Table of Contents
Definition / general | Essential features | Physiology | Diagrams / tables | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Cordeiro-Rudnisky FC, Assarzadegan N. Anatomy, histology & embryology. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/gallbladderhistology.html. Accessed September 14th, 2025.
Definition / general
- The gallbladder is a pear shaped saccular organ connected to the extrahepatic biliary system via the cystic duct
Essential features
- Gallbladder wall is 1 - 2 mm thick and composed of mucosa, muscularis propria and serosa
- No muscularis mucosae or submucosa is present
- With the exception of the common bile duct and the cystic duct at the junction with the gallbladder, the extrahepatic bile ducts do not have a muscle layer
Physiology
- Gallbladder:
- Pear shaped saccular structure located on the inferior surface of the right hepatic lobe
- Wall thickness: 1 - 2 mm
- Composed of fundus, body and neck
- Distal fundus: extends beyond the anterior liver margin
- Central body: most of the gallbladder
- Neck: narrows as it joins the cystic duct
- Extrahepatic biliary tree:
- Right and left hepatic ducts:
- Join to form common hepatic duct (CHD) in the porta hepatis (hilum of liver)
- Common hepatic duct:
- Joins cystic duct to form common bile duct
- Cystic duct:
- Connects gallbladder to common hepatic duct (CHD)
- Has spiral valve of Heister (mucosal folds that avoid collapse)
- Common bile duct:
- Results from the fusion of CHD and cystic duct
- 2 - 9 cm long; passes posterior to the first portion of duodenum, traverses the head of pancreas, enters the second part of duodenum through the ampulla of Vater and discharges gallbladder contents into the duodenal lumen
