Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) description | Virtual slides | Cytology description | Cytology images | Immunofluorescence description | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice question #1 | Practice question #2 | Practice answer #2Cite this page: Qureshi MB, Chundriger Q, Ud Din N. Degenerative joint disease. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/jointsDJD.html. Accessed August 15th, 2025.
Definition / general
- Progressive arthropathy characterized by degenerative changes in articular cartilage, subchondral bone, synovium and ligaments, leading to joint stiffness, chronic pain and deranged joint movement (Nat Rev Drug Discov 2005;4:331)
Essential features
- Degenerative arthropathy with multifactorial etiology
- Most common cause of chronic joint pain in geriatric age group (Medicina (Kaunas) 2020;56:614)
- Associated with joint stiffness and decreased range of motion
- Classic radiologic features include loss of joint space, subchondral bone sclerosis and osteophyte formation
- Diverse histologic features include progressive damage and ultimate loss of articular cartilage, subchondral bone thickening, osteophyte formation, mild chronic inflammation of synovium and degeneration of ligaments and menisci
Terminology
- Osteoarthritis
- Osteoarthrosis
- Wear and tear disease
- Joint degeneration
- Degenerative arthritis
ICD coding
- ICD-10: M19.90 - unspecified osteoarthritis, unspecified site
- ICD-11:
Epidemiology
- Usually affects old age group
- More common in women than men
- More prevalent in the north (Osteoarthritis Cartilage 2011;19:1314, Curr Opin Rheumatol 2018;30:160)
- Risk factors include personal and joint level factors
- Personal factors with increased risk include African American race, female gender, genetic susceptibility, obesity, hyperlipidemia, increased systolic blood pressure, diet related factors (like vitamin D insufficiency) and high bone density / mass
