Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Immunofluorescence description | Immunofluorescence images | Negative stains | Electron microscopy description | Electron microscopy images | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1Cite this page: Kazlouskaya V. Pemphigus vulgaris. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorpemphigusvulgaris.html. Accessed September 16th, 2025.
Definition / general
- Pemphigus vulgaris (PV) is an autoimmune disorder that affects the skin and mucous membranes
- PV is characterized by the presence of IgG antibodies targeting desmoglein 1 or desmoglein 3, leading to the formation of superficial, flaccid bullae and erosions
Essential features
- Pemphigus vulgaris (PV) is an autoimmune skin condition that primarily affects the skin and mucous membranes
- Characterized by the presence of flaccid bullae (blisters) and erosions
- On a histopathology, PV is marked by intraepidermal acantholysis
- Requires aggressive treatment, often involving immunosuppressive therapies to control the immune response and prevent further skin damage
ICD coding
Epidemiology
- Incidence is 2.8 per million person years with a higher incidence in patients from Southern Asia (4.94 per million person years) (Dermatology 2023;239:514)
- Average onset is 40 - 60 years old
- Occurs equally in men and women (Dermatology 2023;239:514)
- May affect neonates via transplacental autoantibody transmission (JAMA Dermatol 2021;157:220)
Sites
- Skin, mucosae, nails (paronychia)
Pathophysiology
- IgG to desmoglein 1 (Dsg1) (skin) or desmoglein 3 (Dsg3) (skin, mucosa)
- Other important biomarkers include elevations in IL4, IL6 and IL17A and a reduction in Treg cells and FOXP3 (J Cutan Med Surg 2024;28:458)
Etiology
- Association with human leukocyte antigen class II: HLADR4 and HLADR14, HLADRB1 0402, 1401, 0503, 0302 (Front Med (Lausanne) 2018;5:226)
- Drug induced pemphigus: thiol drugs (e.g., penicillamine, captopril), nonthiol drugs (e.g., penicillin, cephalosporin, enalapril, rifampin, NSAID) (Front Med (Lausanne) 2023;10:1326359)
Clinical features
- Skin: superficial bullae and erosions with a predilection for upper chest, back, scalp, face
- Small flaccid vesicles may be seen, especially at the beginning of the disease
- Erosions on the mucosae (oral, ocular or genital)
- Hoarseness if larynx or pharynx are involved
