Table of Contents
Definition / general | Essential features | Terminology | General methods of dissection | Cardiac dissection | Dissection of the brain | Vertebral artery dissection (in situ or en bloc removal) | Dissection of superior vena cava, subclavian and jugular veins | Dissection of lower limbs and pelvis for deep vein thrombosis | Removal of the orbital contents | Dissection of the middle ear | Facial dissection | Layer by layer neck dissection | Demonstration of pneumothorax | Demonstration of gas embolus | Dissection of biliary tract | Subcutaneous dissection of trunk and limbs for occult bruising | Subcutaneous dissection for intravenous needle marks | Speculum examination and pelvic exenteration for sexual assault | Clinical images | Gross images | Videos | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Hulme K, Spark A. Autopsy techniques. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/forensicsautopsytechniques.html. Accessed September 16th, 2025.
Definition / general
- Autopsy techniques refer to the manner in which an autopsy is performed in order to assess the body externally and internally to identify the cause and circumstances of death
- Techniques vary based on the training and experiences of the autopsy practitioner and the particulars of the case
Essential features
- Incisions must provide ready access to the site of interest while offering an opportunity for excellent reconstruction
- General methods of autopsy vary and may include the removal of organs individually or en masse with subsequent dissection
- Specific dissections may be required depending on the circumstances of death and autopsy findings; techniques vary by autopsy practitioner and some cases may benefit from subspecialist referral
Terminology
- Postmortem examination techniques
General methods of dissection
- Prior to autopsy
- Follow local standards regarding patient identification and written consent by first of kin (for clinical autopsy)
- Full 3 cavity examination
- Limited to particular areas
- External / noninvasive only (which may allow radiology and taking of samples via a needle)
- Summarize information as available regarding the circumstances of death, if known, including any past medical, occupational and social history, in order to determine the autopsy techniques most likely to yield answers
- Determine if the presence of police or other specialists (e.g., forensic dentists) is needed
- Determine whether radiology will assist the autopsy (Forensic Sci Res 2022;7:385)
- Follow local standards regarding patient identification and written consent by first of kin (for clinical autopsy)
- Complete external examination
- Primary skin incisions
- Anterior body wall incisions
- Y shaped: most common and with excellent reconstruction results
- T shaped
- I shaped or vertical
- Scalp
- Coronal incision in an adult provides ready access for the removal of the crown with excellent reconstruction results as it is behind the hairline
- Anterior body wall incisions
- General autopsy methods
- Letulle
- Organs removed en mass and subsequently dissected
- Best for observing the pathological and anatomical relationships of structures
- Produces a large, bulky mass with which to work
- In brief
- After opening the body, remove the distal duodenum to the rectum and dissect the pelvic organs away from the body wall
- Transect the iliac vessels
- Free the diaphragm then the retroperitoneal organs (bluntly dissect and pull the kidneys forward) from the body wall around each side to the vertebra
- Free the neck structures anterior to the cervical vertebrae moving upward to stop once the tongue is free
- Use the tongue (being wary of damaging the larynx) to strip the organs downward off the vertebrae anteriorly to remove the organs en masse
- Organs are then usually examined sequentially from the posterior aspect
- Ghon
- Organs removed as organ blocks and subsequently dissected
- Thoracic, coeliac, intestines and urogenital system blocks
- In brief
