Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Pathophysiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Serinelli S, de la Roza G. Atypical cartilaginous tumor / chondrosarcoma, grade 1. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/boneatypicalcartilaginoustumor.html. Accessed September 17th, 2025.
Definition / general
- Atypical cartilaginous tumor / chondrosarcoma, grade 1 (ACT / CS1) is a locally aggressive, hyaline cartilage producing neoplasm; tumors in the appendicular skeleton (long and short tubular bones) are termed ACTs, whereas tumors in the axial skeleton (flat bones, including the pelvis, scapula and skull base) should be called CS1
- Primary conventional ACT / CS1 are tumors arising without a benign precursor; secondary conventional ACT / CS1 are tumors arising in association with a preexisting benign precursor.
Essential features
- Abundance of cartilaginous matrix, often hyaline, sometimes with myxoid changes
- Lobular growth pattern with entrapment of pre-existing lamellar bone trabeculae
- Increased cellularity, with small condensed nuclei; binucleated cells are common
- Absence of mitoses and severe nuclear atypia
Terminology
- Primary central atypical cartilaginous tumors: arise in the medulla of bone without a benign precursor
- Primary peripheral atypical cartilaginous tumors: arise on the bone surface without a benign precursor
- Secondary central atypical cartilaginous tumors: arise in the medulla of bone in association with a pre-existing enchondroma
- Secondary peripheral atypical cartilaginous tumors: arise within the cartilaginous cap of a pre-existing osteochondroma
- Reference: Nosé: Diagnostic Pathology - Familial Cancer Syndromes, 2nd Edition, 2020
ICD coding
- ICD-O:
- 9222/1 - atypical cartilaginous tumor
- 9222/3 - chondrosarcoma, grade 1
- ICD-11: XH0FY0 - atypical cartilaginous tumor
Epidemiology
- Third to sixth decades of life
- M = F
- Cumulative incidence of central atypical cartilaginous tumor / chondrosarcoma grade 1: 6.63 per 1 million person years (Surg Oncol 2018;27:402)
- Central atypical cartilaginous tumor / chondrosarcoma grade 1 are more common (85 - 90%) than peripheral (10 - 15%)
- Patients with secondary tumors are younger than those with primary tumors (Clin Orthop Relat Res 2003;411:193)
Sites
- Bones that form by endochondral ossification (Arch Pathol Lab Med 2020;144:71)
- Appendicular skeleton (long and short tubular bones)
- Central atypical cartilaginous tumor:
- Femur, humerus and tibia are most affected
- 50% in metaphysis, 33% in the diaphysis and the rest in the epiphysis
- Rare in the short tubular bones of hands and feet
- Secondary peripheral atypical cartilaginous tumor:
- Tibia and femur are most often involved
Etiology
- Sporadic: 90% of cases; somatic mutations in the isocitrate dehydrogenase genes IDH1 / IDH2 in 50% of tumors, leading to altered hydroxyglutarate levels (J Cancer Metastasis Treat 2021;7:8)
