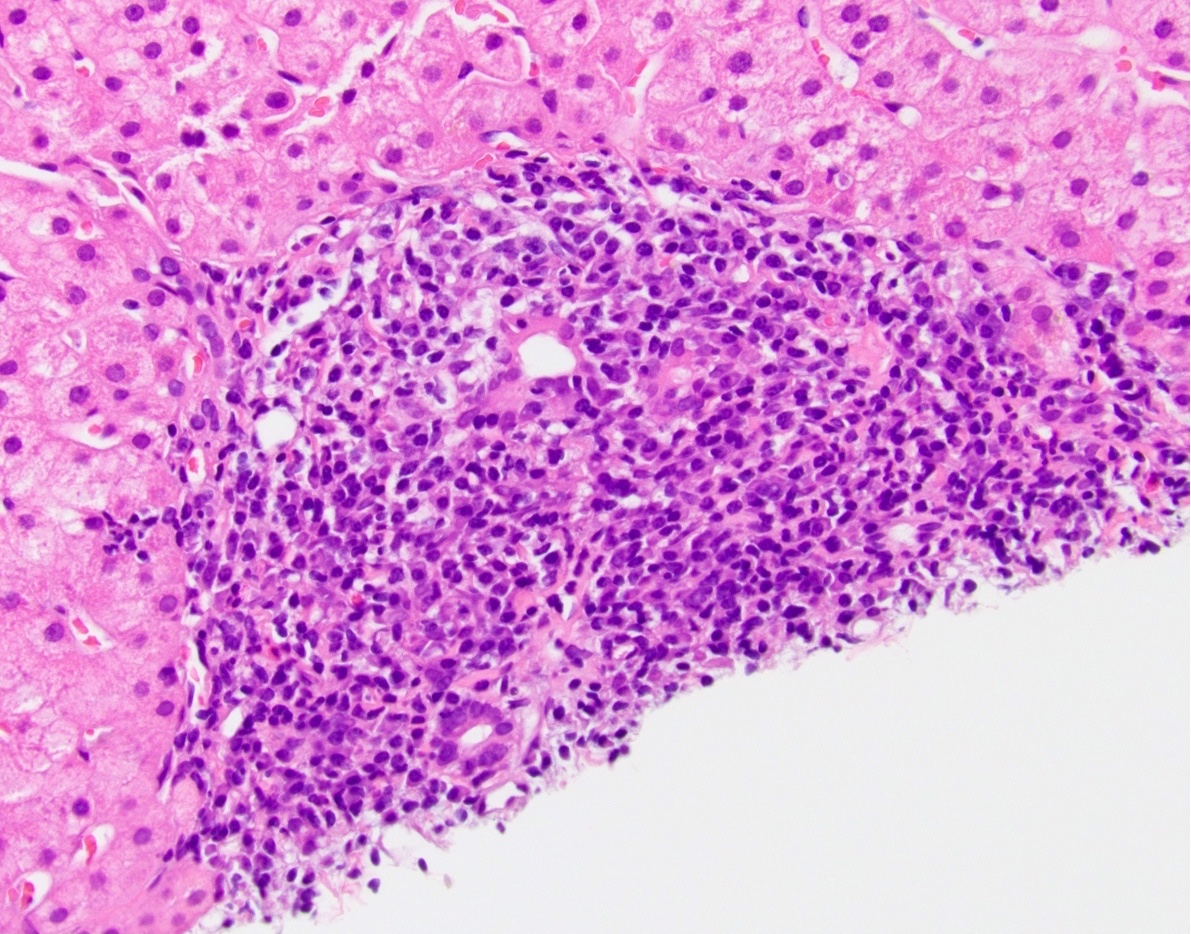
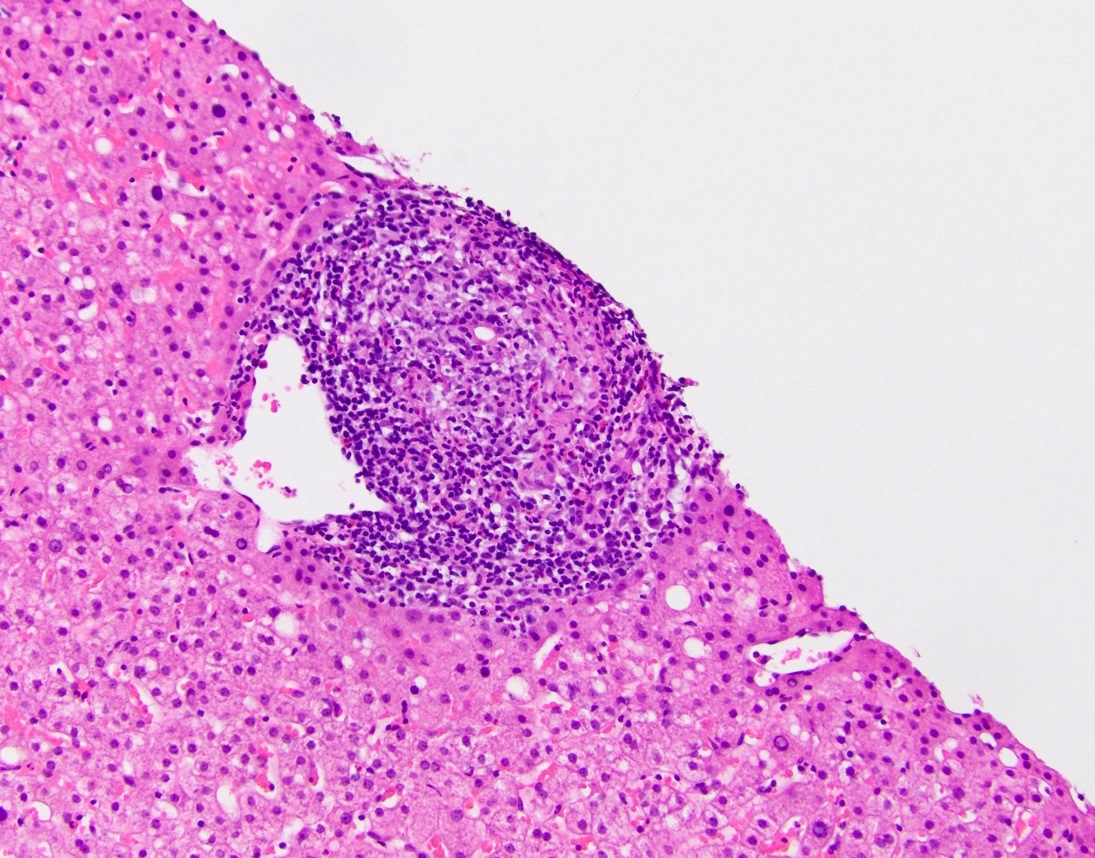
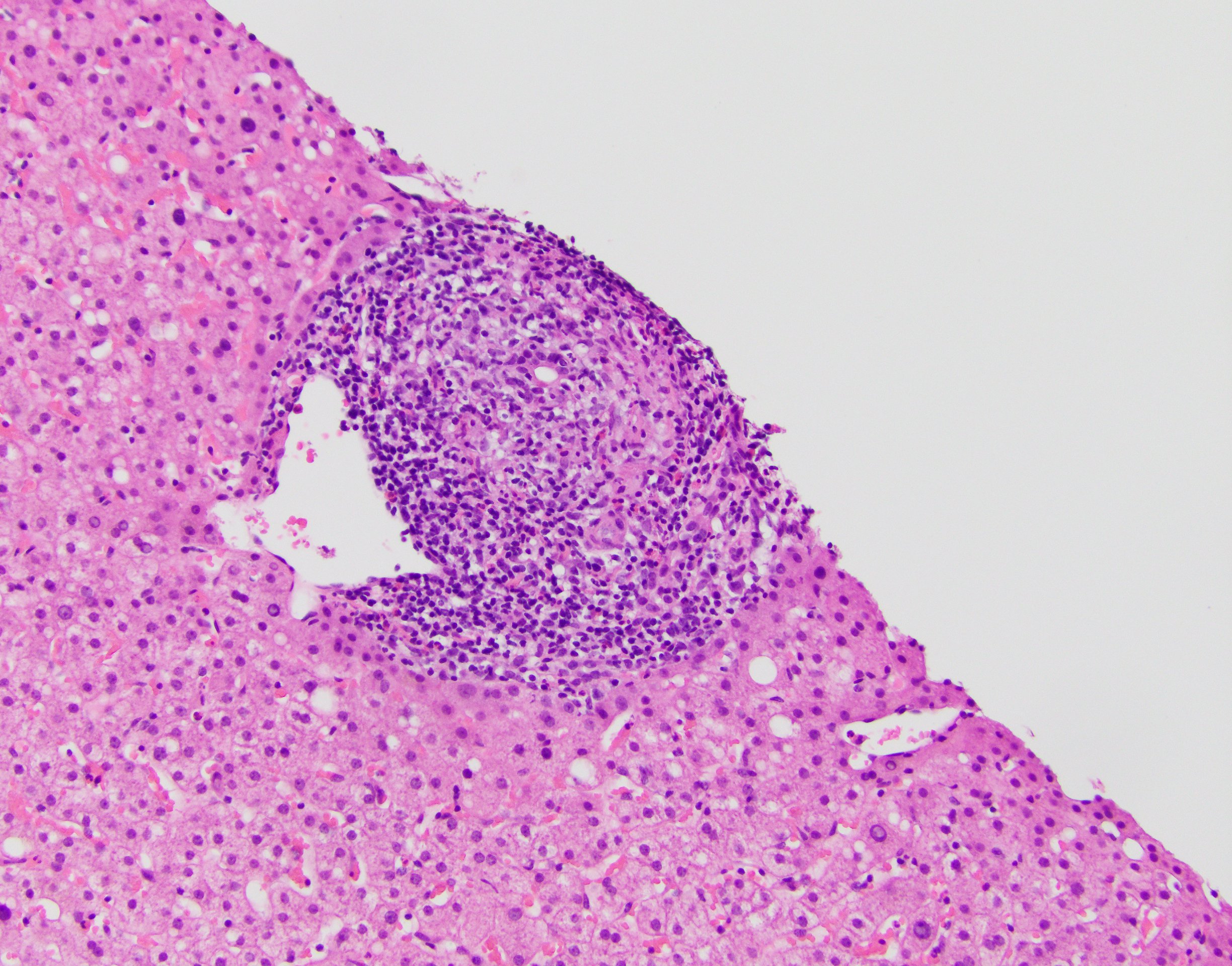
- Dense lymphocytic infiltrate in portal tracts with granulomatous destruction and loss of medium sized interlobular bile ducts, focal and variable within the liver
- May involve sinusoids early
- Periportal Mallory hyaline late, usually minimal neutrophils, variable portal eosinophils; resembles graft versus host disease and graft rejection; ductules derived from periportal hepatocytes are still present; prominent Ito cells with fat vacuoles
- Key finding is the florid duct lesion: interlobular bile ducts (within small portal tracts) are destroyed by poorly formed portal epithelioid granulomas
- Dense lymphocytic infiltrate in portal tracts can also be seen, mimicking hepatitis
- Ductular reaction and duct injury early; duct loss and lobular cholestasis with feathery degeneration late
- Lobules may show macrophage aggregates / small granulomas but typically not much of an inflammatory infiltrate
- The above changes are patchy and may not be present in a given biopsy
- Nodular regenerative hyperplasia may be seen in early disease (Gastroenterology 1992;102:1319)
- Staging:
