Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Videos | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Carreon CK, Roberts DJ. Early first trimester pregnancy loss. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/placentaspontaneousab.html. Accessed September 12th, 2025.
Definition / general
- Early pregnancy loss (EPL) refers to an early, spontaneous, previable pregnancy loss that occurs before 14 weeks gestation
Essential features
- Early first trimester pregnancy loss is a common event and may be recurrent
- Abnormal karyotype occurs in approximately 50% of cases
- Distinction of prominent villous edema (hydropic villous degeneration) from molar gestation is important
Terminology
- Early pregnancy loss
- Spontaneous abortion
- Missed abortion
- 2 subgroups, depending on timing of occurrence (J Clin Pathol 1981;34:819):
- Embryonic (< 10 weeks)
- Fetal (> 10 weeks)
- Spontaneous / missed abortion refers to a nonviable intrauterine pregnancy that often results in passage of placental tissue without an embryo
- Induced abortion refers to termination of pregnancy by artificial means:
- Nonsurgical (medical abortion; e.g., misoprostol)
- Vacuum aspiration
- Dilation and curettage (D&C)
- Dilation and evacuation (D&E)
ICD coding
Epidemiology
- Common event affecting up to 14% of pregnancies with up to as high as 66% of detectable early pregnancies terminating spontaneously (Lancet 1980;2:554, Fertil Steril 1982;38:447, Epidemiology 1990;1:382)