- Nail involvement (paronychia, Beau lines, onychomadesis) (Int J Dermatol 2024;63:1308)
- Isolated crusted lesions on the scalp can be seen, especially in elderly patients (Dermatol Online J 2024;30)
- Signs
- Nikolsky sign: induction of new blister by slight friction
- Asboe-Hansen sign: lateral extension of the intact blister with gentle pressure
Diagnosis
- Diagnosis is made on clinical, histopathologic, immunopathologic and serologic findings (J Eur Acad Dermatol Venereol 2020;34:1900)
- Histopathology and immunopathology
- Skin biopsy for H&E from the edge of the blister
- Direct immunofluorescence (most sensitive); biopsy should be taken from the uninvolved perilesional skin
- Serology
- Enzyme linked immunosorbent assay (ELISA) for IgG or IgA antibodies to Dsg1 and Dsg3
- Indirect immunofluorescence
- Immunoblotting and immunoprecipitation (less used)
- Endoscopy may help identify extraoral mucosal lesions
Laboratory
- Indirect immunofluorescence: intercellular deposition of IgG; monkey esophagus is used as a substrate
- ELISA: IgG against Dsg3 or Dsg1 and Dsg3; ELISA values correlate with the severity of the disease
Prognostic factors
- Mortality is 5 - 15% (Front Immunol 2022;13:895490)
- Historically > 90% 5 year mortality; however, this has been improved with oral steroids and steroid sparing treatments (Int J Dermatol 2005;44:470)
- Poor prognosis factors (J Eur Acad Dermatol Venereol 2010;24:947)
- Younger age at presentation
- Mucosal involvement at presentation
- Relapses
Case reports
- Newborn boy presented with extensive vesicobullous lesions on the anterior side of his chest and abdomen born from mother with known PV (Rev Paul Pediatr 2019;37:130)
- 20 year old man presented with PV affecting nails (Cureus 2024;16:e53609)
- 42 year old man presented with PV and an anal fissure (Int J Surg Case Rep 2024;114:109185)
- 60 year old man and 69 year old woman presented with worsening PV after COVID-19 infection (An Bras Dermatol 2024;99:758)
Treatment
- Rituximab is the first line treatment even for mild cases (Cureus 2024;16:e53609)
- Topical or oral steroids may be tried for very limited PV (Cureus 2024;16:e53609)
- Systemic immunosuppressive medications (azathioprine, mycophenolate mofetil, methotrexate, cyclosporine and dapsone) are used as steroid sparing agents
- Local skin care
