Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Ma L. Chronic histiocytic intervillositis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/placentachronicintervillositis.html. Accessed August 11th, 2025.
Definition / general
- Inflammatory disorder characterized by an infiltrate of maternal mononuclear cells, mainly macrophages and few lymphocytes, in the intervillous space
Essential features
- Presence of intervillous histiocytic infiltrate
- Infectious etiologies should be excluded
- Strongly associated with fetal growth restriction, recurrent spontaneous abortions and stillbirth
Terminology
- Chronic intervillositis of unknown etiology
- Massive chronic intervillositis
ICD coding
- ICD-10: O41.1490 - placentitis, unspecified trimester, not applicable or unspecified
Epidemiology
- Can present at any gestational age but is more common in early (first trimester) gestational losses (Hum Pathol 2000;31:1389)
- ~6 per 10,000 second and third trimester placentas (Hum Pathol 2000;31:1389, Eur J Obstet Gynecol Reprod Biol 2009;143:9)
- 4.4% of spontaneous abortions with a normal karyotype (Hum Pathol 1995;26:1245)
- 0.2 - 0.4% of pregnancies with normal outcome (Virchows Arch 2011;459:565, J Perinat Med 2018;46:613)
Sites
- Placenta
Pathophysiology
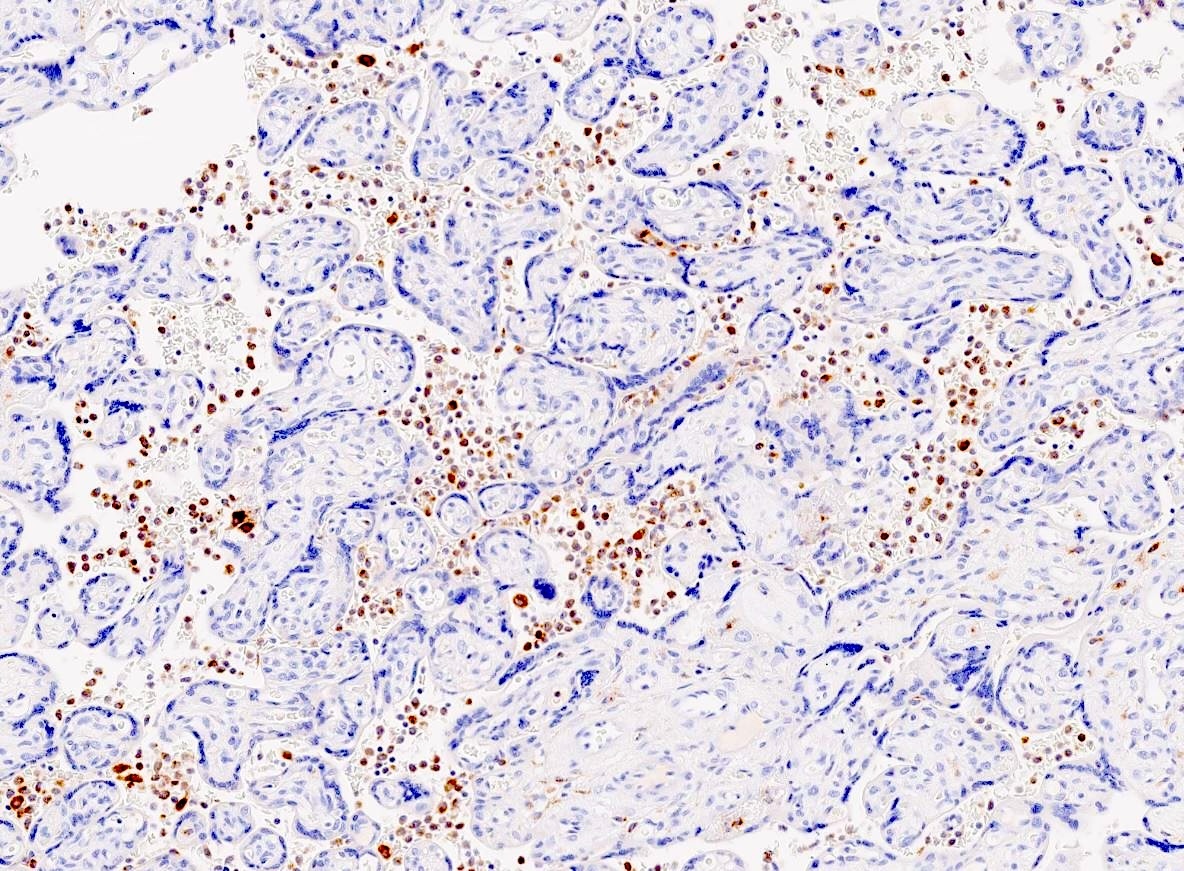
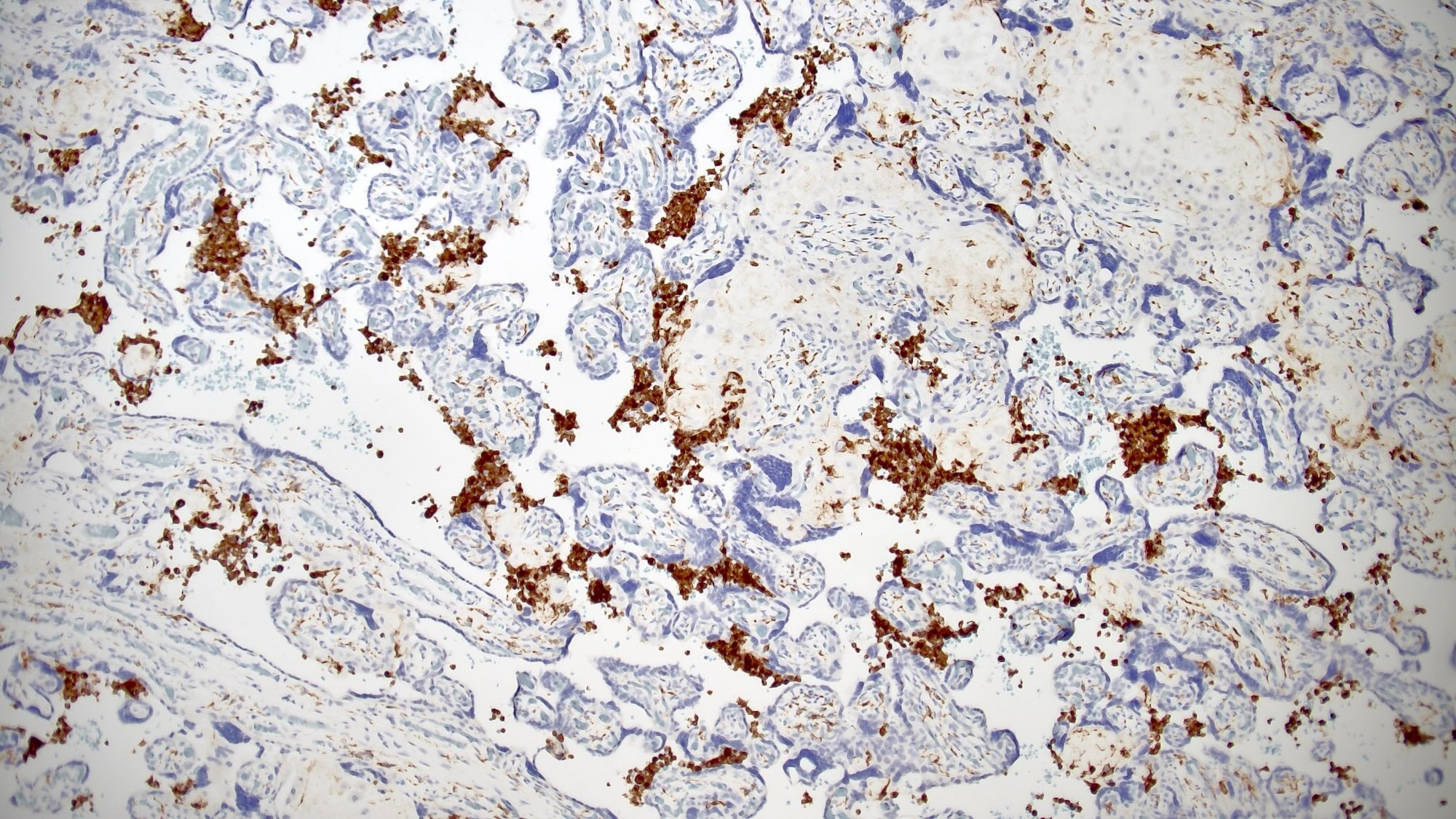
- Maternal CD68+ macrophages and a small proportion of CD4+ and CD8+ T cells infiltrate intervillous space of the placenta, in association with increased fibrin deposition
- Maternal anti-HLA antibodies are hypothesized to interact with (paternal) antigens expressed on the placenta
- Increased deposition of C4d on the surface of syncytiotrophoblasts
- Associated with macrophage recruitment and antibody mediated immune response
- Increased intercellular adhesion molecule 1 (ICAM1) expression by syncytiotrophoblasts
- Hypothesized as a contributory factor in macrophage recruitment
- Reference: Am J Reprod Immunol 2021;85:e13373
Etiology
- Predominant theory is immunologic (excessive maternal inflammation directed towards the placenta) given the following
- Inflammatory cells are maternal (Placenta 2010;31:1116)
- Association with maternal autoimmune diseases (Autoimmunity 2015;48:40, Placenta 2011;32:140)
- Association with neonatal alloimmune thrombocytopenia (Placenta 2016;48:104)
Clinical features
- Usually multigravidas with obstetric history of perinatal losses, including spontaneous abortions, stillbirths, fetal growth restriction and neonatal deaths