- Joint related factors include particular bone / joint shapes, joint malalignment, thigh flexor muscle weakness, engagement in certain occupational / sports activities and joint injury (Ann Phys Rehabil Med 2016;59:134)
- Factors associated with decreased risk include weight loss, high fiber diet and Mediterranean diet
Sites
- May affect any joint
- Most commonly involves the large weight bearing joints like knees and hips along with hands, facet joints and feet (Br Med Bull 2013;105:185)
Pathophysiology
- In general, the chondrocytes attain a catabolic phenotype while the underlying bone cells follow an anabolic phenotype
- Chondrocytes fail to make normal amount and type of chondroid matrix
- Increased degradation of matrix
- Increased break down of cartilage attributed to deficiency of tissue inhibitors of metalloproteinase, aberrant production of matrix metalloproteinase (MMP) 13 and upregulation of cathepsin B (Biorheology 2002;39:237)
- Production and repair of cartilage extracellular matrix is regulated by insulin-like growth factors 1 and 2 (IGF1 and IGF2), which themselves are modulated by IGF binding proteins
- Reaction of differentiated chondrocytes to IGFs is enhanced by growth hormone
- Osteoarthritic cartilage shows reduced response to IGFs (Curr Opin Rheumatol 2011;23:492)
- Also, osteoarthritis is associated with aberrations of growth hormone, IGF and synthesis of IGF binding proteins
- This dysfunction also affects function of osteoblasts increasing osteoblastic activity
- Cytokines, specifically interleukin 1 (produced by the synoviocyte layer), upregulates MMPs production, increasing turnover of articular cartilage extracellular matrix (Aging Clin Exp Res 2003;15:364, Biorheology 2002;39:237)
- Interleukin 1, tumor necrosis factor alpha and nitric oxide induce chondroapoptosis
- Antiapoptotic molecule BCL2 production in decreased