- Free the tongue as described for Letulle and strip the organs downward off the vertebrae anteriorly stopping at the lower esophagus
- Transect the esophagus and descending aorta at this level and remove the thoracic block
- Tie and cut the duodenal / jejunal junction then the rectum
- Work from one end of the bowel to the other, cutting across the mesentery close to the bowel wall to remove the intestines en bloc
- Remove the rest of the abdominal organs with a method similar to Letulle
- Virchow
- Organs removed from the body and inspected one by one (Virchow: Post-Mortem Examinations, With Especial Reference To Medico-Legal Practice, 1880)
- In brief
- After opening the body, inspect the abdominal contents and the pleural cavities
- Open the pericardium and remove the heart, followed by each lung
- Assess the neck (pharynx, larynx, parathyroid glands, thyroid gland) and remaining organs in the thorax (predominantly the esophagus)
- Move to the abdomen and remove the spleen, intestines, liver and pancreas
- Open the stomach in situ
- Remove the kidneys and adrenal glands from the retroperitoneum, tracing the ureters to the bladder
- Remove the pelvic organs
- Inspect and open the large arteries and veins in the abdomen and pelvis
- Rokitanksy
- Debated as to the exact original technique
- Organs inspected and incised in situ
- Considered to provide less information
- Of benefit if there is a highly transmissible disease
- In reality, each autopsy practitioner performs their own modified autopsy technique depending on their training, experiences and the particulars of the case
- All autopsies require thorough documentation of positive findings and relevant negative findings including the taking of photographs (with visible identifiers and scale)
- Letulle
- After autopsy
- Consider further investigations
- Histology
- Blood spot card (previously known as a Guthrie card)
- Biochemistry
- Microbiology
- Virology
- Toxicology
- Genetics
- Other
- Summarize information to determine the provisional cause of death
- Compile histology and other investigation results into final report, completed at a later date
- Consider further investigations
Cardiac dissection
- See Forensic heart dissection
- Standard line of flow
- Indicated in all autopsies due to the prevalence of cardiac causes of sudden natural death in all ages and to rule out its contribution in unnatural deaths
- Heart is usually separated from the body at the level of the transverse pericardial sinus allowing for several centimeters of aorta and pulmonary artery above the respective valves and intact atria; care must be taken to assess for major aberrant anatomy when separating the heart from the body
- Several methods exist for organ dissection, most commonly the major named coronary arteries are first assessed for aberrant anatomy and disease
- Arteries can be opened longitudinally or transversely, the latter being regarded as more accurate
- Assessment frequently requires decalcification, which can be completed on already sectioned arteries or on a whole artery (later sectioned)
- Next, the ventricles are sliced perpendicular to the interventricular septum (IVS) from the apex to the level of the midpapillary muscle
- Right atrium is opened and inspected by cutting between the superior and inferior vena cava
- Cut is made opposite the septum from the atrium, through the tricuspid valve and through the right ventricle
- Cut is made on the anterior surface of the heart through the pulmonary valve
- On the left side of the heart, the atrium is opened by cutting between 2 pulmonary veins
- Cut is made opposite the septum from the atrium, through the mitral valve and through the left ventricle
- Cut is made on the anterior surface through the aortic valve to inspect the valve and coronary ostia
- Measurements should include at a minimum the weight of the heart in total, size of each chamber, thickness of each wall and valve orifice
