Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Case reports | Treatment | Virtual slides | Cytology description | Cytology images | Positive stains | Videos | Sample pathology report | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Brčić L, Olteanu GE, Mataić A. Pleural effusion. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/pleurapleuraleffusion.html. Accessed September 16th, 2025.
Definition / general
- Pleural effusion is an excessive buildup of fluid between the layers of the pleura outside the lungs
Essential features
- The most common causes of pleural effusion are congestive heart failure, cancer, pneumonia and pulmonary embolism
- Pleural fluid is classified as a transudate or exudate based on modified Light criteria
- The International System for Serous Fluid Cytopathology standardized the way to report cytopathology diagnoses of serous fluids, which includes 5 different categories: nondiagnostic (ND), negative for malignancy (NFM), atypia of undetermined significance (AUS), suspicious for malignancy (SFM) and malignant (MAL)
- Treatment is based on the underlying condition and whether the effusion is causing severe respiratory symptoms
ICD coding
Epidemiology
- Estimated 1.5 million patients in the U.S. experience pleural effusion each year (JAMA Netw Open 2021;4:e2120306)
- Age of pleural effusion varies depending on the underlying cause
Sites
- Pleura
Pathophysiology
- Pleural effusion represents a disturbance of equilibrium between production and resorption of pleural fluid (Dtsch Arztebl Int 2019;116:377)
Etiology
- There are > 50 causes of pleural effusion; the most common are congestive heart failure, cancer, pneumonia and pulmonary embolism (Arch Bronconeumol 2014;50:161)
Diagrams / tables
Clinical features
- Patients can be asymptomatic or can present with cough, dyspnea and pleuritic chest pain (Am Fam Physician 2014;90:99)
- Depending on the cause, the fluid may be either transudative or exudative
- Pleural fluid is classified as a transudate or exudate based on modified Light criteria; pleural fluid is considered an exudative effusion if at least 1 of the criteria is met
- Pleural fluid protein/serum protein ratio of > 0.5
- Pleural fluid lactate dehydrogenase (LDH)/serum LDH ratio of > 0.6
- Pleural fluid LDH is > 66% of the upper limits of normal laboratory value for serum LDH
Diagnosis
- Detailed medical history should be obtained from all patients presenting with a pleural effusion, as this may help to establish the etiology
- Physical examination includes inspection, palpation, percussion and auscultation (Cleve Clin J Med 2008;75:297)