- 60% of the population have common channel for pancreatic duct and common bile duct
- Remainder of the population have 2 ducts in parallel
- Right and left hepatic ducts:
- Gallbladder stores and releases bile
- Gallbladder empties into cystic duct, which connects it to the extrahepatic biliary tree
- Extrahepatic biliary tree serves as conduit for bile flow
- Bile excretion is normally 500 - 1000 mL/day
- Bile is concentrated 5 - 10x via active absorption of electrolytes accompanied by passive movement of water
- Cholecystokinin causes gallbladder contraction and release of stored bile into the gut
- Bile is critical for intestinal absorption of dietary fat but the gallbladder is not
- Bile is 66% bile salts, is bicarbonate rich and has 3% organic solutes
- 95% of secreted bile salts are reabsorbed in the ileum and are subsequently returned to the liver via portal blood (called enterohepatic circulation of bile salts)
- Cholesterol is eliminated via loss of 0.5 g of bile salts per day
- Bile salts:
- Cholates, chenodeoxycholates, deoxycholates, lithocholates, ursodeoxycholates
- Major hepatic products of cholesterol metabolism
- Family of water soluble sterols with carboxylated side chains
- Highly effective detergents, solubilize water insoluble lipids secreted by the liver (usually lecithin) into the biliary tree and promote dietary lipid absorption within the gut
- Lecithin (phosphatidylcholine):
- Hydrophobic, nonaqueous
- Has minimal solubility in water
Diagrams / tables
