Table of Contents
Definition / general | Essential features | Physiology | Clinical features | Laboratory | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Immunohistochemistry & special stains | Electron microscopy description | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Layman AJ, Bois MC. Histology. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/hearthistology.html. Accessed September 14th, 2025.
Definition / general
- Specialized muscle cells, namely cardiomyocytes, allow for synchronized contractions to facilitate the pumping of blood throughout the body
Essential features
- Heart wall consists of 3 layers: endocardium, myocardium and epicardium
- Variation in the relative thickness of each of these layers exists between ventricles and atria, and between left and right sided chambers
- Myocardium is primarily composed of cardiac myocytes: specialized striated muscle cells organized in fascicles and bands
Physiology
- Heart serves as a pump that drives 2 parallel vascular circuits:
- Systemic circuit:
- Blood is ejected from the left ventricle through the aortic valve during systole at a normal pressure of 120 mmHg
- Blood travels through the ascending aorta, aortic arch and descending aorta; it then progresses through peripheral arteries, arterioles and eventually the systemic capillary beds, before entering the venous return
- Systemic venous blood returns to the right atrium from the superior and inferior vena cava at a pressure of < 5 mmHg
- Pulmonic circuit:
- Spontaneous contraction of the right atrium moves deoxygenated blood through the tricuspid valve to the right ventricle
- Ventricular contraction (systole) moves blood from the ventricle through the pulmonic valve to the pulmonary artery at a normal pressure of 25 mmHg
- Blood travels through the arteries and arterioles of the lung before reaching the alveolar capillaries
- Newly oxygenated blood returns to the left atrium via 4 pulmonic veins at a normal pressure of approximately 10 mmHg
- Left atrial contraction moves blood through the mitral valve into the left ventricle
- Coronary circulation
- The subendocardium is the last layer in the cardiac wall to receive blood flow from the coronary arteries and is most prone to ischemic injury
- Systemic circuit:
- The cardiac conduction system allows for coordinated atrioventricular contraction via the conduction of electrical impulses by specialized myocardial cells (J Interv Card Electrophysiol 2016;46:9)
