Table of Contents
Definition / general | Terminology | Epidemiology | Diagrams / tables | Pathophysiology | Clinical features | Treatment | Microscopic (histologic) description | Positive stainsCite this page: Rishi A, Cornish TC. Fissure. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/anusanalfissure.html. Accessed August 27th, 2025.
Definition / general
- Most common benign lesion resulting from high intraluminal anal pressure
- Painful linear separation or tear of anal canal mucosa distal to dentate line and extending either superficial or deep into anal mucosa
- Fissures are most commonly located at posterior commissure overlying external and internal sphincter bifurcation as it divides to circle the rectum, implying that the sphincter cuff is weakest at posterior anal wall
- Most commonly post traumatic and located in midline; nonmidline anal fissures should raise suspicion of malignancy, inflammatory bowel disease or infection
- Trauma may be due to constipation, instrumentation, childbirth or sexual abuse
- Nontraumatic cases include infections (tuberculosis, cytomegalovirus, herpes, syphilis, gonorrhea, chlamydia), inflammatory bowel disease (4% of Crohn's disease patients have fissures as initial manifestation) or malignancy involving anal mucosa
- Histopathology is generally nonspecific but may have etiology specific features
Terminology
- Acute anal fissure: typically heals after conservative treatment in < 6 weeks
- Chronic anal fissure: resistant to conservative treatment and may require surgical management
Epidemiology
- Most commonly affects infants and young / middle aged individuals
- Equally prevalent in males and females
Diagrams / tables
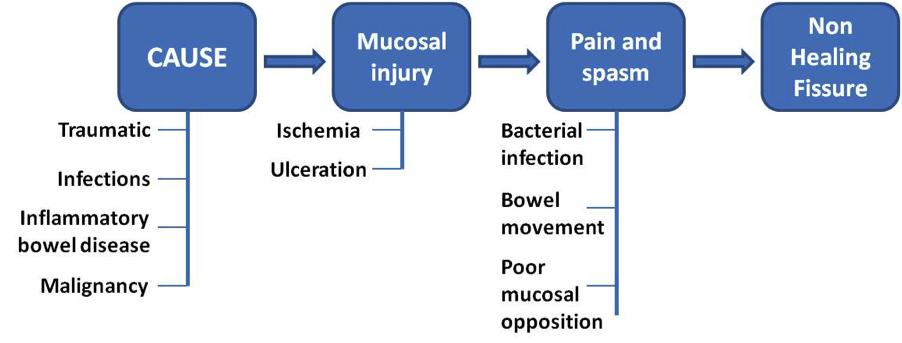
Pathophysiology
- The basic mechanism of injury is stretching of the anal mucosa beyond its physiological limits, which causes mucosal defects in areas with poor muscular support
- The initiation of a mucosal tear leads to a vicious cycle of healing and repeated injury due to stretching from continuous bowel movements
- The impaired healing and pain leads to persistent spasm of the internal sphincter and increased mean average resting luminal pressure
- The persistent spasm leads to nonopposition of the tear, impaired wound healing, bacterial colonization and progression to chronic anal fissure in up to 40% of patients (World J Gastrointest Pharmacol Ther 2011;2:9)
Clinical features
- 90% of fissures are located in the posterior anal wall
- Midline anterior fissures are more common in females due to anatomical location of vagina and related weak muscular support
- Acute fissures usually have severe tearing pain associated with passage of stools, bright red rectal bleeding evident as streaks of blood, perianal eczema and pruritis
- Chronic fissures are usually less painful
- Physical examination may show a midline defect, superficial tear or laceration of variable depth and size depending on cause and duration
- Chronic fissure may appear as hypertrophied skin tag
Treatment
- Most common treatment is medical and conservative, which includes warm baths and increased fiber intake
- Warm sitz baths may lead to healing of anal fissures via a somatoanal reflex that results in relaxation of internal anal sphincter
- Better healing occurs with topical steroids and local topical anesthetics but caution and medical supervision is advised before using topical agents
- Operative management is indicated after failure of conservative or more extensive medical management (Clin Colon Rectal Surg 2011;24:22)
Microscopic (histologic) description
- May be nonspecific; shows ulcerated transitional or columnar mucosa with acute and chronic inflammation, granulation tissue, reactive and regenerative epithelial changes or foreign body giant cell reaction
- Anal fissures related to specific etiology may show epithelioid cell granulomas as in tuberculosis, fungal infection or Crohn's disease (Quizlet: Gastrointestinal Pathology [Accessed 15 October 2021])
- Lymphogranuloma venereum and syphilis induced ulcers may show intense inflammation rich in plasma cells (Am J Surg Pathol 2013;37:38)
Positive stains
- For tuberculosis, acid fast bacilli stains may be positive (Indian J Dermatol Venereol Leprol 2008;74:386)
- Also cultures from anal discharge (Isr Med Assoc J 2013;15:782)