- Abnormal loading of cartilage causes interleukin 1 and MMP upregulation in joints
- Chondrocyte senescence leads to decreased ability of chondrocytes to maintain the integrity of cartilage matrix, chondrocyte functional loss and propensity to undergo apoptosis (Ann Phys Rehabil Med 2016;59:333)
- Damaged chondrocytes act as antigen presenting cells for T cells, initiating a cell mediated immune response
- Humoral immunity mediated by antibodies against chondrocyte membrane proteins, proteoglycan link protein and cartilage proteins plays role in osteoarthritis (J Clin Med 2022;12:5)
- Impaired balance between osteoblastic and osteoclastic activity causes marked osteoblastic bone deposition causing subchondral bone sclerosis and osteophyte formation
Etiology
- Most cases are idiopathic
- Infection
- Trauma (Clin Orthop Relat Res 2009;467:1800)
- Metabolic bone disease
- Inflammatory arthropathies (rheumatoid disease most common)
- Osteonecrosis
- Age
- Hormonal change
- Ethnic origin (Dtsch Arztebl Int 2010;107:152)
- Lifestyle (alcohol, tobacco)
- Factors affecting joint load, like genetic predisposition, increased weight, deranged anatomy (Nat Rev Rheumatol 2012;8:77, Orthopedics 2005;28:s207)
Diagrams / tables
Clinical features
- Pain during or after movement of joint (SICOT J 2022;8:14)
- Joint stiffness in the morning or after being inactive (Nurs Stand 2009;24:35)
- Tenderness when light pressure is applied to or around joint
- Decreased flexibility, limited range of motion
- Grating sensation, popping or crackling sound on movement of joint
- Bone spurs (extra bits of bone) around the affected joint
- Swelling
- Gradual loss of joint function
Diagnosis
- Diagnosis is based on integration of history, physical examination, laboratory and radiologic findings (JAMA 2021;325:568)
- Histopathologic findings help in diagnosis and assessment of severity of disease process
Laboratory
- No specific blood tests (Aging Clin Exp Res 2003;15:373)
