Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Hossein-Zadeh Z, Lee L. Acute self limited colitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/colonacuteselflimited.html. Accessed October 2nd, 2025.
Definition / general
- Defined as a transient, most likely infectious, disorder of the colon, which usually resolves completely within 2 - 4 weeks (Odze: Odze and Goldblum Surgical Pathology of the GI Tract, Liver, Biliary Tract and Pancreas, 3rd Edition, 2014)
- Due to infections, nonsteroidal anti-inflammatory drugs (NSAIDs) or other drugs, bowel preparation or procedure associated injury (e.g., gluteraldehyde disinfection of endoscope) (Arnold: Atlas of Gastrointestinal Pathology - A Pattern Based Approach to Neoplastic Biopsies, 1st Edition, 2019)
- Not always acute or self limited
Essential features
- Due to infections, NSAIDs or other drugs, bowel preparation or procedure associated injury (e.g., gluteraldehyde disinfection of endoscope) (Arnold: Atlas of Gastrointestinal Pathology - A Pattern Based Approach to Neoplastic Biopsies, 1st Edition, 2019)
- Wide variety of pathogens, most commonly bacterial organisms such as Campylobacter jejuni, Salmonella, Shigella species, E. coli and Yersinia enterocolitica (Odze: Odze and Goldblum Surgical Pathology of the GI Tract, Liver, Biliary Tract and Pancreas, 3rd Edition, 2014)
- Sudden onset, early fever, often with numerous (> 6) bowel movements daily
Terminology
- Acute self limited colitis
- Infectious colitis
ICD coding
- ICD-10: K52.9 - noninfective gastroenteritis and colitis, unspecified
Sites
- Large intestine
Pathophysiology
- Most commonly associated with bacterial enterocolitis (Int J Mol Sci 2020;21:4748)
- Bacterial virulence factors include:
- Adherence to epithelial cells
- Enterotoxins
- Invasion factors
- Cytotoxicity
- Adherence:
- Via fimbriae or pili
- Process of adherence destroys the microvilli brush border
- Enterotoxins:
- Toxins bind to cell membrane, enter cells, activate massive electrolyte secretion (cholera toxin, E. coli heat labile and heat stable toxins produce traveler's diarrhea)
- No white blood cells in stool
- Invasion factors:
- C. jejuni, Salmonella and Shigella species, E. coli and Y. enterocolitica are organisms that invade the tissue and cause epithelial injury and death
- These organisms invade via microbe simulated endocytosis, then cause cell lysis and cell to cell spread
- Tissue invasion also results in the production of inflammatory cytokines that trigger an acute inflammatory reaction
- Cytotoxins are polypeptides that cause tissue injury by inhibiting protein synthesis, disrupting tight junctions and depleting adenosine triphosphate (ATP) within cells
- Endothelial injury results in the activation of the coagulation cascade that ultimately leads to an ischemic colitis pattern of tissue injury (Odze: Odze and Goldblum Surgical Pathology of the GI Tract, Liver, Biliary Tract and Pancreas, 3rd Edition, 2014)
- Cytotoxicity:
- Shiga toxin, enterohemorrhagic E. coli
Etiology
- Wide variety of pathogens, most commonly bacterial organisms such as Campylobacter jejuni, Salmonella, Shigella species, E. coli and Yersinia enterocolitica (Odze: Odze and Goldblum Surgical Pathology of the GI Tract, Liver, Biliary Tract and Pancreas, 3rd Edition, 2014)
- Clinical manifestation of acute self limited colitis is related to the ability of microorganisms to invade mucosa or produce enterotoxins
- Ingestion of preformed toxins (Staphylococcus aureus, Vibrio cholera, Clostridium perfringens)
- Infection by enteroinvasive organisms which invade and destroy mucosal epithelium cells
- Infection by viral organisms (cytomegalovirus [CMV], herpes simplex virus [HSV], HIV, etc.)