- Enchondromatosis:
- Ollier disease and Maffucci syndrome: somatic postzygotic mutation in IDH1 / IDH2 (Nat Genet 2011;43:1262, Front Endocrinol (Lausanne) 2021;12:763349)
- Metachondromatosis: germline mutation in PTPN11 with loss of function
- Osteochondromatosis: germline mutations in EXT1 / EXT2 (Nosé: Diagnostic Pathology - Familial Cancer Syndromes, 2nd Edition, 2020, J Bone Oncol 2018;13:114)
Pathophysiology
- Mechanisms involved in the transformation of benign cartilaginous lesions to malignant lesions have not been entirely elucidated
Clinical features
- Pain, enlarging mass or pathologic fracture (Clin Orthop Relat Res 2003;411:193)
- Worsening of clinical symptoms in pre-existing enchondromas / osteochondromas
- Can be asymptomatic
Diagnosis
- Imaging studies (Xrays, MRI, CT) and tissue biopsy
- Because of high concordance of biopsy sample and presumed diagnosis on imaging studies alone, a diagnostic biopsy is often not necessary (J Am Acad Orthop Surg Glob Res Rev 2021;5:e21.00277)
- The diagnostic distinction of ACT / CS1 from other cartilaginous lesions requires strict clinical and radiologic correlation combined with histologic examination, with the most important histologic feature being infiltration and encasement of preexisting trabecular bone (Arch Pathol Lab Med 2020;144:71)
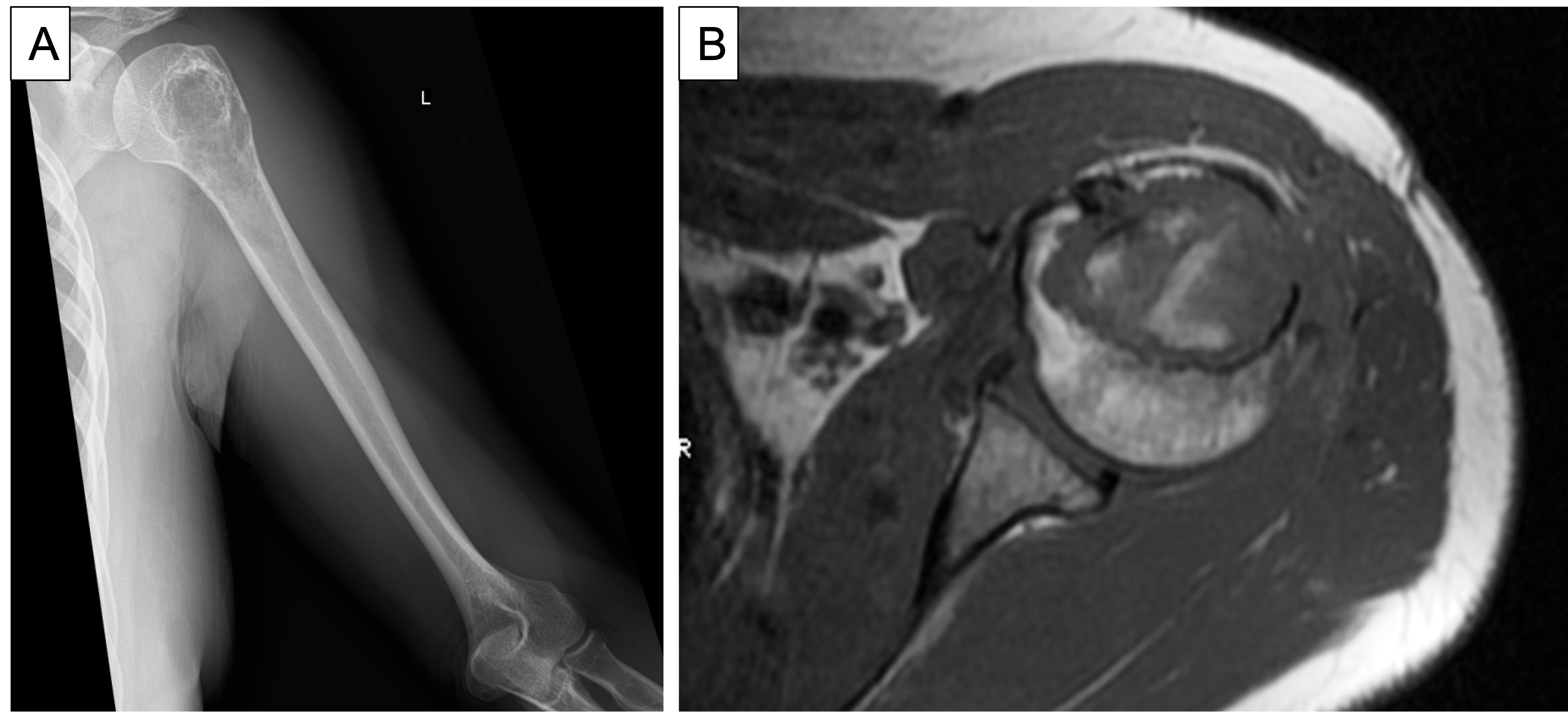
Radiology description