- Often sporadic (97% of the time) but can be recurrent (defined as 3 or more failed pregnancies) (Clin Obstet Gynecol 2016;59:464)
- Overall, 80% of early pregnancy loss occurs in the first trimester and the risk of miscarriage decreases beyond 12 weeks gestational age (StatPearls: Miscarriage [Accessed 6 January 2022])
Pathophysiology
- Intrinsically abnormal gestation leading to spontaneous loss
- Maternal or environmental factors affecting an otherwise normal gestation
Etiology
- Abnormal karyotype detected in approximately 50% of spontaneous EPL; highest in embryonic (< 10 weeks gestational age) losses, with up to 70% in losses occurring prior to 6 weeks (Ultrasound Obstet Gynecol 2015;45:89)
- Lethal trisomies - 30%: trisomy 16 accounts for 30% of all trisomies
- Monosomy X - 10%
- Triploidy - 2%
- Other etiologies:
- Maternal factors: physiologic or structural conditions (e.g., intrauterine scarring or abnormal septation, masses involving the uterine wall) or active disease process (e.g., autoimmune disorders, endocrinopathy, thrombophilia) (Nat Rev Dis Primers 2020;6:98)
- Teratogen exposure
- Infection (septic abortion)
Clinical features
- Spontaneous passage of blood or tissue (Obstet Gynecol 2009;114:860)
- May be incidentally discovered without associated contractions or vaginal bleeding
