Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1Cite this page: Magliocca K. Ameloblastic carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/mandiblemaxillaameloblasticcarcinoma.html. Accessed September 23rd, 2025.
Definition / general
- Ameloblastic carcinoma is a rare primary odontogenic carcinoma of the jaw that exhibits ameloblastic differentiation, cytologic atypia, an increased number of mitotic figures, expansion of the basal layer and often punctate tumor necrosis
- Most commonly arises within the bone of maxilla and mandible
Essential features
- Rare; represents ≤ 2% of all odontogenic tumors (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005;99:191, Int J Oral Maxillofac Surg 2007;36:20, Oral Surg Oral Med Oral Pathol Oral Radiol 2019;127:151)
- Essential criteria: exhibits a histological resemblance to ameloblastoma with increased cytologic atypia
- Desirable criteria: intraosseous jaw tumor, tumor necrosis, associated ameloblastoma precursor, BRAF mutations in a subset
- May show a combination of spindle cell, stellate, squamous, epithelioid or (limited) clear cell morphologies
- Evidence of squamous differentiation is most reliably demonstrated by immunostaining for p40, p63 and CK5
Terminology
- Not recommended by WHO: malignant ameloblastoma, dedifferentiated ameloblastoma
ICD coding
- ICD-O: 9270/3 - ameloblastic carcinoma
- ICD-11: 2B5J & XH4M89 - malignant miscellaneous tumors of bone or articular cartilage of other or unspecified sites & odontogenic tumor, malignant
Epidemiology
- Accounts for ≤ 2% of all odontogenic tumors (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005;99:191, Int J Oral Maxillofac Surg 2007;36:20, Oral Surg Oral Med Oral Pathol Oral Radiol 2019;127:151)
- Mean age: 46.1 years (median: 45 years; range: 2 - 93 years) (J Oral Pathol Med 2024;53:174)
- Sex predilection appears to vary between studies
- Slight female predominance (J Oral Pathol Med 2024;53:174)
- Male predominance (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;103:799, Oncol Lett 2014;8:914, Eur Arch Otorhinolaryngol 2017;274:3803)
Sites
- More common in mandible than maxilla (Eur Arch Otorhinolaryngol 2017;274:3803, Oral Surg Oral Med Oral Pathol Oral Radiol 2016;121:e154, Head Neck 2019;41:4191)
Pathophysiology
- BRAF p.V600E or TP53 mutations have been reported in up to 40% of cases (Tumour Biol 2015;36:5649, Oral Oncol 2015;51:e77, J Oral Pathol Med 2019;48:413, Orphanet J Rare Dis 2020;15:316)
Etiology
- Etiology is largely unknown
- Majority of cases arise de novo