- Radiographically, it appears as an ill defined lytic lesion with geographical destruction, cortical scalloping and thickening of the cortex, often containing popcorn calcifications (Eur J Radiol 2015;84:2222)
- MRI shows lesions > 2 cm with cortical remodeling, deep scalloping and enhancement
- MRI is the best validated method to detect an atypical cartilaginous tumor arising in an osteochondroma
- Cartilaginous cap thickness of > 2 cm in osteochondroma may raise concern for malignant transformation but is not entirely sufficient (Rofo 2021;193:262)
- Presence of cortical expansion, followed by the presence of deep endosteal scalloping and a size > 6 cm, is the key imaging feature for differentiating enchondroma from atypical cartilaginous tumor, on both CT and MRI (Acta Radiol 2022;63:376)
Radiology images
Prognostic factors
- Atypical cartilaginous tumors show good prognosis, after curettage (J Bone Joint Surg Am 2016;98:303)
- Locally aggressive behavior
- Local recurrence in 7.5 - 11% of central atypical cartilaginous tumors and in 16 - 17.5% of secondary peripheral atypical cartilaginous tumors, due to incomplete excision in difficult locations (Eur J Orthop Surg Traumatol 2017;27:805, Clin Orthop Relat Res 2003;411:193)
- In approximately 10% of recurring atypical cartilaginous tumors, progression to a higher grade is seen
- Outcome is worse in tumors located in the axial skeleton (chondrosarcomas)