- Conceptus with abnormal karyotype can manifest as abnormally low levels of human chorionic gonadotrophin (hCG)
- Failure to develop a yolk sac, fetal pole or reduced chorionic sac diameter
- Absent cardiac activity
- Blighted ovum: often indicates pre-embryonic loss; gestational sac is identified but without developing embryonic structures (StatPearls: Anembryonic Pregnancy [Accessed 17 January 2022])
Diagnosis
- Diagnosis may be confirmed by serology (hCG levels), ultrasound findings and microscopic tissue analysis
Laboratory
- Inappropriately low hCG levels for gestational age
Radiology description
- Ultrasound findings that are diagnostic of or suspicious for early pregnancy failure (Radiopaedia: Failed Early Pregnancy [Accessed 10 January 2022])
Prognostic factors
- Sporadic cases are often followed by successful pregnancies
- For recurrent EPL, the mother, her partner and products of conception must be evaluated for cytogenetic, anatomic, hormonal or immunologic causes of pregnancy failure (StatPearls: Anembryonic Pregnancy [Accessed 17 January 2022])
Case reports
- 28 year old woman with pregnancy loss at 9 weeks gestation with subsequent maternal fever, arthralgia and rash and pancytopenia (BMJ Case Rep 2021;14:e243968)
- 30 year old woman with 2 consecutive miscarriages within a 7 month period (Int J Gynecol Pathol 2016;35:38)