Clinical features
- Abdominal pain, watery or bloody diarrhea (Int J Mol Sci 2020;21:4748)
- Causes symptoms within hours (including explosive diarrhea)
- Sudden onset, early fever, often with numerous (> 6) bowel movements daily
- Complications of dehydration, sepsis, perforation can occur secondary to potential massive fluid loss and loss of mucosal barrier
- Inflammatory process usually resolves completely within 2 - 4 weeks
Diagnosis
- Stool cultures (Gastroenterology 1994;107:755)
- Colonoscopy with mucosal biopsy
- Imaging studies can show nonspecific thickening of the bowel wall; however, they are seldom performed
Laboratory
- Peripheral blood and fecal leukocyte count
Radiology description
- Limited role since inflammatory abnormalities are nonspecific (e.g., colonic wall thickening)
Prognostic factors
- Depends on specific underlying infectious agent (Gastroenterology 1994;107:755)
- Immune status of host
- Generally good with appropriate therapy
- Commonly self limited disease (2 - 4 weeks)
Case reports
- 8 week old and 10 month old immunocompetent boys with CMV colitis, causing self limited colitis (Pediatr Infect Dis J 2016;35:573)
- 34 year old woman with Yersinia enterocolitica colitis mimicking acute appendicitis (Emerg Radiol 2008;15:123)
- 72 year old immunocompromised man with multidrug resistant Campylobacter colitis (BMC Infect Dis 2016;16:409)
Treatment
- Supportive therapy with rehydration
- Rarely may require antibiotics or steroids
Gross description
- Mucosal erythema, erosion, friability (Case Rep Infect Dis 2012;2012:810943)
- Ulceration, erosion, pseudopolyps, hyperemia
- Exudates may be present (pseudomembranes)
- Mass lesions are unlikely
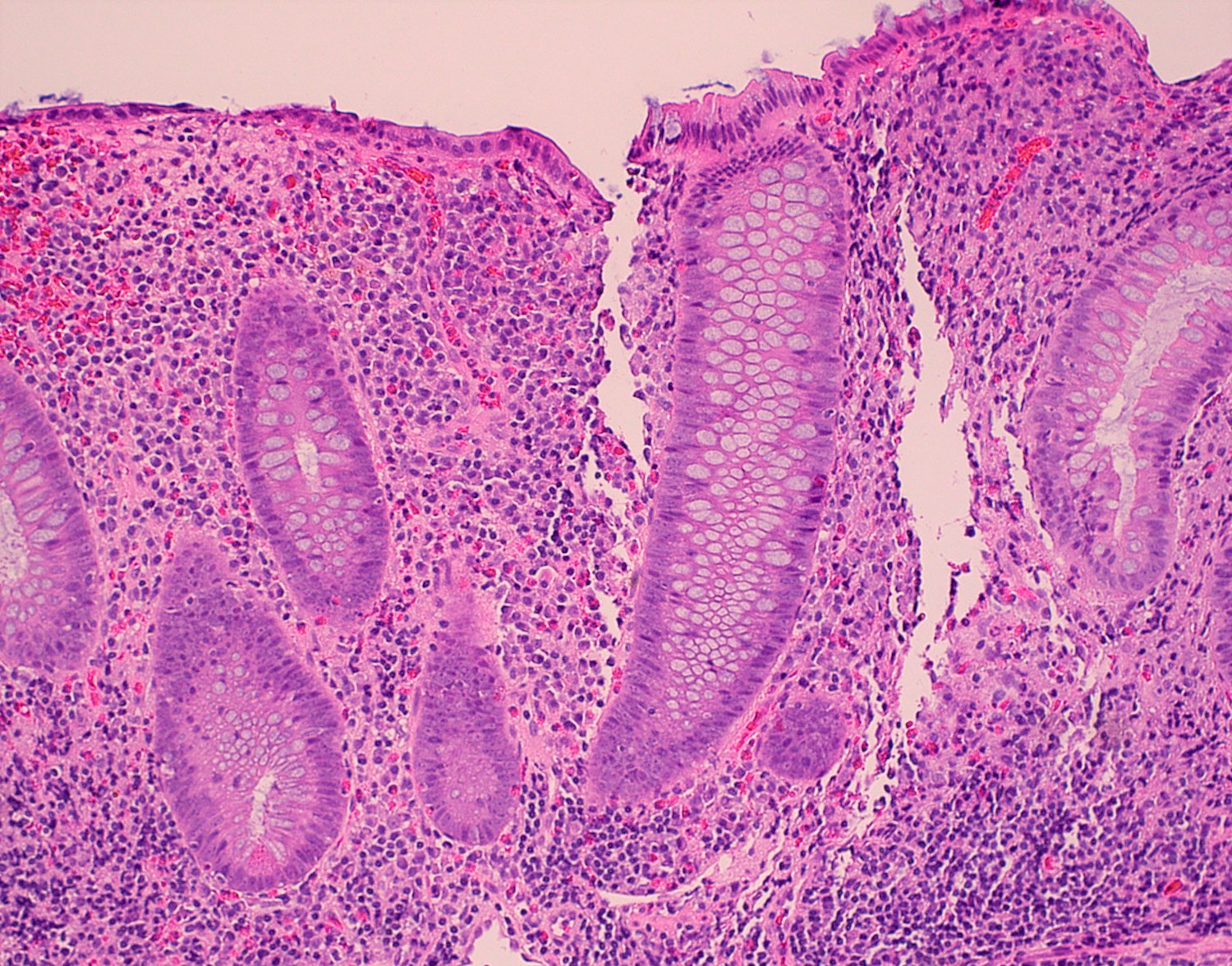
Microscopic (histologic) description
- Inflammation of lamina propria (active much more than chronic), edema, hemorrhage (Br Med J (Clin Res Ed) 1984;289:270)