- Florid duct lesions or portal hepatitis
- Ductular reaction or periportal hepatitis
- Bridging/septal fibrosis or bridging necrosis
- Cirrhosis
Microscopic (histologic) images
Positive stains
- Note: None of these stains are routinely used for diagnosis
- S100: highlights dendritic cells in the basement membrane in early stage disease (Am J Pathol 1989;134:741)
- CD1a: highlights Langerhans cells in biliary epithelium (Am J Surg Pathol 2012;36:732)
- Copper stains: positive within hepatocytes in all chronic cholestatic conditions, including PBC
Sample pathology report
- Liver, biopsy:
- Biliary pattern injury with mild chronic portal inflammation, ductular reaction, and focal changes suggestive of florid duct lesion (see comment)
- Comment: The histologic findings, in addition to the patient’s reported history of antimitochondrial antibody, are consistent with primary biliary cholangitis. A trichrome stain shows minimal periportal fibrosis.
Differential diagnosis
- Autoimmune cholangitis:
- Essentially the same diagnosis, except AMA is negative
- Autoimmune hepatitis:
- More normal alkaline phosphatase, antismooth muscle antibody positive and AMA negative, elevated IgG rather than IgM, lobular inflammation
- Secondary biliary cirrhosis:
- Cirrhotic liver in the setting of longstanding large duct injury
- No AMA or florid duct lesions
- Primary sclerosing cholangitis:
- Minimal inflammation, classic imaging findings
- Large duct obstruction:
- Clinical presentation often acute
- Cholestasis early in the disease process, rather than late
- Drug induced liver injury:
- Can mimic; clinical correlation necessary
Additional references
Board review style question #1
- Which of the 2 following features are considered pathognomonic for primary biliary cholangitis?
- Antimitochondrial antibody and florid duct lesions
- Antineutrophil cytoplasmic antibody and onion skin fibrosis
- Antinuclear antibody and ductular reaction
- Antismooth muscle antibody and interface hepatitis
Board review style answer #1
A. Antimitochondrial antibody and florid duct lesions
Comment Here
Reference: Primary biliary cholangitis
Comment Here
Reference: Primary biliary cholangitis
Board review style question #2
Board review style answer #2
D. Ursodeoxycholic acid. This is primary biliary cholangitis.
Comment Here
Reference: Primary biliary cholangitis
Comment Here
Reference: Primary biliary cholangitis