- Thoracentesis is a procedure for aspirating fluid from the pleural space by percutaneous insertion of a needle through the chest wall with or without the insertion of a catheter; it can be ultrasound guided (J Hosp Med 2018;13:126)
Laboratory
- For distinguishing transudates from exudates, serum and pleural fluid levels of protein and LDH are taken
- Pleural fluid drainage is recommended if the pH is < 7.20; the equivalent glucose level considered low is < 3.30 mmol/L (60 mg/dL) (J Thorac Dis 2023;15:2885)
- Amylase rich pleural effusion (ARPE) is defined as either a pleural amylase greater than the upper limit of serum amylase or a pleural fluid to serum amylase ratio of > 1 (J R Coll Physicians Edinb 2010;40:119)
- B type natriuretic peptide (BNP), N terminal proBNP (NTproBNP) and midregional proatrial NP (MRproANP), either in blood or pleural effusion, are effective tools for diagnosis of heart failure (PLoS One 2015;10:e0134376)
Radiology description
- Chest radiographs: a posteroanterior view reveals effusions of volume 200 mL or larger, a lateral view shows effusions of volume 50 mL or larger
- Radiographic signs
- Meniscus sign on a frontal radiograph (> 200 mL)
- Blunting of costophrenic sulcus on lateral view (> 50 mL)
- Subpulmonic effusion: lateral displacement of the apex of the pseudodiaphragm