- Fulton technique is used for assessing ventricular hypertrophy and involves separating the left ventricle (including the IVS) from the right ventricle and weighing them separately to calculate a ratio, with 2.3 - 3.3:1 (LV:RV) being considered normal (Br Heart J 1952;14:413)
- Postsurgery (coronary artery bypass grafting [CABG], valve replacement, ascending aorta repair / replacement)
- Assessment is often made much more difficult by fibrous adhesions around the heart and metal stents
- Rarely, postmortem coronary angiography prior to autopsy may be indicated and compared to antemortem angiography
- If the surgery is recent or likely to be involved in the cause of death, it is critical to receive clinical notes including any operation reports
- With CABG, it is essential to study both the native and grafted vessels for patency and check the ostia
- Following valvular surgery, it is important to note the type of valve prosthesis as well as assess for any paravalvular leak, signs of thrombi or vegetations, degradation of the cusps or position of the components such that function would be affected
- Safe implantable cardioverter defibrillator (ICD) removal
- Consideration should be given for the removal of the device in a manner that avoids electric shock to the mortuary staff but enables data to be collected that may assist in determining the cause of death (J Forensic Sci 2022;67:1924, Circulation 2018;137:2730)
- Most mortuaries will have local management protocols available for safe removal; optimally, the device should be electronically inactivated by transcutaneous programming but this requires a device specific programmer
- ICD magnet placed over the device generator will disable all antitachycardia therapies as well as prevent electrical noise from being recorded by the device; if neither is available and delaying the autopsy is impossible, 2 layers of rubber or plastic gloves have been shown to provide sufficient protection in laboratory models (Europace 2009;11:1317)
- Once deactivated, free the generator from its subcutaneous pocket (identified by the scar from insertion) and use a wrench to unscrew the leads; this deactivates the ICD, which can then be sent to a cardiac physiologist for assessment
- Cardiac conduction system
- Indicated for deaths considered compatible with sudden cardiac death where no other cardiac cause has been identified
- Most commonly, the region of the atrioventricular node is dissected and assessed microscopically; the node is removed by opening the right atrium and ventricle and cutting out a square of tissue of the interatrial and IVS between the foramen ovale and coronary sinus, including the anterior leaflet of the tricuspid valve
- Sinoatrial node is less often dissected; the node is removed by opening the posterior surface of the superior vena cava (SVC) and cutting out a square of tissue around the junction of the SVC and the base of the right atrial appendage
- Consider involving a cardiac pathology specialist when complex cardiac problems are anticipated; they may prefer the heart fixed and sent whole or advise on additional investigations prior to review
Dissection of the brain
- Fixed versus unfixed
- Advantage of not fixing the brain prior to examination is that the return of the complete body is not delayed; a fixed brain provides the ability to complete an examination in finer detail with better photography and histology (including immunohistochemistry), which allows for better specialist neuropathological outcomes
- Weight should be taken and excess blood removed prior to fixation
- There are many methods to fix the brain
- It can be suspended upside down in a large bucket of 10% buffered formalin for at least 4 weeks; suspension methods include resting in a hairnet or with the basilar artery tied with string to the handles of the bucket
- Formalin should be intermittently replaced (an example routine would be after ~3 days, then every week); high strength formalin (37%) can be used
- Short fixation period (1 - 4 days) may be useful in some circumstances as a compromise (J Clin Pathol 2013;66:50, J Clin Pathol 2006;59:393)