- 30 and 34 year old women with cases of first trimester miscarriages with double trisomies (Fetal Diagn Ther 2008;24:106)
Treatment
- Surgical removal of products of conception by D&C, D&E or vacuum aspiration (Rev Obstet Gynecol 2011;4:5)
- Labor induction by misoprostol (prostaglandin E1 analog)
- Watchful waiting for complete expulsion of products of conception
- Treatment of underlying disease (etiology specific management) for recurrent EPL
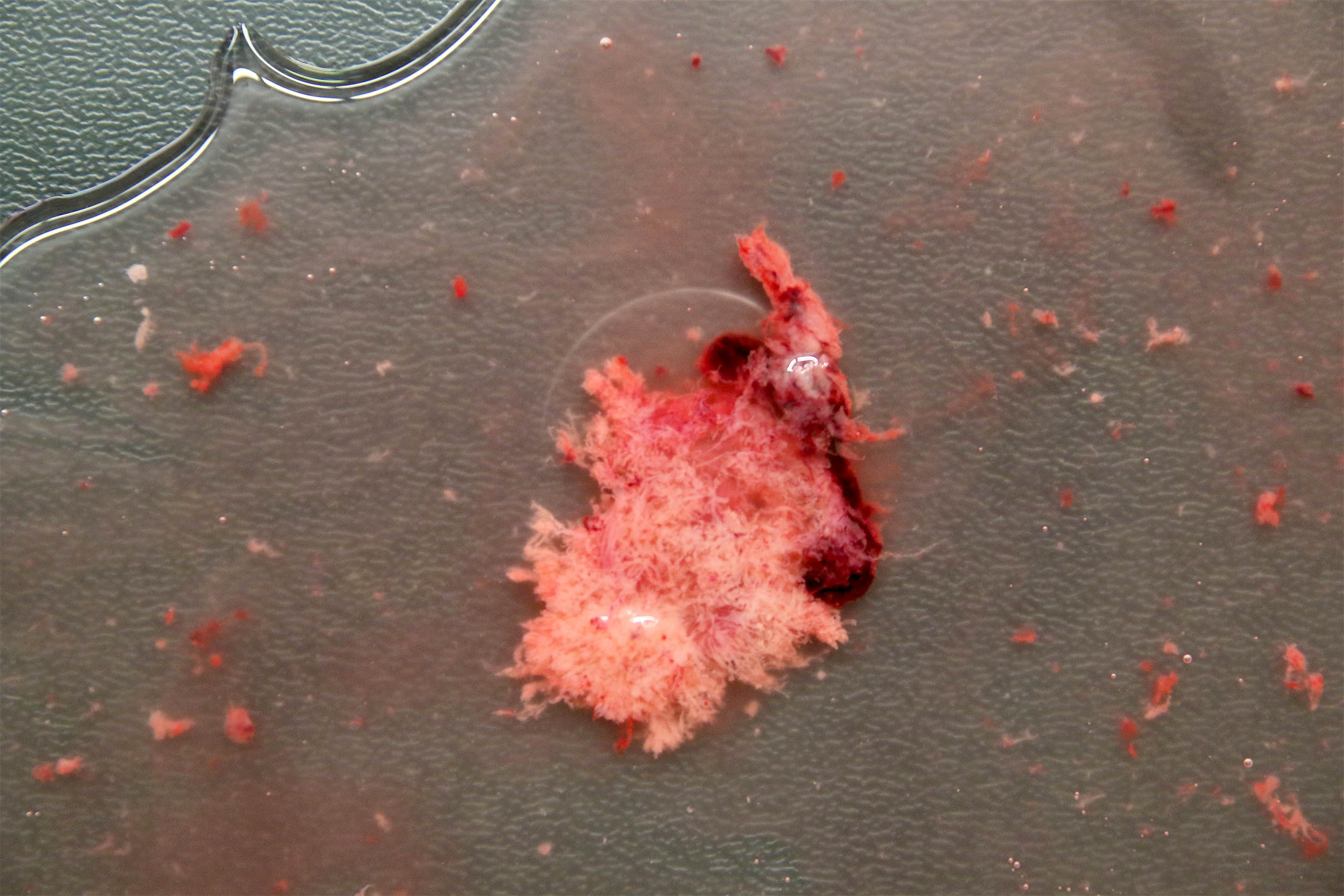
Gross description
- Specimen often consists of fragments of placental tissue (chorionic villi, membranes / gestational sac that may be intact or disrupted and decidua)
- Despite identification of embryo or fetus on ultrasound, an embryo is often not identified / recognized in surgical specimens (J Clin Pathol 1981;34:819)
Gross images
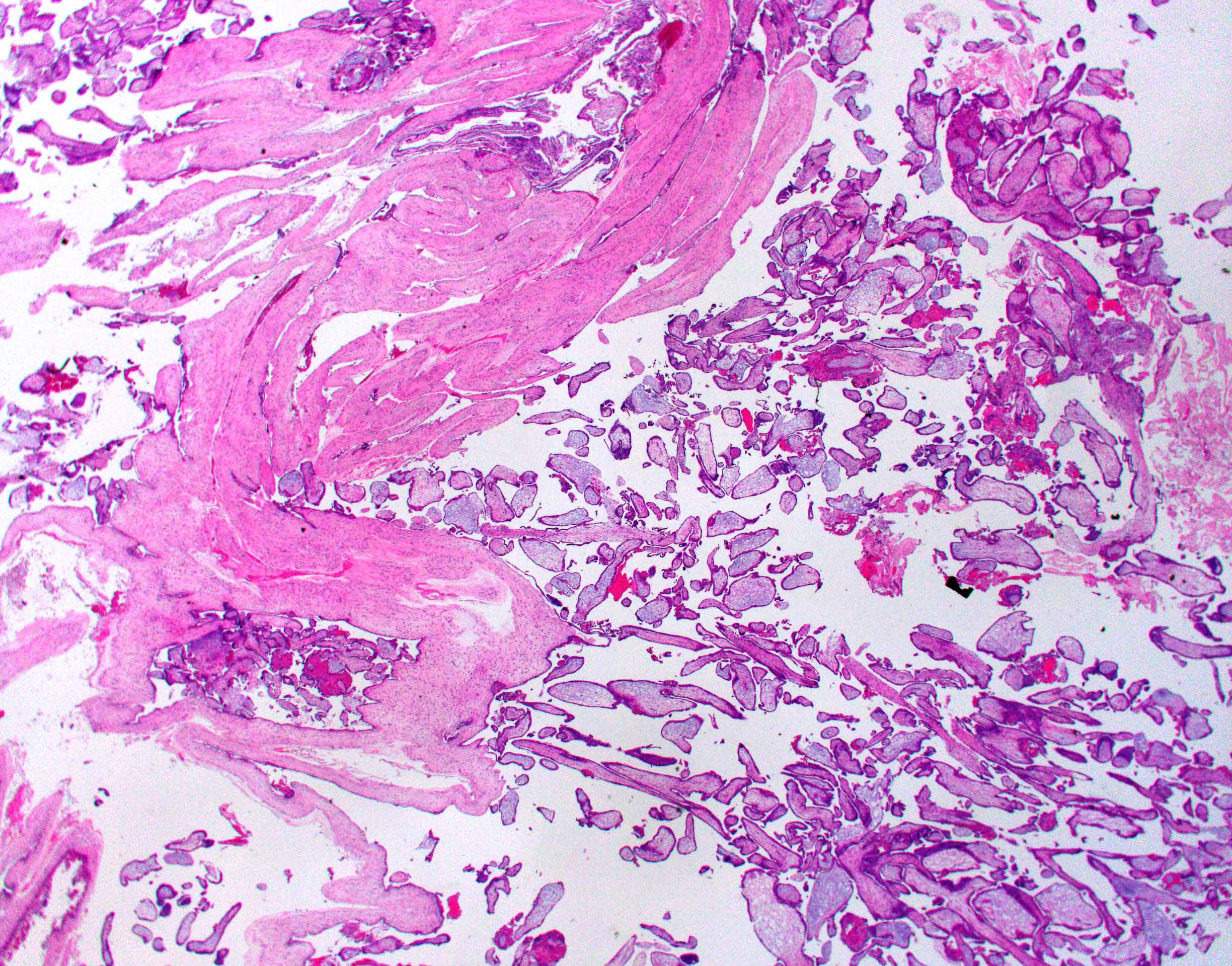
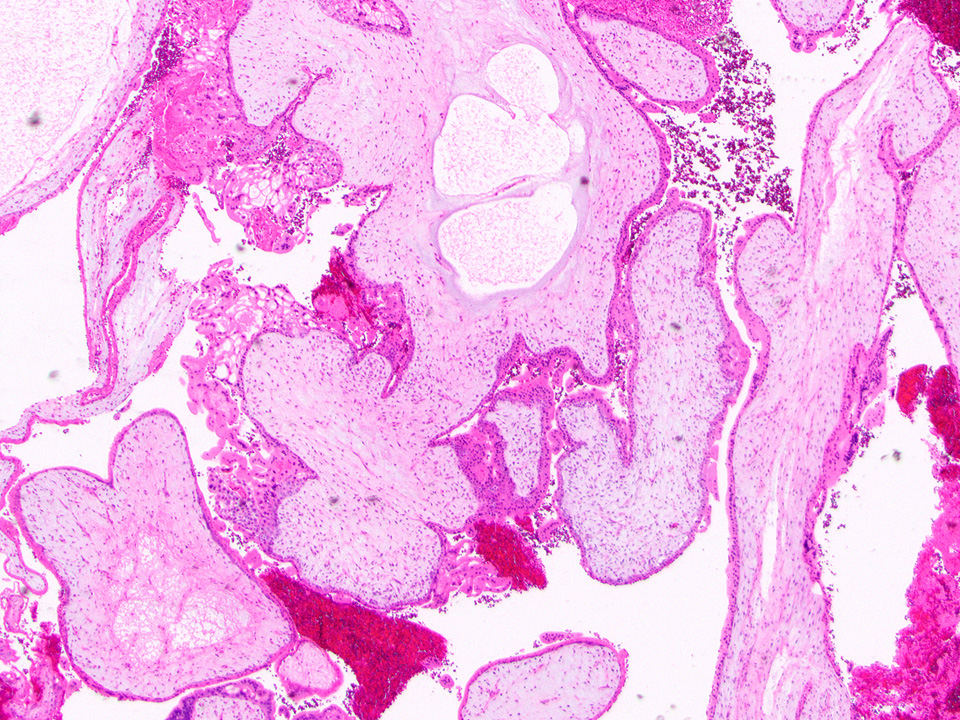
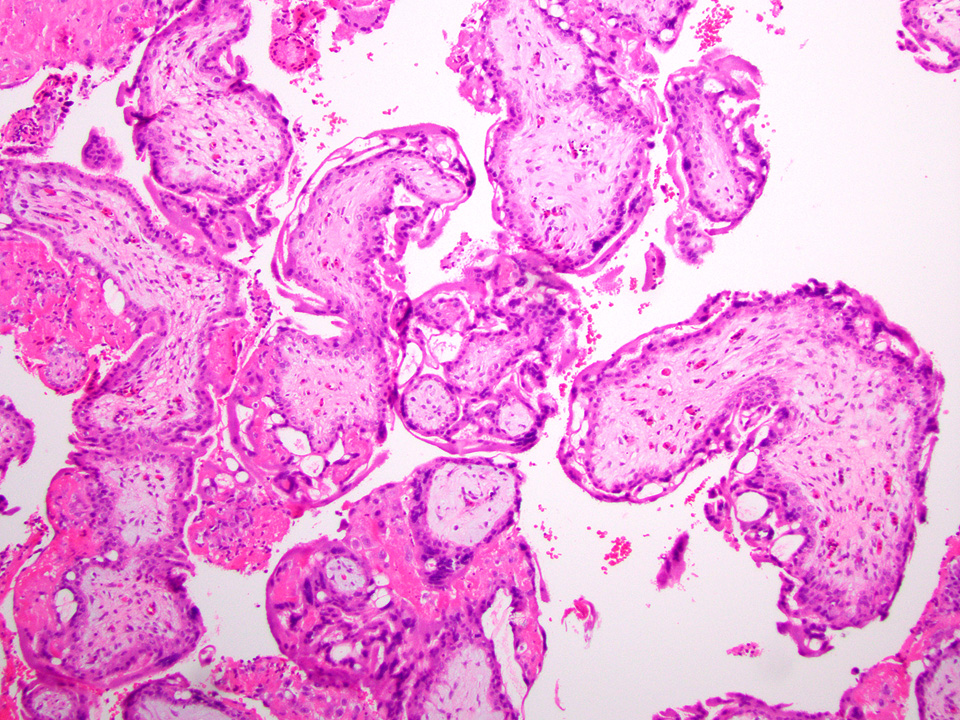
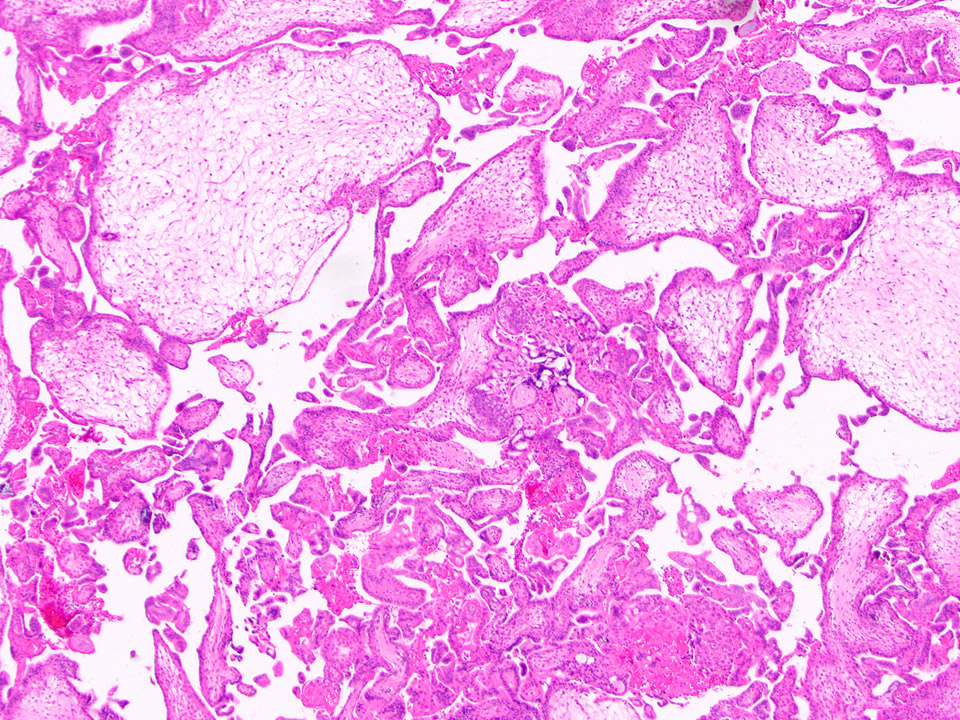
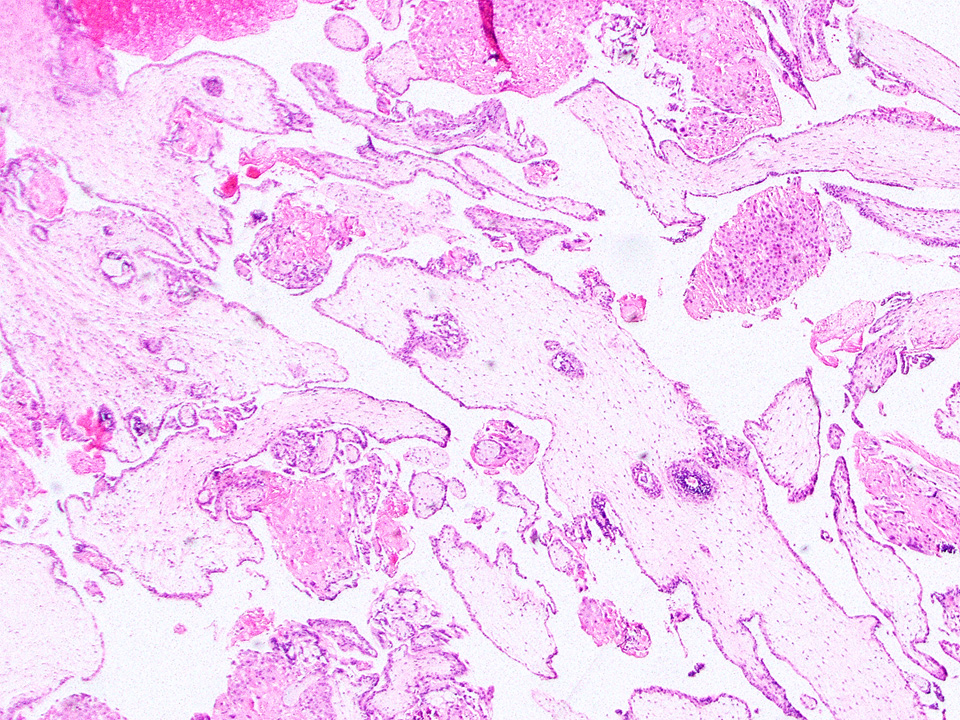
Microscopic (histologic) description
- Removed or passed products of conception may contain:
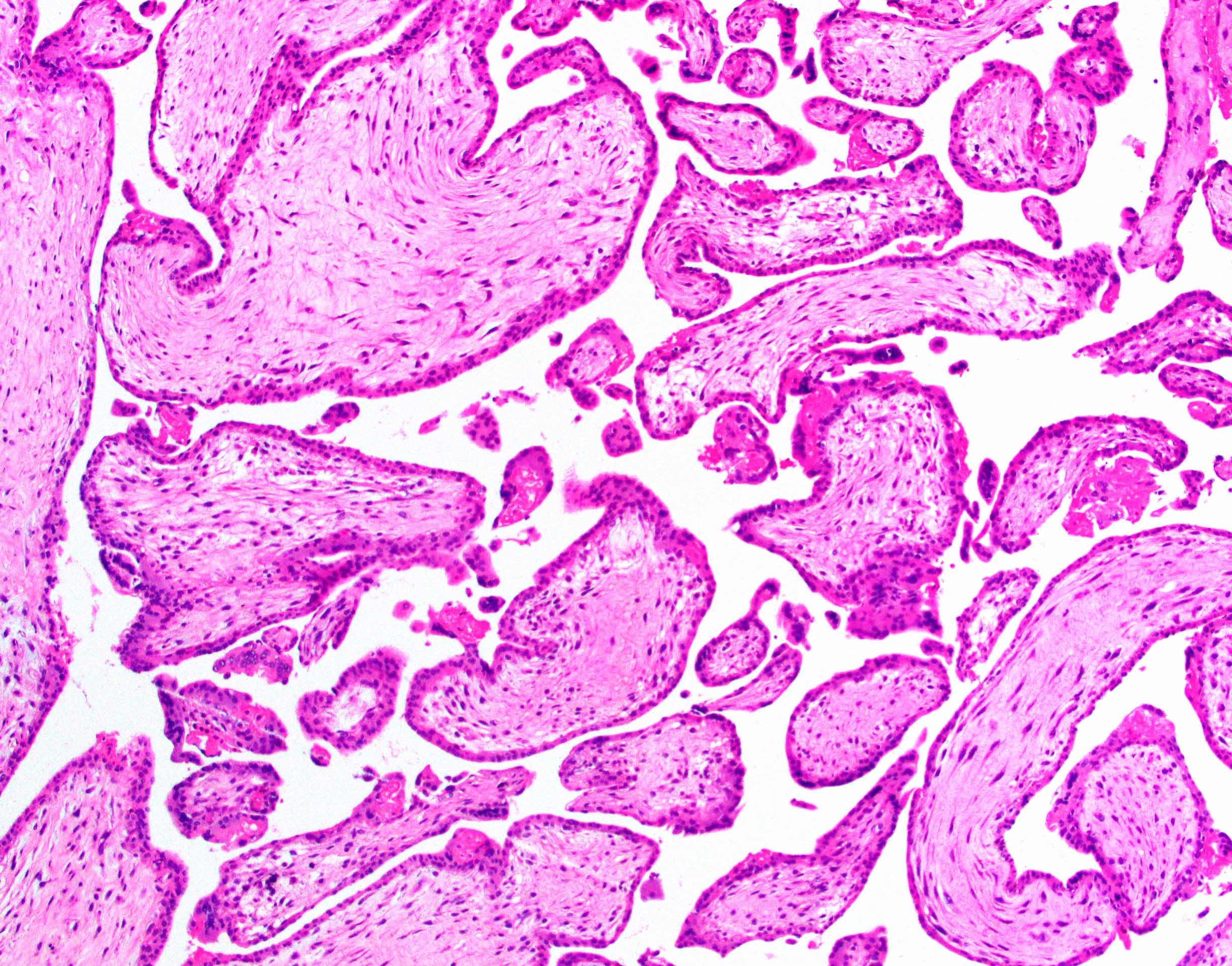
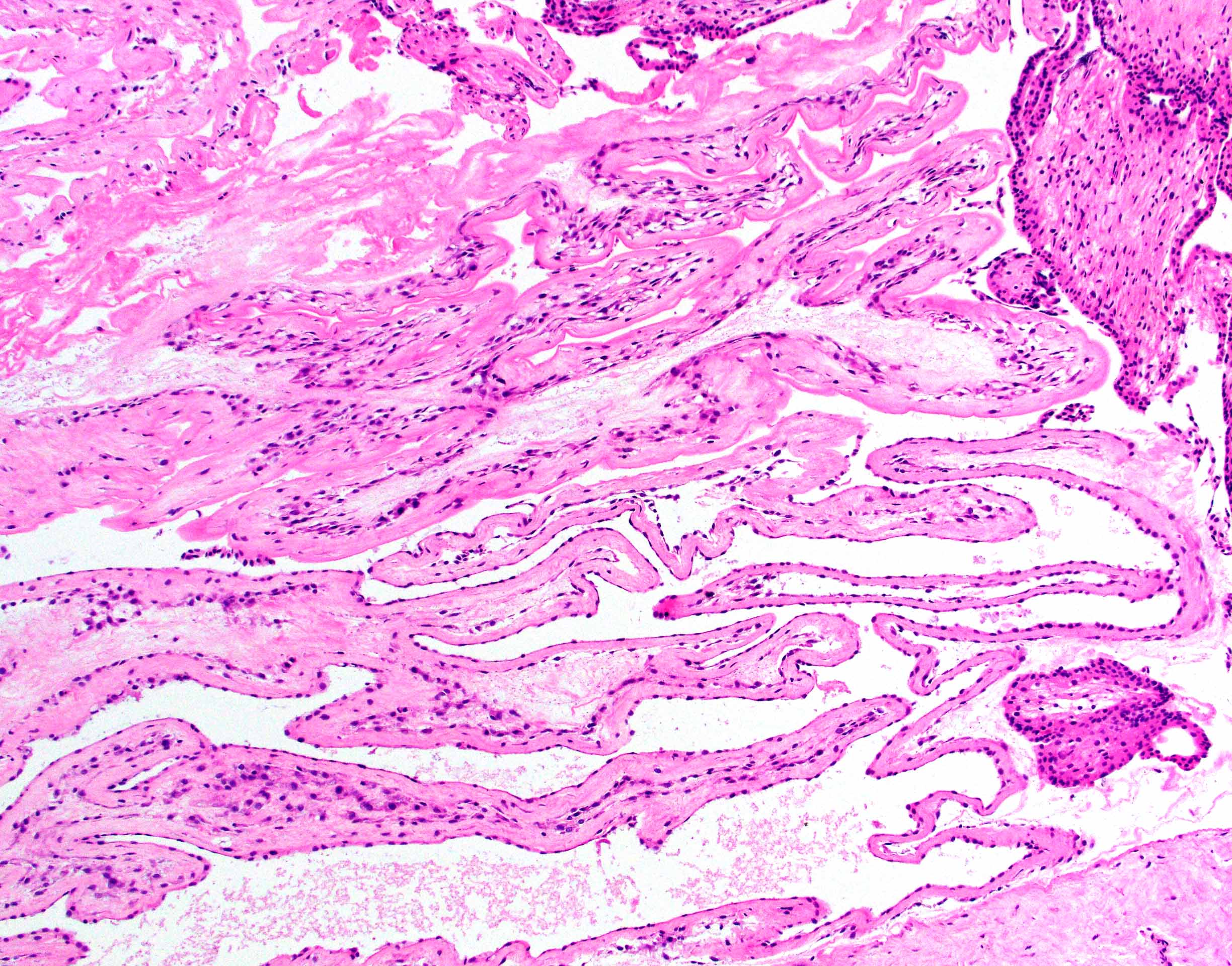
- Early first trimester chorionic sac (< 8 weeks): thin chorion and scant villi that are sparsely or nonvascularized
- Villous trophoblast is bilayered (mononuclear cytotrophoblast inner layer and multinucleated syncytiotrophoblast outer later) and circumferential with occasional polarized trophoblast protrusions