- Ultrasound allows the detection of small amounts of pleural locular fluid, with positive identification of amounts as small as 3 - 5 mL
- According to the characteristics of the pleural effusion on ultrasound, it can appear as anechoic (black), complex nonseptated (black with white strands), complex septated (black with white septa) or homogeneously echogenic (white) (J Bras Pneumol 2014;40:1)
- On chest computed tomography (CT), free flowing fluid will collect initially in deep lateral and posterior pleural recesses (Respir Med 2017;124:88)
Case reports
- 7 year old Turkish girl presented to a local hospital with fever, chest pain and vomiting (J Med Case Rep 2019;13:344)
- 30 year old man presented with complaints of low grade, intermittent fever for 2 years, right sided chest pain for 2 months and weight loss (Trop Doct 2021;51:111)
- 33 year old man with a history of sudden onset, pleuritic, right sided chest pain of 2 days duration (Breathe (Sheff) 2017;13:e46)
Treatment
- Treatment is based on the underlying condition and whether the effusion is causing severe respiratory symptoms
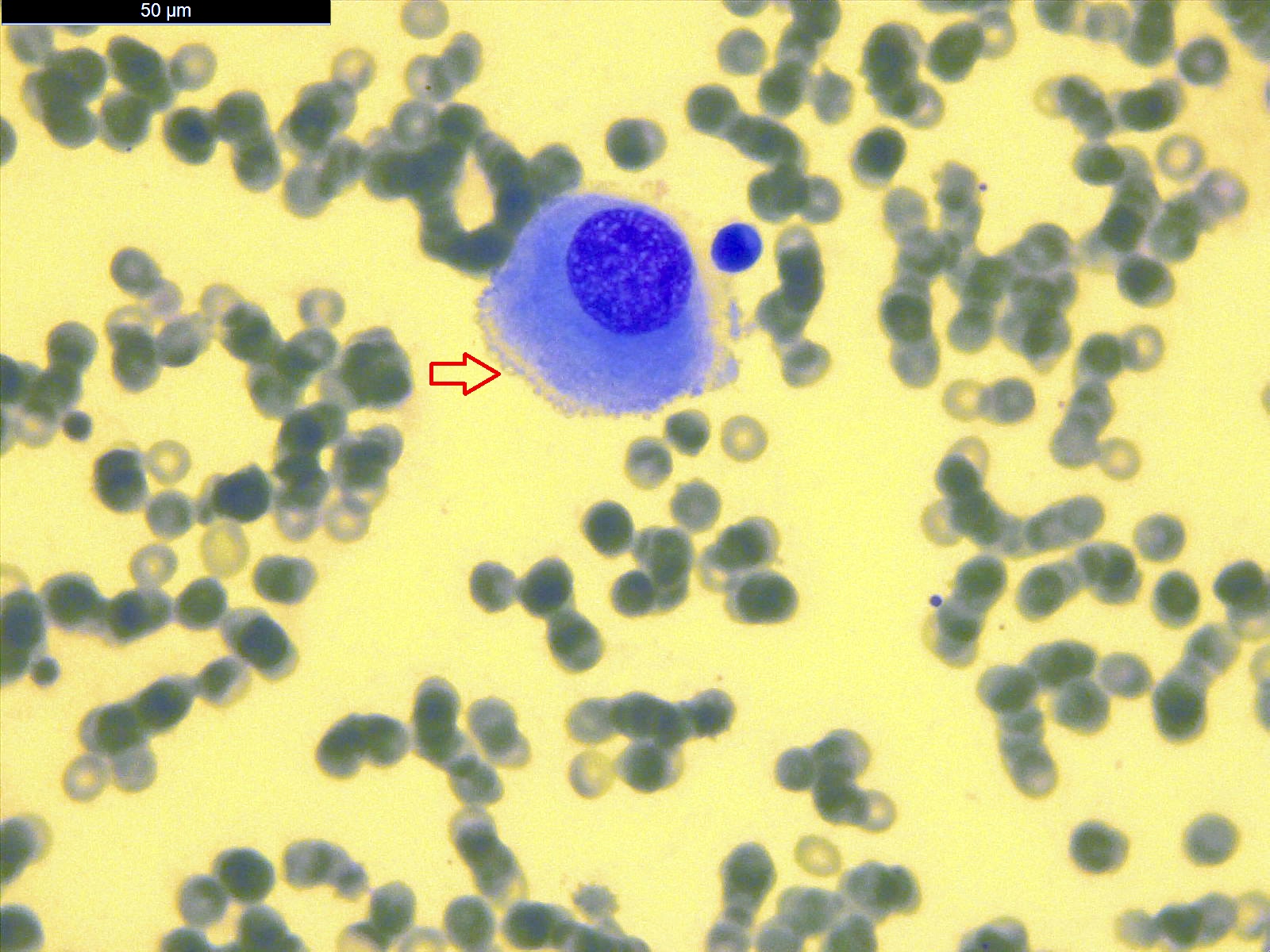
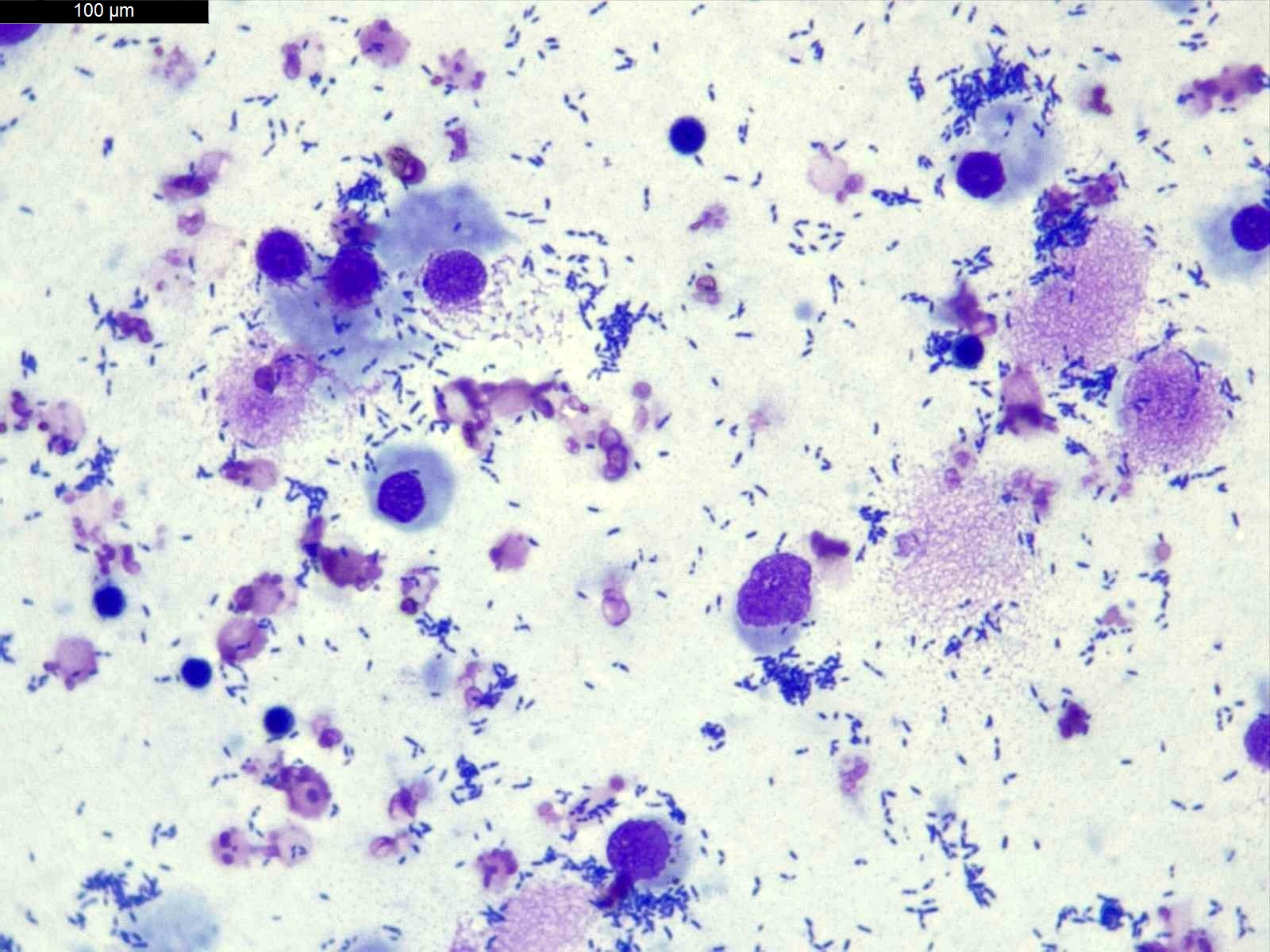
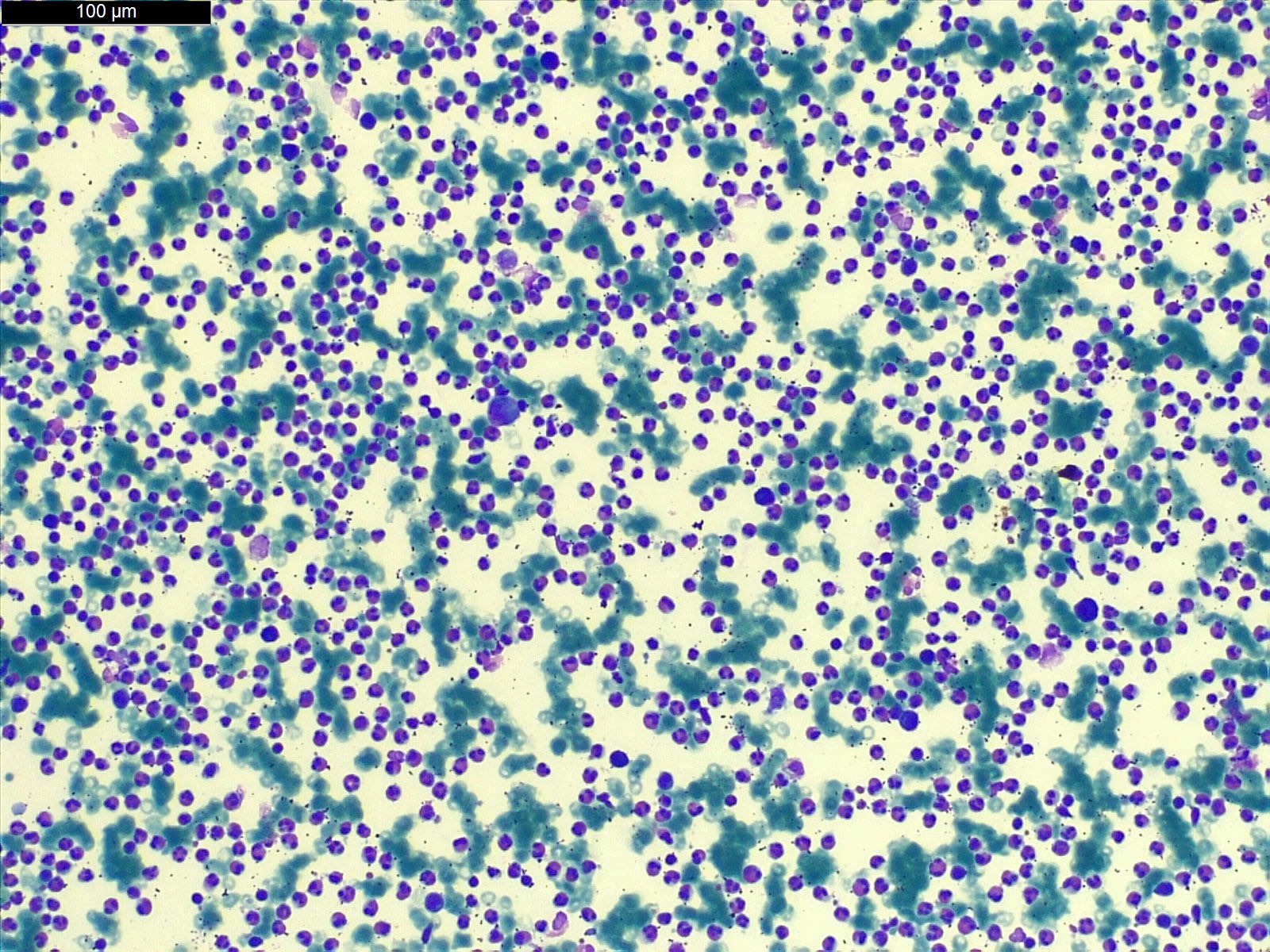
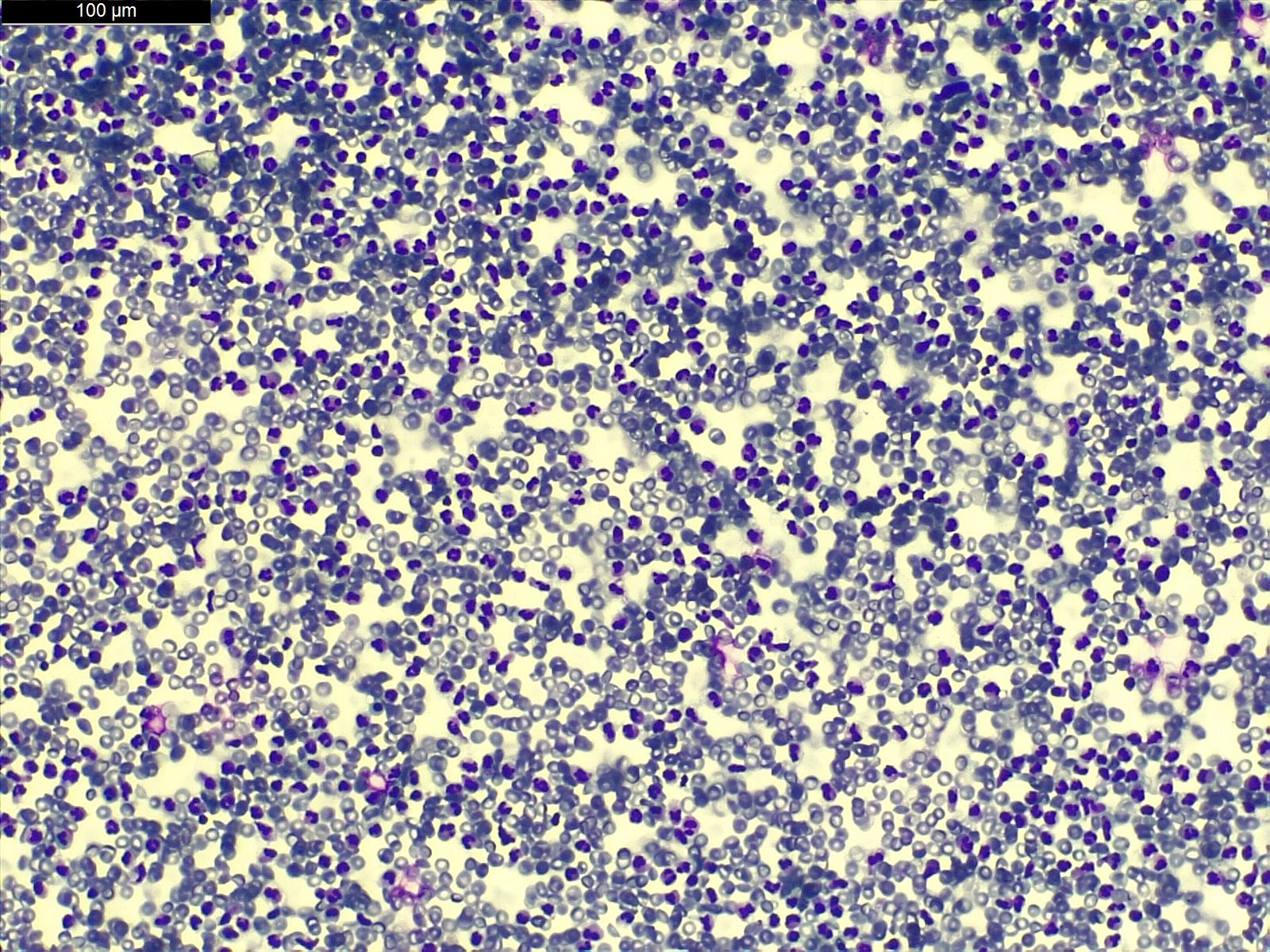
Cytology description
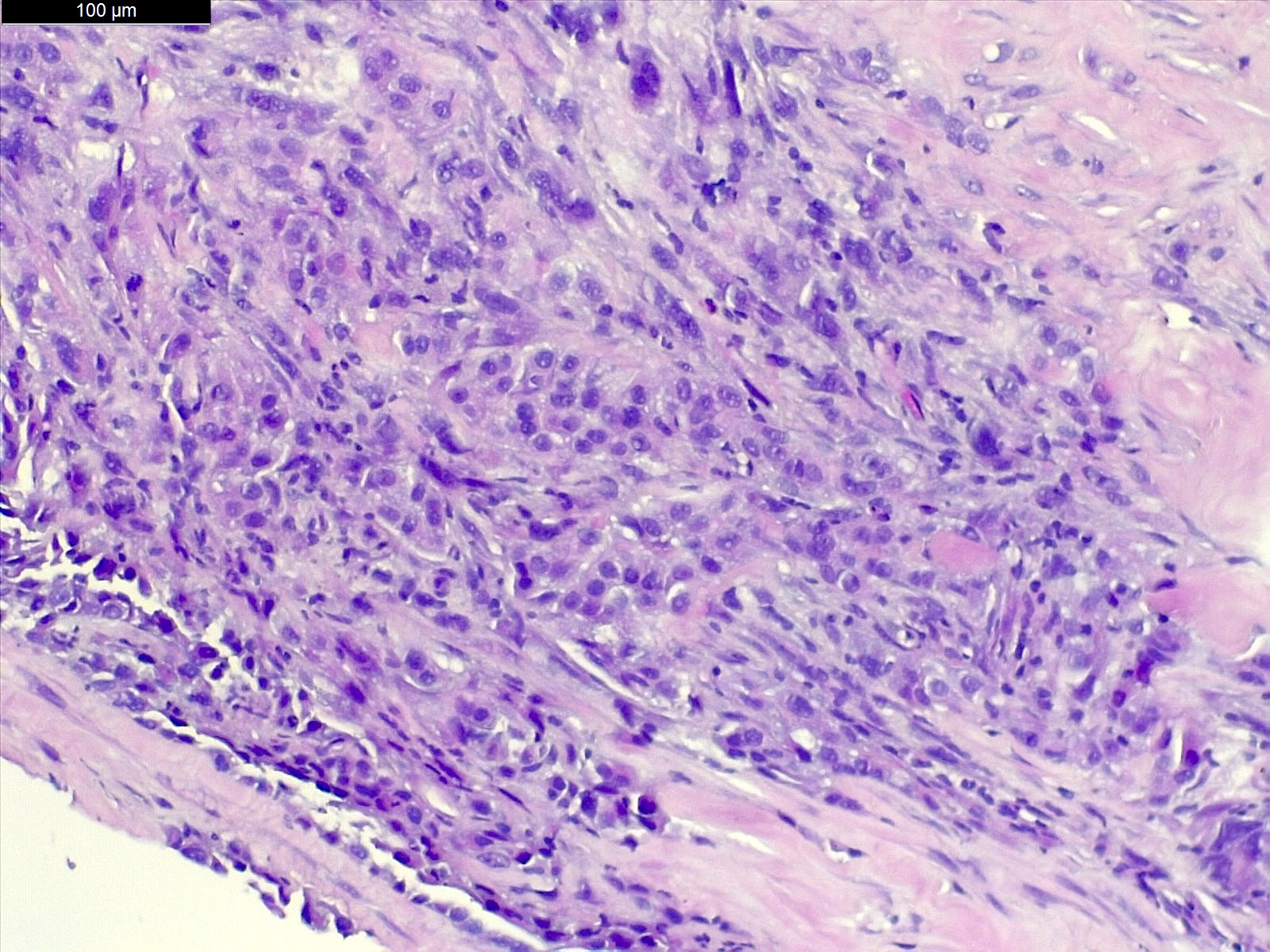