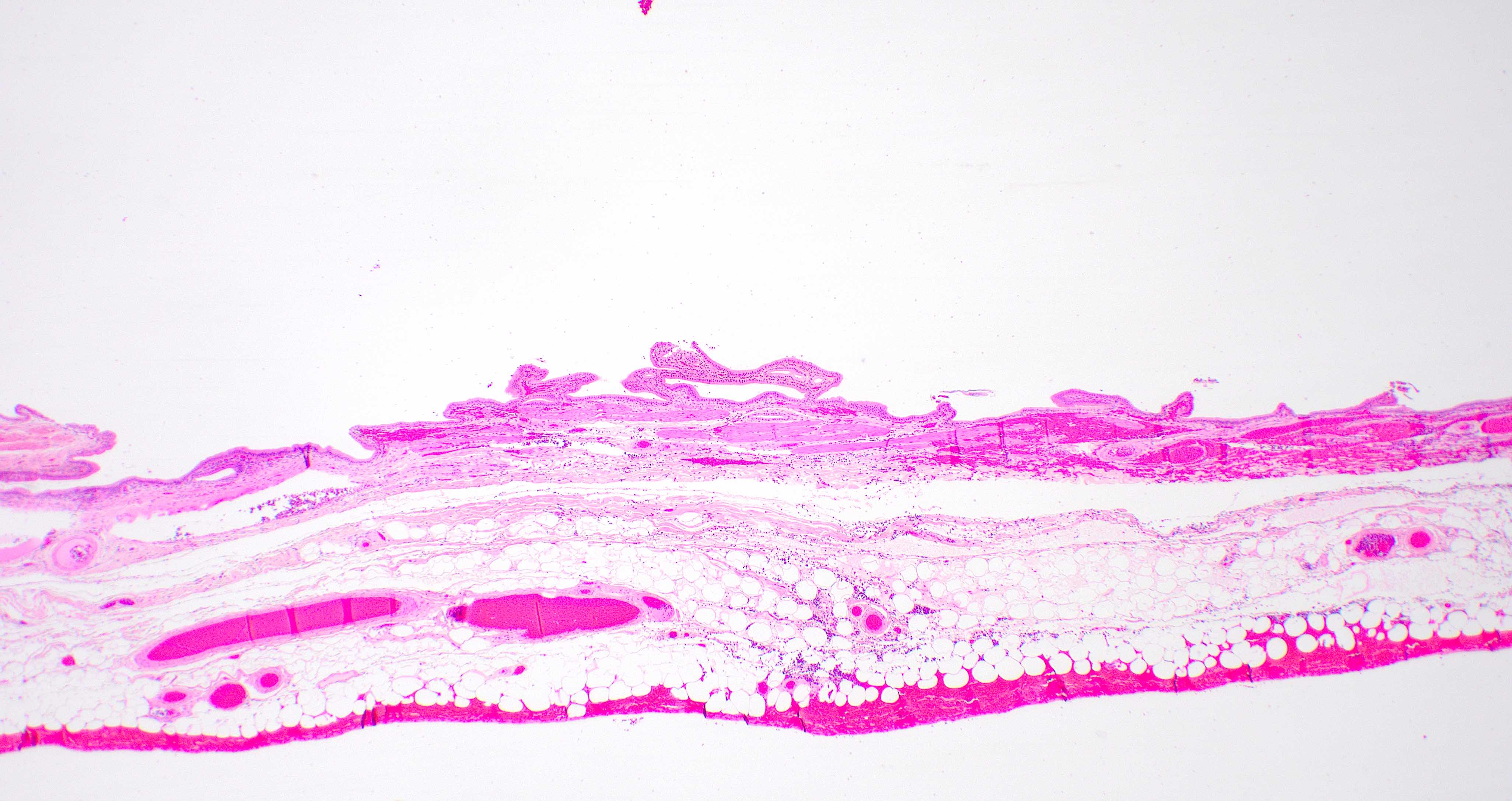
Microscopic (histologic) description
- Gallbladder:
- Microscopic layers: mucosa, muscular wall, perimuscular subserosal connective tissue and serosa; muscularis mucosae and submucosa are not present
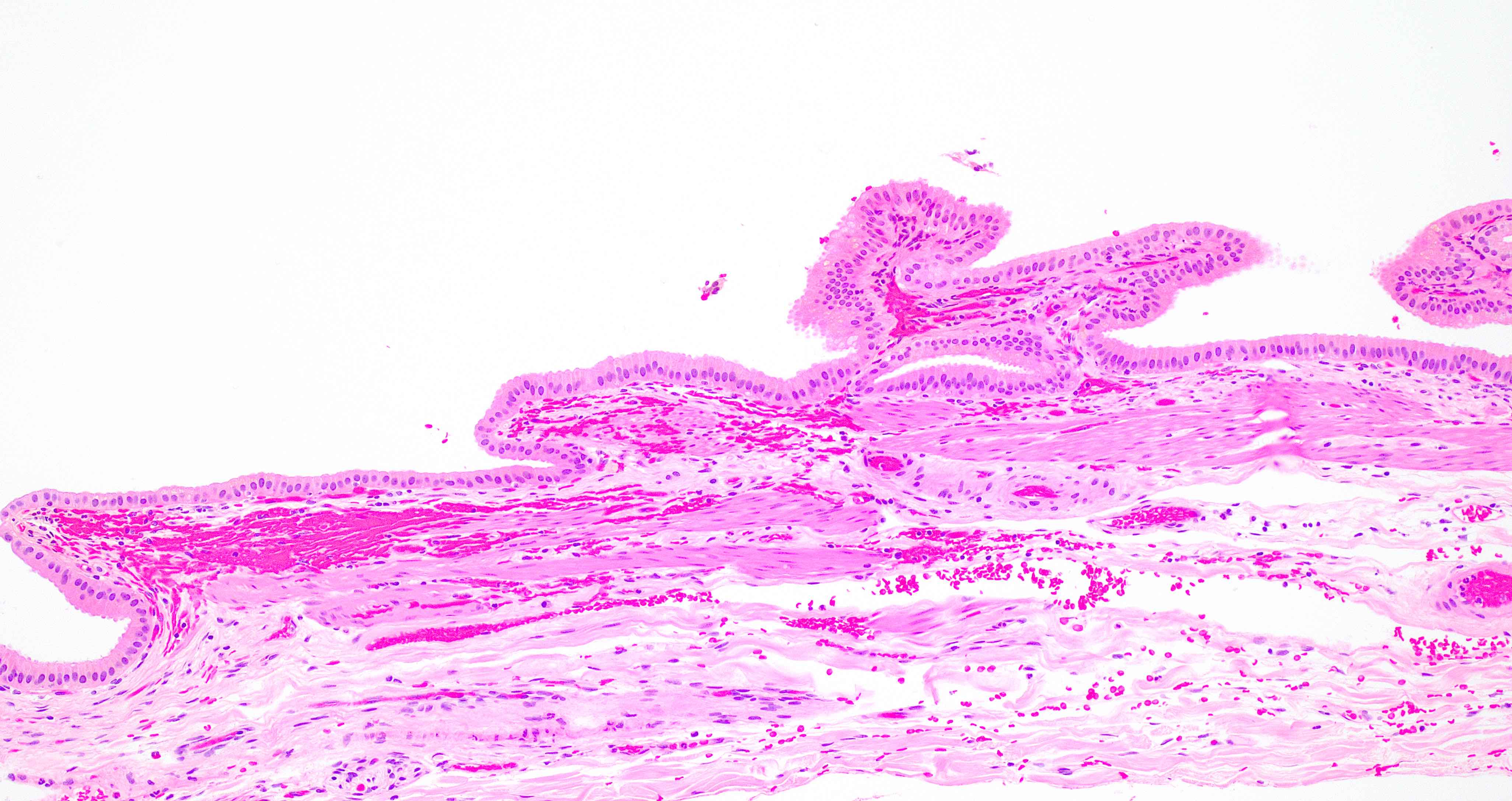
- Mucosa:
- Branching folds composed of surface epithelium and lamina propria
- Cores of lamina propria are lined by a single layer of columnar epithelial cells
- Epithelial cells have eosinophilic cytoplasm with variably present apical vacuoles; nuclei are basally oriented, oval and uniform, with inconspicuous nucleoli
- There are also inconspicuous scattered basal epithelial cells located above the basement membrane
- Tubuloalveolar mucus glands are present only in the neck region; true glands are not present outside the neck in normal gallbladder
- Goblet cells are not present in normal gallbladder epithelium
- Lamina propria is composed of loose connective tissue, blood vessels and lymphatics; few lymphocytes, plasma cells, mast cells and histiocytes are usually present (Mills: Histology for Pathologists, 3rd Edition, 2007)
- Muscular wall:
- Loose bundles of smooth muscle fibers without well formed distinct layers
- Resembles muscularis mucosae
- Adjacent to lamina propria without an intervening submucosa
- Perimuscular subserosal connective tissue (adventitia):
- Perimuscular connective tissue composed of collagen, elastic tissue, fat, vessels, lymphatics and nerves
- May contain lymph nodes and paraganglia
- Serosa:
- Peritoneum covers the portion of gallbladder that is not connected to the liver
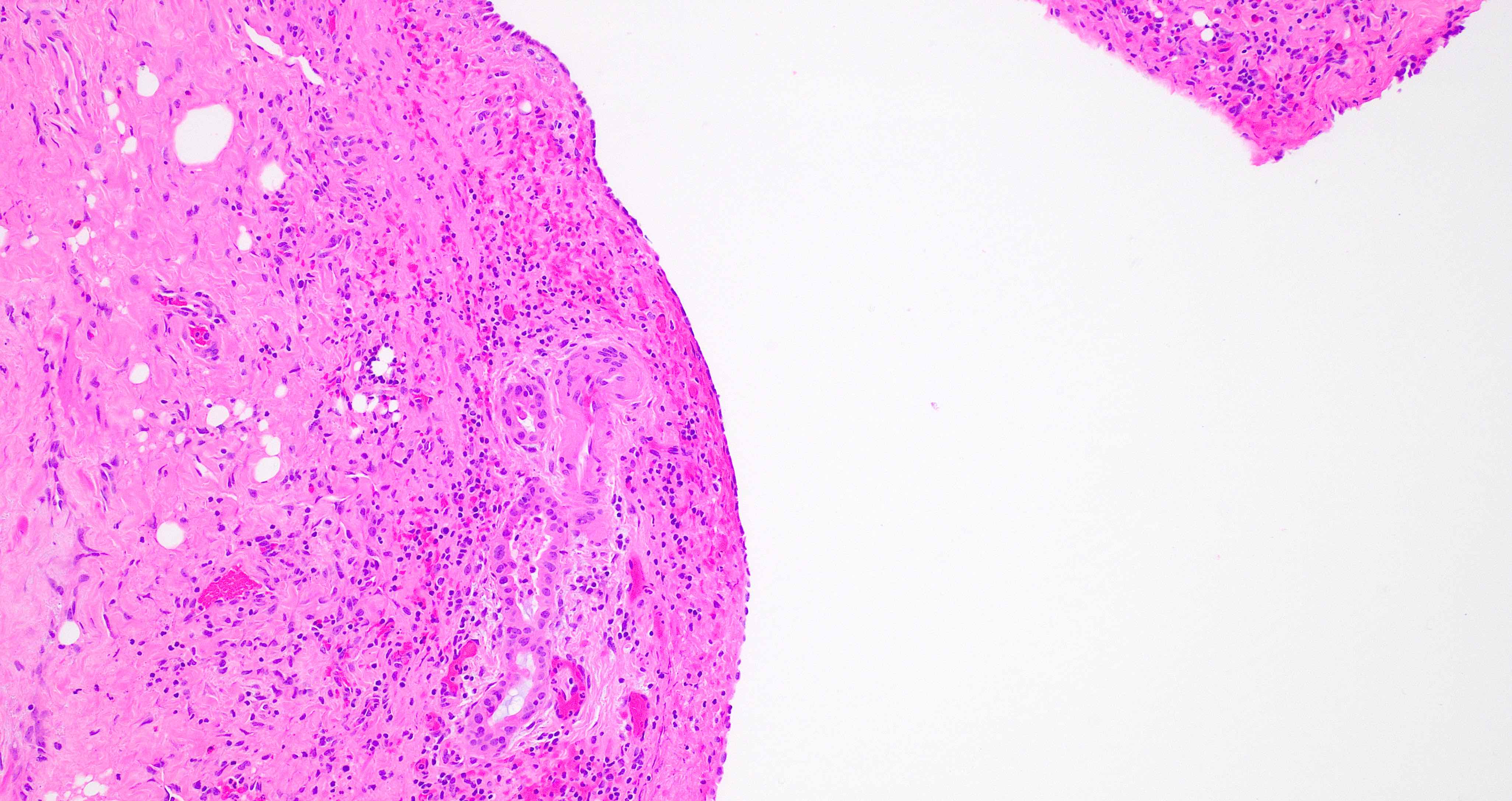