- In one series, 93% of women with chronic histiocytic intervillositis reported such history (Placenta 2018;64:1)
- Preterm deliveries are common, many due to severe fetal growth restriction (Hum Pathol 2000;31:1389)
- Associated maternal autoimmune diseases in up to 29% of cases (Autoimmunity 2015;48:40)
- May be associated with assisted reproduction induced pregnancy (Placenta 2010;31:1116)
- Associated with specific rare fetal diseases
- Several cases of neonatal alloimmune thrombocytopenia, chromosomally or syndromically anomalous fetuses and fetal skeletal anomalies (Pediatr Dev Pathol 2013;16:32, Hum Pathol 2000;31:1389, Am J Med Genet A 2016;170:2960)
Diagnosis
- Microscopic examination of the placenta
Laboratory
- Mothers with gestations affected by chronic histiocytic intervillositis often have elevated alkaline phosphatase (Placenta 2011;32:140)
- Elevated by 2.5x the normal reference range
- Reported in ~50% of cases
- Prognostic significance is unclear
Radiology description
- Abnormal ultrasound findings (Placenta 2018;64:1)
- Abnormal echotexture, echogenic cystic lesions, oligohydramnios and abnormal placental dimensions
- Any 1 of these features reported in only ~44% of cases
- Abnormal uterine artery Doppler results present in 27 - 40% of cases (Placenta 2013;34:149, Placenta 2011;32:140, Placenta 2018;64:1)
Prognostic factors
- High but variable rate of recurrence (25 - 100%) (Placenta 2018;61:80, Placenta 2010;31:1106, Eur J Obstet Gynecol Reprod Biol 2009;143:9)
- Recurrences do not seem to correlate with the severity of clinical sequelae
- Fetal / infant sequelae include significant increase in perinatal mortality
- Spontaneous abortion, intrauterine fetal demise and fetal growth restriction (Hum Pathol 2000;31:1389, Hum Pathol 1995;26:1245)
- Risk factor for transplacental fetal transmission of SARS-CoV-2 (Arch Pathol Lab Med 2021;145:517)
Case reports
- 23 year old gravid woman with COVID-19 infection presented with reduced fetal movements at 25 weeks of gestation (Pediatr Dev Pathol 2021;24:450)
- 32 year old gravid woman with scan at 21 weeks of gestation showing fetal growth restriction and oligohydramnios (J Obstet Gynaecol Can 2017;39:676)
- 41 year old woman with a history of 13 first trimester miscarriages (Malays J Pathol 2020;42:439)
Treatment
- There are no standardized guidelines or validated treatments for subsequent pregnancies