- For cytology, different cytological preparation methods can be used, including conventional direct smear, cytospin, liquid based preparations and cell blocks, each with its own strengths and limitations (Am J Cancer Res 2021;11:43)
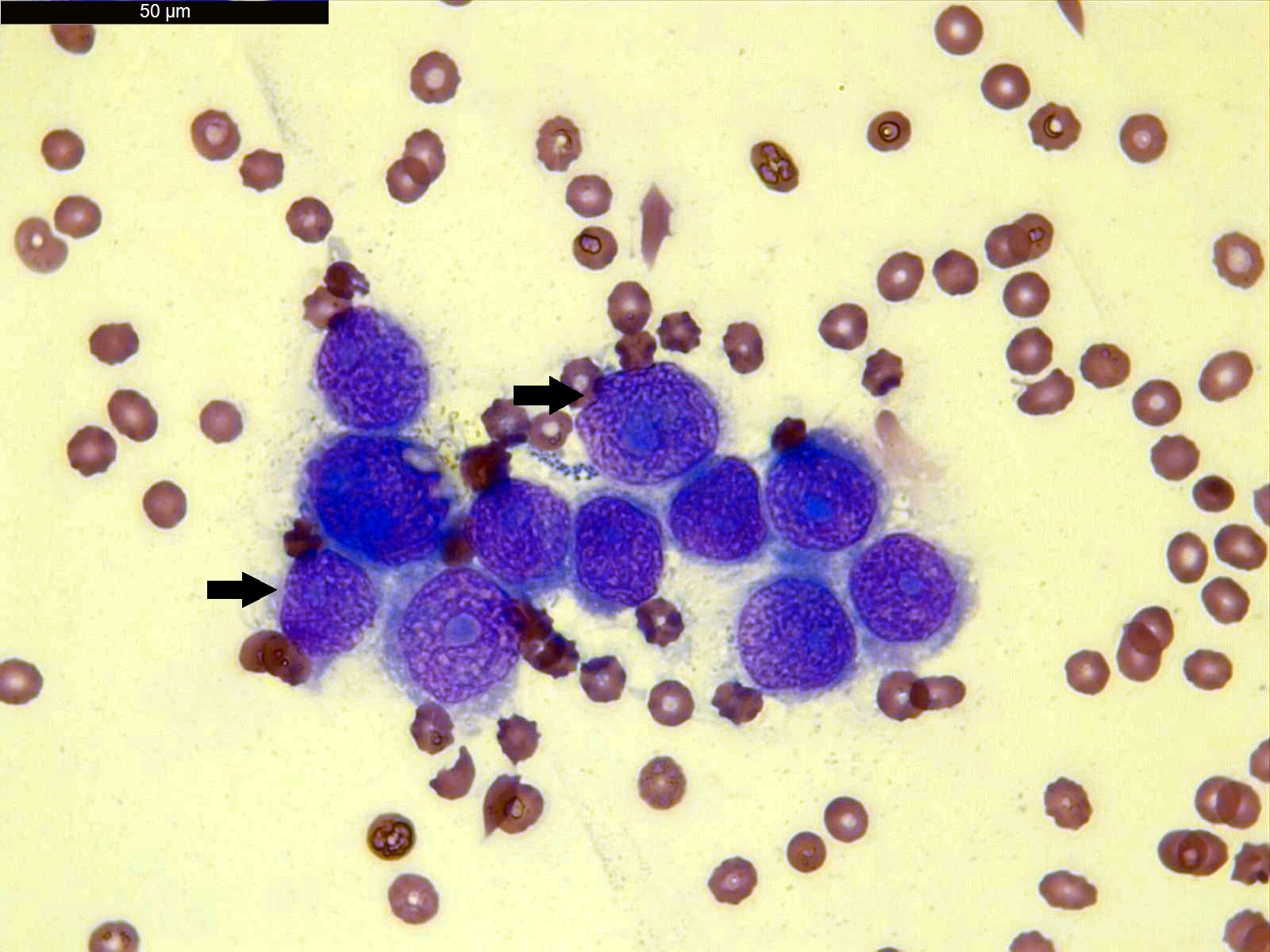
- Differential count of pleural fluid white blood cells (WBCs) aids differentiation of the causal diseases
- It is determined by counting 100 cells under a light microscope (400x)
- Lymphocytes, neutrophils, histiocytes, eosinophils, mesothelial cells, malignant cells and atypical cells are differentiated (World J Surg Oncol 2021;19:180)
- The international system for reporting serous fluid cytopathology standardized the way to report cytopathology diagnoses of serous fluids, which includes 5 different categories: nondiagnostic (ND), negative for malignancy (NFM), atypia of undetermined significance (AUS), suspicious for malignancy (SFM) and malignant (MAL) (see International system for reporting serous fluid cytopathology)
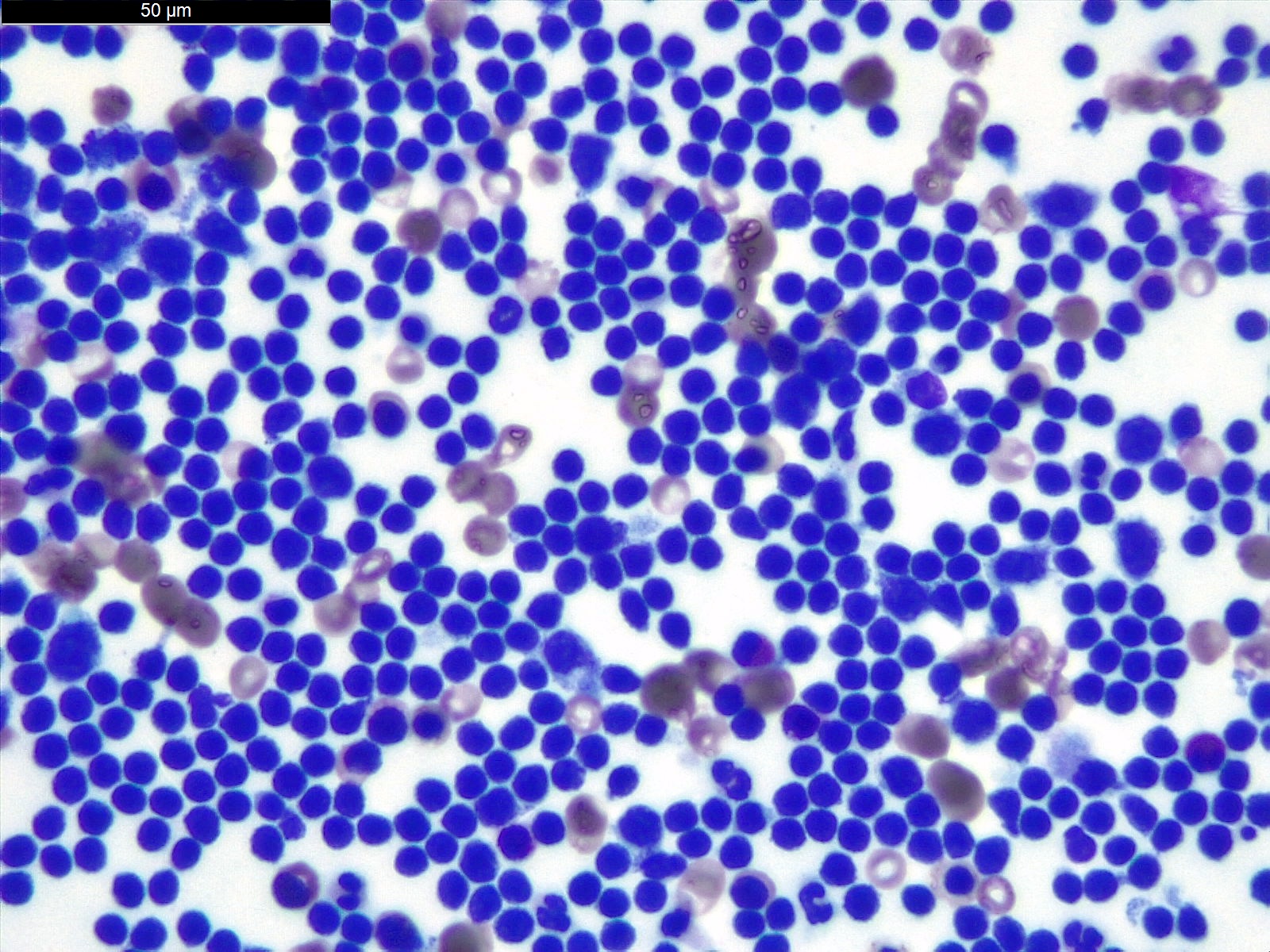
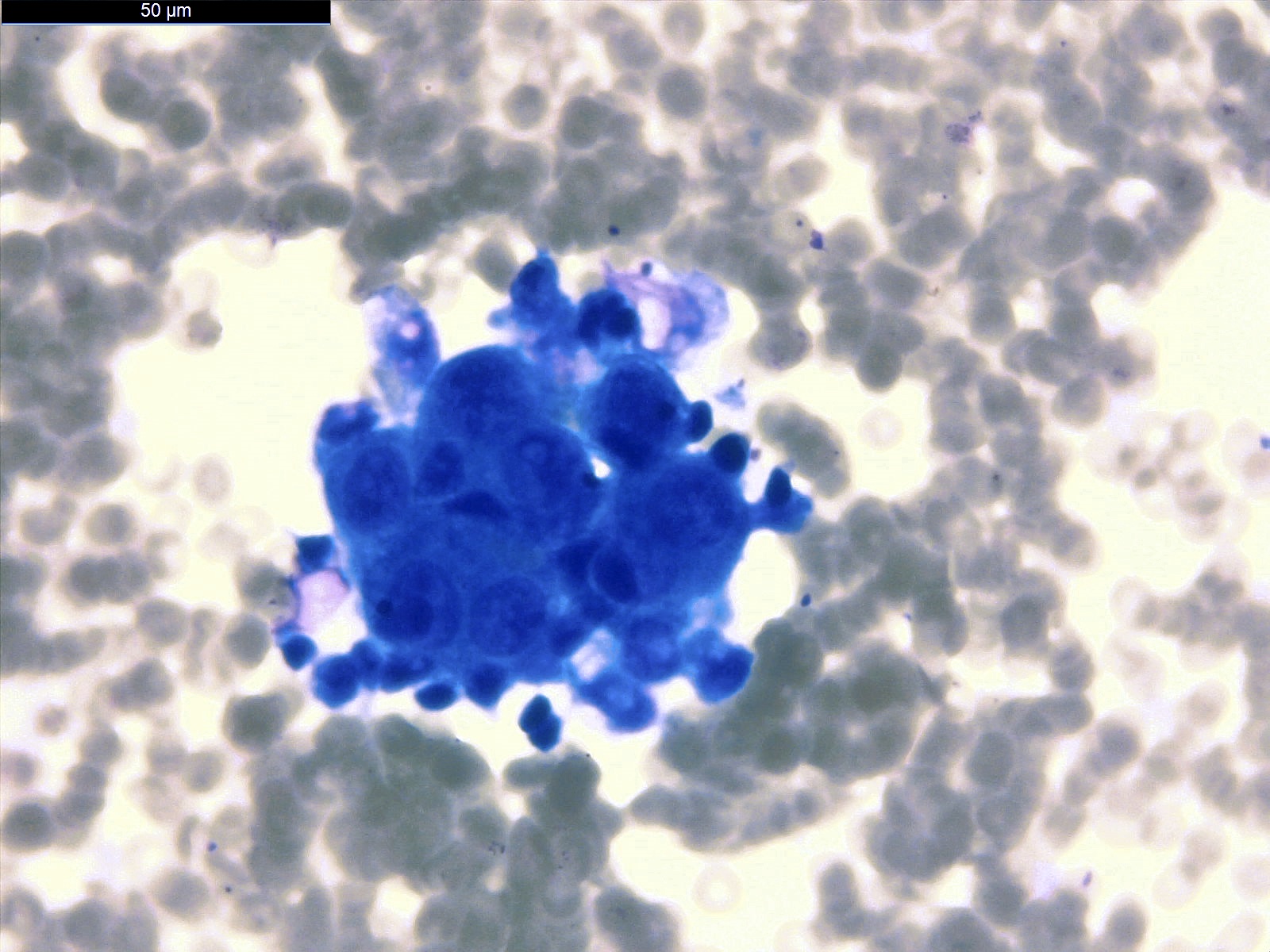
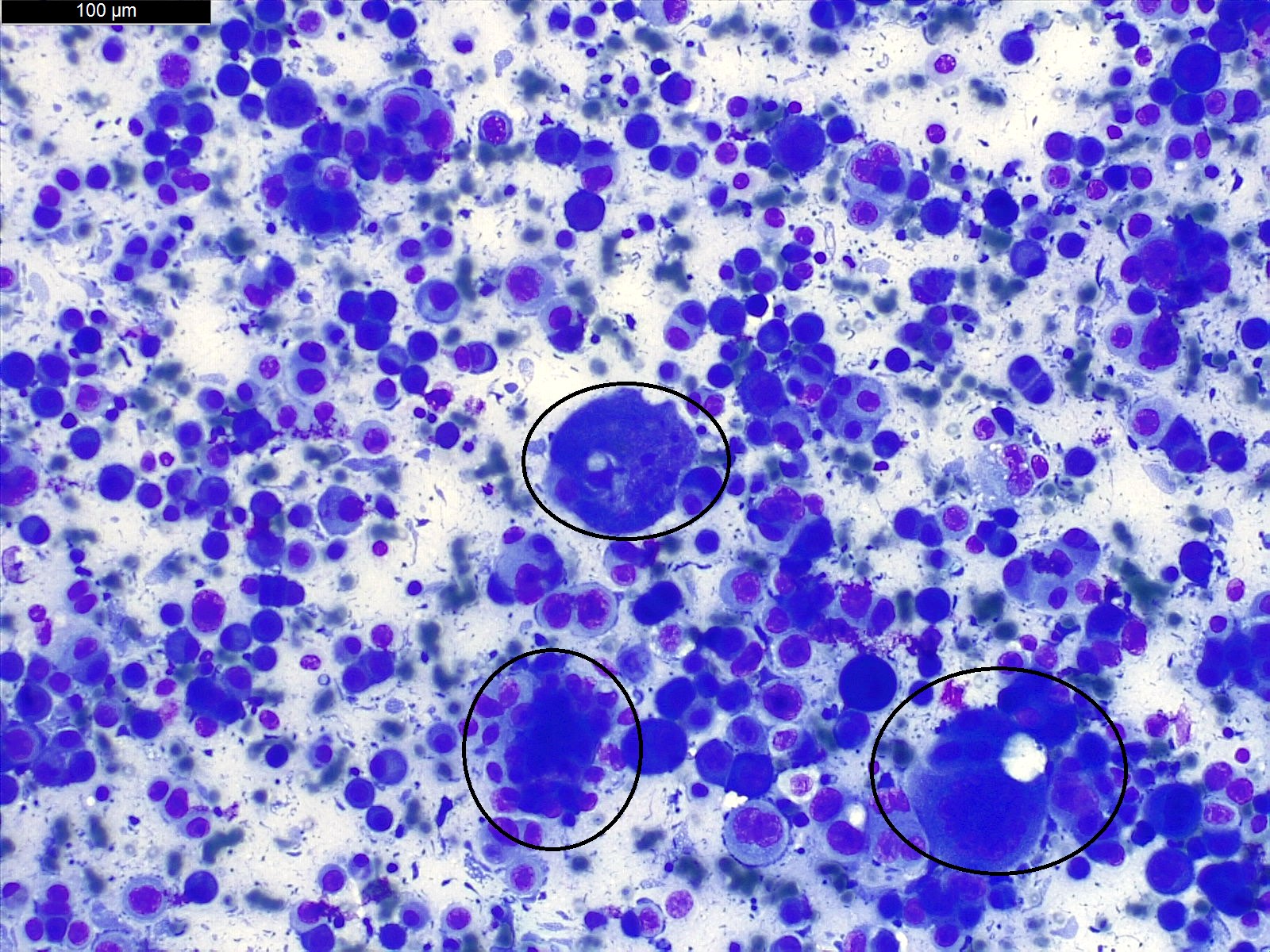
Cytology images
Contributed by Gheorghe-Emilian Olteanu, M.D., Ph.D.
Positive stains
- Selection of an appropriate panel of immunostains is dependent upon the clinical profile of the patient, the site of effusion, imaging findings and serum tumor markers (Cytopathology 2022;33:678, Surg Pathol Clin 2018;11:523)