- At present it is uncertain whether the presence of an IDH mutation is associated with prognosis (Clin Sarcoma Res 2017;7:8)
Case reports
- 36 year old man with atypical cartilaginous tumor / low grade chondrosarcoma of the proximal phalanx of the third finger (Case Rep Orthop 2019;2019:6402979)
- 37 year old man with atypical cartilaginous tumor / grade 1 chondrosarcoma of the distal phalanx of the great toe (J Cancer Res Ther 2012;8:123)
- 40 year old man with atypical cartilaginous tumor / grade 1 chondrosarcoma of the femur (Kaohsiung J Med Sci 2009;25:552)
- 62 year old woman with atypical cartilaginous tumor / grade 1 chondrosarcoma of the distal phalanx of the great toe (J Am Podiatr Med Assoc 2007;97:156)
- 76 year old man with atypical cartilaginous tumor / grade 1 chondrosarcoma of the middle phalanx of the ring finger, accompanied by enchondromata (Arch Orthop Trauma Surg 2003;123:42)
Treatment
- Intralesional excision with curettage, adjunctive high speed burring and bone void augmentation (J Am Acad Orthop Surg Glob Res Rev 2021;5:e21.00277)
Gross description
- Fragments from curettage are composed of glistening white-gray cartilage; yellow-white chalky areas of calcification are often present
- In resection specimens, central atypical cartilaginous tumors are well defined, permeate the medullary cavity, scallop endosteal surface and produce cortical thickening
