Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Sarungbam J. Urothelial papilloma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bladderpapilloma.html. Accessed August 15th, 2025.
Definition / general
- Papillary urothelial neoplasm characterized by delicate fibrovascular cores lined by urothelium of normal thickness and cytology
Essential features
- Rare papillary urothelial neoplasm with a benign clinical course: rare recurrence if completely excised
- Exophytic tumor composed of thin papillary fronds lined by prominent umbrella cells
- Should be distinguished from its morphologic mimics, including papillary urothelial neoplasm of low malignant potential (PUNLMP), urothelial carcinoma, polypoid cystitis and fibroepithelial polyp
Terminology
- Transitional cell papilloma
ICD coding
Epidemiology
- Rare urothelial neoplasm, comprises ~1% of all papillary bladder neoplasm
- Patients are generally younger than those with urothelial carcinoma
- Generally, < 50 years of age (Mod Pathol 2003;16:623)
- Can also be seen in children
- M:F - 1.9:1 (Cancer 1999;86:2098, Pathology 2014;46:37)
- Often presents as solitary lesion (Cancer 1999;86:2098)
- Usually presents de novo, also rarely seen in patients with other prior urothelial neoplasms (Mod Pathol 2003;16:623)
Sites
- Any site in the bladder, most commonly the posterior or lateral wall (Mod Pathol 2003;16:623)
Etiology
- Unknown at this time but often associated with KRAS / HRAS mutations
Clinical features
- Painless hematuria, gross or microscopic
Diagnosis
- Imaging: ultrasound (USG)
- Cystoscopy: papillary / elevated lesions, variable size, often unifocal (Mod Pathol 2003;16:623)
- Biopsy / transurethral resection of bladder tumor needed for diagnosis
Laboratory