- Sinoatrial (SA) node:
- Pacemaker of the heart located near the sinotubular junction, where the superior vena cava meets the right atrium
- Depolarization of the sinoatrial node cells allows for conduction of the electrical impulse through the conduction tracts within the wall of the right atrium:
- Posterior tract (Thorel tract)
- Middle tract (Wenckebach tract)
- Anterior tract (Bachmann bundle): extends to left atrium
- Depolarization also facilitates atrial contraction
- Atrioventricular (AV) node:
- Receives impulses from the sinoatrial nodal tracts, in order to propagate electrical cardiac impulse and facilitate ventricular contraction
- Located in the right atrium, in the space between the ostium of the coronary sinus, septal leaflet of the tricuspid valve and tendon of Todaro (Koch triangle) (Koch triangle)
- Bundle of His:
- Located in the membranous septum that separates the right atrium from the left ventricle
- Relays electrical impulses to the left and right bundle branches of the ventricular (muscular) septum
- Sinoatrial (SA) node:
Clinical features
- Clinical evaluation of cardiac structure and function is multifaceted and may include:
- Imaging:
- Echocardiogram
- Stress echocardiogram
- Xray / computerized tomography
- Cardiac MRI
- Coronary artery angiography
- Testing:
- Electrocardiogram
- Biopsy (see below)
- Serology (see Laboratory section)
- Imaging:
- Common cardiac pathology specimens include:
- Endomyocardial biopsy (J Clin Pathol 2006;59:121):
- Interventionalist uses a bioptome via an endovascular procedure, to sample endocardium and myocardium from the right ventricular septum
- Most common indication for endomyocardial biopsy is in the setting of transplant rejection monitoring
- In the appropriate clinical context, biopsies may also be used for the evaluation of heart disease, especially if there is concern for myocarditis, amyloidosis, hemochromatosis, drug toxicity or storage disorders
- Septal myectomy:
- Surgeon enters the left ventricle, either through the aortic valve (after aortotomy) or through the apical ventricular wall (ventriculotomy)
- Endocardium and myocardium are shaved for evaluation of septal abnormalities seen on echocardiogram