- Secondary peripheral atypical cartilaginous tumors show a thick (> 2 cm), lobulated cartilaginous cap; the cap should be measured perpendicular to the bone / cartilage interface at its thickest portion (Clin Orthop Relat Res 2003;411:193, Mod Pathol 2012;25:1275)
Gross images
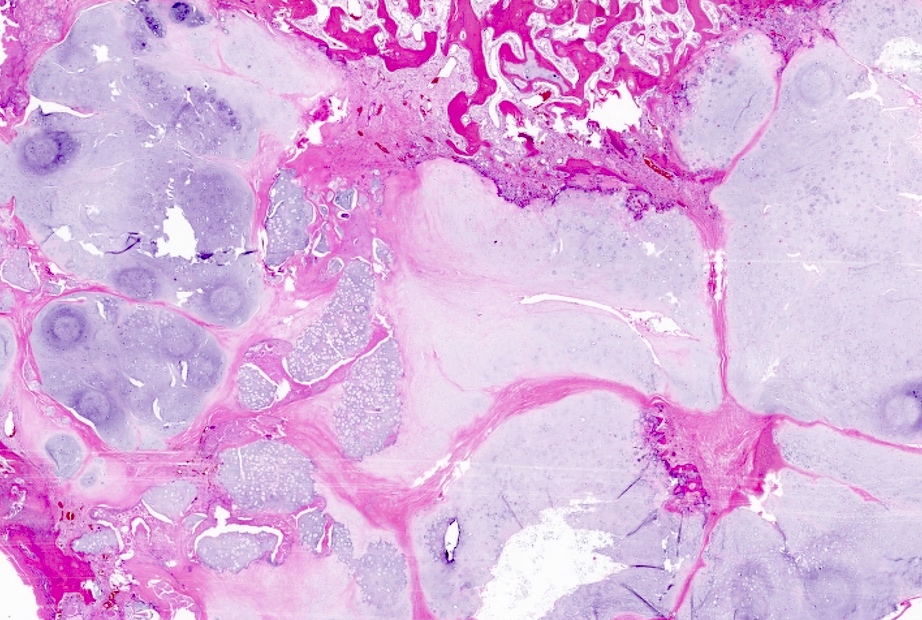
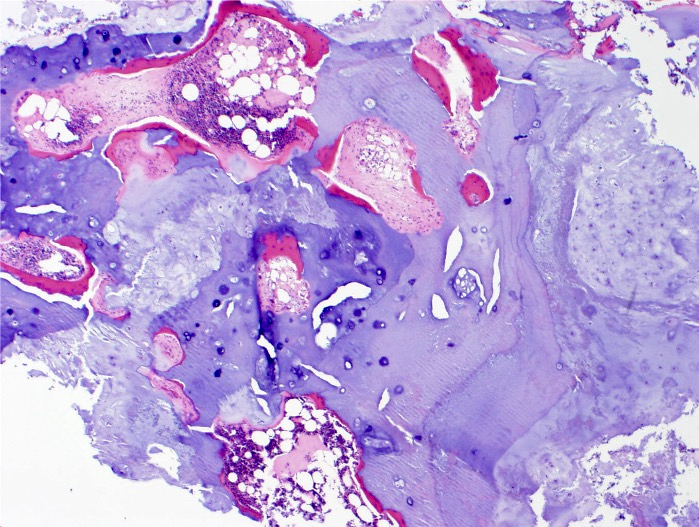
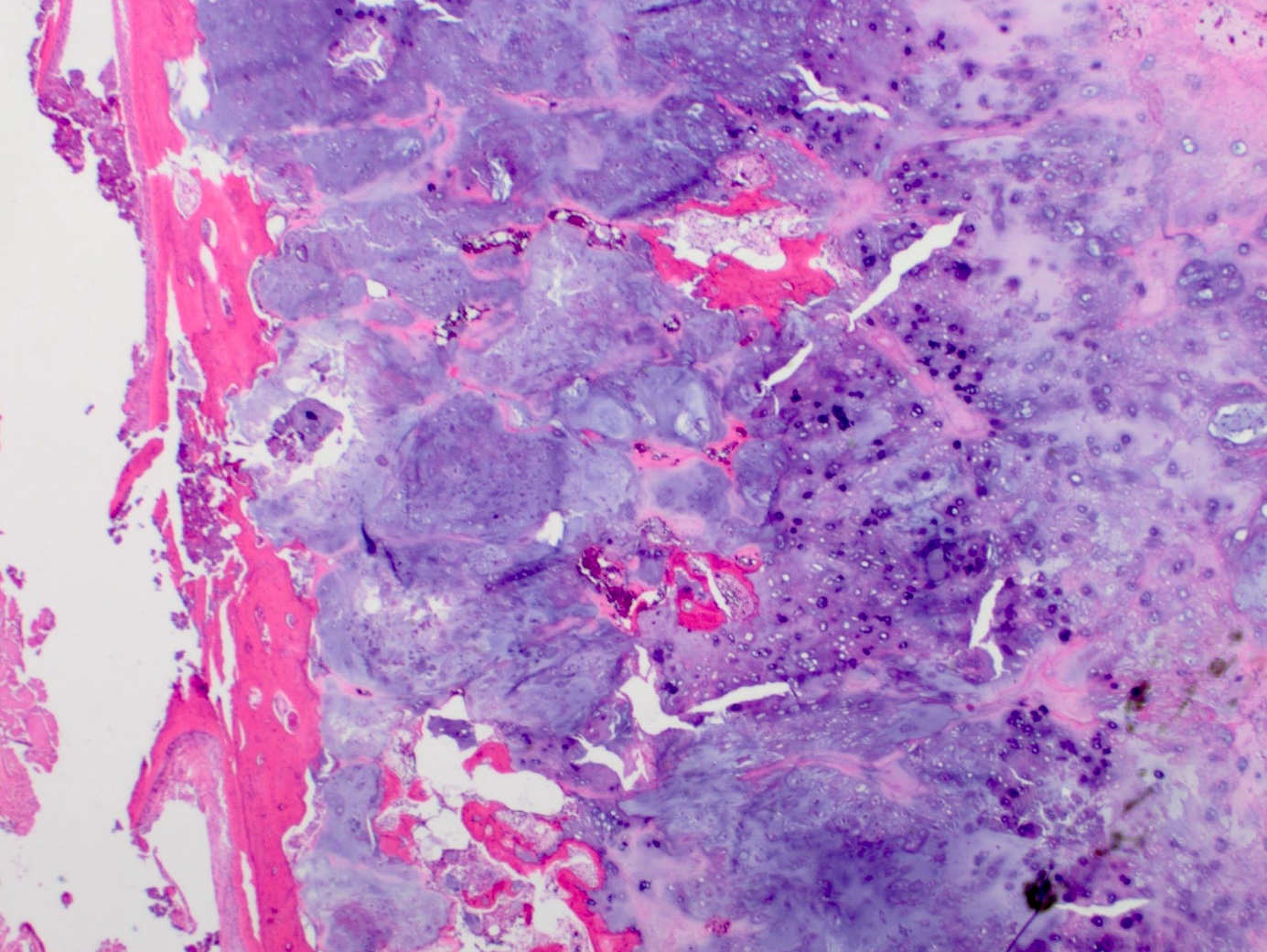
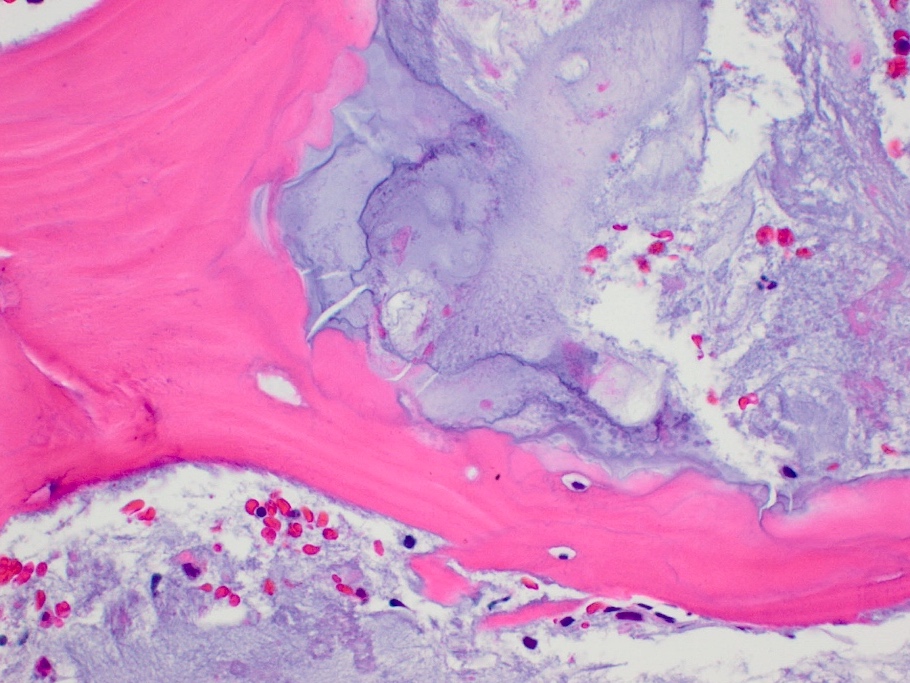
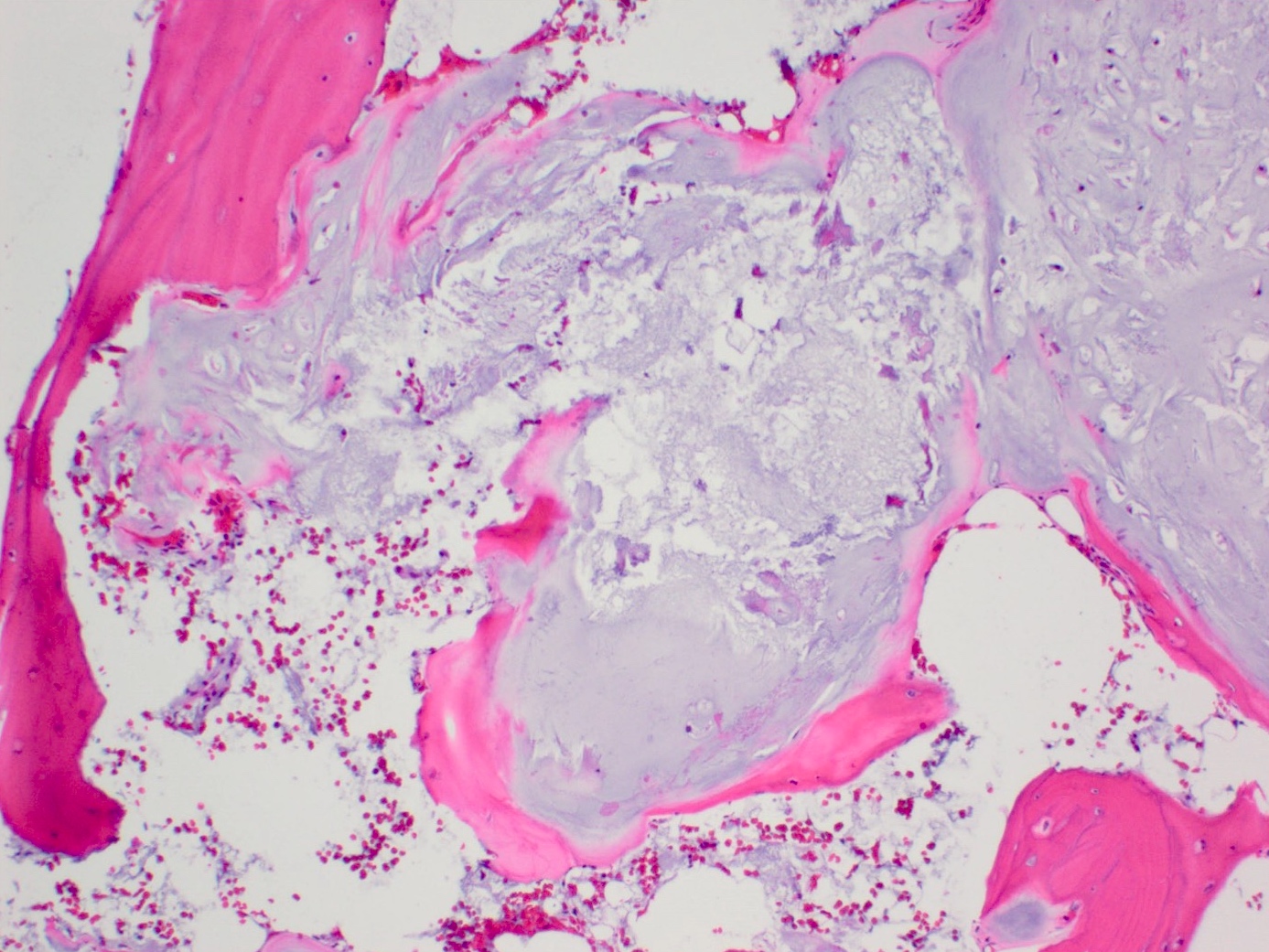
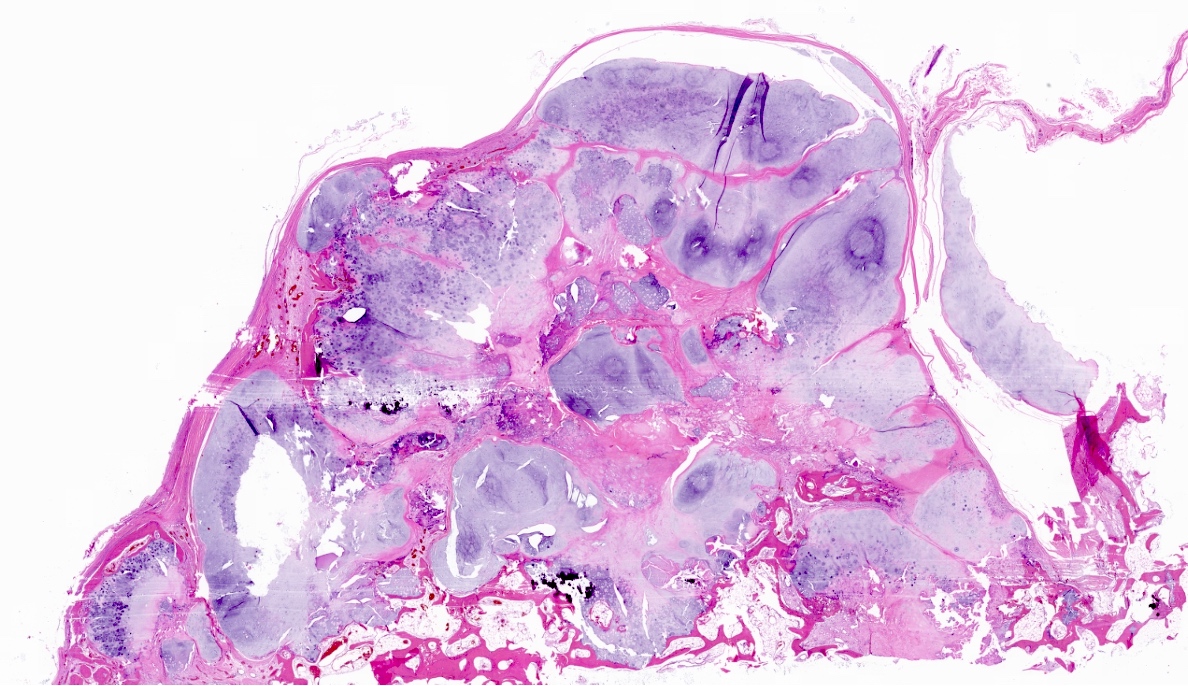
Microscopic (histologic) description
- Lobulated growth pattern (J Dent Res Dent Clin Dent Prospects 2011;5:98)
- Lobules have irregular shapes and sizes and may be separated by fibrous bands containing small vessels (Virchows Arch 2012;460:95)
- Lobules are composed of abundant hyaline cartilage matrix (sometimes with mucoid / myxoid changes) and permeate and entrap lamellar bone trabeculae
- Cellularity is slightly higher than in enchondroma
- Cells show moderate eosinophilic to vacuolated cytoplasm
- Nuclei are small and uniform with condensed chromatin (lymphocyte-like); sometimes they show open chromatin with visible nucleoli (Am J Surg Pathol 2009;33:50)
- Mitoses and significant nuclear pleomorphism are absent
- Binucleation can be observed
- Necrosis can be seen
- In cases arising from pre-existing enchondromas, areas of enchondroma with calcifications can be present
- In cases arising from pre-existing osteochondroma, evidence of this tumor can be seen (Mod Pathol 2012;25:1275)