- Some develop in longstanding untreated ameloblastoma or in locally recurrent ameloblastoma after treatment (Oral Surg Oral Med Oral Pathol 1984;57:168, Oral Surg Oral Med Oral Pathol Oral Radiol 2014;118:e146, Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000;90:716)
Clinical features
- Many cases present with rapidly progressive jaw swelling at the involved site, which may extend into the overlying mucosa (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;108:904, Oral Surg Oral Med Oral Pathol Oral Radiol 2016;121:e154)
- Symptoms such as nasal congestion, exophthalmos, toothache, paresthesia, toothache or tooth mobility are related to localized mass effect of the tumor in maxilla or mandible (Eur Arch Otorhinolaryngol 2017;274:3803, Head Neck 2019;41:4191)
Diagnosis
- WHO blue book histological criteria for diagnosis of ameloblastic carcinoma
- Essential: exhibits a histological resemblance to ameloblastoma with increased cytologic atypia
- Desirable: an intraosseous jaw tumor, tumor necrosis, associated ameloblastoma precursor, BRAF mutations in a subset
Laboratory
- Occasionally associated with hypercalcemia of malignancy (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000;90:716)
- In hypercalcemia of malignancy, laboratory abnormalities may include
- Elevated total and ionized calcium
- Suppressed parathyroid hormone (PTH) levels
- Normal or low 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D levels
- Increased alkaline phosphatase levels
Radiology description
- Contrast enhanced computed tomography (CT) shows an expansile, largely hypodense lytic intraosseous jaw lesion with poorly defined margins as well as medullary and cortical bone destruction (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;108:904)
- Commonly exhibits extension into soft tissues; magnetic resonance imaging (MRI) may help delineate (J Clin Imaging Sci 2022;12:58)
- Moderate fluorodeoxyglucose (FDG) uptake on positron emission tomography (PET) CT helps detect metastasis (Dentomaxillofac Radiol 2010;39:449)
Radiology images
Prognostic factors
- Ameloblastic carcinoma is rare and the paucity of cases not only precludes an accepted pathologic staging paradigm but also undermines assessment of most prognostic factors; some investigators have attempted to understand the importance of some factors below (see associated references)
- Points to consider in assessment of prognosis
- Stage: no accepted staging paradigm for odontogenic malignancies
- Age: disease spans a broad age range
- Primary anatomic location: mandible versus maxilla
- Tumor size
- Extension beyond bone into soft tissues
- Histological variables