- Special techniques and protective equipment are required for any brain that could harbor prion disease; mostly done in specialty departments with their own strict management protocol to reduce the risk of transmission to staff (J Clin Pathol 1993;46:193)
- Autopsy is still essential despite some value in postmortem radiology (PLoS One 2018;13:e0201434)
- In brief
- For routine work, the brain is removed from the skull, then the cerebellum and brain stem are separated from the cerebrum at the level of the midbrain
- Cerebellum is sectioned through the vermis then separated from the brain stem through the cerebellar peduncles
- Cerebellum is sectioned radially and the brain stem cranial to caudal
- Cerebrum is serially sliced into ~10 mm thick slices from anterior to posterior
- All slices are laid out in sequence for careful cleaning and then close inspection as abnormalities can be subtle
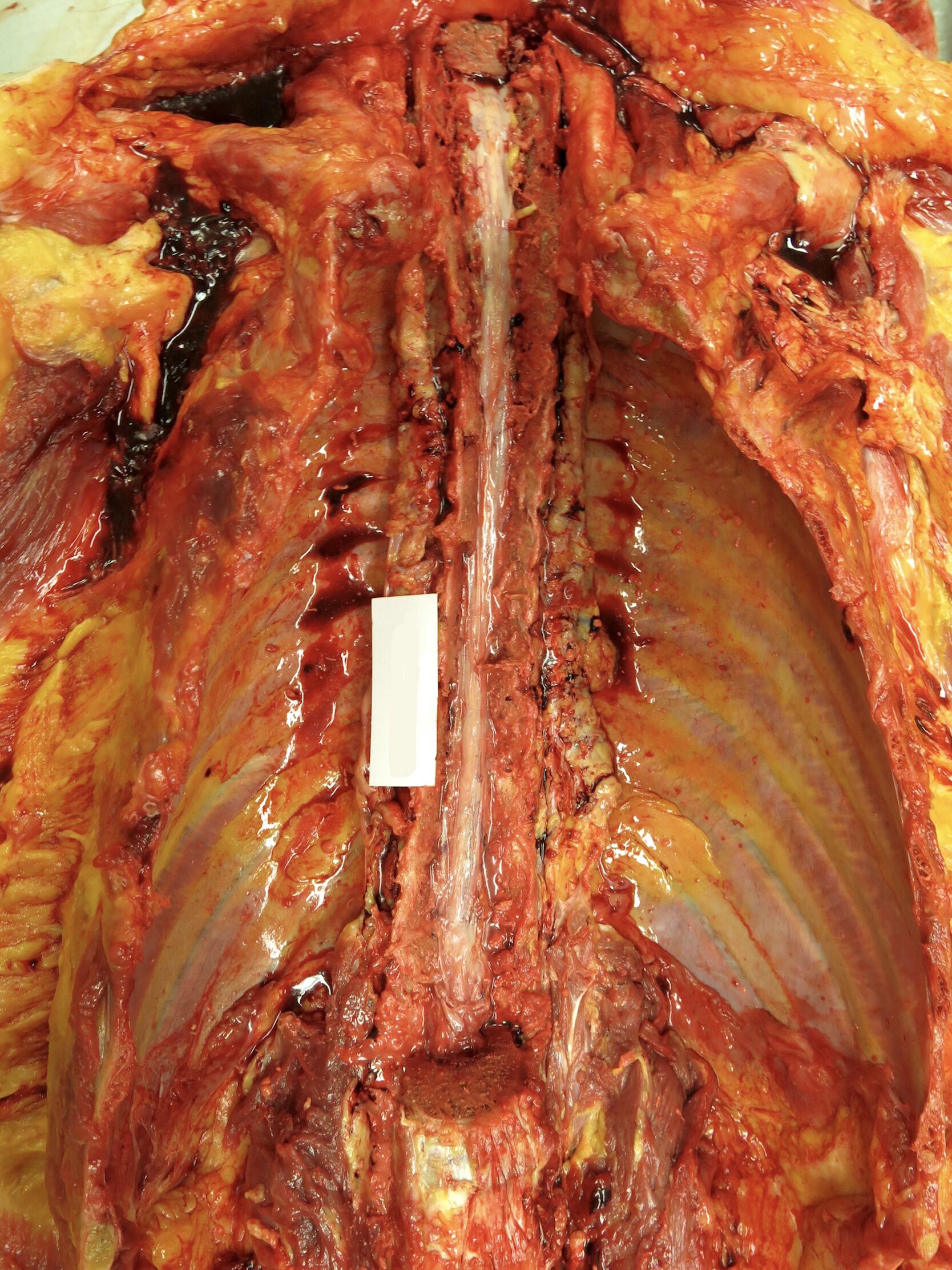
- Dissection of the arteries of the base of the brain
- Indicated for subarachnoid hemorrhage to identify aneurysm
- After the cerebellum and brain stem have been separated, the vessels of the circle of Willis and tributaries are lifted from the surface and penetrating small arteries are transected; leaving the transection of the most peripheral branches until all the central dissection is completed provides traction for easier dissection
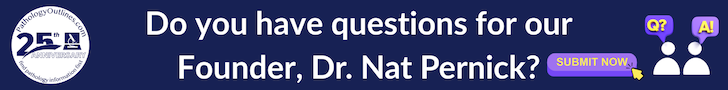
- Removal of the brain and spinal cord in continuity
- Posterior incision is made from the occiput to the coccyx and soft tissue is dissected away from the bone
- Oscillating saw divides both laminae throughout the spine and the posterior column of the spine is lifted
- Dura is opened to expose the spinal cord, which is then dissected free from its nerve roots
- Once the brain has been exposed in the usual manner, a wedge of occipital bone must be removed in order to free the cerebellum from its dura, after which the spinal cord can be delivered upward through the foramen magnum
- If only partial examination of the spinal cord is required or for other reasons, an anterior approach is performed, the spinal column can be accessed anteriorly after organ removal (see Clinical images and Gross images)
- Oscillating saw divides the pedicles of the vertebrae on both sides and the anterior column of the spine is lifted
- Dura is either opened to expose the spinal cord or left intact and removed with the spinal cord, which is then dissected free from its nerve roots and removed from the spinal canal
- If the spinal cord taken is longer than several vertebrae, it is best fixed suspended by its caudal end to prevent it from curling
- See Gross images
Vertebral artery dissection (in situ or en bloc removal)
- Indicated for circumstances of death suggestive of arterial injury, such as relatively minor neck trauma (e.g., sport, osteopathic manipulation, low speed motor vehicle incident, fall from standing height, unilateral blunt force injury to the mandible) with delayed sudden death or stroke symptoms prior to death
- Consider postmortem angiography as a guide to a site of suspicion or as an alternative to dissection (Forensic Sci Med Pathol 2023;19:135)
- Dissection can involve removal of the entire cervical spine en bloc with subsequent fixation and decalcification before examination or in situ identification of the artery as it traverses from its origin in the thorax, through the lateral pedicles of the inferior cervical spine to the posterior elements more superiorly
- This latter dissection requires significant time and skill and has a high rate of iatrogenic injury; access is gained through a posterior neck dissection as detailed below (J Clin Pathol 2006;59:1000, J Forensic Sci 2012;57:212)
Dissection of superior vena cava, subclavian and jugular veins
- Indicated for investigation of trauma, origin of pulmonary embolus, upper limb venous obstruction or vasculitis