- Usually lacks features of chronicity:
- Crypt architectural distortion
- Basal lymphoplasmacytosis
- Pyloric gland metaplasia
- Paneth cell metaplasia in the left colon
- Neutrophil induced epithelial injury (cryptitis or crypt abscess)
- Severe cases have crypt abscesses, extensive necrosis, hemorrhage and microthrombi
- Over time, neutrophils disappear (within second / third weeks) with persistent monocytic infiltration
- Colonic lymphocytosis can be seen in resolving phase
- Epithelial vacuolization, nuclear disarray, lymphocytosis, intranuclear inclusion can be seen in viral etiologies
Sample pathology report
- Colon, cecum, endoscopic biopsy:
- Active colitis (see comment)
- Comment: The cecal biopsy shows colonic mucosa with a variable degree of crypt architectural distortion and neutrophil mediated epithelial injury, diagnostic of active colitis. No granulomas or evidence of dysplasia is identified. The findings are nonspecific and may be seen in the setting of intestinal infection, medication / drug associated injury and idiopathic inflammatory bowel disease. Definitive diagnosis will require synthesis of all available clinical, endoscopic, radiologic and pathologic evidence.
Differential diagnosis
- Inflammatory bowel disease:
- Chronic mucosal injury, crypt distortion, basal lymphoplasmacytosis, pyloric gland metaplasia (Cureus 2017;9:e1817)
- Irritable bowel syndrome:
- Type of functional gastrointestinal disorder
- These problems cause the digestive tract to be very sensitive and change how the bowel muscles contract; the result is abdominal pain, diarrhea and constipation (Inflamm Bowel Dis 2018;24:2479)
- Adverse drug reaction:
- Apoptosis and intraepithelial lymphocytosis could be observed
Additional references
Practice question #1
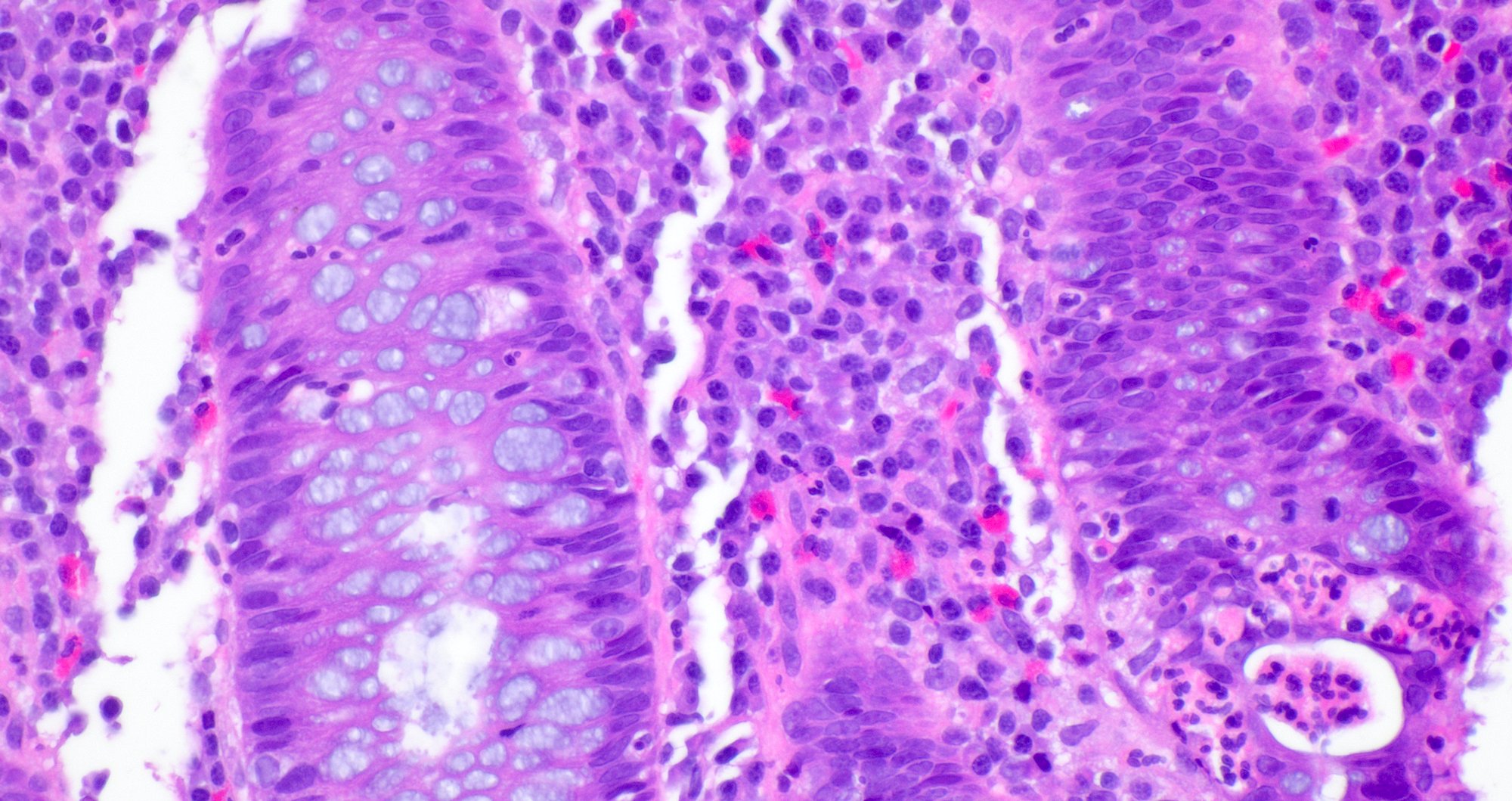