- Mid first trimester chorionic sac (8 - 10 weeks): may exhibit recognizable amnion, early stromal collagenization of chorion and proximal villi and increased volume of distal villi with distinct capillaries
- Later first trimester chorionic sac (> 10 weeks): may exhibit loose fusion of amnion and chorion, a more collagenized chorion and stem villi, more distinct walls of fetal vessels and numerous villi with increasing demarcation between proximal and distal branches
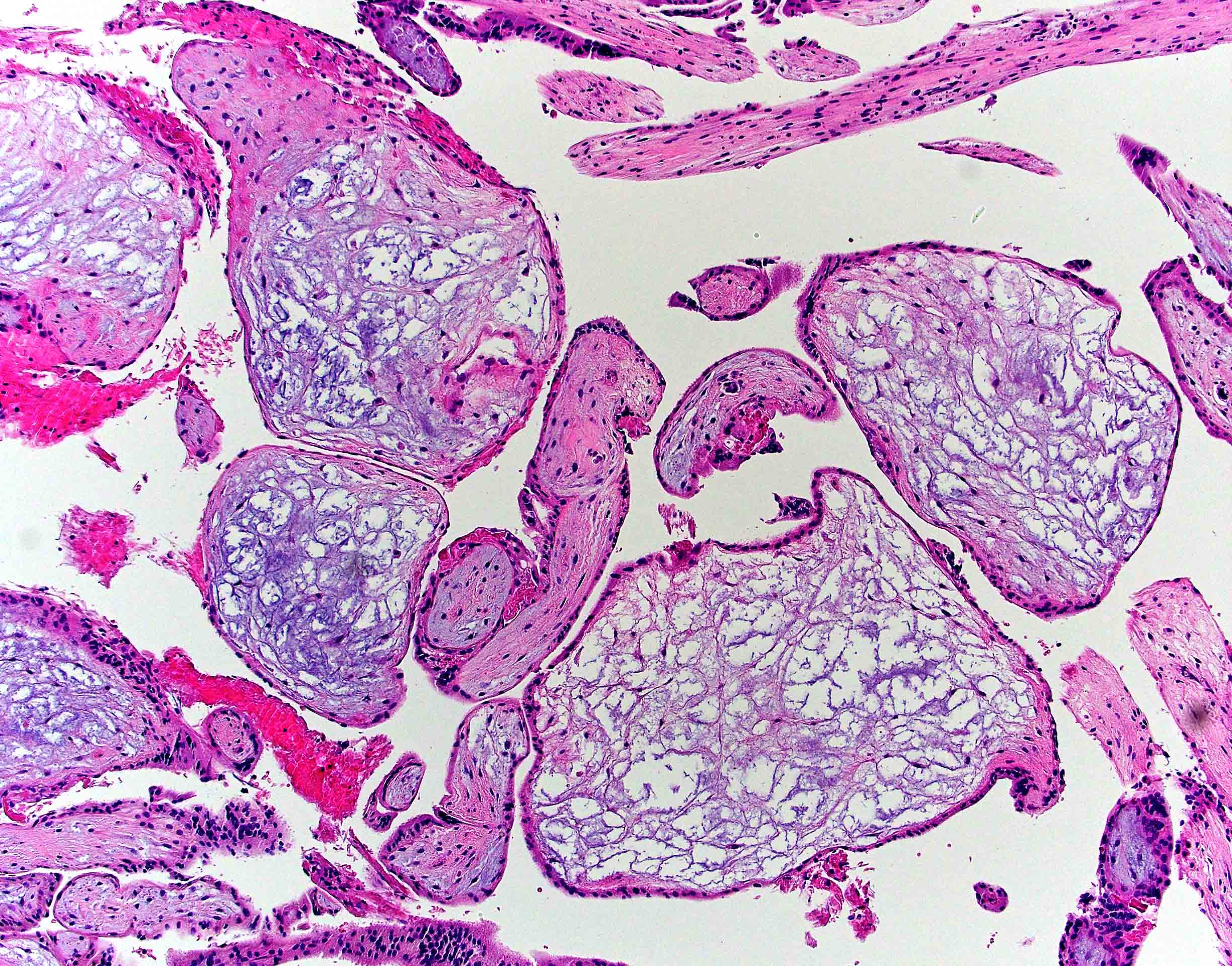
- Spectrum of villous changes in immature chorionic villi following embryonic death (Placenta 2005;26:114):
- Cellular debris within villous vessels - earliest change
- Villous edema with myxoid stromal degeneration - may be confused with molar gestation
- Collagenized avascular villi (villous sclerosis / fibrosis)
- Villous edema and sclerosis / fibrosis often coexist
- Other findings: prominent perivillous fibrin with prolonged retention or in medical abortions, otherwise pathologic
- Spectrum of villous morphology in nonmolar abnormal karyotype (Hum Pathol 1995;26:201):
- Dysmorphic appearance (lacks sensitivity and specificity): highly irregular villous shapes / outlines, occasional trophoblastic inclusions
- Gestational / decidualized endometrium:
- Not uncommon to see inflammatory cells, especially lymphocytes but not plasma cells (plasma cells are pathologic)