- Aberrant bile ducts (ducts of Luschka):
- Present in 10% of cholecystectomy specimens, often buried in gallbladder wall adjacent to liver, may contain a collar of fibrous tissue, may communicate with intrahepatic bile ducts
- Histologically composed of lobular aggregates of small ductules lined by bland cuboidal to columnar biliary type epithelium (Am J Surg Pathol 2011;35:883)
- Rokitansky-Aschoff sinuses:
- Outpouchings of gallbladder mucosa that penetrate the muscle wall
- May be acquired herniations
- Ectopic or heterotopic tissue:
- Variety of ectopic tissues can be found in the gallbladder wall and biliary tract, namely liver, pancreas, adrenal, gastric, thyroid and cartilage, resulting in tumor-like lesions (Zimmermann: Ectopias and Heterotopies as Tumor-like Lesions of the Hepatobiliary Tract [Accessed 17 February 2022], Medicine (Baltimore) 2019;98:e18293, Case Rep Gastroenterol 2018;12:170, Cases J 2009;2:6786, Medicine (Baltimore) 2018;97:e0058)
- Endometriosis can also occur in the gallbladder wall and cause occult bleeding
- Extrahepatic bile ducts:
- Epithelial layer:
- Single layer of columnar cells with round, basally located nuclei
- Subepithelial stroma:
- Composed of fibroblasts, collagen, small vessels and scattered inflammatory cells
- Muscle layer:
- Present along the common bile duct and at the junction of the cystic duct and gallbladder
- Peribiliary connective tissue:
- Consists of adipose tissue, vessels, nerves and ganglion cells
- Epithelial layer:
- Peribiliary mucous glands:
- Considered a local progenitor cell niche in extrahepatic biliary epithelium (Liver Int 2012;32:554)