A 35 year old, previously healthy female complained of right lower abdominal pain and intermittent diarrhea. The clinical impression was acute appendicitis. An appendectomy was performed. Grossly, the appendix appeared normal. Histologically, there was patchy chronic and acute inflammation as shown in the image above. Which of the following statements about this infection is correct?
- A patient with this infection is likely to die within 6 months
- Long term antibiotics are the treatment of choice in this patient
- The patient most likely has a colitis and requires supportive therapy
- This infection may be disseminated and tests to discover additional foci are mandatory
Practice answer #1
C. The patient most likely has a colitis and requires supportive therapy. This patient most likely has CMV colitis demonstrated by nuclear and cytoplasmic inclusions, commonly referred to as owl eye inclusions, which are Cowdry type A inclusions. CMV colitis can mimic chronic idiopathic inflammatory bowel disease, graft versus host disease and acute appendicitis.
Comment Here
Reference: Acute self limited colitis
Comment Here
Reference: Acute self limited colitis
Practice question #2
Paneth cell metaplasia is an indicator for chronic mucosal injury in which part of the colon?
- Ascending colon
- Cecum
- Sigmoid colon
- Terminal ileum
- Transverse colon
Practice answer #2
C. Sigmoid colon. Paneth cells are normally absent in the left colon. When present, they serve as an indicator for chronic mucosal injury. However, Paneth cells are normally present in the right colon; hence, sigmoid colon is the correct choice. If Paneth cell metaplasia is seen in the sigmoid colon, this is an indicator for chronic mucosal injury.
Comment Here
Reference: Acute self limited colitis
Comment Here
Reference: Acute self limited colitis