Videos
Pleural effusion causes, signs and symptoms, diagnosis and treatment
Pleural effusion: explanation of Xray findings
The international system of serous effusion cytopathology
Sample pathology report
- International system for reporting serous fluid cytopathology was an effort to standardize terminology with standardized cytomorphologic criteria for reporting pleural, peritoneal and pericardial effusion (see International system for reporting serous fluid cytopathology)
- Negative for malignancy
- Pleural effusion:
- Adequacy: Satisfactory for evaluation
- Diagnosis: Negative for malignancy (see comment)
- Comment: Hypercellular effusion consisting of lymphoid cells (lymphocytic effusion); compatible with patient's clinical diagnosis of tuberculosis.
- Pleural effusion:
- Malignant
- Pleural effusion:
- Adequacy: Satisfactory for evaluation
- Diagnosis: Malignant effusion, consistent with metastatic adenocarcinoma of primary breast origin (see comment)
- Comment: The cytospin preparations are hypercellular, with large, 3 dimensional groups of malignant cells with cannonball appearance. The cells have enlarged, pleomorphic nuclei, coarse chromatin and prominent nucleoli. Given the cytomorphological features and the patient’s known history of breast carcinoma, the diagnosis is consistent with malignant effusion from a metastatic breast adenocarcinoma.