- SVC can be identified where it enters the right atrium once the breastplate has been removed; from here, the subclavian veins and internal jugular veins (IJV) can be traced and if indicated, opened longitudinally along their course
- Alternatively, the IJV can be identified at the time of neck dissection running in the carotid sheath (that also contains the vagus nerve and carotid artery)
Dissection of lower limbs and pelvis for deep vein thrombosis
- Indicated for investigation of trauma, origin of pulmonary embolus, lower limb venous obstruction or vasculitis
- Measure the widest part of both calves as part of external examination
- Several methods exist; one approach is made through a long vertical incision following the medial border of the tibia
- This incision is continued medially and horizontally at the level of the popliteal fossa superiorly and Achilles tendon inferiorly
- Skin and subcutaneous tissue is reflected
- Exposed calf muscle is removed and serially sectioned in the transverse plane to demonstrate the deep veins in cross section (Ann Vasc Dis 2016;9:15)
- Simpler method involves a transverse incision in the popliteal fossae, which can expose the veins in cross section; by milking the blood from the calf, any clots can be identified
- Large veins in the pelvis can be identified once the abdominal and pelvic organs have been removed; the common iliac vein will have been transected and the large veins can be opened longitudinally along their course both within the pelvis (internal iliac vein) and at their entry point through the femoral canal (external iliac vein)
Removal of the orbital contents
- Most commonly indicated in pediatric nonaccidental injury cases (Leg Med (Tokyo) 2003;5:S288)
- Do not aspirate vitreous humor prior to examination as the retina may be damaged
- Several methods exist
- One approach is to remove a flap of bone from the anterior cranial fossa with an oscillating saw; the orbital contents are carefully separated from the surrounding bone circumferentially both anteriorly to meet the conjunctiva and posteriorly to include the optic nerve
- Further dissection of the eye is best done after fixation in formalin (at least 48 hours is usually recommended)
- See Clinical images
Dissection of the middle ear
- Most commonly indicated for systemic sepsis of unknown cause
- Methods range from simple (but destructive) removal of the bone overlying the middle ear (tegmen tympani) to en bloc removal of the middle ear requiring decalcification prior to sectioning with an oscillating saw
- One example is Cobbler's Cut technique (J Forensics Res 2014;5:2)
- For the simplest method, once the brain has been removed and dura stripped from the middle cranial fossa, chip the bone overlying the middle ear off with a chisel; the area of interest is located posterior and lateral to the foramen spinosum (transmits the middle meningeal artery) and anterior to the ridge of the petrous temporal bone
- This will provide access to sample any fluid for microbiology but fine anatomical detail will be lost
- See Clinical images
Facial dissection
- Each part of a postmortem should be considered as essential to justify its intrusiveness; therefore, one must weigh the value of facial dissection versus the ability to reconstruct the face or compromise the embalmer's ability to access facial vessels, especially given the value of postmortem radiology
- Most commonly indicated for assessing trauma to the face
- Standard Y incision of the anterior body can be used by continuing to reflect the skin and subcutaneous tissue with the skin carefully reflected upward, exposing the face; alternatively, a high Y incision can be used
- Depending on the level of inspection required, examination can be limited to the bones of the jaw and facial skeleton, leaving the oral mucosa attached and without breaching the oral cavity; alternatively, it can be extended further upward (including the removal of the eyes in continuity allowing for examination of the bony eye sockets) if necessary
Layer by layer neck dissection