- Prevention of secondary infection (especially herpes simplex virus)
- Intravenous immune globulin, immunoadsorption, plasmapheresis, extracorporeal photopheresis or cyclophosphamide for refractory cases
Clinical images
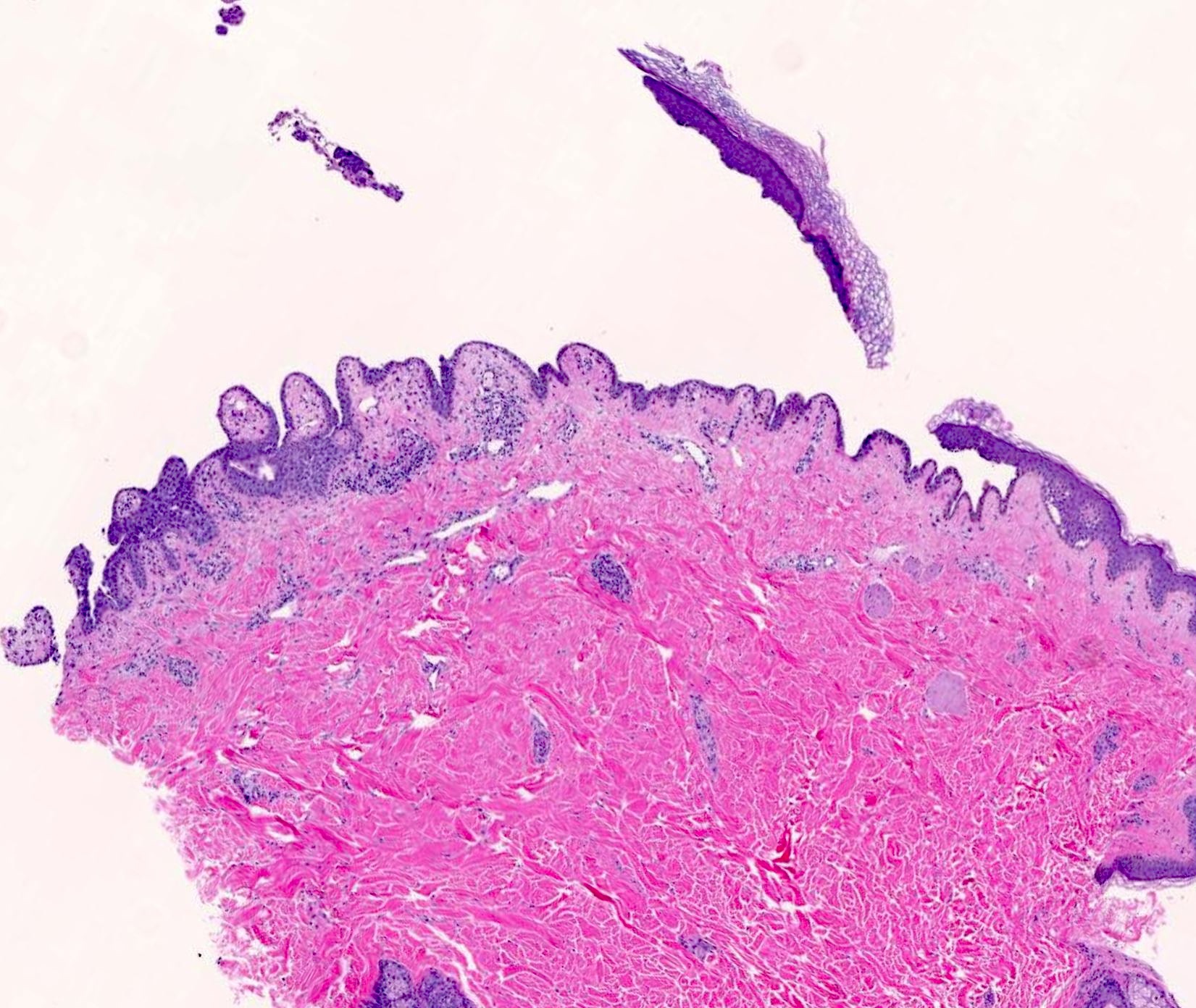
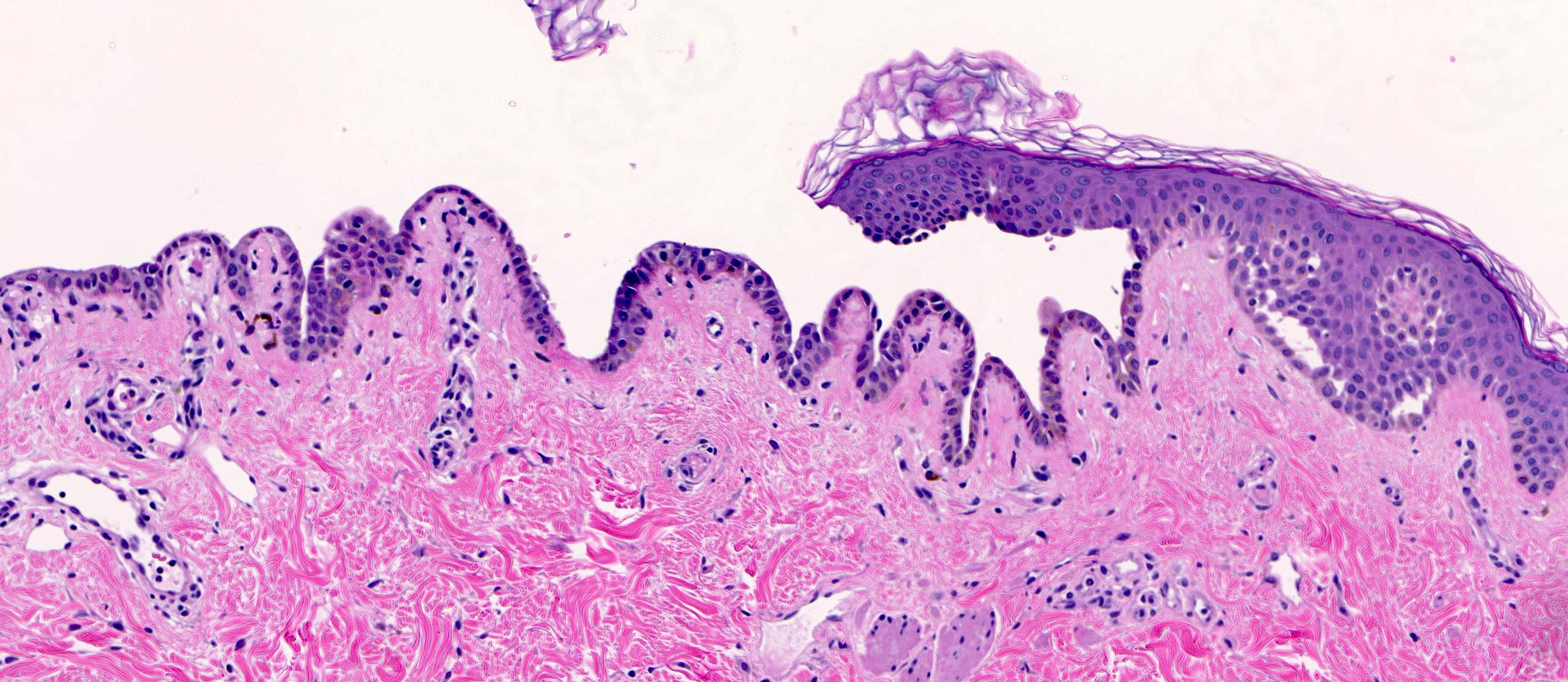
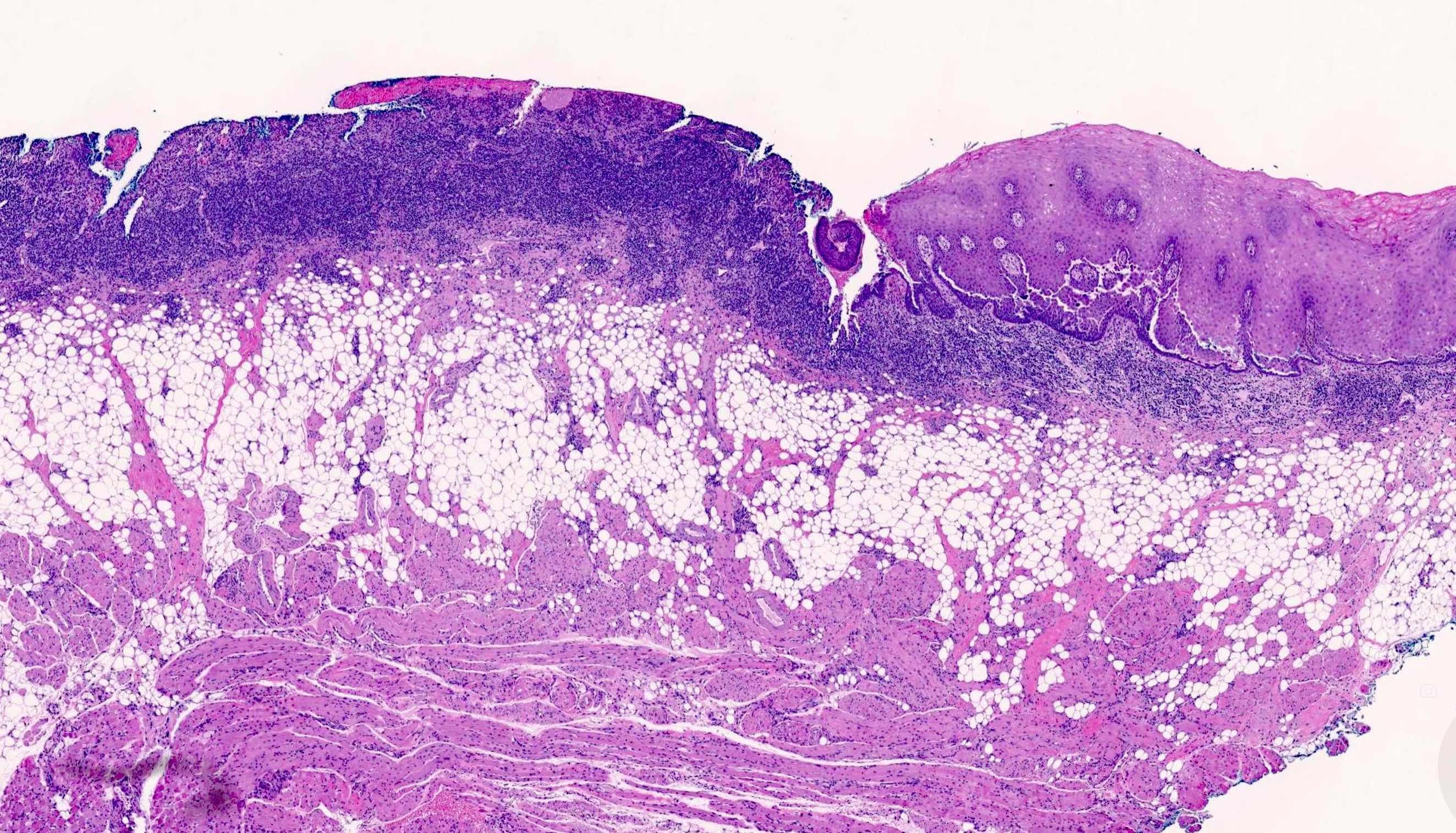
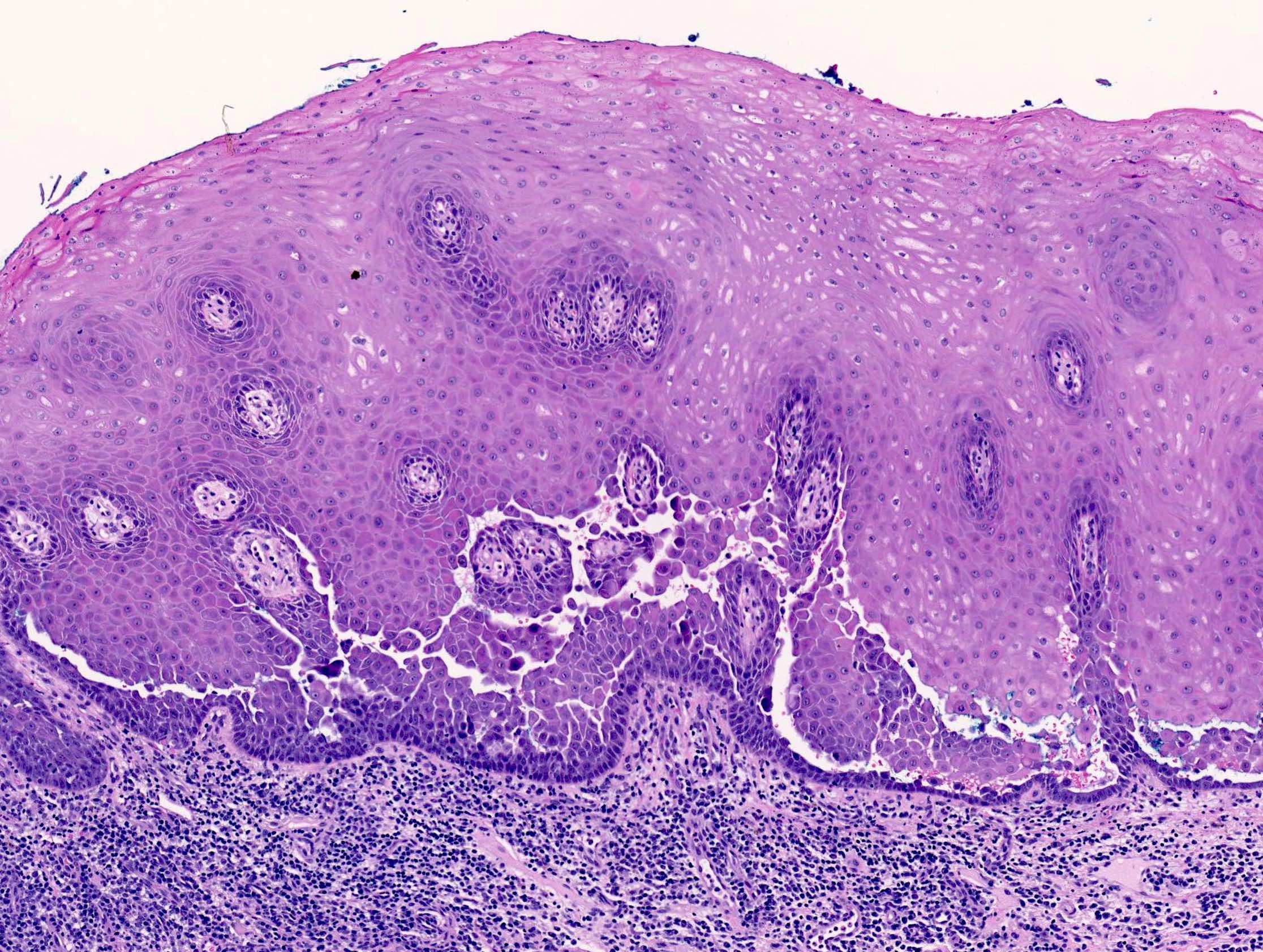
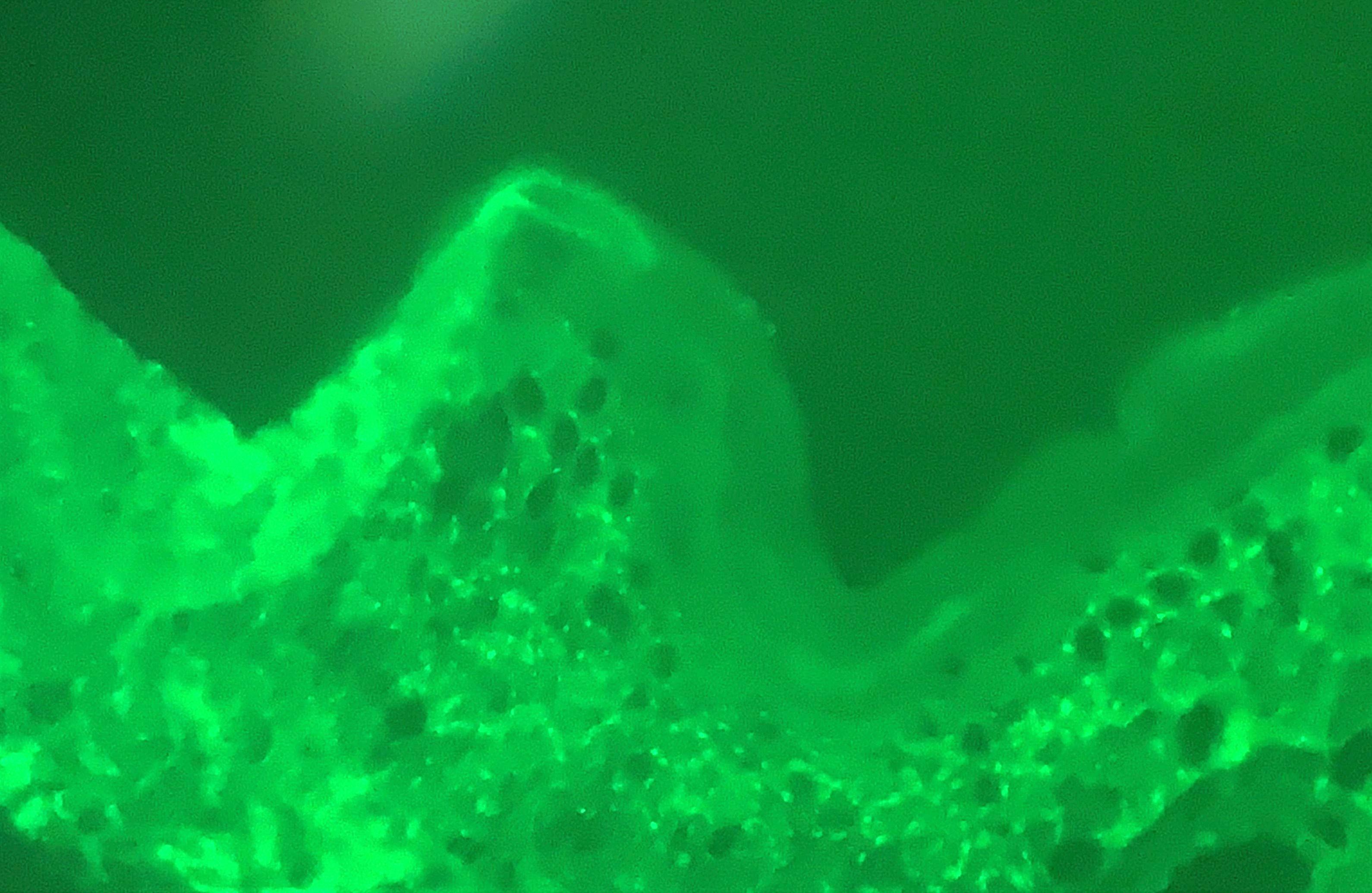
Microscopic (histologic) description
- Suprabasilar acantholysis
- Basal layer remains attached (tombstone sign)
- Intraepidermal vesicles with round acantholytic keratinocytes
- Intraepidermal eosinophils and sometimes neutrophils
- Follicular involvement
- No significant dyskeratosis
- Miniaturization of the sebaceous glands in the scalp lesions (also seen in pemphigus foliaceus) (J Cutan Pathol 2017;44:835)
Microscopic (histologic) images
Cytology description
- Rarely used but may be helpful as a quick tool or if other diagnostic resources are limited
- Tzanck smears from the erosions or blister bottom may be performed (Diagn Cytopathol 2007;35:403)
- Acantholytic cells are larger round cells with large nuclei surrounded by clear halo and inconspicuous nucleoli