- Most common indication / etiology is hypertrophic cardiomyopathy but in the right demographic ruling out amyloidosis or storage disease is prudent
- Apical core resection: full thickness ventricular wall excision, allowing for placement of a ventricular assist device
- Atriotomy: normally excised for access to the heart chambers in a valve replacement procedure
- Atrial appendage: may be excised during procedures to replace heart valves, to reduce stroke risk in atrial fibrillation or for coronary artery bypass (Eur J Cardiothorac Surg 2018;53:i33)
- Orthotopic heart transplant
- Autopsy
- Endomyocardial biopsy (J Clin Pathol 2006;59:121):
Laboratory
- Serologic markers of acute coronary syndrome (UpToDate: Biomarkers of Myocardial Injury Other Than Troponin [Accessed 15 January 2021]):
- Troponin I / troponin T:
- Normal proteins present in myocardium which are released into systemic circulation following myocyte injury
- May remain elevated for up to 10 - 14 days post insult
- Creatinine kinase (CK / CK-MB):
- Enzyme that is present in both cardiac and skeletal muscle
- Elevations begin 4 - 6 hours post insult and resolve within 36 - 48 hours
- Isoenzyme CK-MB is proportionally greater in cardiac muscle but is present in larger absolute quantities in skeletal muscle
- Formerly the preferred test of choice, now replaced by troponin due to its higher specificity for cardiac injury than CK-MB
- Myoglobin:
- Heme complexed protein that is present in wide range of cell types and is released in response to damage
- Low specificity makes this an antiquated test that should rarely be employed
- Lactate dehydrogenase:
- Legacy test, no longer in use
- Troponin I / troponin T:
- Serologic markers of heart failure (UpToDate: Natriuretic Peptide Measurement in Heart Failure [Accessed 15 January 2021]):
- Brain natriuretic peptide (BNP, proBNP, NT proBNP)
- Three distinct proteins / cleavage products initially found in brain but also present in ventricular myocytes
- Released in response to increased ventricular pressure
- Elevated BNP is highly sensitive but not very specific for heart failure
- Atrial natriuretic peptide (ANP)
- Protein present in atrial myocytes
- Released in response to dilation of atria due to increased volumes
- Brain natriuretic peptide (BNP, proBNP, NT proBNP)
Gross description
- Isolated myocardial specimens:
- Endocardium: thin, shiny, translucent layer without fibrotic (tan-white) thickening