Microscopic (histologic) images
Positive stains
Negative stains
Molecular / cytogenetics description
- Primary peripheral and central atypical cartilaginous tumors show hotspot mutations at the IDH1 p.Arg132 and the IDH2 p.Arg172 positions (Histopathology 2012;60:363, Mol Oncol 2021;15:3679, Cells 2020;9:968)
- IDH1 p.Arg132Cys mutation is the most frequently found
- Secondary central atypical cartilaginous tumors arising from enchondromas, a finding that often occurs as part of the genetic syndromes (Ollier disease and Maffucci syndrome), are also characterized by IDH mutations
- Secondary peripheral atypical cartilaginous tumors arising in association with osteochondromas show mutations in EXT1 and EXT2 (Clin Cases Miner Bone Metab 2016;13:110)
- Reference: J Cancer Metastasis Treat 2021;7:8
Videos
Chondrosarcoma versus enchondroma: bone pathology with Dr. Andrew Rosenberg
Sample pathology report
- Bone, left 5th and 4th metatarsals, excision:
- Atypical cartilaginous tumor (see microscopic description)
- Microscopic description: Examination of the histopathologic sections reveals mature trabecular bone with juxtaposed cartilaginous proliferation, characterized by low to moderate cellularity, chondrocytes with occasional binucleated cells and mild atypia in a hyaline cartilage matrix. Foci of necrosis, nonischemic type are seen. Given the presence of nonischemic type necrosis, the large size of the tumor and the cellular atypia, the tumor is most consistent with atypical cartilaginous tumor that may have arisen from an osteochondroma.