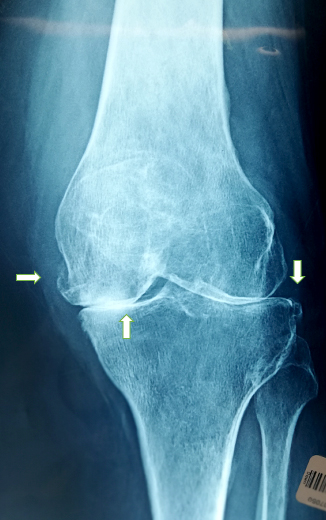
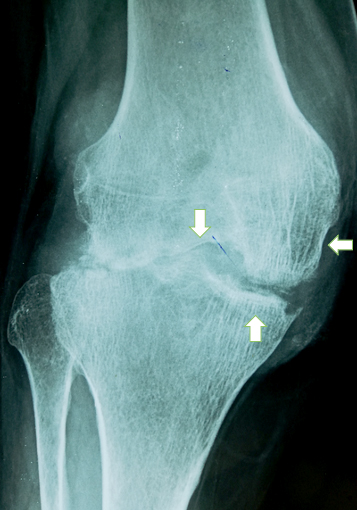
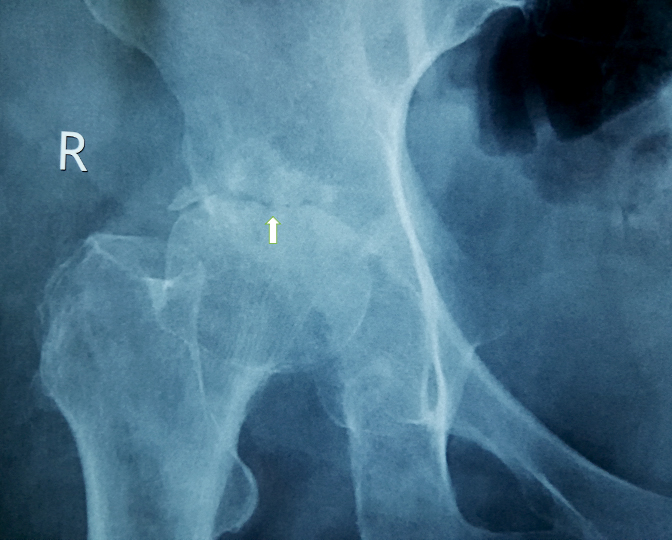
Radiology description
- Narrowing of joint space: usually asymmetric
- Subchondral sclerosis
- Sclerosis involving joint margins
- Osteophytosis
- Joint erosions
- Subchondral cysts
- Bone marrow edema-like lesions, adjacent to regions of cartilage damage
- Synovitis (50%)
- Plain radiograph: most commonly used for assessment of bony changes (Best Pract Res Clin Rheumatol 2006;20:27)
- Ultrasound: detects joint effusion and synovitis
- CT: very efficient modality for detecting bony changes
- MRI: accurate in assessing bony and soft tissue changes, detects cartilage loss and bone marrow changes; contrast helps reveal synovitis (Radiology 2020;296:5)
- Technetium 99m methyl diphosphonate (99mTc MDP) / PET with 18FDG or 18F: used for multiple joint examination
Prognostic factors
- Gradual progression
- Articular cartilage is avascular and cannot rebuild, hence the degenerative changes cannot be reversed
- Hip osteoarthritis: superolateral type of migration of the femoral head, subchondral sclerosis, high Kellgren Lawrence (KL) grade at baseline, high intensity sporting activities and being overweight (Arthritis Res Ther 2019;21:192)
- Knee osteoarthritis: age, body mass index, ethnicity, comorbidity, infrapatellar synovitis, joint effusion, medial femorotibial cartilage loss, high serum level of hyaluronic acid and baseline severity of disease (Arthritis Res Ther 2015;17:152)
- Physical workload is a prognostic factor for both types of osteoarthritis (Nat Clin Pract Rheumatol 2007;3:78)
Case reports
- 32 and 33 year old women presented with right hand joint pain (J Orthop Case Rep 2014;4:6)
- 35 year old woman presented with a tear in the rotator cuff (Bull Hosp Jt Dis 1998;57:216)
- 58 year old woman presented with an intra-articular mass and unilateral hip osteoarthritis (Skeletal Radiol 2018;47:717)