- Urine cytology is negative for malignant cells
Radiology description
- Ultrasound: endovesical papillary lesion
Radiology images
Prognostic factors
- Recurrences have been reported in 0 - 8.8% (Mod Pathol 2000;13:1315, Am J Surg Pathol 2004;28:1615, Mod Pathol 2003;16:623)
- Reported progression to higher grade lesion 0 - 8.8% but in fact extremely uncommon (Am J Surg Pathol 2004;28:1615, J Urol 2007;178:1201, Pathology 2014;46:37)
Case reports
- 9 year old boy with gross hematuria (BMJ Case Rep 2017;2017:219341)
Treatment
- Resection: transurethral resection of bladder tumor (TURBT)
Gross description
- Soft, pink, small isolated growth with delicate papillary structures, usually pedunculated
Microscopic (histologic) description
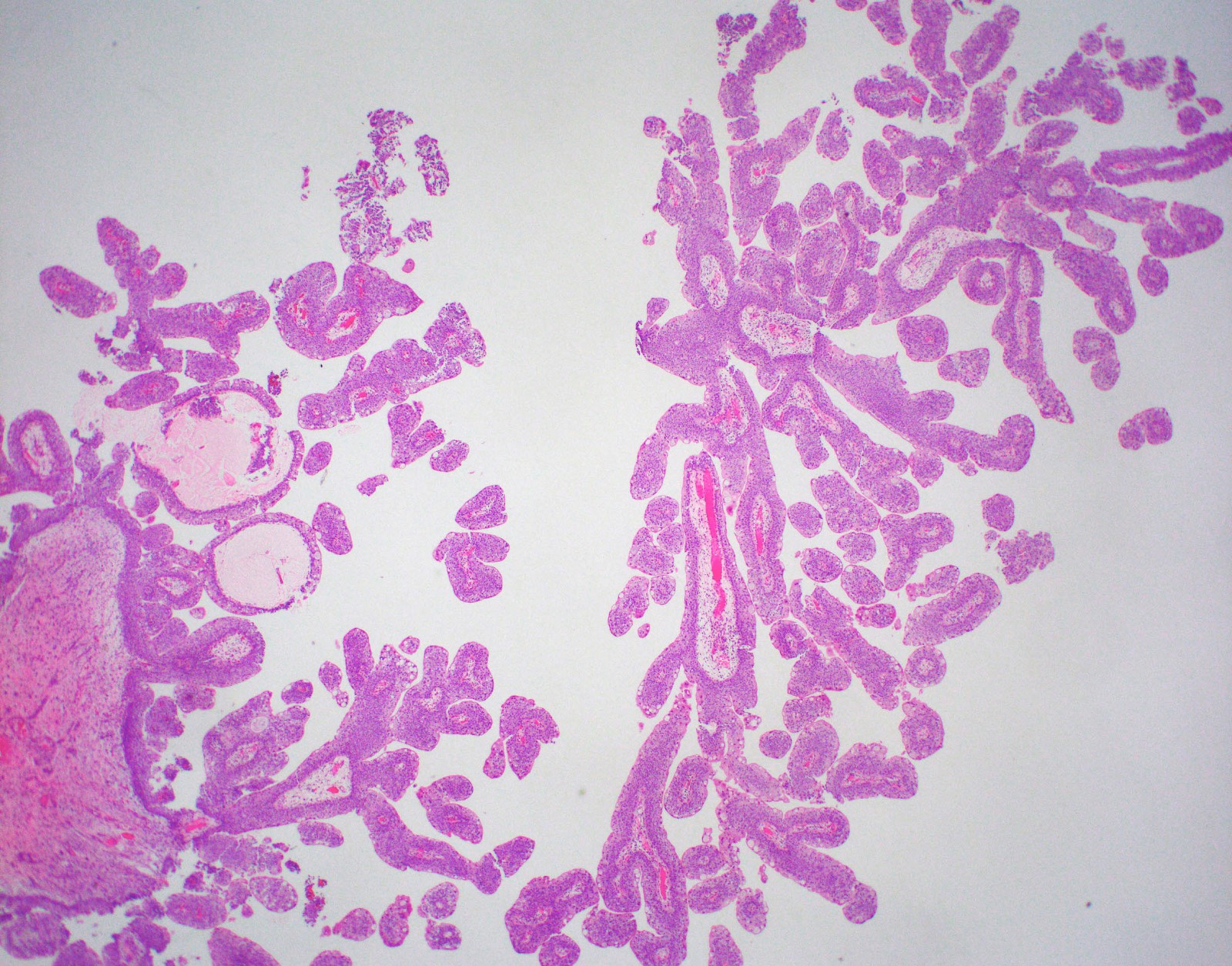
- Predominantly exophytic tumor
- Discrete papillary structures with central fibrovascular cores with hierarchical branching pattern but without fusion
- Papillae appear to float above urothelial surface due to transverse sectioning of branching papillae
- Papillae usually slender with scant stroma around fibrovascular cores
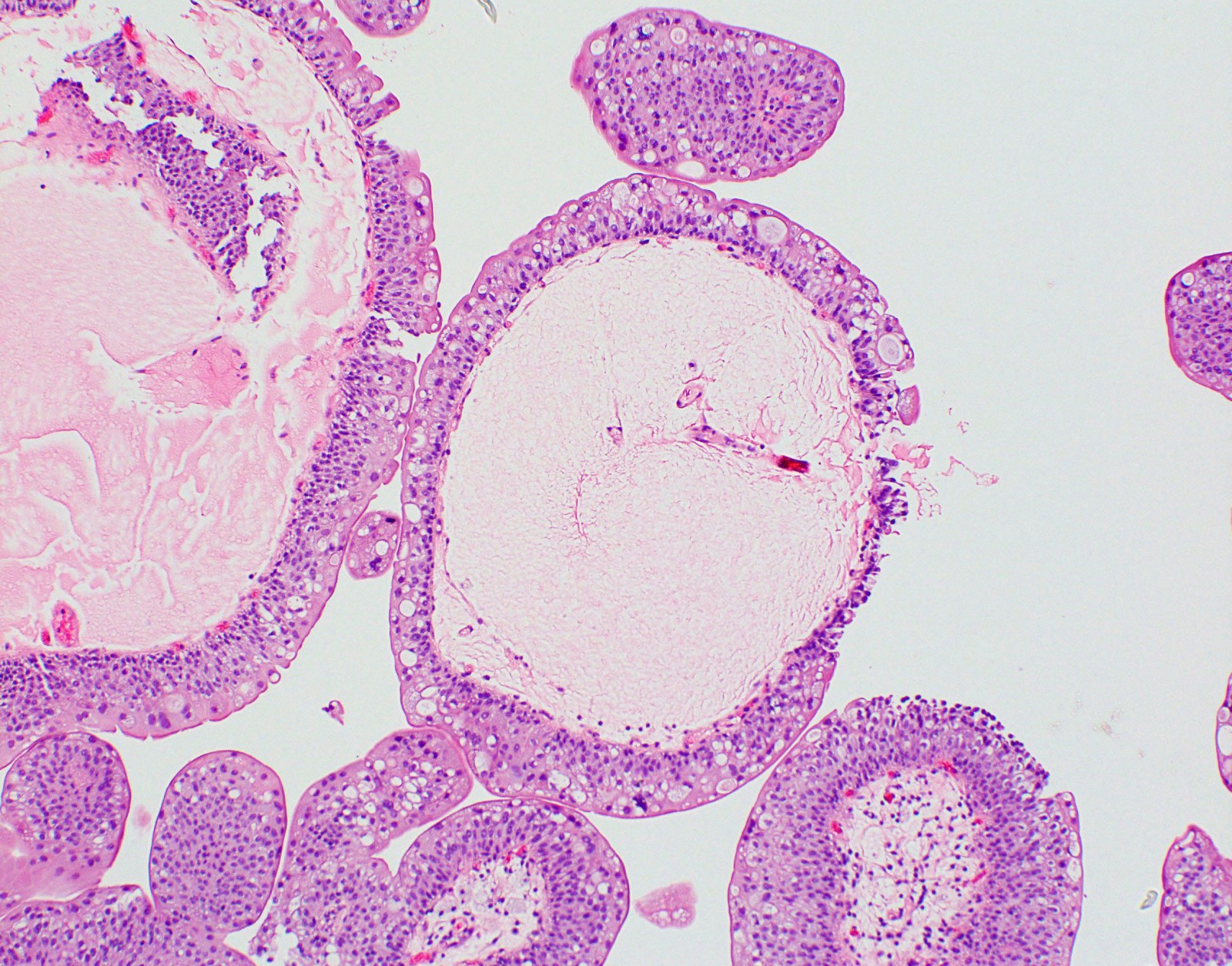
- May have large papillae with marked stromal edema or cystitis cystica-like invaginations
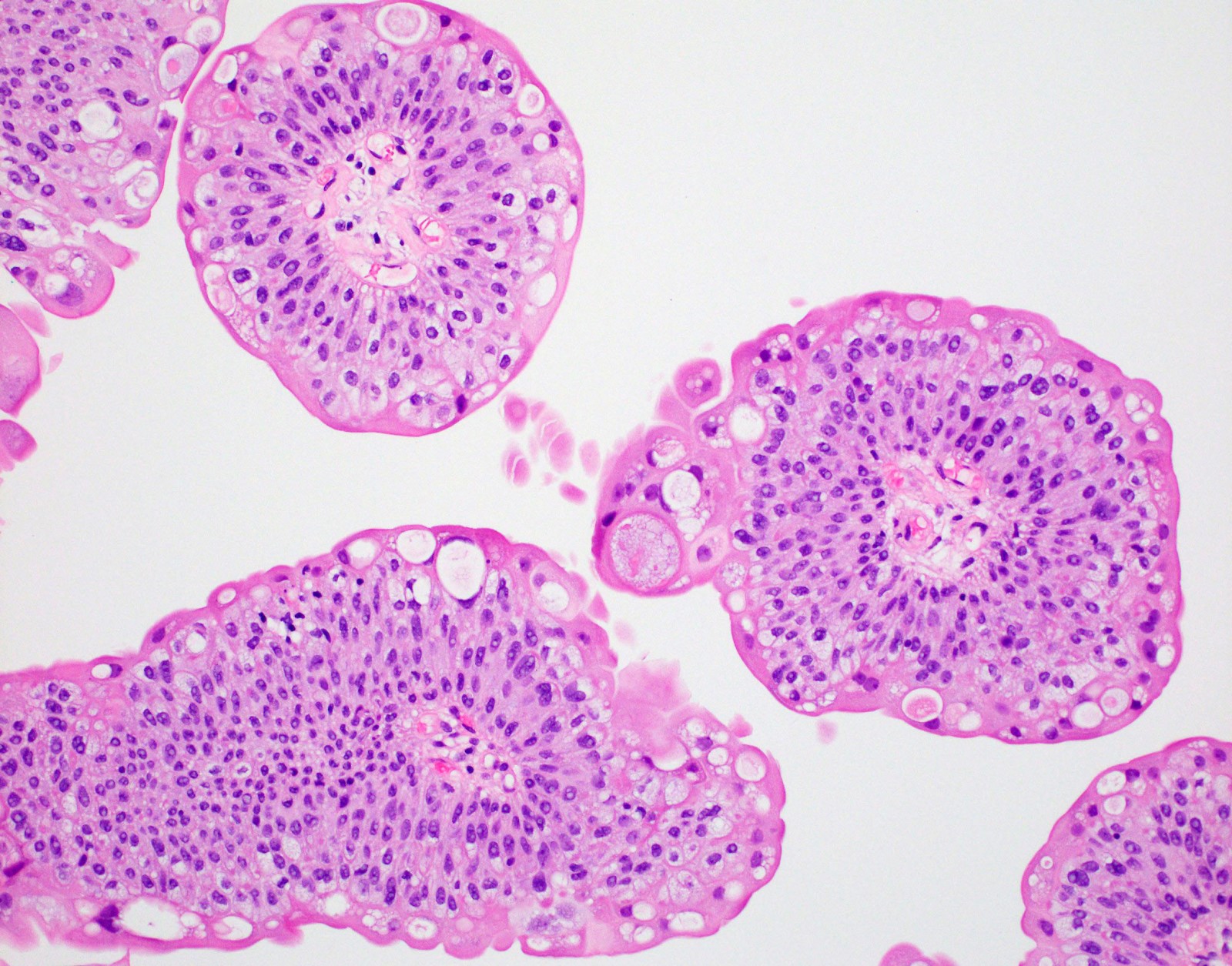
- Papillary structures are lined by urothelium of normal thickness and cytology; often with prominent umbrella cells layer
- Umbrella cells may show cytoplasmic vacuolization and degenerative type atypia
- There should be no marked cytologic atypia, increased thickness of the urothelium or increased mitotic / apoptotic figures
- Diffuse papillomatosis: rarely bladder mucosa covered / replaced by multiple papillomas (Virchows Arch 2002;441:109)
Microscopic (histologic) images