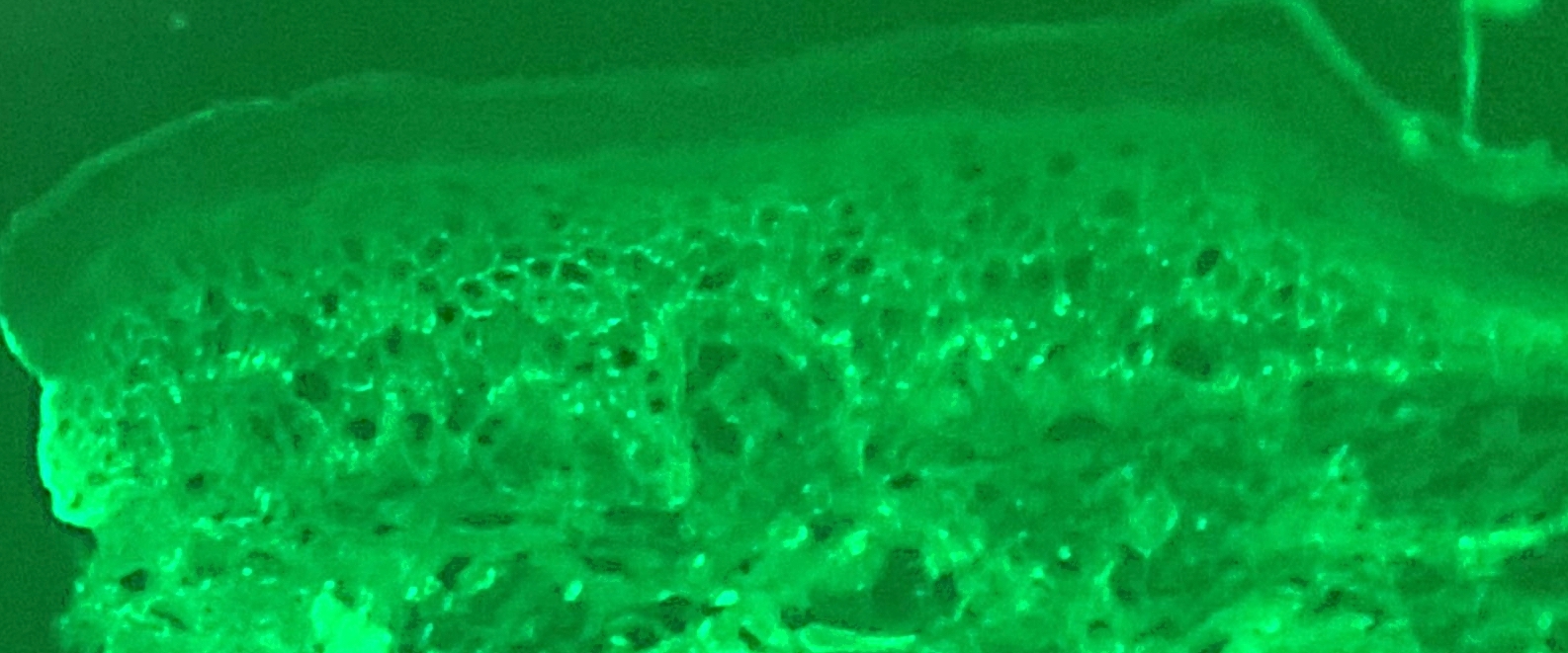
Immunofluorescence description
- Intercellular IgG and C3 in the epidermis (chicken wire pattern) (J Am Acad Dermatol 1986;14:52)
Immunofluorescence images
Electron microscopy description
- Dilatation of intercellular space, stretched desmosomes, acantholytic cells
Electron microscopy images
Sample pathology report
- Skin, punch biopsy, chest:
- Intraepidermal acantholysis, consistent with pemphigus vulgaris (see comment)
- Comment: Examination of the specimen shows intraepidermal acanthosis with eosinophil and neutrophil exocytosis. There is a perivascular infiltrate with eosinophils in the dermis. Neither fungal microorganisms nor basement membrane changes are seen with interpretation of PAS histochemical stain.
- Skin, punch biopsy, chest perilesional for direct immunofluorescence:
- Consistent with pemphigus vulgaris (see comment)
- Comment: 5 immunofluorescence stains were ordered and scored subjectively on a scale from 0 - 3+
- IgG: 2+, intercellular epidermal
- IgM: 0, negative
- IgA: 0, negative
- C3: 2+, intercellular epidermal
- Fibrin: 0, negative