Treatment
- Conservative treatment: physical therapy, oral NSAIDs and local steroid injection
- Joint arthroplasty: unbearable pain, severely limited range of motion (PM R 2012;4:S97)
- Systemic immune / inflammatory cause: specific treatment of cause may improve / slow down the degenerative process (F1000Res 2020;9:325)
Clinical images
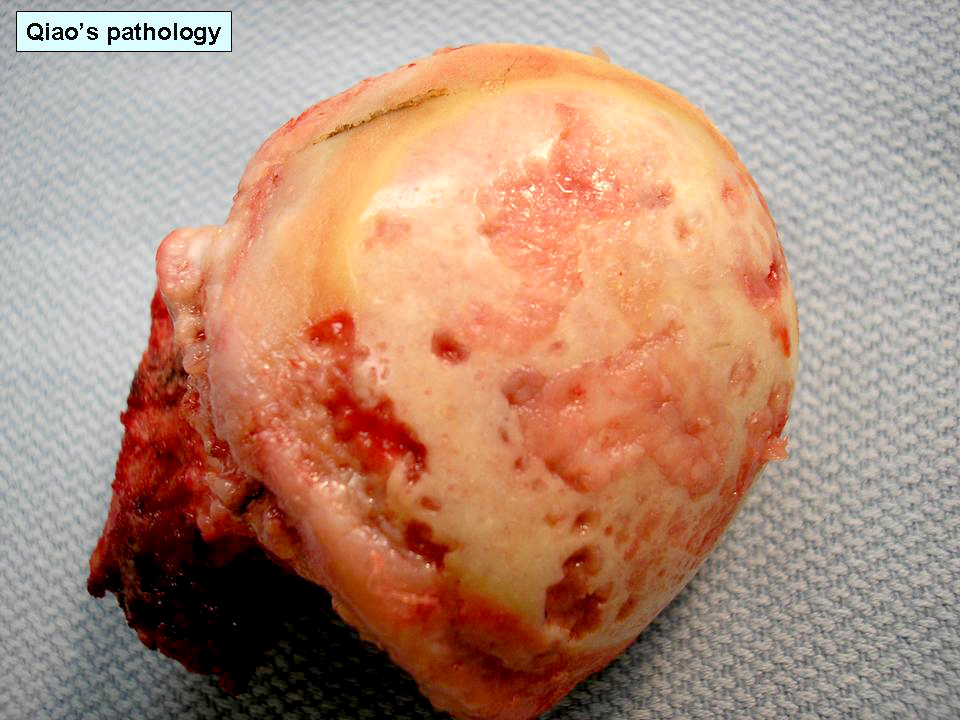
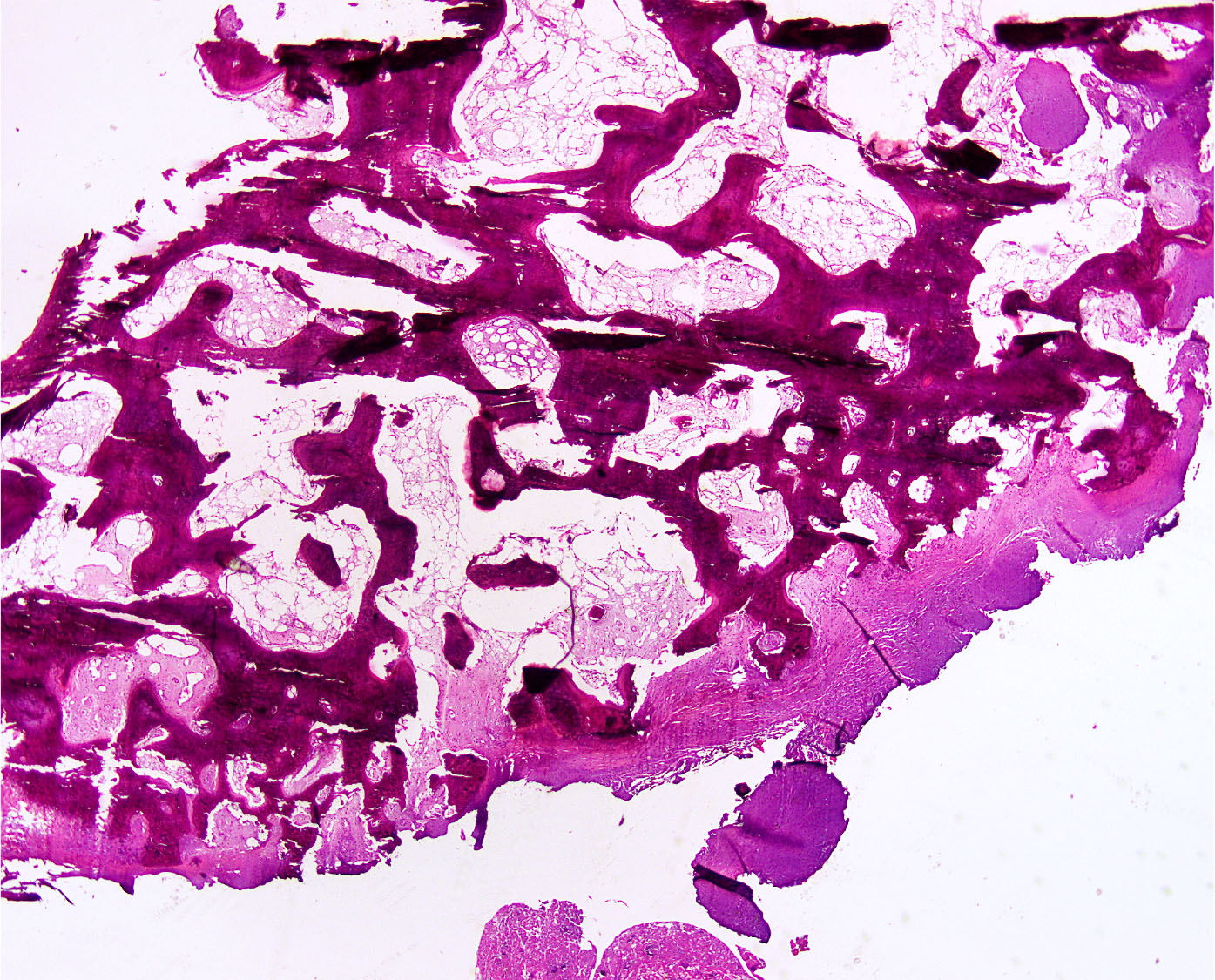
Gross description
- Erosion and loss of articular cartilage (focal, segmental or diffuse)
- Flattening of joint surface, concave deformity in tibial plateau
- Bone erosions and deformities
- Osteophytes: bony outgrowths usually seen at periphery of joint covered by fibro / hyaline cartilage; have reddish marrow as compared to marrow of medullary cavity
- Eburnation of bone: loss of articular cartilage causes exposed bone to articulate on bone; the exposed bone forms a smooth hard surface owing to repeated abrasions (Radiol Technol 2011;83:37)
- Subarticular pseudocysts called geodes
- Large geodes may cause collapse of articular plate, microfractures and osteonecrosis
- Intra-articular loose bodies (joint mice): fragmented pieces of articular cartilage / osteophytes
- Synovium may appear finger-like
- Sections should be taken from articular changes as well as soft tissue including synovium and menisci
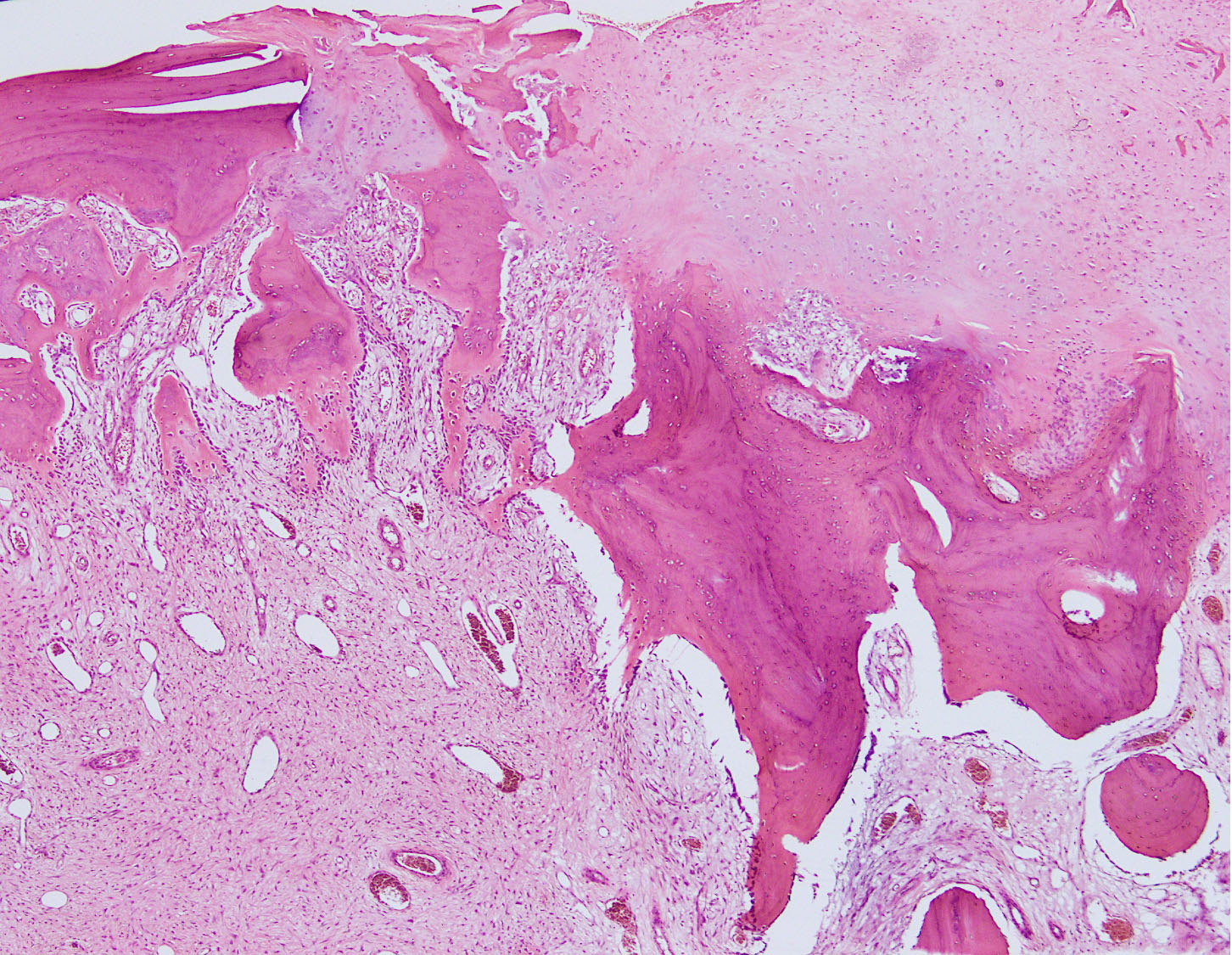
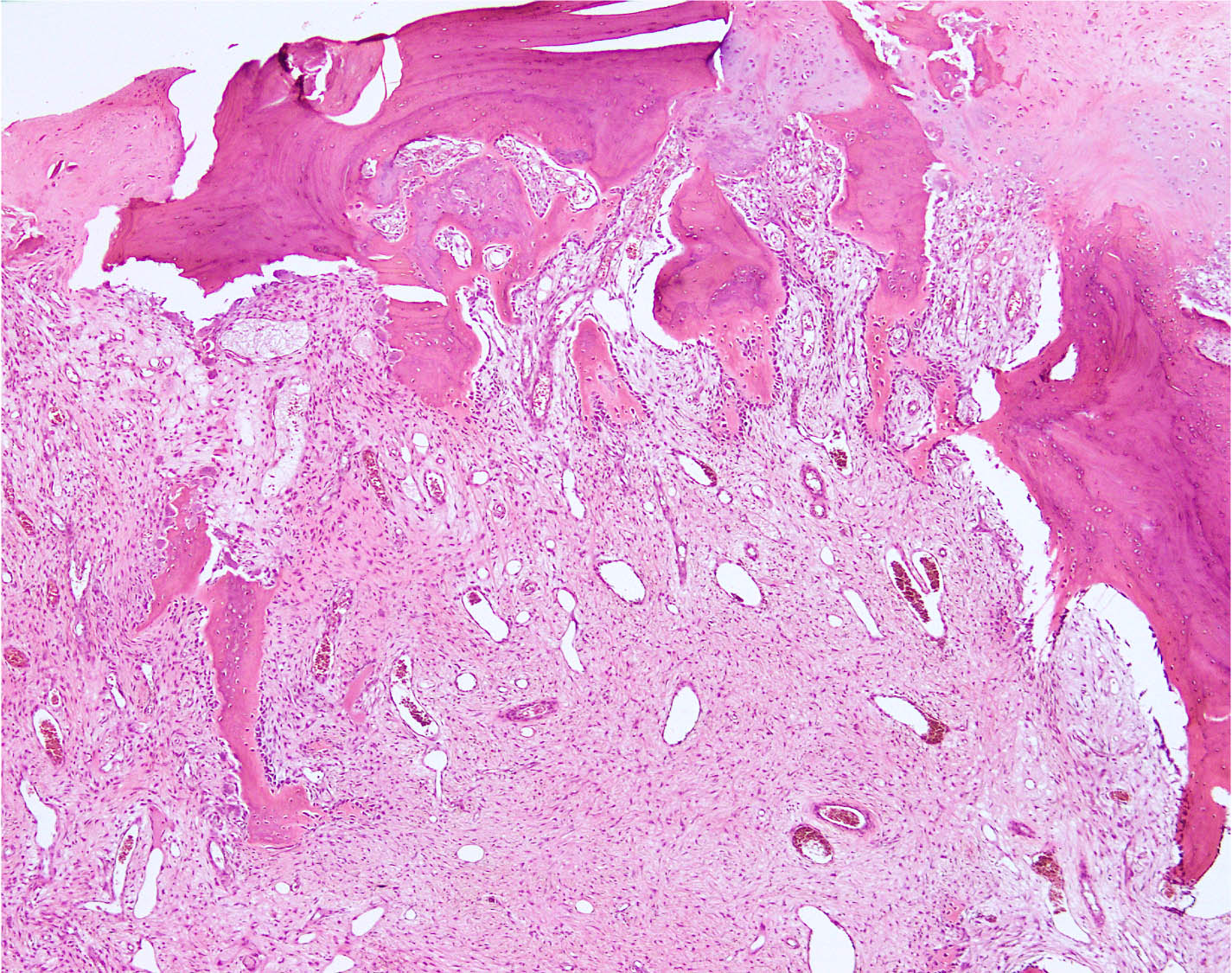
Microscopic (histologic) description
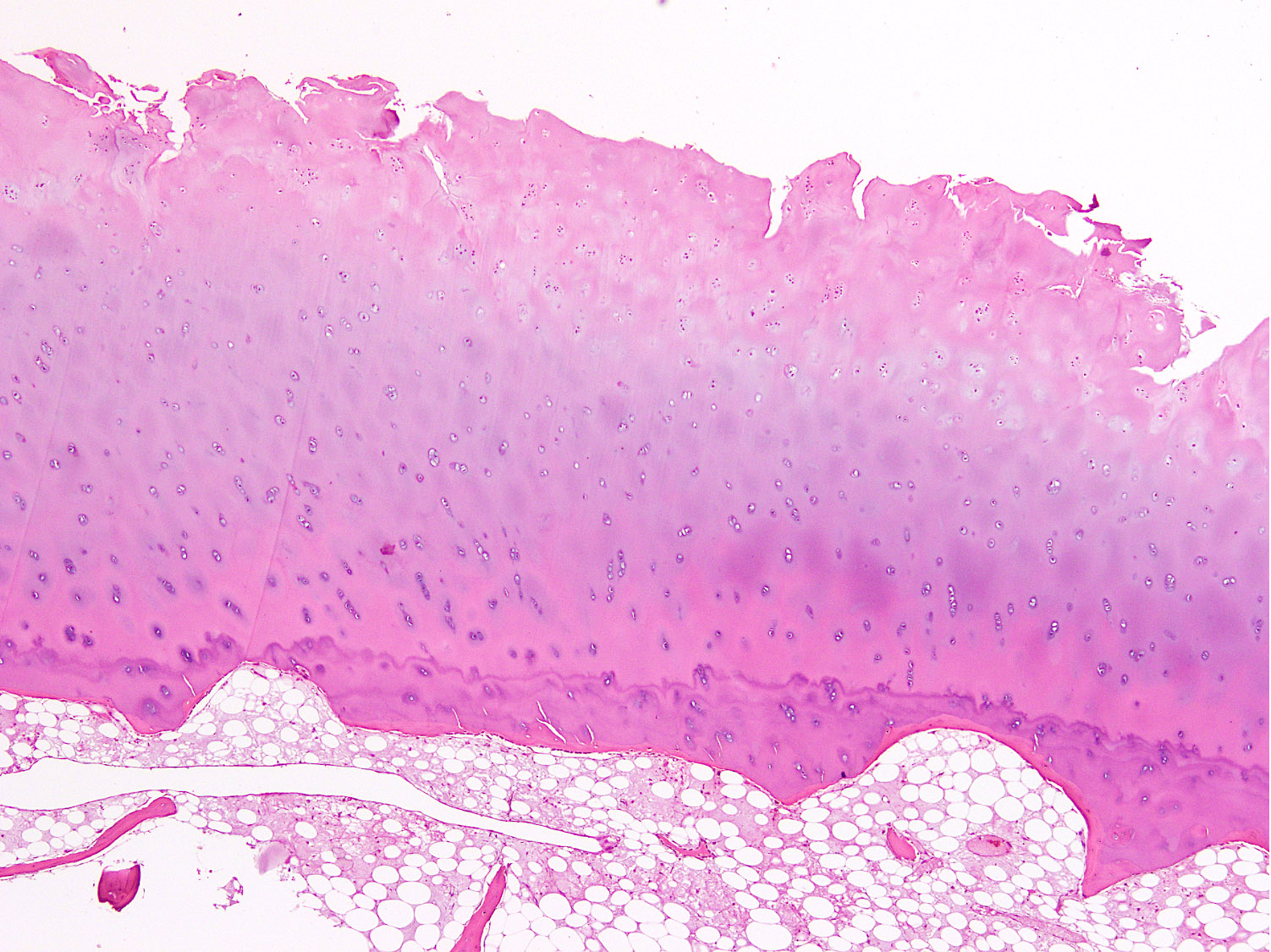
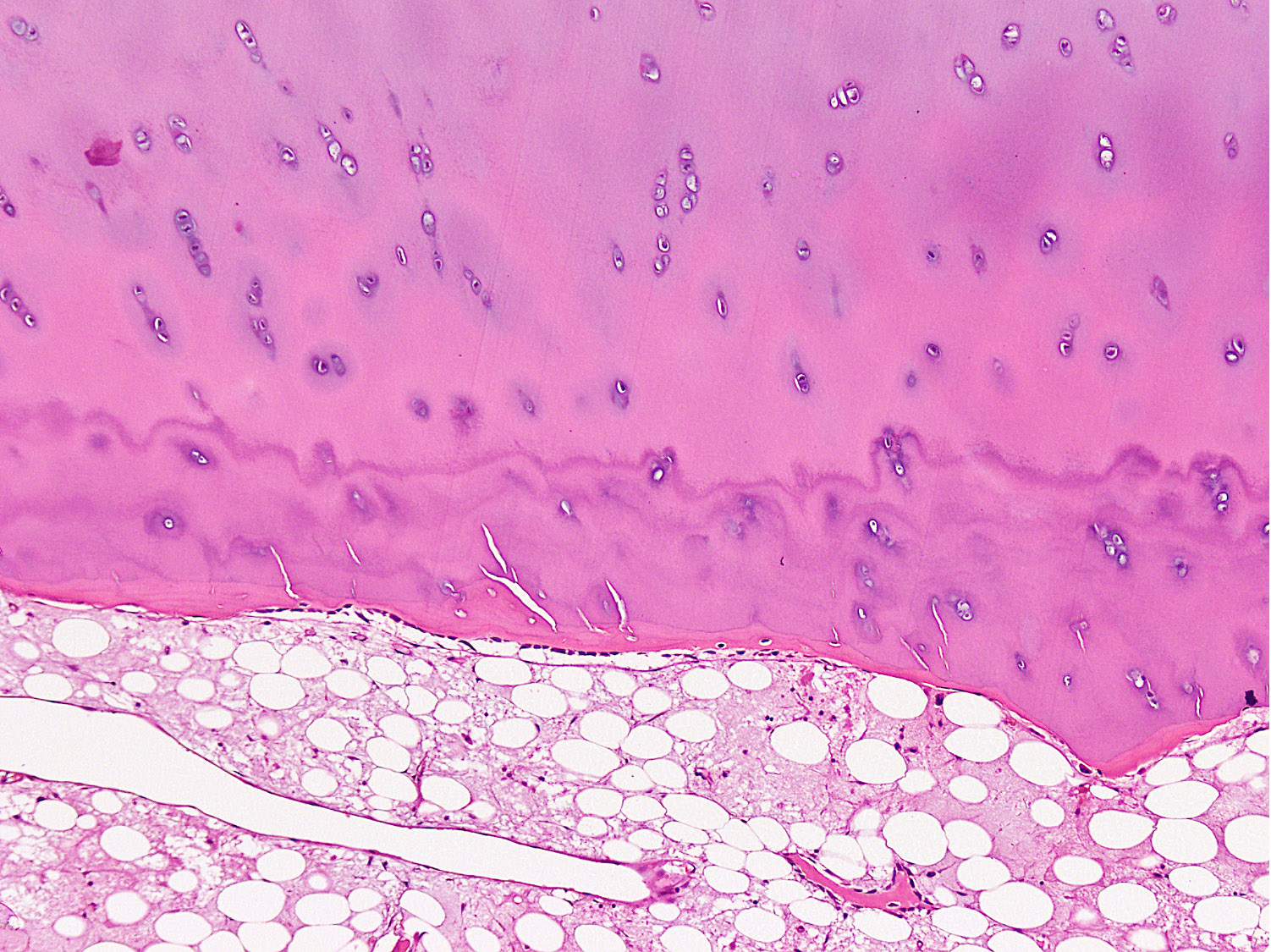
- Articular cartilage changes
- Begin with localized changes
- First change is loss of proteoglycan from the superficial layers of articular cartilage
- This loss damages the collagen network, leading to development of cracks, splits and fissures in the cartilage (Vet Pathol 2014;51:968)
- They extend from the surface towards subchondral bone