- Complete after brain and thoracic organs have been removed to reduce pressure within blood vessels that may lead to artefactual bleeding within tissues (Acad Forensic Pathol 2016;6:45)
- Anterior approach is commonly done in daily practice to assess injury to the neck structures, including if sustained pressure to the neck as a cause of or contributor to death (see Asphyxia)
- Similar to facial dissection, the standard Y incision of the anterior can be utilized by continuing to reflect the skin and subcutaneous tissue upward, exposing the neck; alternatively, a high Y incision can be used
- Then, each layer of muscles (platysma, then sternocleidomastoid, then the strap muscles) is separated at their caudal attachments and reflected upward for assessment
- IJV and common carotid arteries can then be opened longitudinally to assess for intimal tears
- Tongue and neck are then removed en bloc for further dissection
- Precervical fascia and underlying cervical spine can now be seen and any abnormalities are exposed
- Tissue bloc is further assessed on the bench by opening the cervical esophagus posteriorly, separating the thyroid for further sectioning, completely separating and stripping the hyoid bone for close inspection (and photography) and opening the larynx
- Document (including photographs) any surface or tissue hemorrhage, deformation or fractures in any structures; the interpretation of possible injuries can be controversial and should be approached with caution (Acad Forensic Pathol 2016;6:45)
- Posterior approach is used to document injury to the soft tissues of the back of the neck including subcutaneous bruising or to access to the vertebral arteries in the upper cervical vertebrae (as described above); several methods exist (Kitulwatte: Dissection Technique of the Posterior Neck and Vertebral Arteries [Accessed 16 June 2023])
- One approach is with an inverted T incision with the horizontal aspect extending over the scapula
- After the skin and subcutaneous tissue are reflected, the muscle groups can be reflected laterally; these muscles are typically divided into superficial (trapezius), intermediate (splenius capitis, splenius cervicis and semispinalis capitis) and deep (deep paraspinal and deep subcapital muscles) groups
- Once removed, the extracranial vertebral artery and spinous processes of the atlas and axis will be seen along with the important atlantoaxial and atlantooccipital ligaments
- See Clinical images
Demonstration of pneumothorax
- Usually well visualized on postmortem radiology (Leg Med (Tokyo) 2016;18:25)
- Once the subcutaneous tissues have been reflected from the anterior thorax, create a pool of water inside the pocket formed between the reflected tissues and lateral chest wall
- Insert an instrument underneath the water surface between the ribs and into the pleural space; if gas is released under pressure, a pneumothorax could be considered
- In the setting of a limited postmortem, a needle thoracostomy is performed similarly to those done with live patients (a large needle attached to a 50 mL syringe partially filled with water and aspirated in the second intercostal space midclavicular line in a supine patient) and could yield evidence for the presence of a pneumothorax
- Decomposition can produce gas in the chest so care must be taken in the interpretation of gas released in this setting
- Findings should be considered along with other signs of clinically significant pneumothorax, such as circumstances of death and other autopsy findings including mediastinal shift, hemithorax volume changes and lung bullae
Demonstration of gas embolus
- Indicated for pulmonary barotrauma / cerebral artery gas embolism (PBT / CAGE) diving fatality where there has been a rapid ascent and rapid loss of consciousness after resurfacing; venous air embolism may occur secondary to trauma, iatrogenic causes (intravenous lines, cardiopulmonary bypass, neurosurgery or gas assisted surgery or endoscopy), childbirth, abortion or rarely from criminal intervention