- Unevenly distributed within large intrahepatic ducts and all extrahepatic bile ducts
- Lobular architecture; are surrounded by fibroconnective tissue (important in distinguishing from well differentiated carcinoma)
Microscopic (histologic) images
Practice question #1
Which of the following is true about normal gallbladder and extrahepatic tree histology?
- Gallbladder lacks muscularis mucosae and submucosa
- Goblet cells are present in normal gallbladder epithelium
- Muscle layer is not present along the common bile duct and at the junction of the cystic duct and gallbladder
- Tubuloalveolar mucus glands are present throughout the entire gallbladder
Practice answer #1
A. Gallbladder lacks muscularis mucosae and submucosa, unlike any other luminal GI structure. Tubuloalveolar mucus glands are present only in the neck region. True glands are not present outside the neck in normal gallbladder. Muscle layer is present along the common bile duct and at the junction of the cystic duct and gallbladder. Goblet cells are not present in normal gallbladder epithelium.
Comment Here
Reference: Gallbladder & extrahepatic bile ducts - Anatomy, histology & embryology
Comment Here
Reference: Gallbladder & extrahepatic bile ducts - Anatomy, histology & embryology
Practice question #2
Practice answer #2
A. Benign Luschka duct. Luschka ducts are benign glands on the serosal aspect of the normal gallbladder. Note the bland cytology.
Comment Here
Reference: Gallbladder & extrahepatic bile ducts - Anatomy, histology & embryology
Comment Here
Reference: Gallbladder & extrahepatic bile ducts - Anatomy, histology & embryology