- Literature reports use of steroids, aspirin, low molecular weight heparin, hydroxychloroquine and intravenous immunoglobulin (IVIG)
- Reference: Am J Obstet Gynecol 2023;228:187
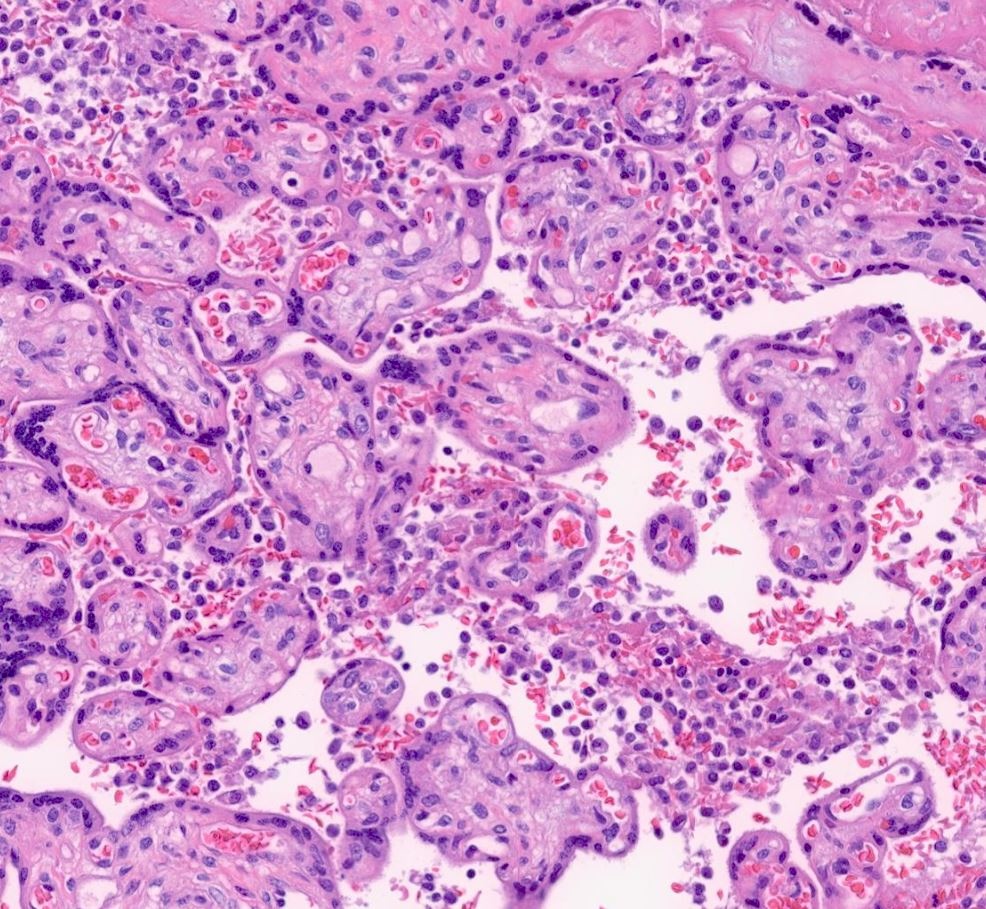
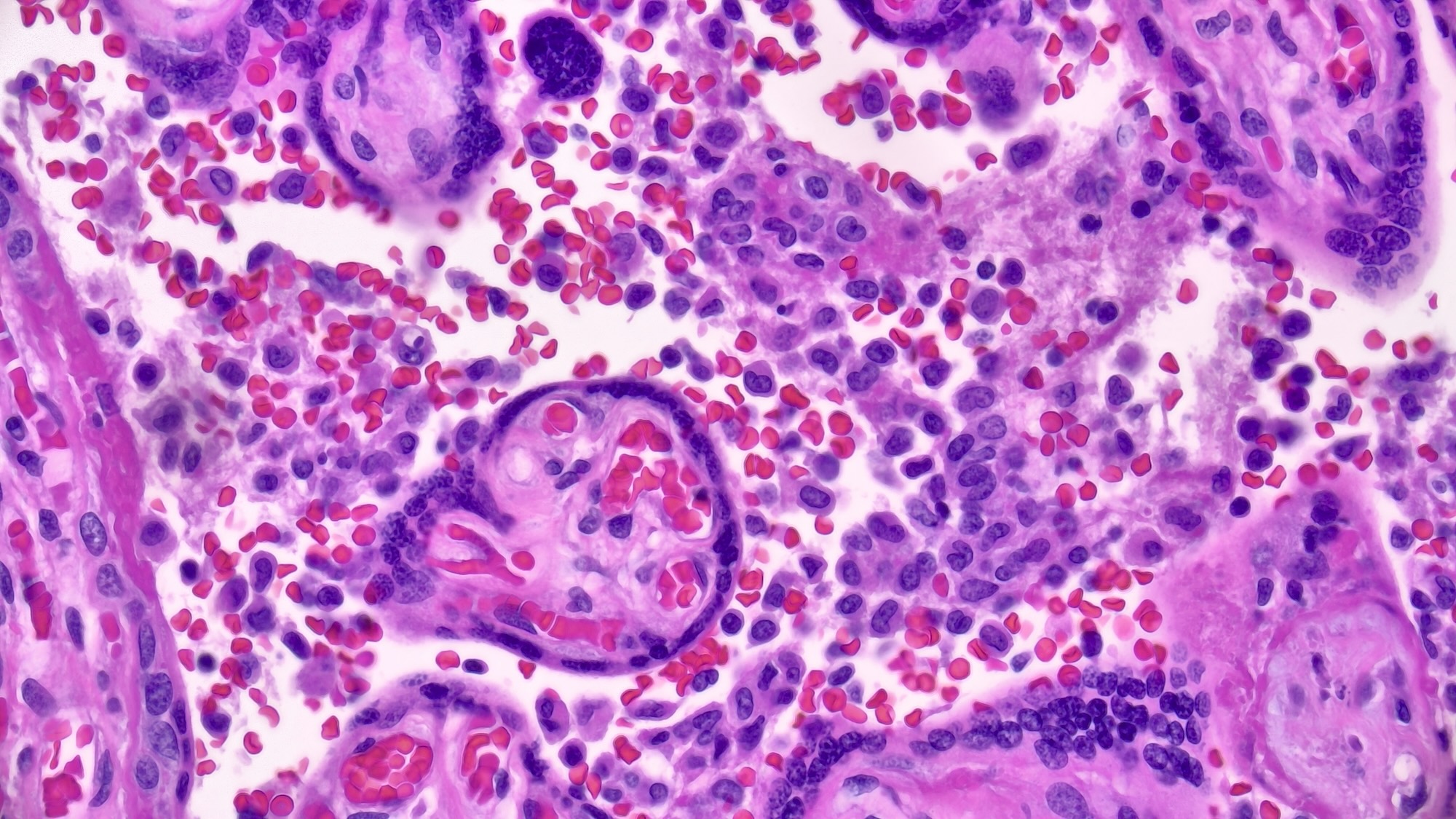
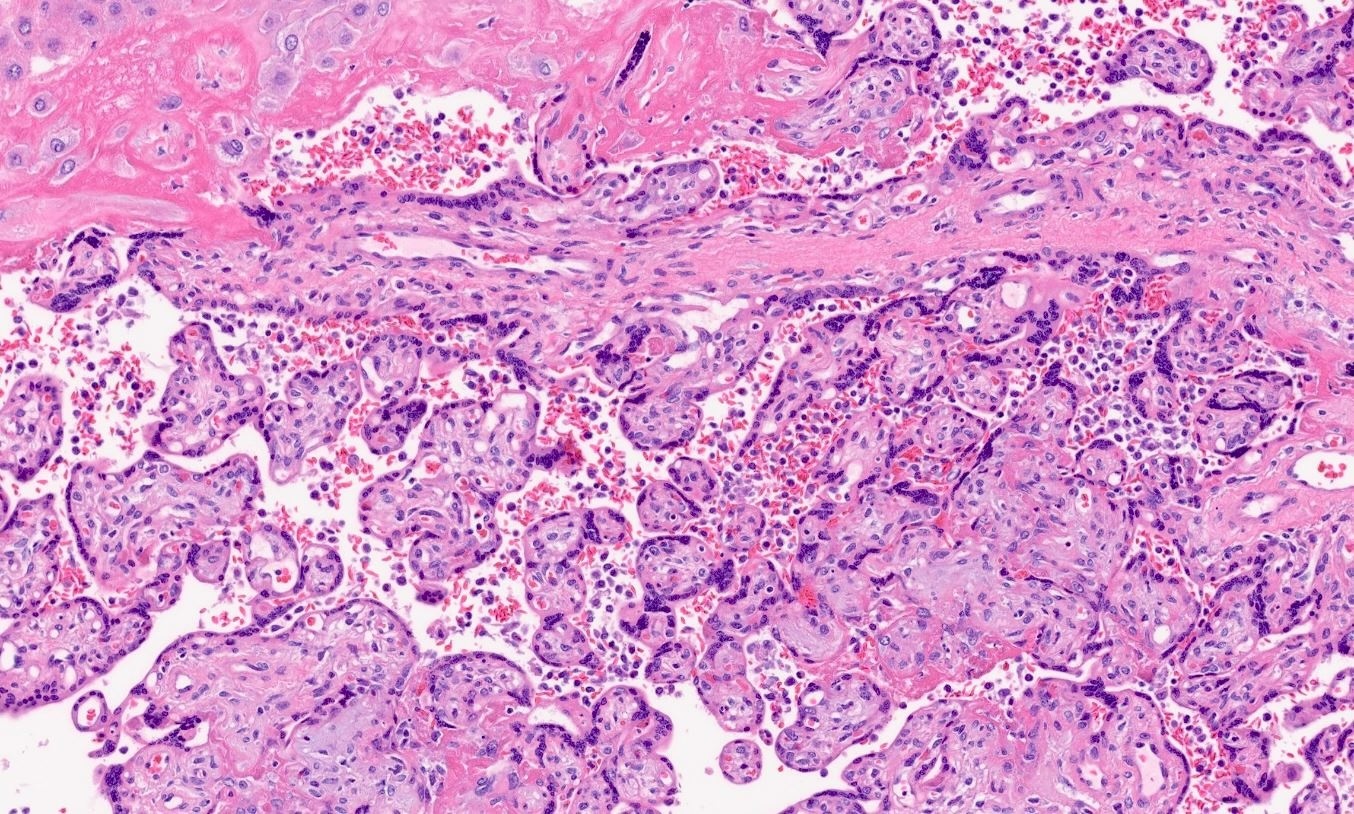
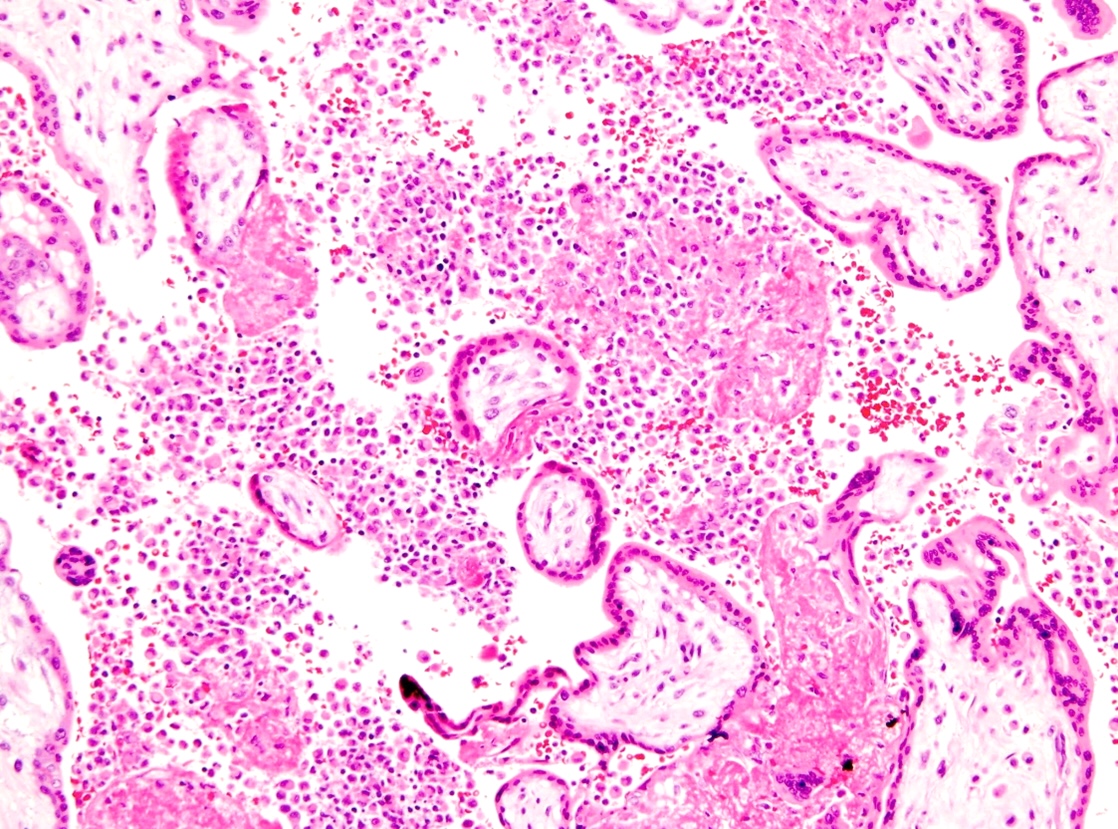
Microscopic (histologic) description
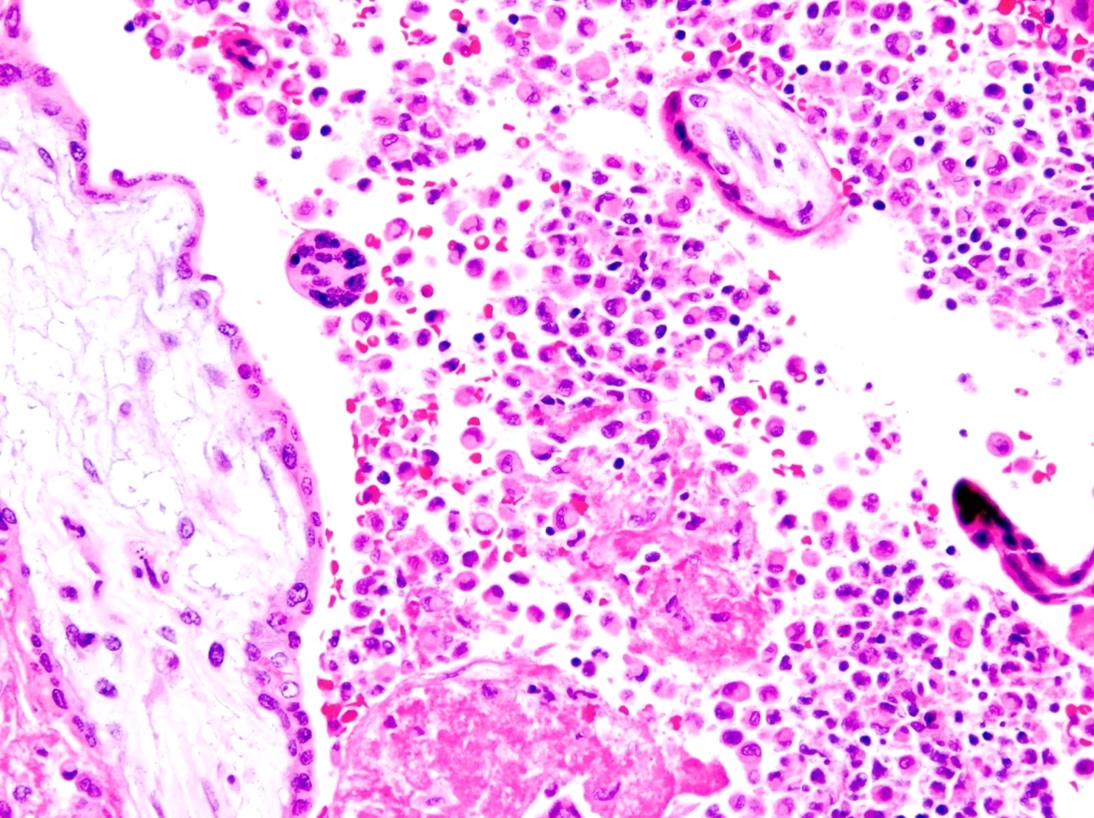
- Presence of an infiltrate of mononuclear cells, mainly histiocytes and few lymphocytes, in the intervillous space
- Intervillositis is present in at least 5% of the intervillous space
- 80% of infiltrate should be CD68+ histiocytes
- Associated increased perivillous or intervillous fibrin deposition is often seen but not essential for diagnosis
- Chronic villitis may be present but is much less prominent than the histiocytic intervillositis
- Villous trophoblast necrosis may be present to varying degrees
- Reference: Placenta 2018;61:80
Microscopic (histologic) images
Positive stains
Sample pathology report
- Placenta, cesarean section:
- Mature third trimester placenta
- Chronic histiocytic intervillositis (see comment)
- Fetal membranes with no significant pathologic change