- For a diving fatality, postmortem imaging must be completed within 8 hours of death due to decomposition or off gassing
- Off gassing is where nitrogen that has been absorbed into the tissues with diving forms bubbles in the tissues and vessels if the diver ascends rapidly and dies or dies on the bottom and is rapidly brought to the surface
- This will result in gas artifact that is difficult to differentiate from pulmonary barotrauma and cerebral air gas embolism as a cause of death (J Clin Pathol 2006;59:489)
- For demonstration of gas in the heart, the anterior pericardium is carefully opened and the pericardial space is filled with water; the right and left ventricles are penetrated under the water's surface to assess for the presence of gas
- In order to be sure not to disturb the great vessels, the upper third of the sternum can be left intact until the testing is completed (Ulus Travma Acil Cerrahi Derg 2019;25:311)
- Significant venous air embolism is ~100 - 250 mL but is much less when arterial
- Demonstration of gas in the cerebral circulation is best seen with postmortem radiology prior to dissection as artefactual introduction of gas into the cerebral vessels is common
- Bubbles within the vessels of the circle of Willis and deep arteries of the brain might provide evidence for nonartefactual cerebral gas if the brain has been removed after careful clamping of both of the internal carotid and vertebral arteries; however, this is fraught with difficulty and should be interpreted with caution (Am J Forensic Med Pathol 2018;39:61)
- Gas can be produced during tissue decomposition, so care must be taken with the interpretation of gas in this setting
Dissection of biliary tract
- Indicated for checking the patency of the biliary system in the setting of malignancy, systemic sepsis, trauma or after adjacent abdominal surgery
- Several methods exist
- Can be dissected with the organs in situ or from the posterior aspect after the abdominal organs have been removed as a block
- One approach identifies the ampulla of Vater in the duodenum, which is then probed and opened longitudinally to its insertion into the gallbladder and common bile duct
- May be aided by the cannulation of the biliary system and injection of dye (such as methylene blue) or with the assistance of a suitably experienced surgeon
Subcutaneous dissection of trunk and limbs for occult bruising
- Commonly indicated in cases of homicide for evidence of blunt force injury to determine age of injuries as circumstances of death
- Possible bruising should be sampled for histology to confirm
- Reflection may be done in layers, with sequential reflection of the skin, fat and muscles
- Routine anterior body incision will enable assessment of the anterior trunk
- Posterior trunk can be dissected through a midline posterior longitudinal incision, which can be carried over the back of the buttocks if limb examination is also required
- Limbs should have a longitudinal incision on the posterior surface for best reconstruction results (Forensic Sci Int 2018;284:85)
- Photography of bruising may be enhanced with ultraviolet light
Subcutaneous dissection for intravenous needle marks
- Curved skin incision is made around the area with the needle puncture mark and the skin and subcutaneous fat are reflected to demonstrate the underlying vessel
- In some cases, the puncture mark is obvious (marks may be hidden by cigarette burns or tattoos) and macroscopic assessment of the perivascular tissues for fibrosis can be made
- Cross sections of the vessel and adjacent soft tissue can be submitted for histology and surrounding subcutaneous tissues sent for toxicological testing
- If sending tissue for toxicology, control specimens should be taken from the opposite side of the body and sent in a separate container
- See Clinical images
Speculum examination and pelvic exenteration for sexual assault
- Consider involving the local jurisdiction specialist in sexual assault to attend the autopsy to assist with interpretation of possible injuries and the taking of samples