- Presence / absence of benign precursor ameloblastoma (Oral Surg Oral Med Oral Pathol 1984;57:168, J Oral Maxillofac Surg 2007;65:777)
- Histopathological patterns (Oral Oncol 2018;77:118)
- Tumor necrosis
- Mitotic rate
- Perineural or lymphovascular invasion
- Margin status (note: without an R0 initial resection, there is no disease free interval)
- Presence of specific gene alterations
- Variability in treatment
- Use of surgery alone
- Surgery in combination with adjuvant radiation therapy or proton therapy
- Use of standard chemotherapy versus targeted therapy
- Local recurrence: up to 40% of cases (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;108:904, Oncol Lett 2015;9:459)
- Regional metastases to cervical nodes occur in up to 13% of patients (Eur Arch Otorhinolaryngol 2017;274:3803, Pol J Pathol 2018;69:243, Orphanet J Rare Dis 2020;15:316)
- Distant metastasis develops in 33% of cases, most commonly in the lung, followed by the brain, liver and bone (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;104:e17, Eur Arch Otorhinolaryngol 2017;274:3803)
- 5 year overall survival rate is 70% (Orphanet J Rare Dis 2020;15:316, Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;108:904)
Case reports
- 31 year old man with headache and vision loss (J Clin Imaging Sci 2022;12:58)
- 61 year old woman with neck pain and right arm weakness (Neurosurgery 2021;88:E537)
- 68 year old man with a maxillary mass (Int J Surg Pathol 2023;31:442)
- 72 year old woman with mandibular pain (Maxillofac Plast Reconstr Surg 2023;45:17)
Treatment
- Primary treatment is heterogeneous, ranging from surgery alone to a combination of adjuvant therapies, including radiation therapy, traditional chemotherapy or targeted therapy (Oral Surg Oral Med Oral Pathol Oral Radiol 2019;127:e56, Eur Arch Otorhinolaryngol 2016;273:3293)
- Surgery: radical surgical resection is treatment of choice
- Radiation therapy: no established protocol
- Targeted therapy: BRAF or ALK inhibitor, depending on molecular findings (Eur Arch Otorhinolaryngol 2016;273:3293)
Clinical images
Gross description
- Cut surfaces reveal a solid mass with irregular borders and limited cystic change (Dentomaxillofac Radiol 2010;39:449, Oral Surg Oral Med Oral Pathol Oral Radiol 2016;121:e54)
Gross images
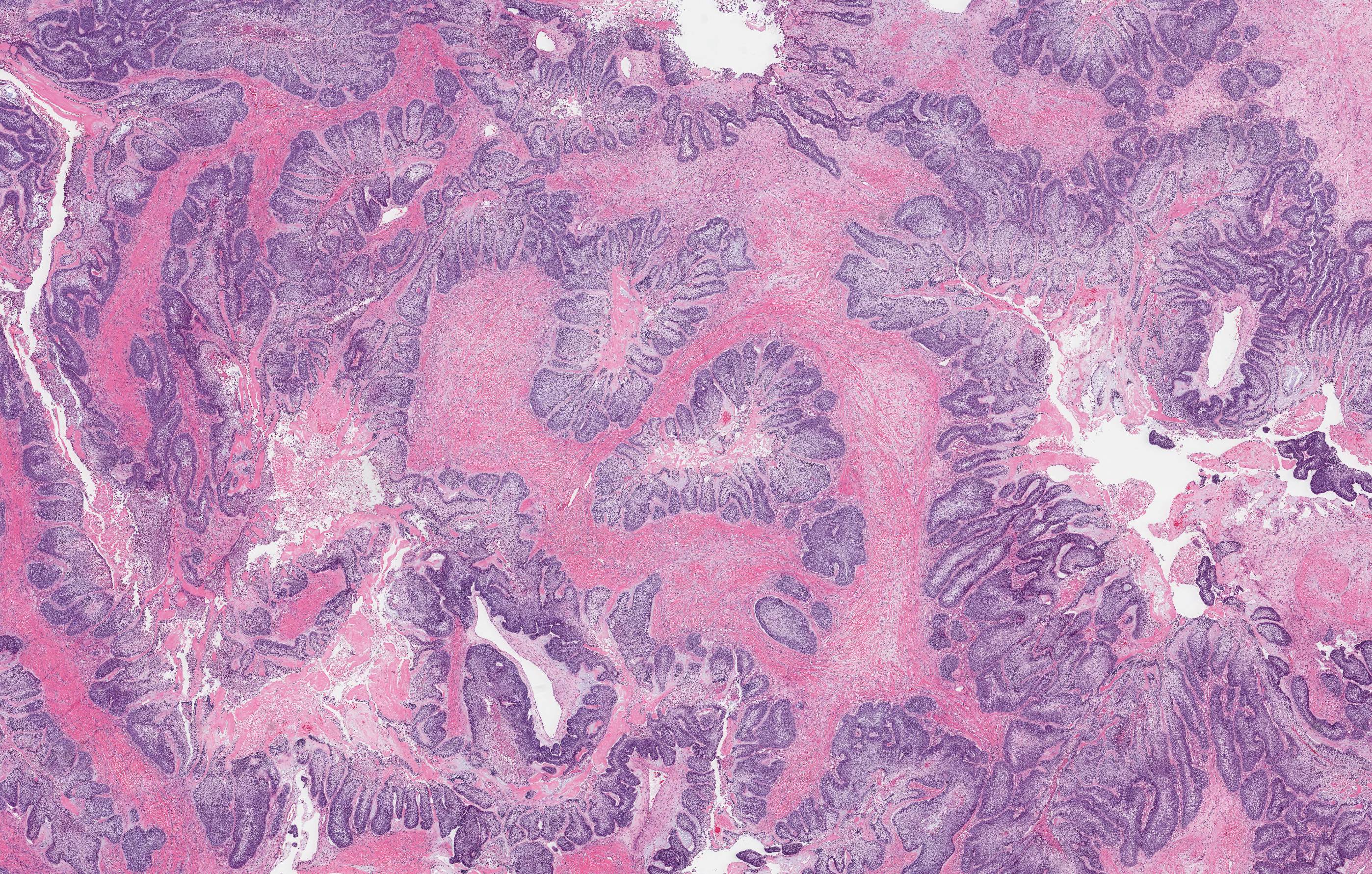
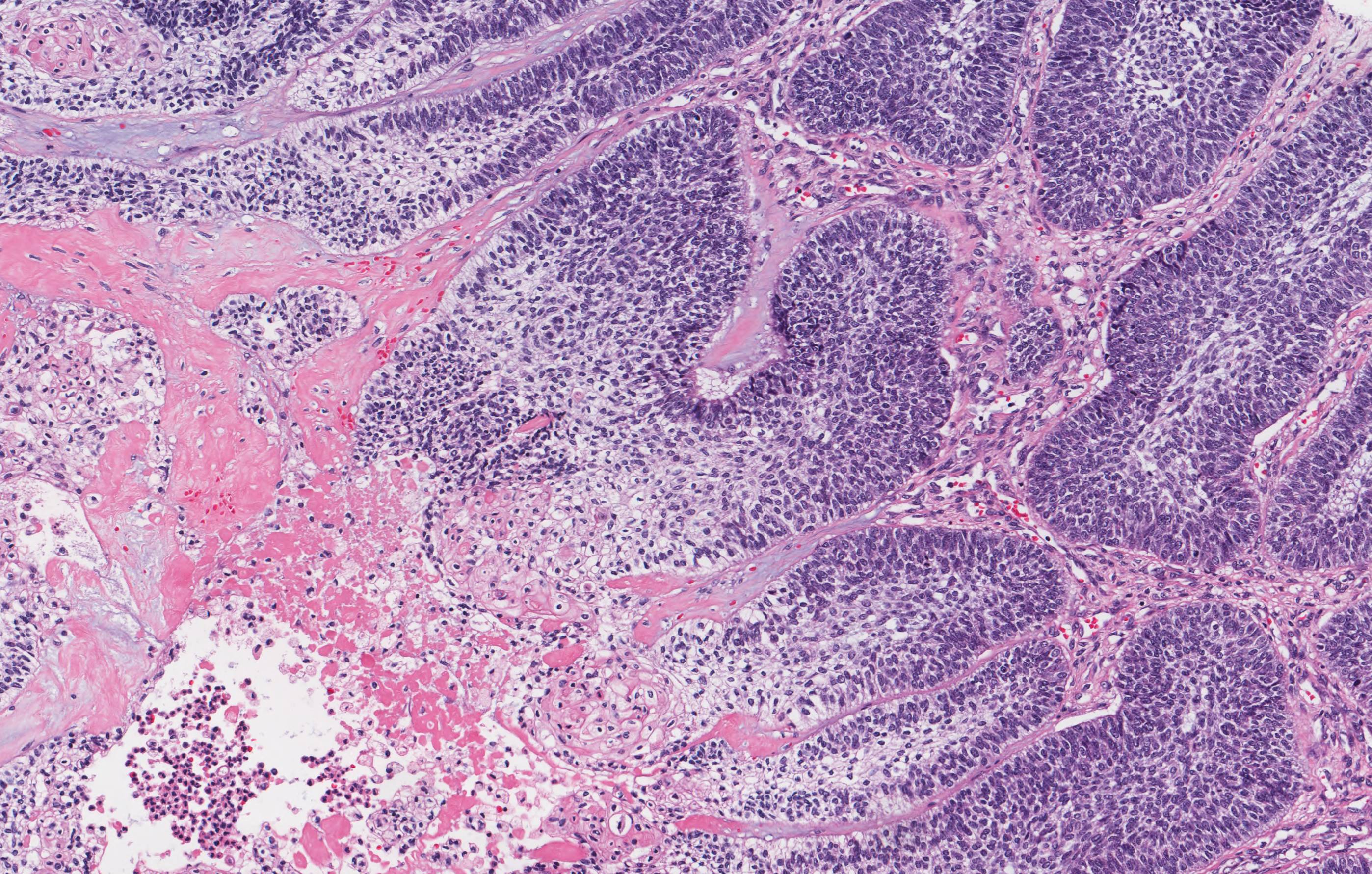
Microscopic (histologic) description
- Malignant tumor with varied morphology
- Most commonly, tumor architecture is follicular, plexiform or solid nests of ameloblastoma-like epithelium