- Variable amount of decidual necrosis with inflammatory debris
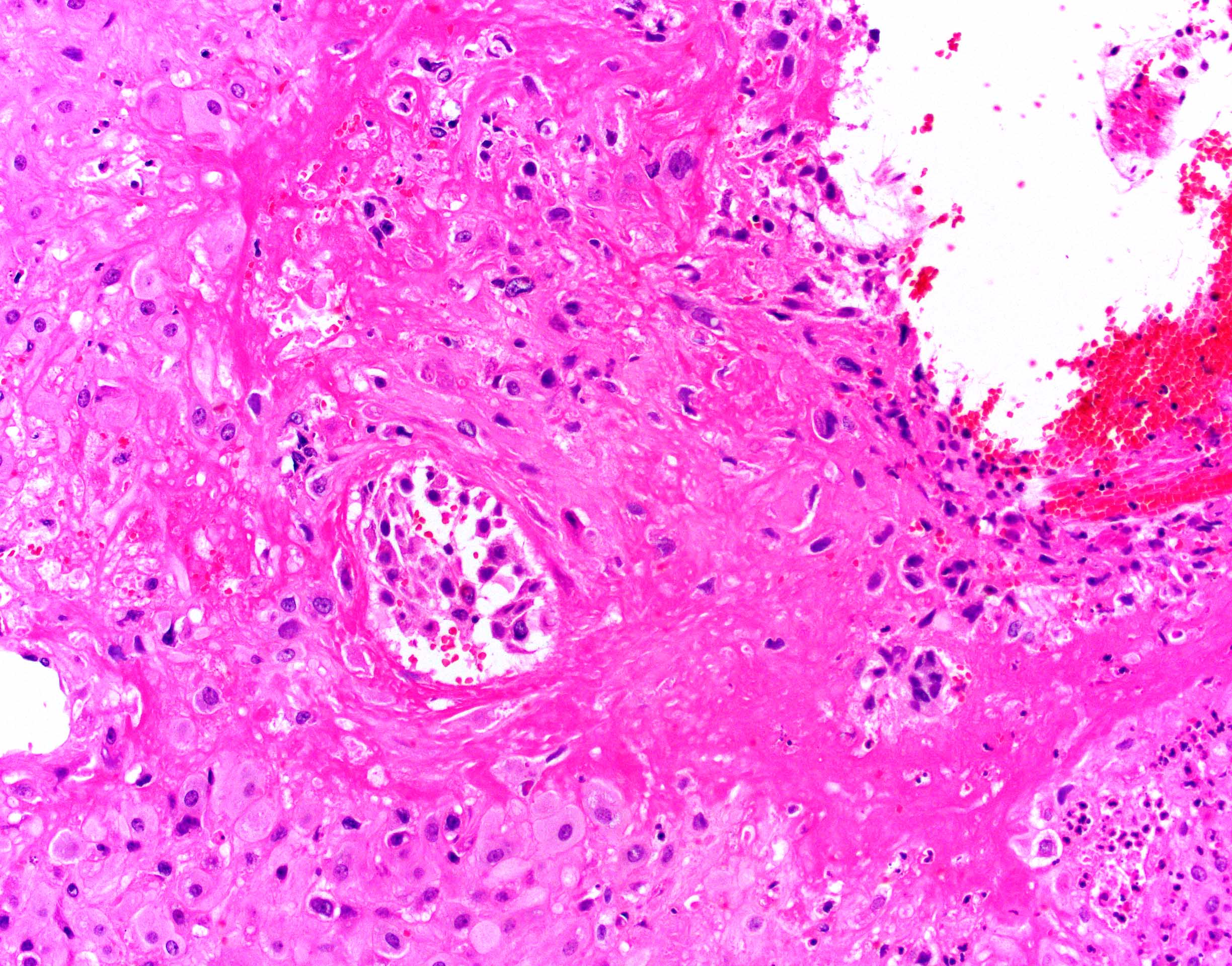
- Placental implantation site:
- Extravillous trophoblast (EVT) within decidualized endometrium, visible maternal vascular remodeling, fibrinoid material in decidua, EVT within vascular wall or within vessel lumens
- Confirms intrauterine pregnancy even in the absence of chorionic villi
- Be careful with interpreting rare villi or syncytiotrophoblast in the absence of implantation site as this could indicate, although rarely, villous migration from a tubal pregnancy
- Other recognizable pathologies (intervillous / maternal space should be empty; if material is present, rule out these pathologies) (Hum Reprod 2007;22:313):
- Chronic histiocytic intervillositis (Malays J Pathol 2020;42:439)
- Massive perivillous fibrin deposition (look for extravillous trophoblast proliferation; otherwise, increased fibrin may be seen with embryonic demise secondary to prolonged retention in utero or secondary to medical abortions)
- Infectious etiologies: marked chronic lymphoplasmacytic or acute inflammation within the maternal vascular space or causing villitis (septic abortions - a critical value)
- Reference: Fetal Pediatr Pathol 2018;37:191
Microscopic (histologic) images
Contributed by Chrystalle Katte Carreon, M.D. and Drucilla J. Roberts, M.D.