- Chondrocyte lacunae are reduced in number and appear empty due to chondrocyte apoptosis
- Clones of chondrocytes (chondrocyte clusters) form adjacent to fissures and in deeper parts in order to repair the damaged cartilage but their functional ability is compromised (Curr Rheumatol Rep 2019;21:38)
- Damaged cartilage thus appears more cellular due to unevenly distributed chondrocytes throughout the matrix
- Pannus composed of fibroblasts and type I collagen forms at the periphery and in regions of matrix loss, bridging across fissures
- Discrete hematoxyphilic lines (duplication of tide marks) form at the interface between mineralizing and nonmineralizing cartilage
- Gradual progressive damage results in loss of articular cartilage from articular surface resulting in exposure of bone / calcified cartilage
- Changes involve both opposing articular surfaces, causing bone to articulate on bone, followed by eburnation
- Eburnated bone looks like cortical bone without periosteum in transverse sections
- Eburnated bone is damaged and reparative fibrocartilage islands form and may grow to develop a complete fibrocartilaginous covering over the eburnated surface (Calcif Tissue Int 2021;109:303)
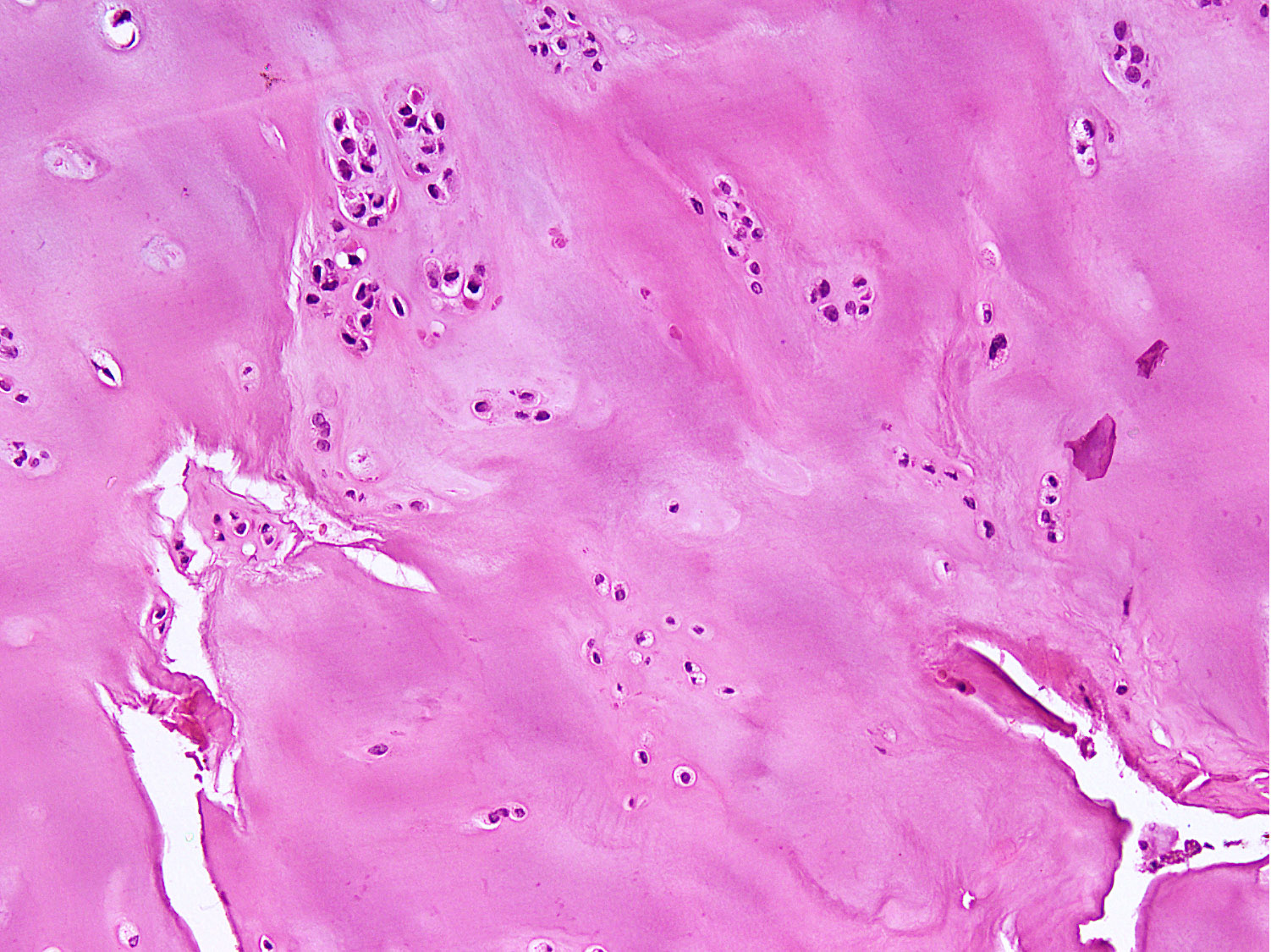
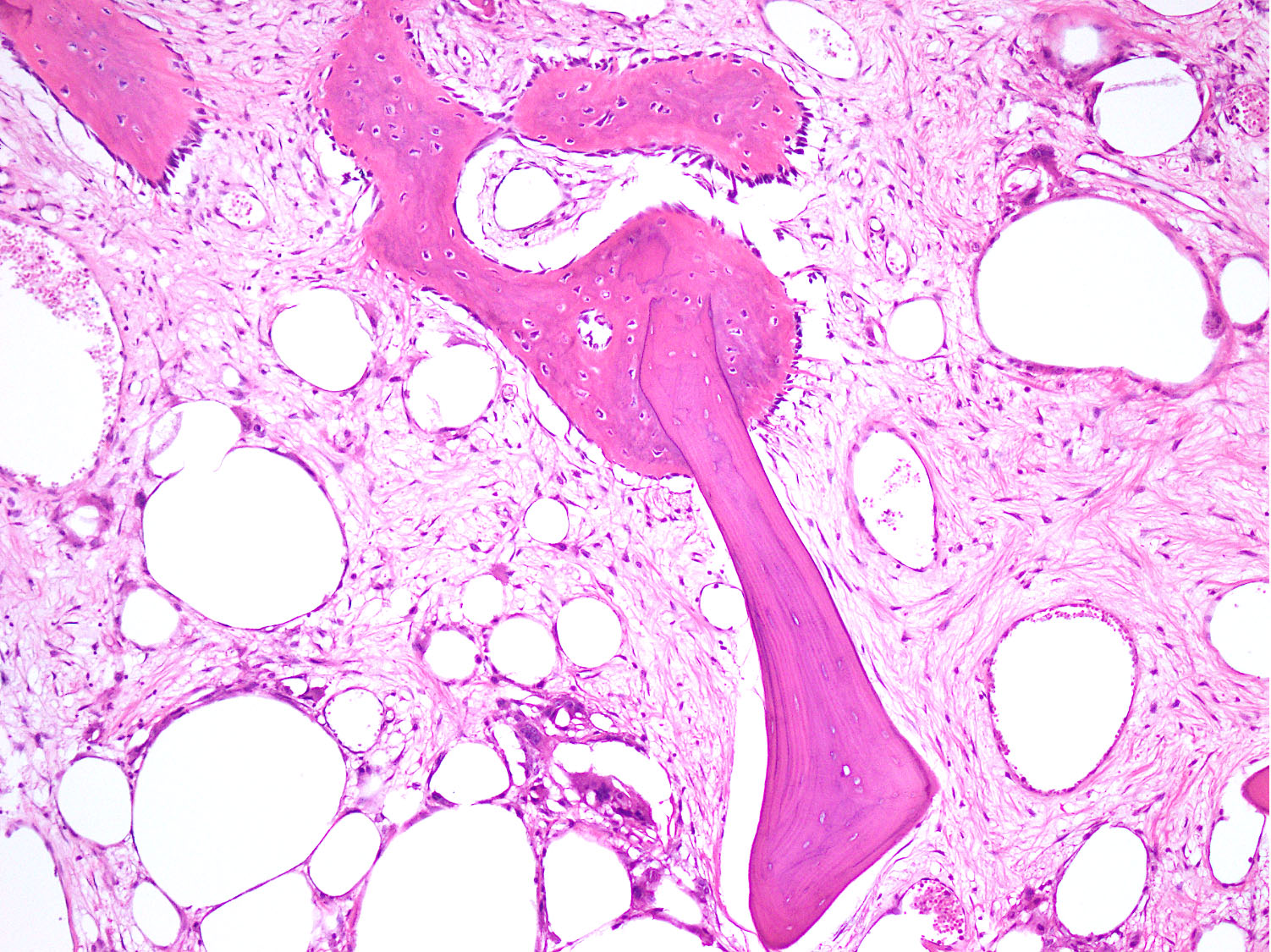
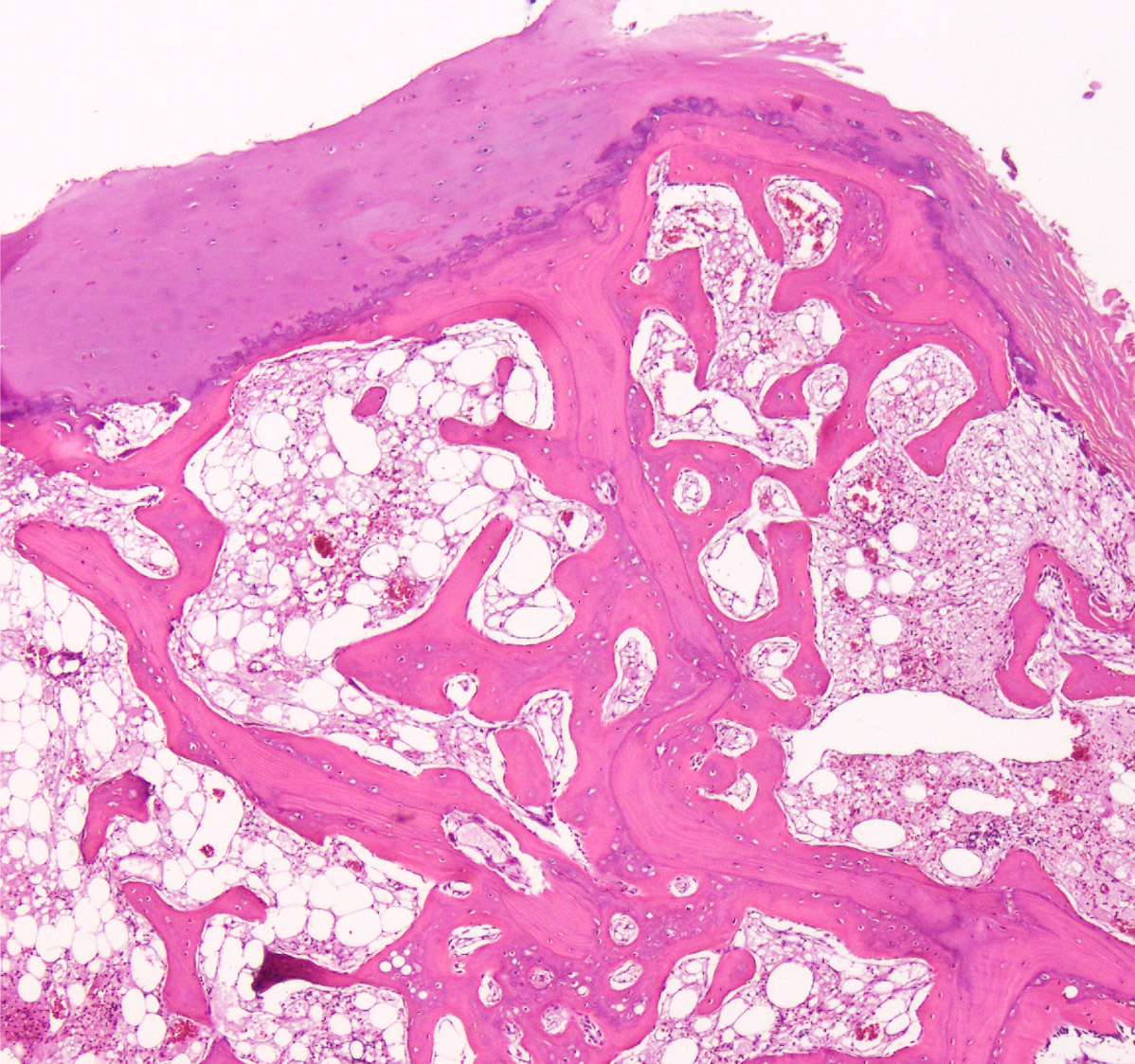
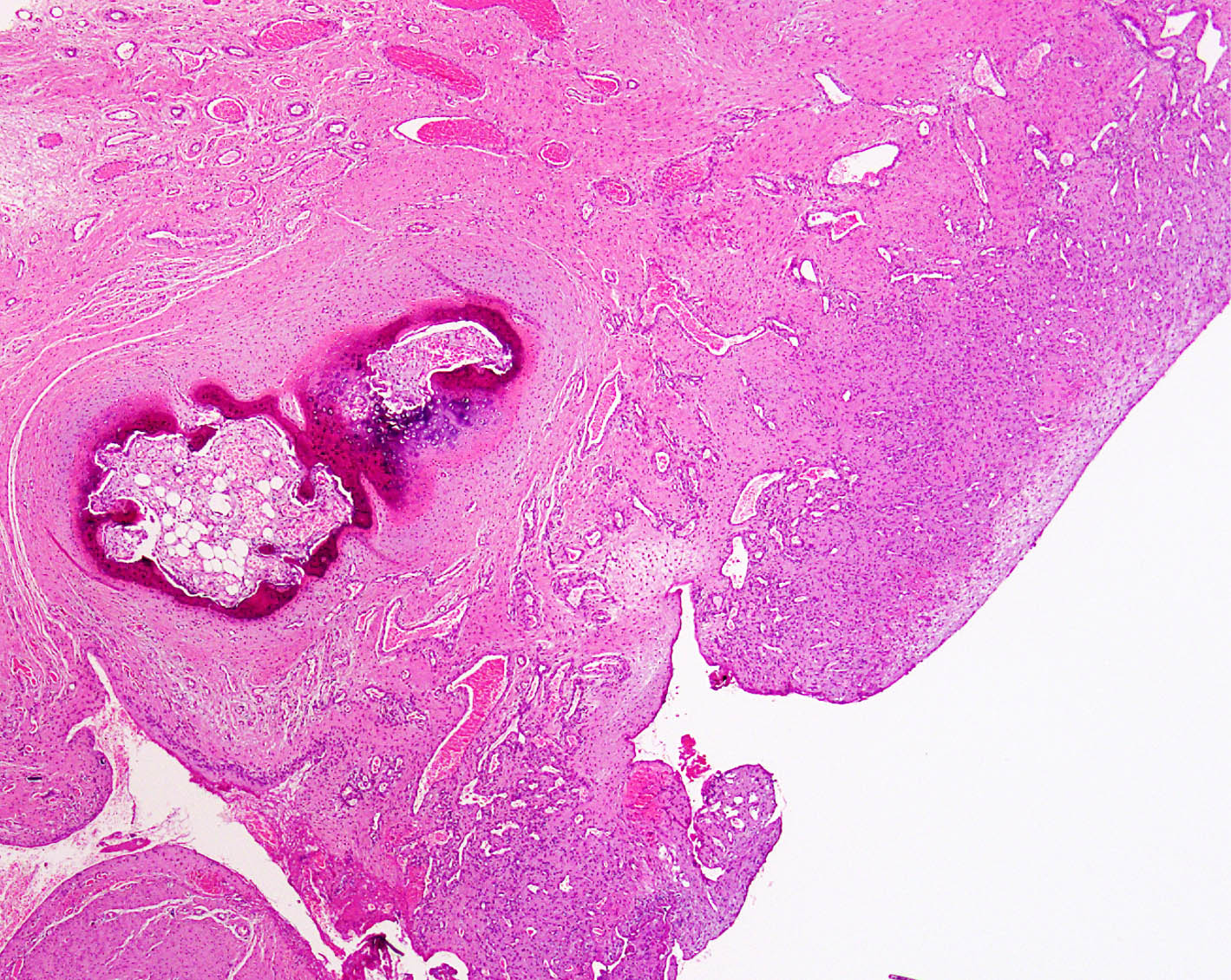
- Subchondral bone changes
- There is increased osteoblastic activity that results in subchondral bone sclerosis and osteophyte development (Microsc Res Tech 1997;37:333)
- Mid zone chondrocytes near cartilage edge induce new bone formation via ingrowth of capillaries and endochondral ossification
- With progression, the process of bone formation extends centrally
- New bone formation within cartilage separates the cartilage into 2 layers; one above the surface of osteophyte and the other buried deep within bone in line of articular surface