- Pleural effusion:
Practice question #1
The distinction between a transudate and an exudate is based on Light criteria and is determinative for the evaluation and treatment of a pleural effusion. What parameter(s) among the listed is / are the Light criteria for drawing this distinction?
- Amylase in the effusion fluid
- NTproBNP in the effusion fluid
- pH level in the effusion fluid
- Protein and LDH in the effusion fluid and in the serum
Practice answer #1
D. Protein and LDH in the effusion fluid and in the serum. The difference between transudate and exudate are based on modified Light criteria, which includes pleural fluid protein/serum protein ratio of > 0.5, pleural fluid lactate dehydrogenase (LDH)/serum LDH ratio of > 0.6 and pleural fluid LDH > 66% of the upper limits of normal laboratory value for serum LDH. Answers A, B and C are incorrect because analyzing amylase, NTproBNP and pH level in effusion fluid can help in detecting the cause of pleural effusion but these do not help in differentiating between transudate and exudate.
Comment Here
Reference: Pleural effusion
Comment Here
Reference: Pleural effusion
Practice question #2
Regarding pleural effusion, which of the following is true?
- Pleural fluid is classified as a transudate or exudate based on Bethesda criteria
- The international system for reporting serous fluid cytopathology standardized the way to report cytopathology diagnosis of serous fluids, which includes 5 different categories
- Treatment is the same, regardless of the underlying condition and whether the effusion is causing respiratory symptoms
- Uncommon causes of pleural effusion are congestive heart failure and cancer
Practice answer #2
B. The international system for reporting serous fluid cytopathology standardized the way to report cytopathology diagnosis of serous fluids, which includes 5 different categories: nondiagnostic (ND), negative for malignancy (NFM), atypia of undetermined significance (AUS), suspicious for malignancy (SFM) and malignant (MAL). Answer D is incorrect because the most common causes of pleural effusion are congestive heart failure, cancer, pneumonia and pulmonary embolism. Answer A is incorrect because pleural fluid is classified as a transudate or exudate based on modified Light criteria. Answer C is incorrect because treatment is based on the underlying condition and whether the effusion is causing severe respiratory symptoms.
Comment Here
Reference: Pleural effusion
Comment Here
Reference: Pleural effusion