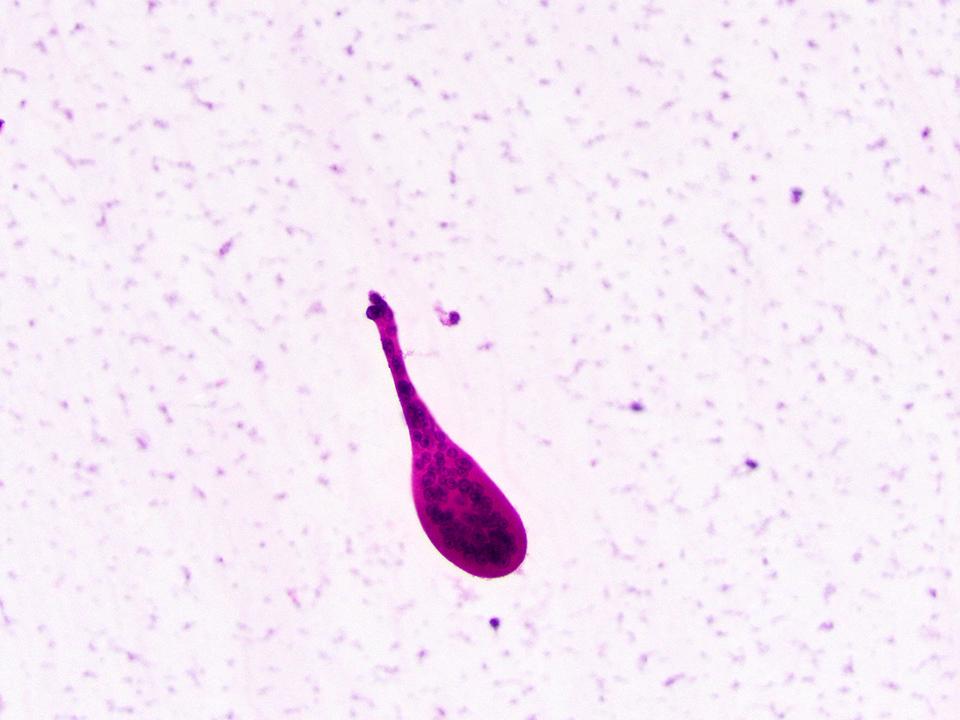
Cytology description
- Although not routinely performed, cytologic analysis may, on some occasions, aid in the identification of rare trophoblast cells, which supports the clinical impression of intrauterine pregnancy
Videos
PathCast: products of conception by Dr. Vanda Torous
Sample pathology report
- Products of conception, D&E:
- Fragments of necrotic immature chorionic villi
- Decidua with patchy necrosis and placental implantation site
- Products of conception, spontaneously passed:
- Necrotic, empty gestational sac
- Necrotic decidua with placental implantation site
- Uterine contents, D&E:
- Decidualized endometrium
- No chorionic villi or trophoblast present; entire specimen examined (see comment)
- Comment: Pregnancy has not been confirmed and ectopic pregnancy cannot be excluded. Clinical correlation is necessary.
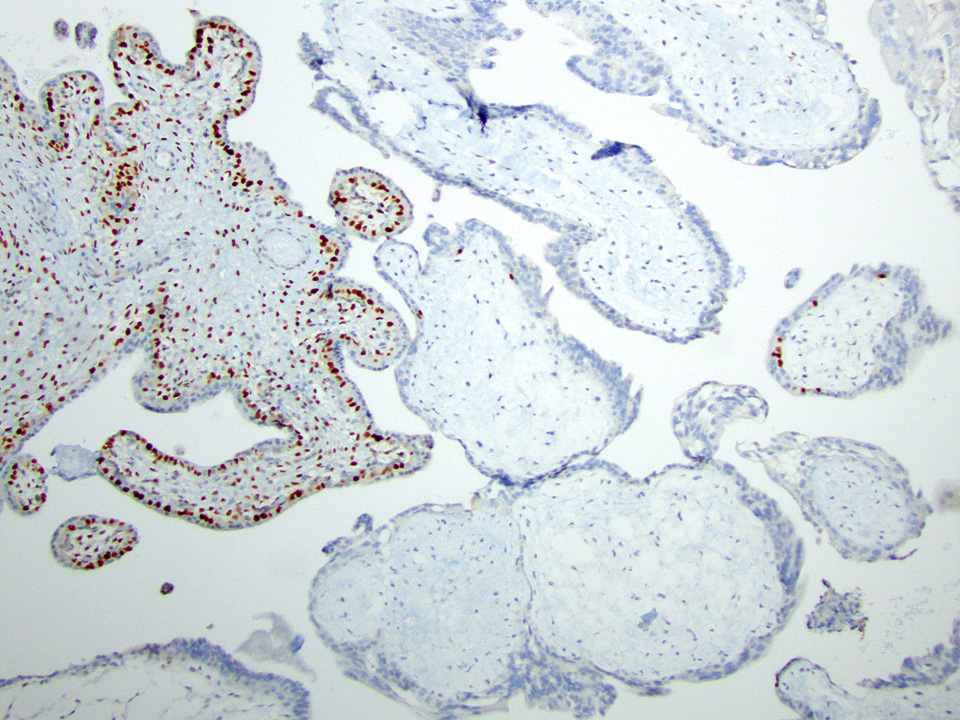
Differential diagnosis
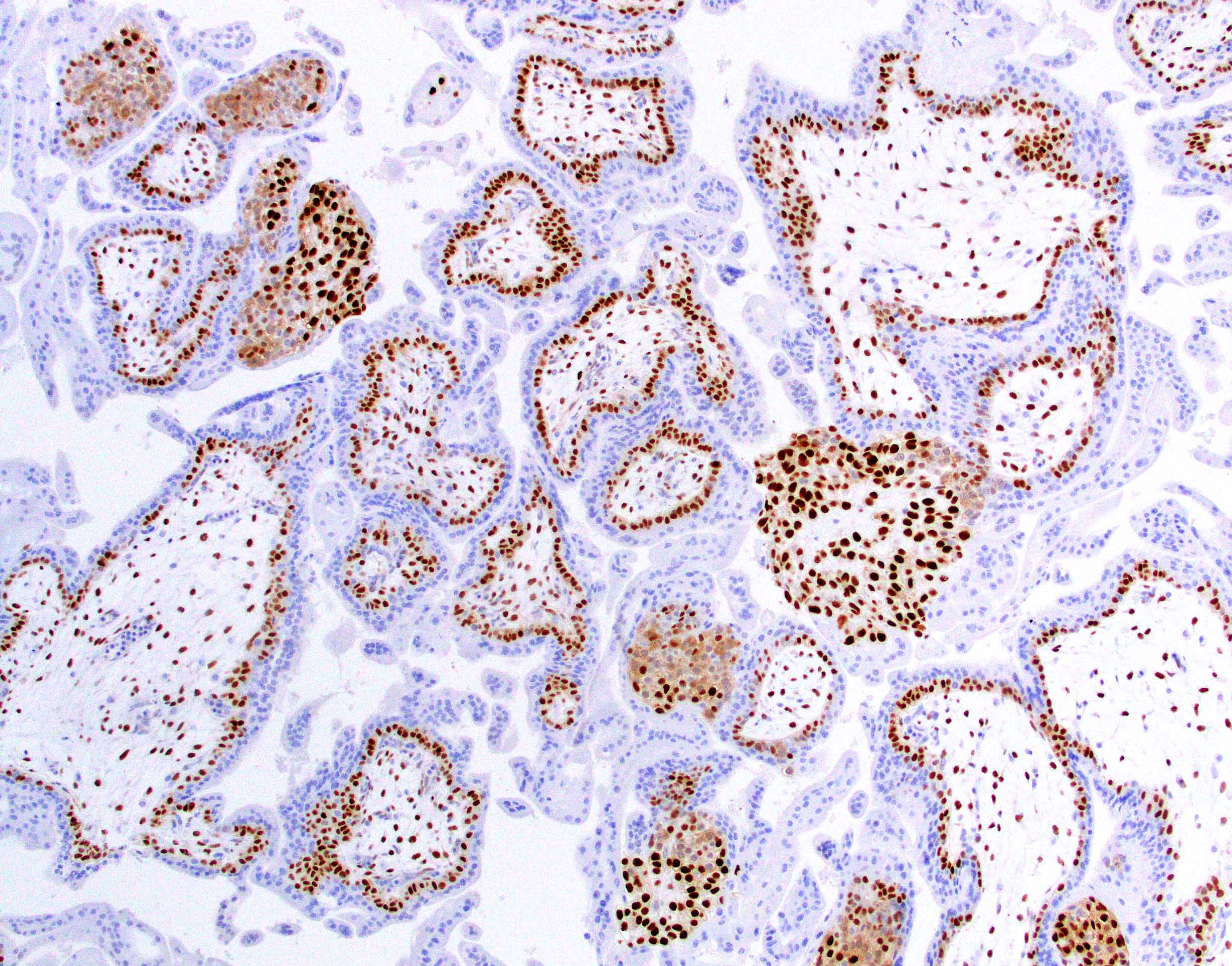
- Hydatidiform mole (Int J Gynaecol Obstet 2021;155:86, Hum Pathol 1998;29:505, Hum Pathol 1996;27:708):
- Complete mole:
- Gestational trophoblastic disease characterized by diffuse hydropic enlargement of chorionic villi with associated trophoblastic hyperplasia
- Distinguishing features
- Uniformly enlarged chorionic villi
- Marked and often circumferential trophoblast proliferation, both cytotrophoblastic and syncytiotrophoblastic
- Loss of the normal nuclear p57 staining in cytotrophoblasts and villous stromal cells; therefore, p57 immunostain is often helpful in distinguishing complete mole (absence of the normal pattern of staining in chorionic villi) versus edematous villi (normal pattern of staining with nuclear staining in villous cytotrophoblasts and stromal cells
- Distinguishing features
- Gestational trophoblastic disease characterized by diffuse hydropic enlargement of chorionic villi with associated trophoblastic hyperplasia
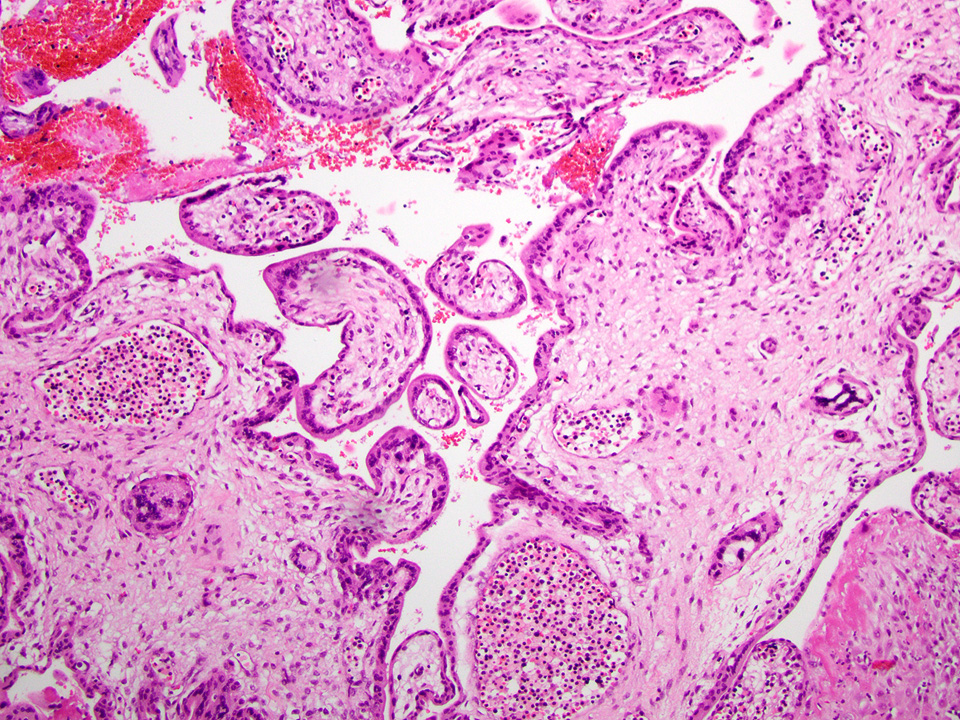
- Partial mole:
- Gestational trophoblastic disease characterized by an admixture of normal and enlarged chorionic villi with irregular contours and mild trophoblastic hyperplasia
- Distinguishing features
- Chorionic villi of different sizes
- Mild focal to circumferential, syncytiotrophoblastic hyperplasia
- Scalloped villous outlines
- Trophoblast inclusions
- Excess tissue grossly
- Retained normal p57 staining pattern; therefore, p57 immunostain will not distinguish a partial hydatidiform mole from a nonmolar gestation
- Flow cytometry for ploidy analysis; partial hydatidiform moles are nearly always triploid (Mod Pathol 1995;8:775, Hum Pathol 2000;31:914)
- Distinguishing features
- Aneuploid nonmolar conceptions can be challenging to distinguish from a partial mole because of overlapping histomorphology but can be differentiated from a partial hydatidiform mole by carefully searching for partial mole features as described above
- Gestational trophoblastic disease characterized by an admixture of normal and enlarged chorionic villi with irregular contours and mild trophoblastic hyperplasia
- Complete mole:
Additional references
Practice question #1
Which of the following is rarely present in early product of conception specimens?
- Decidualized / gestational endometrium
- Embryonic / fetal tissue
- Immature chorionic villi
- Placental implantation site
Practice answer #1
B. Embryonic / fetal tissue. Despite frequent identification on ultrasound, embryo or fetus are often not recognized on product of conception specimens.
Comment Here
Reference: Early first trimester pregnancy loss
Comment Here
Reference: Early first trimester pregnancy loss
Practice question #2
Practice answer #2
A. Absence of circumeferential trophoblastic proliferation. Circumferential trophoblastic proliferation should raise suspicion for molar pregnancy, particularly complete mole.
Comment Here
Reference: Early first trimester pregnancy loss
Comment Here
Reference: Early first trimester pregnancy loss