- Myocardium: uniform tan-brown to red striated tissue with firm but pliable texture
- No areas of gray-brown mottling and no areas of dense fibrosis
- Epicardium: thin, shiny and translucent without fibrosis; epicardial fat may be present
- Explant and autopsy specimens:
- Evaluation of the surgical or autopsy specimen should be conducted with a systematic approach (Allen: Moss & Adams' Heart Disease in Infants, Children, and Adolescents, 8th Edition, 2012)
- In addition to review of clinical history, gross evaluation should include the following:
- Position in the thoracic cavity
- Sidedness (situs)
- Evaluation of systemic connections and epicardial surface
- Coronary artery distribution and patency
- Inspection of endocardium and myocardium via short axis sectioning and opening of chambers along lines of blood flow
- Inspection for septal defects
- Evaluation of semilunar and atrioventricular valves
- Determination of atrioventricular concordance
- Measurement of heart weight, wall thickness and chamber dimension (at midventricular level)
Gross images
Microscopic (histologic) description
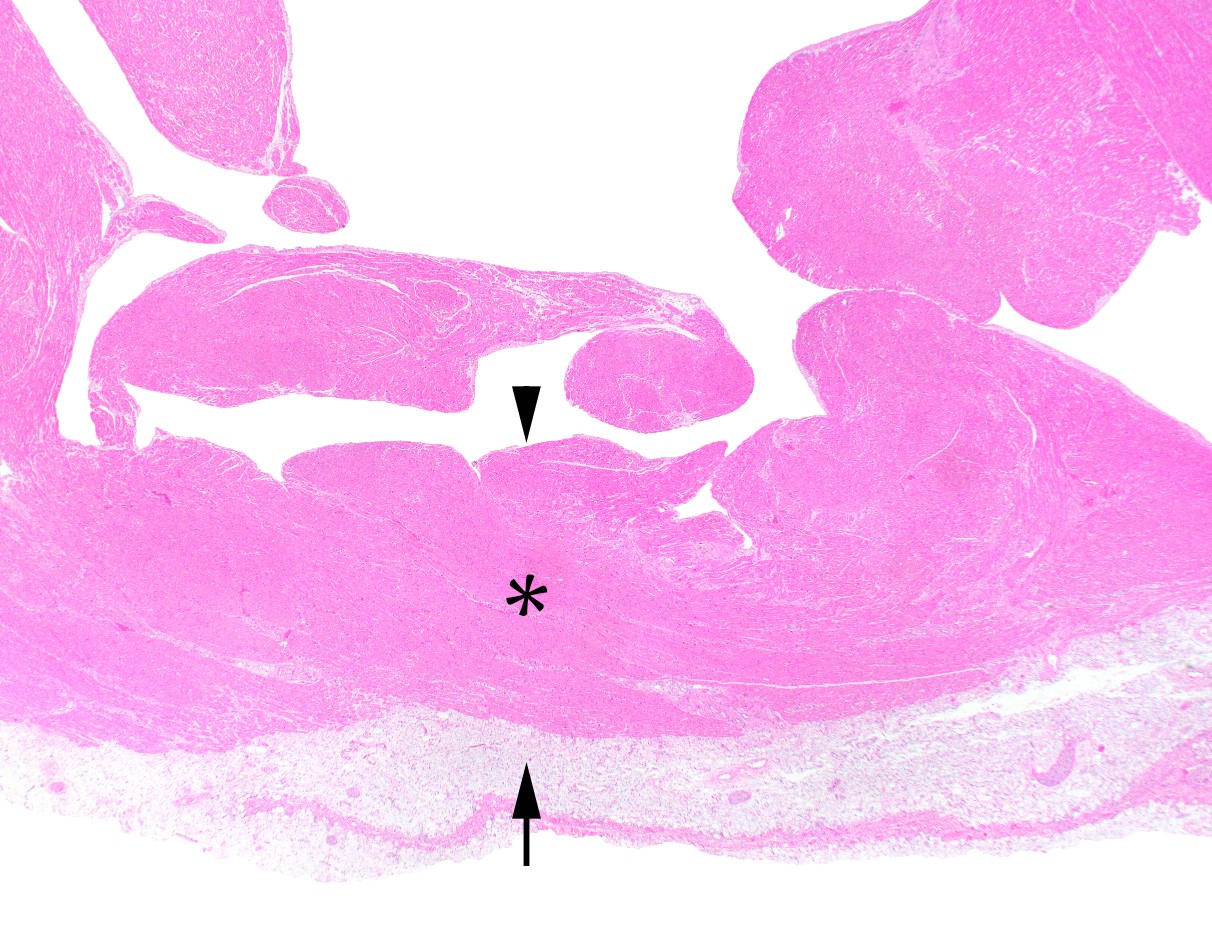
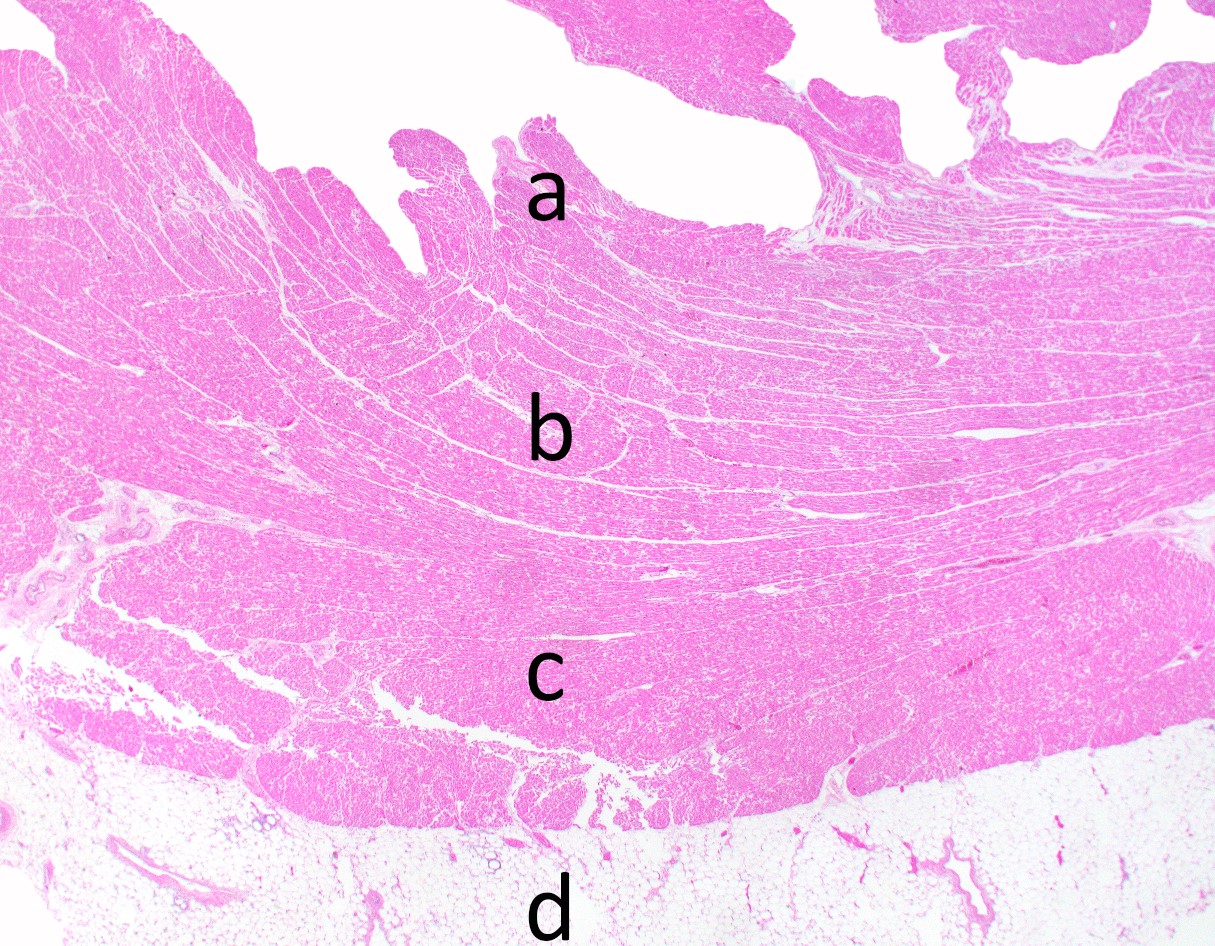
- Endocardium (innermost layer):
- Thin tissue which lines all 4 chambers of the heart
- Consists of 3 layers: endothelium, subendothelium and elastic layer
- Endothelium is a thin single cell layer that is continuous with the endothelial lining of the systemic vasculature
- Subendothelial layer may have variable thickness; it is most prominent in the left atrium
- Elastic layer is the thickest layer of the endocardium and shows prominent elastic fibers admixed with smooth muscle cells
- Myocardium (middle layer):
- Organized in 3 layers / regions:
- Subepicardial (superficial)
- Middle
- Subendocardial (deep)
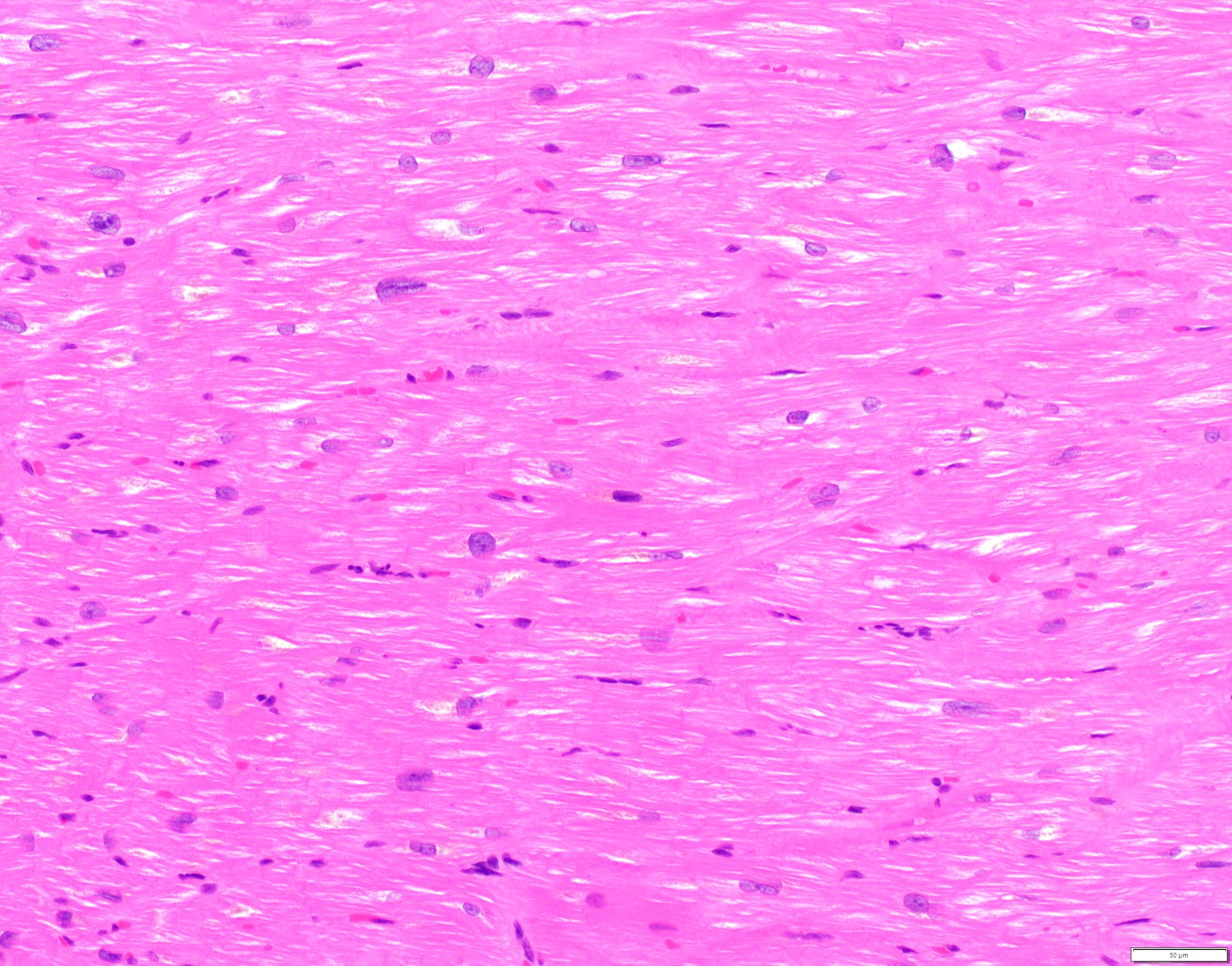
- Cardiac myocytes:
- Striated involuntary muscle cells measuring approximately 10 - 20 micrometers in diameter (3 - 5 red blood cells thick)
- Components:
- Sarcolemma: thin cell membrane
- Nucleus: small, round and basophilic, approximately the size of 1 red blood cell
- Sarcoplasm:
- Contains longitudinal myofibers composed of myofilaments, giving it the striated appearance
- Myofilaments (actin and myosin) are arranged in a staggered pattern to form the sarcomere, the contractile unit of the myocyte
- Interstitium:
- Composed of fibroblasts, extracellular matrix, adipocytes and scattered inflammatory cells
- Penetrating capillaries and arterioles originating from the epicardial coronary arteries are present throughout the interstitium and supply blood and oxygen to the cardiac myocytes, in an epicardial to subendocardial distribution
- Organized in 3 layers / regions:
- Epicardium (outermost layer) (Prog Cardiovasc Dis 2017;59:327):
- Composed of mesothelial cells that are part of the innermost layer of pericardium (visceral pericardium), along with subjacent fibroconnective and vascular tissue
- Benign fibrotic thickening may occur over the anterior surface of the heart giving rise to the soldier's patch
- Epicardial fat may also be considered part of the epicardial layer
- Reference: Buja: Cardiovascular Pathology, 4th Edition, 2015
Microscopic (histologic) images
Immunohistochemistry & special stains
- Immunohistochemical stain targeting skeletal muscle will also stain cardiac myocytes
- IHC: actin, desmin, vimentin (Cytobios 1986;45:195)
- Special stains may be used in evaluation of normal myocardium:
- Congo red in the evaluation for amyloid (apple green birefringence) (Hum Pathol 2014;45:1766)
- Sulfated Alcian blue in the evaluation for amyloid (sea foam green) (J Clin Pathol 1976;29:22)
- Prussian blue in the evaluation for iron (Rev Esp Patol 2019;52:45)
- Masson trichrome in the evaluation for interstitial fibrosis (Circulation 2018;138:1224)
Electron microscopy description
- Sarcomere (Environ Health Perspect 1978;26:159):
- Composed of myofilaments arranged in a staggered pattern (alternatively actin and myosin)
- Bound by perpendicular electron dense Z bands
- Contraction pulls Z bands closer and relaxation allows for them to move further apart
- Orderly spacing of parallel myofilaments
- Nucleus:
- Fine chromatin with single nucleolus
- Mitochondria:
- Circular to ovoid structures of relatively uniform size with prominent layered cristae
- Intercalated disk:
- Jagged electron dense line representing cell - cell junctions between myocytes
- Lipofuscin:
- Radio dense material associated with age related changes
- Often perinuclear in distribution
Practice question #1
Practice answer #1
Practice question #2
Which structure is referred to as the pacemaker of the heart?
- Atrioventricular node
- Bachmann bundle
- Bundle of His
- Sinoatrial node
Practice answer #2