- At the junction of capsular and ligamentous insertions into bone osteophytes form via endochondral ossification from areas of chondroid metaplasia
- Intra-articular osteophytes may break and form intra-articular loose bodies
- Osteophytes have a shell of cortical bone continuous with the subchondral bone and cortical bone of the shaft
- Eburnated bone may show small areas of necrosis (absence of osteocyte nuclei) secondary to damage
- Necrosis is more common above cysts
- Bone cysts (geodes) form in advanced osteoarthritis due to the permeation of synovial fluid through bone channels into marrow (Arthritis Res Ther 2013;15:223)
- Cysts contain synovial fluid or fracture callus-like tissue (i.e., new cartilage, woven bone, fibrocartilage or fibrous tissue); they may also contain hypocellular myxoid material and inflammatory cells (lymphocytes and few plasma cells)
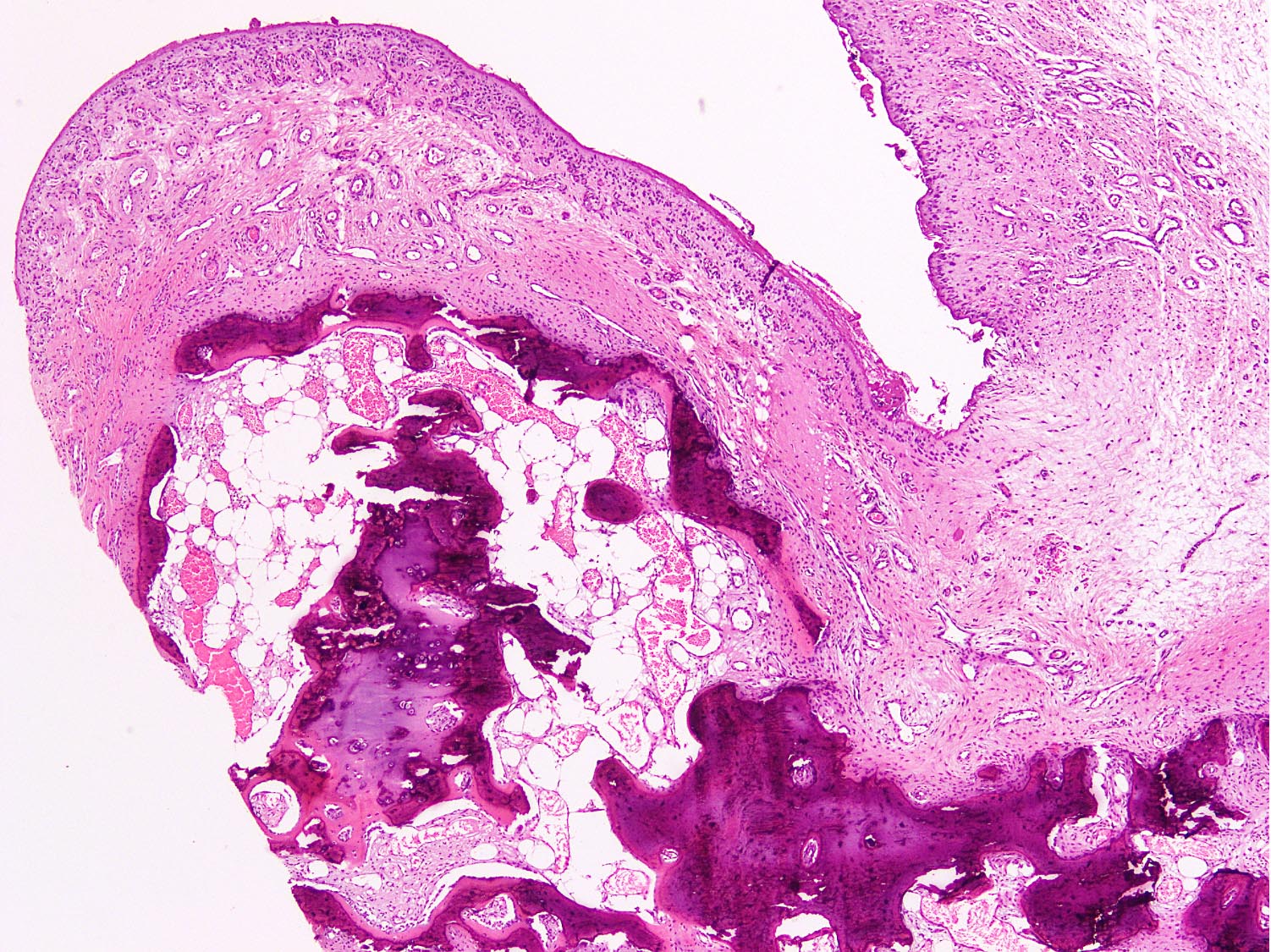
- Synovium changes
- Villous configuration
- Synovial hypertrophy and hypervascularity (Arthritis Res Ther 2017;19:18)
- Multinucleation of synoviocytes is often present
- May appear inflamed initially with perivascular edema and mast cell infiltrate
- Inflammation is usually not diffuse or subsynovial
- Edema may become marked, specifically around dilated subintimal vessels; called serous synovitis
- Progressive synovial fibrosis occurs in advanced arthropathy with associated subintimal perivascular chronic inflammatory cells (predominant lymphocytes and occasional plasma cells) (Clin Exp Rheumatol 1988;6:41)
- Neutrophils are usually absent
- Small fragments of cartilage and bone within and below the synoviocyte layer
- Calcified debris within synovium may induce florid histiocytic response, which may have multinucleated cells; called dendritic synovitis
- May have large bone particles when damage is marked and rapid
- Calcium pyrophosphate dihydrate crystals may be present
Microscopic (histologic) description
Contributed by Nasir Ud Din, M.B.B.S.