- Peripheral palisading, nuclear reverse polarity and stellate reticulum must be evident at least focally
- Tumor may comprise areas of squamous, spindle cell morphology or clear cell change (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;103:799, Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;108:904, Oral Surg Oral Med Oral Pathol Oral Radiol 2014;118:e146, Histopathology 2016;69:687, Oral Surg Oral Med Oral Pathol Oral Radiol 2019;128:e113)
- Tumor grows in undulating bulky cords, nests or sheets with pushing borders or angulated infiltrative nests at the advancing front
- Tumor cells at the periphery of islands are often large with prominent nucleoli
- Pleomorphism can be marked
- Increased mitotic activity
- Necrosis is often present (central tumor islands or single cell)
- Extension into the mucosa does not distinguish benign ameloblastoma from carcinoma
- Dispersed invasion and perineural infiltration are uncommon findings (Arch Pathol Lab Med 2019;143:587, Orphanet J Rare Dis 2020;15:316)
Microscopic (histologic) images
Cytology description
- Fine needle aspiration (FNA) biopsy may detect possible metastasis in known cases (Dentomaxillofac Radiol 2010;39:449)
Positive stains
- CK19, CK5, p63 (Med Oral Patol Oral Cir Bucal 2017;22:e324)
- SOX2 can be positive but is variable and of limited utility in confirming a diagnosis of ameloblastic carcinoma (F1000Res 2024;13:557, Head Neck Pathol 2024;18:92)
- p53 overexpression in some but not all cases (Histopathology 2016;69:687, F1000Res 2024;13:557, J Microsc Ultrastruct 2022;12:165)
- Ki67 often elevated (F1000Res 2024;13:557, Head Neck Pathol 2024;18:92)
- BRAF V600E immunostain positive in a subset of cases (J Oral Pathol Med 2021;50:85)
Negative stains
Molecular / cytogenetics description
- BRAF is the most frequently mutated gene; the most frequent mutation is BRAF V600E (Tumour Biol 2015;36:5649, Orphanet J Rare Dis 2020;15:316)
- Molecular abnormalities involving ALK or TP53 may also occur but are less common (Oral Surg Oral Med Oral Pathol Oral Radiol 2014;118:e146, Oral Oncol 2022;132:105946)
- TERT promoter mutations are uncommonly identified (J Oral Pathol Med 2023;52:271)
Sample pathology report
- Bone, left mandible and level 1 neck contents, radical resection:
- Ameloblastic carcinoma (8.2 cm) (see comment)
- Tumor necrosis: present
- Mitotic rate: 15 per 2 mm2
- Soft tissue invasion: present
- Perineural invasion: not identified
- Lymphovascular invasion: not identified
- Specimen surgical margin status
- All surgical margins negative for carcinoma
- Carcinoma, 2 mm from nearest margin; posterior soft tissue