- IgG and C3 immunofluorescence is seen throughout the epidermis with the intercellular pattern suggestive of pemphigus vulgaris but correlation with clinical findings is necessary
Differential diagnosis
- Grover disease (transient acantholytic dyskeratosis):
- Distribution on trunk with sparing of mucosae, face, scalp
- Suprabasilar acantholysis with dyskeratosis
- Negative immunofluorescence
- Darier disease (keratosis follicularis):
- Rare genetic disorder
- Seborrheic distribution
- Suprabasilar acantholysis with dyskeratosis
- Negative immunofluorescence
- Hailey-Hailey disease (benign familial chronic pemphigus):
- Rare genetic disorder with mutation in ATP2C1 gene
- Distribution with preference for intertriginous zones, neck, chest
- Follicular involvement is rare
- Acanthosis with acantholytic cells throughout the full thickness of the epidermis (brick wall look)
- Negative immunofluorescence
- Other pemphigus subtypes:
- Direct immunofluorescence / antibodies vary
- Warty dyskeratoma:
- Benign, solitary lesion
- Verrucous epidermal hyperplasia, exoendophytic silhouette, suprabasilar acantholysis with dyskeratosis
- Negative immunofluorescence
Practice question #1
A 65 year old patient presents with mucosal erosions and the skin findings shown. What are the expected histopathological features of this condition?
- Acantholytic dyskeratotic cells and parakeratotic columns with negative direct immunofluorescence
- Dilapidated brick wall appearance with negative direct immunofluorescence
- Focal acantholysis with various patterns and negative direct immunofluorescence
- Intraepidermal acantholysis with chicken wire pattern IgG on direct immunofluorescence
Practice answer #1
D. Intraepidermal acantholysis with chicken wire pattern IgG on direct immunofluorescence. The image depicts widespread erosions and crusted lesions on the scalp and upper body, consistent with the clinical presentation of pemphigus vulgaris (PV). PV is an autoimmune disease characterized by acantholysis and IgG or C3 deposits on direct immunofluorescence (DIF). Answers B and C are incorrect because a negative DIF typically rules out PV. Answer A is incorrect because the presence of dyskeratotic cells is not typical of PV. Additionally, the negative DIF excludes PV as this condition usually shows specific immunoreactant deposits.
Comment Here
Reference: Pemphigus vulgaris
Comment Here
Reference: Pemphigus vulgaris