Cytology description
- Synovial fluid increases in volume and may lead to effusion
- Viscid fluid contains debris of articular cartilage (chondrocyte clusters), calcium pyrophosphate crystals, hydroxyapatite crystals, bone, synovial villi or fibrils (Arthritis Rheum 1985;28:511)
- Cell count is low (500 - 1,000 cells/mm3)
- Cell types include macrophages, synoviocytes and lymphocytes
- Blood / marrow / marrow derived lipid in cases of geode damage
Cytology images
Immunofluorescence description
- Not required for diagnosis (Acta Biomater 2022;146:274)
Positive stains
- Immunostains are not required for diagnosis (J Orthop Res 2017;35:1990)
- Special stains are helpful (Osteoarthritis Cartilage 2010;18:S113)
Negative stains
- Not required for diagnosis
Electron microscopy description
- Basic calcium phosphate and calcium pyrophosphate crystals in synovial fluid (J Clin Rheumatol 2016;22:369, Clin Rheumatol 2018;37:2847)
Molecular / cytogenetics description
- Epigenetic mechanisms include DNA methylation, histone modifications and microRNAs (Medicine (Baltimore) 2021;100:e27868, Ann Rheum Dis 2019;78:1420, Ann Rheum Dis 2015;74:569, Osteoarthritis Cartilage 2012;20:339)
Videos
Osteoarthritis - causes, symptoms, diagnosis, treatment & pathology
Sample pathology report
- Left head of femur, left knee replacement:
- Features are consistent with degenerative joint disease (see comment)
- Comment: Histology shows eburnated bone covered by fibrocartilaginous islands. There is loss of articular cartilage and subchondral bone sclerosis. Underlying subchondral cysts are present containing reactive woven bone, fibrous tissue and fibrocartilage. Peripheral osteophytes are present. Morphologic features and radiologic findings strongly support the diagnosis of degenerative joint disease.
Differential diagnosis
- Superficial subarticular insufficiency fracture:
- Type of stress fracture caused by repetitive and excessive stress to the subchondral bone (Jpn J Radiol 2022;40:443)
- Usually affects osteoporotic females and overweight middle aged males
- Acute onset of pain, may have pain for a few months
- Not identified by conventional radiography; MRI is more efficient
- Chronic fracture may show changes of osteoarthritis and osteonecrosis
- Avascular necrosis:
- Usually affects younger patients
- Bilateral presentation if disease is associated with collagen vascular diseases, steroid therapy or inherited diseases, like Gaucher disease
- Geographic subchondral bone and marrow necrosis (Am J Clin Pathol 2021;155:565)
- Intact, partially separated / detached articular cartilage surface
- Articular cartilage may appear smooth and fibrillated to folded and cracked
- Necrosis more marked than small foci of osteonecrosis in osteoarthritis
- Increased number of large bone particles in synovium
- Neuropathic joint (Charcot joint):
- Destructive arthropathy commonly associated with loss of proprioception
- Rapid joint erosion, destructive features of osteoarthritis are present
- Very little or no bone formation
- Less stable joint, more prone to damage by secondary insult
- Striking regional subarticular bone resorption
- Rheumatoid arthritis:
- Affects small bones of adult women
- Proliferative synovitis (synovial hyperplasia) with dense florid lymphoplasmacytic infiltrate in contrast to mild inflammatory component in osteoarthritis
- Necrobiotic nodules, fibrosis and organizing fibrin
- Pseudogout (calcium pyrophosphate crystal deposition disease):
- Calcium pyrophosphate dihydrate crystal accumulation in extracellular cartilage matrix, synovium and joints
- Affects older adults and the elderly
- Involves weight bearing joints, such as knees, hips, shoulders, wrists and ankles
- Weakly polarizable rhomboid shaped calcium pyrophosphate crystals show positive birefringence
- Septic arthritis:
- Usually affects young adults and children
- Involves a single joint
- Increased neutrophils and neutrophilic collections within tissue
Additional references
Practice question #1
Practice question #1
C. Duplication of tidemarks. The image shows duplication of tidemarks, which refers to discrete hematoxyphilic lines that form at the interface between mineralizing and nonmineralizing cartilage. Answer A is incorrect because cartilage fissuring is present at the upper edge. Articular cartilage osteoarthritic changes begin with loss of proteoglycan from the superficial layers of articular cartilage. This loss damages the collagen network leading to development of cracks, splits and fissures in the superficial cartilage. Answer B is incorrect because clones of chondrocytes (chondrocyte clusters) form adjacent to fissures and in deeper parts in order to repair the damaged cartilage. Answer D is incorrect because pannus is composed of fibroblasts and type I collagen that forms at the periphery and in regions of matrix loss, bridging across fissures. Answer E is incorrect because subchondral bone cysts are cysts that form below cartilage in advanced osteoarthritis due to the permeation of synovial fluid through bone channels into marrow.
Comment Here
Reference: Degenerative joint disease
Comment Here
Reference: Degenerative joint disease
Practice question #2
Bone typically follows an anabolic phenotype in degenerative joint disease. What is the term used for bony outgrowths usually seen at the periphery of osteoarthritic joints?
- Eburnated bone
- Geodes
- Loose bodies
- Osteoma
- Osteophytes
Practice answer #2
E. Osteophytes are bony outgrowths usually seen at periphery of joint covered by fibro / hyaline cartilage. Answer C is incorrect because intra-articular osteophytes may break and form intra-articular loose bodies. Answer A is incorrect because loss of articular cartilage causes exposed bone to articulate on bone and the exposed bone forms a smooth hard surface owing to repeated abrasions, referred to as eburnation. Answer B is incorrect because subchondral bone cysts (geodes) are cysts that form in advanced osteoarthritis due to the permeation of synovial fluid through bone channels into marrow. Cysts contain synovial fluid or fracture callus-like tissue (i.e., new cartilage, woven bone, fibrocartilage or fibrous tissue); they may also contain hypocellular myxoid material and inflammatory cells. Answer D is incorrect because osteoma is a benign bone forming tumor composed of mature cortical type or less frequently, trabecular bone, typically involving the craniofacial skeleton.
Comment Here
Reference: Degenerative joint disease
Comment Here
Reference: Degenerative joint disease