- Level I neck contents
- 6 lymph nodes, negative for carcinoma (0/6)
- Submandibular salivary gland with reactive changes
- Comment: At present, there is no universally accepted pathologic staging protocol for ameloblastic carcinoma, reflecting the rarity of this malignancy. In view of this limitation, a detailed summary of histopathologic features with potential relevance to clinical management is provided above.
Differential diagnosis
- Ameloblastoma:
- May share some of the same histological features (peripheral palisading, reverse polarization, stellate reticulum) but should not show features of malignancy (pleomorphism with hyperchromasia, atypical mitoses)
- Maxillary ameloblastoma can show high cellularity but is less commonly BRAF mutated
- Oral squamous cell carcinoma:
- Ideally exhibits surface dysplasia; mucosal precursor lesion
- May invade underlying bone but uncommonly is centered within the bone of the jaw
- Displays prominent intercellular bridges, a hallmark of squamous differentiation
- BRAF V600E negative
- Clear cell odontogenic carcinoma (Am J Surg Pathol 2013;37:1001):
- Malignant epithelial odontogenic tumor composed primarily of nests and islands of clear cells
- May have focal peripheral palisading similar to ameloblastoma but typically lacks the cytologic atypia seen in ameloblastic carcinoma
- EWSR mutation
Additional references
Practice question #1
When confronted with an intraosseous mandibular epithelial tumor, which collection of microscopic features is most suggestive of ameloblastic carcinoma?
- Acantholysis, dyskeratosis, extensive ghost cell type keratinization
- Cellular atypia, increased mitotic activity, tumor necrosis
- Fibrous stroma, psammoma bodies, multinucleated giant cell reaction
- Perineural invasion, clear cytoplasm, EWSR1 mutation
Practice answer #1
B. Cellular atypia, increased mitotic activity, tumor necrosis would be most suggestive for ameloblastic carcinoma of the available choices. Answer A is incorrect because extensive ghost cell type keratinization is more commonly seen in odontogenic ghost cell tumors and not typically in ameloblastic carcinoma. Answer C is incorrect because fibrous stroma, psammoma bodies and multinucleated giant cell reaction are often described in papillary thyroid carcinoma and are unrelated to ameloblastic carcinoma. Answer D is incorrect because perineural invasion, clear cytoplasm and EWSR1 mutation are features of clear cell odontogenic carcinoma, not ameloblastic carcinoma.
Comment Here
Reference: Ameloblastic carcinoma
Comment Here
Reference: Ameloblastic carcinoma