- Prior to any instrumentation or dissection any samples needed for evidentiary purposes (sexual fluids or DNA) must be taken to avoid potential contamination (Acad Forensic Pathol 2018;8:912)
- Lithotomy position may assist in examination and dissection
- Speculum examination is completed as per the local jurisdiction protocols for sexual assault and is similar to that completed on a live victim
- Several methods exist for the dissection of the vagina / rectum
- Traditionally, the routine anterior body incision is continued inferiorly to pass over the pubic symphysis and surround the vagina / rectum
- Pubic bones are sawed through ~5 cm on either side of the pubic symphysis and the tissues are separated away from the inner surface of the pelvic brim until the pelvic contents can be removed en bloc
- Tissue is fixed in formalin before dividing in the sagittal plane for assessment of the vagina / rectum
- This pelvic exenteration is disfiguring and consideration should be given to less invasive approaches where possible
- Less destructive technique involves making an elliptical incision around the external genitalia, meeting anteriorly to the clitoral hood anteriorly and posteriorly to the anus posteriorly, extending laterally at approximately the level of the labia majora
- This incision is continued into the deep pelvic tissues, following the contours of the inner aspect of the pelvis, to eventually communicate with the abdominal cavity; the entire tissue block including anus to rectum and vagina to uterus and ovaries can then be removed
- Lateral incisions from the anus to the cut end of the rectal stump and from the vagina, through the cervix and through the uterus can then be made and the entirety of the genital tract examined for injury
- Bladder is also opened and inspected
Clinical images
Gross images
Videos
Opening of the skull and removal of the brain
Removal of the orbital contents
Full body autopsy, including the brain, with modified Virchows technique
Simple method to check patency of the biliary system
Dissection of the heart (after separation from the body)
Additional references
Practice question #1
Practice answer #1
B. Removal of the brain and thoracic organs. This is important to complete before performing a layered anterior neck dissection to reduce the pressure within the blood vessels and prevent any resultant artefactual bleeding. Answers A, C and D are incorrect because facial dissection, removing the cervical spinal cord and sampling vitreous fluid do not reduce the pressure within the blood vessels of the neck.
Comment Here
Reference: Autopsy techniques
Comment Here
Reference: Autopsy techniques
Practice question #2
Which of the following statements is correct in regard to trying to demonstrate gas embolus as a cause of death?
- 20 mL of air removed from the right ventricle can be considered as definitely causing death
- Any bubbles within the circle of Willis can be considered as definitely causing death
- Consideration of the interval between death and postmortem is unimportant
- For a diving fatality, postmortem imaging must be completed as soon as possible but definitely within 8 hours
Practice answer #2
D. For a diving fatality, postmortem imaging must be completed as soon as possible but definitely within 8 hours. This is critical for minimizing potential gas artifact caused by decomposition or off gassing. Answer B is incorrect because artefactual introduction of gas into the cerebral circulation during postmortem is common and this finding should be interpreted with caution. Answer A is incorrect because most pathologists would consider a significant venous air embolism in the heart to be of a much greater volume than 20 mL. Answer C is incorrect because decomposition produces gas so the larger the interval between death and postmortem, the more likely that gas identified within blood vessels is artificial.
Comment Here
Reference: Autopsy techniques
Comment Here
Reference: Autopsy techniques