- Unremarkable 3 vessel umbilical cord
- Comment: A CD68 immunostain (performed with adequate positive and negative controls) highlights the macrophages in the intervillous space, supporting the diagnosis. Chronic histiocytic intervillositis is an idiopathic inflammatory condition with a high recurrence rate that is characterized by abundant macrophages in the intervillous space and is associated with fetal growth restriction and recurrent miscarriages.
Differential diagnosis
- Chronic villitis, infectious or unknown etiology:
- When present, intervillositis is a minor component (typically < 5% of intervillous space)
- There may be evidence suggesting that they represent a spectrum of the same disorder (Placenta 2015;36:681)
- Massive perivillous fibrin deposition:
- Consists of mostly acellular intervillous fibrin
- Rare intervillositis
- SARS-CoV-2 placentitis:
- Maternal history of acute viral syndrome
- Presence of associated syncytiotrophoblast necrosis
- Infection detected using in situ hybridization or immunohistochemistry
- Placental malaria:
- Presence of histiocytic intervillositis with hemozoin pigment in the histiocytes and perivillous fibrin deposits
- Malaria parasites identified within maternal red blood cells
- Acute chorioamnionitis:
- When present, intervillositis is predominantly neutrophilic
Practice question #1
Practice answer #1
A. Chronic histiocytic intervillositis. The image depicts an infiltrate of histiocytes in the maternal intervillous space, consistent with chronic histiocytic intervillositis.
Answer B is incorrect because massive perivillous fibrin deposition is characterized by excessive acellular fibrin deposition, which encases chorionic villi and obliterates the intervillous space.
Answer C is incorrect because mucopolysaccharidosis type I, also known as Hurler syndrome, is a metabolic storage disorder; metabolic storage disorders are characterized by cytoplasmic vacuolization of villous cells, which is not seen here.
Answer D is incorrect because villous stromal vascular karyorrhexis is characterized by nuclear fragmentation and degeneration of villous stromal and endothelial cells, along with the presence of red blood cell fragments. This represents an early stage of distal terminal villous ischemia, which ultimately progresses to avascular villi.
Comment Here
Reference: Chronic histiocytic intervillositis
Comment Here
Reference: Chronic histiocytic intervillositis
Practice question #2
A 35 year old patient delivered a placenta with findings depicted in the image above. Which of the following statements is most likely true?
- The patient has a history of hypertension
- The patient has a history of partial hydatidiform mole
- The patient has a history of positive rapid plasma reagin (RPR) tests
- The patient has a history of recurrent miscarriages
Practice answer #2
D. The patient has a history of recurrent miscarriages. The image depicts an infiltrate of histiocytes in the maternal intervillous space, consistent with chronic histiocytic intervillositis. Chronic histiocytic intervillositis is an idiopathic inflammatory disorder associated with fetal growth restriction, recurrent spontaneous abortion and stillbirth. Answer B is incorrect because chronic histiocytic intervillositis has no association with gestational trophoblastic disease. Answer C is incorrect because a positive RPR is a nonspecific test result for syphilis, which is an infectious process. Answer A is incorrect because the image findings do not show features of maternal vascular malperfusion.
Comment Here
Reference: Chronic histiocytic intervillositis
Comment Here
Reference: Chronic histiocytic intervillositis