Positive stains
- CK20 is positive in the umbrella cell layer
Negative stains
- No p53 abnormality
Molecular / cytogenetics description
- Targeted next generation sequencing (NGS) and whole exome sequencing (WES) showed (J Pathol 2019;248:260)
- Activating mutations involving the MAPK / ERK pathway, in particular KRAS and HRAS genes, are common alterations
- KRAS mutations more frequent than HRAS
- Mutations in chromatin modifiers (often associated with urothelial carcinoma) are rare
- Low tumor mutational burden
- No APOBEC (apolipoprotein B mRNA editing catalytic polypeptide-like) mutational signature (identified in about 70% of muscle invasive urothelial carcinomas)
- Other earlier studies have shown
- FGFR3 mutations in 75% (J Pathol 2002;198:245)
- TERT promoter mutation in 46% (12/26) (Eur Urol 2017;71:497)
- However, these findings have not been replicated in the newer study using NGS and WES
Sample pathology report
- Urinary bladder, right lateral trigone, transurethral resection of bladder tumor:
- Urothelial papilloma
Differential diagnosis
- Papillary urothelial neoplasm of low malignant potential (PUNLMP):
- Complex papillary structures with branching and fusion
- Increased cellular proliferation, resulting in increased thickness of the urothelium
- No architectural abnormality (maintained polarity)
- No nuclear atypia
- Lacks prominent umbrella cell layer
- Noninvasive papillary urothelial carcinoma low grade:
- Complex papillary structures with branching and fusion
- Usually increased thickness of urothelium with architectural and cytologic atypia
- Papillary carcinoma without increased thickness shows marked cytologic and architectural abnormality
- Lacks prominent umbrella cell layer
- Polypoid / papillary cystitis:
- Usually has history of urothelial irritation, e.g. stones, radiation, stents etc. (Am J Surg Pathol 2008;32:758, J Urol 2013;189:1091)
- Best evaluated at low power microscopy
- Predominantly nonbranching broad base fronds with edematous / fibrotic stroma associated with inflammation
- Lining urothelium shows reactive atypia
- Lacks prominent umbrella cell layer
- Fibroepithelial polyp:
- More often seen in children, though they can be seen in adults
- Can be a polypoid mass or a papillary lesion
- Usually has broader stalks with dense fibrous tissue cores
- Lacks prominent umbrella cell layer
Practice question #1
Practice answer #1
D. Urothelial papilloma. Note the papillary architecture with thin fibrovascular cores, a normal appearing urothelial lining and prominent umbrella cell layer.
Comment Here
Reference: Urothelial papilloma
Comment Here
Reference: Urothelial papilloma
Practice question #2
- Which of the following is true regarding urothelial papilloma?
- Associated with high rate of recurrence and progression
- Lined by urothelium of normal thickness and cytology
- Seen in an older age group than urothelial carcinoma
- Umbrella cell atypia excludes the diagnosis
Practice answer #2
B. Urothelial papilloma is an exophytic papillary neoplasm lined by urothelium of normal thickness and cytology. Urothelial papilloma is often seen in a younger age group than urothelial carcinoma and has no or a very low recurrence rate. A prominent umbrella cell layer is characteristic. The umbrella cells often show marked atypia and this should not be used to change the diagnosis from urothelial papilloma to urothelial carcinoma.
Comment Here
Reference: Urothelial papilloma
Comment Here
Reference: Urothelial papilloma