- The specimen consists of multiple unoriented fragments and the surgical margins cannot be assessed.
Differential diagnosis
- Enchondroma:
- Lower cellularity
- Regular distribution of cells
- No atypia
- No entrapment of pre-existing lamellar bone
- < 20% myxoid changes in the matrix (Am J Surg Pathol 2009;33:50)
- Grade 2 conventional chondrosarcoma:
- Increased cellularity
- Mitotic activity
- Myxoid matrix degeneration
- Spindle cell changes at the periphery of the lobules
- Increased vascularization
- Increased nuclear pleomorphism
- Osteochondroma:
- Differential for secondary peripheral atypical cartilaginous tumor
- Cartilaginous cap < 2 cm in thickness
Additional references
Practice question #1
A 41 year old woman complained of an enlarging mass at her left proximal humerus. Xrays showed a lucent lesion with indistinct borders and endosteal scalloping. MRI showed an irregular, expansile, avidly enhancing mass. A biopsy of the lesion was performed and is shown above. What is the diagnosis?
- Atypical cartilaginous tumor
- Chondrosarcoma, grade 3
- Enchondroma
- Mesenchymal chondrosarcoma
- Osteochondroma
Practice answer #1
Practice question #2
Which gene is more frequently mutated in atypical cartilaginous tumors?
- BRAF
- EGFR
- H3-3A
- IDH1
- KRAS
Practice answer #2