Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1Cite this page: Kaur G, Vyas M. Lymphangiectasia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/smallbowellymphangiectasia.html. Accessed April 25th, 2024.
Definition / general
- Dilated small intestinal lacteals, which may be primary or secondary
- Primary intestinal lymphangiectasia is a rare disorder resulting in lymph leakage into the small bowel lumen and responsible for protein losing enteropathy, leading to lymphopenia, hypoalbuminemia and hypogammaglobulinemia (Orphanet J Rare Dis 2008;3:5)
Essential features
- Lymphagiectasia can be primary or secondary; primary intestinal lymphangiectasia is more common in children, though in rare cases it can present in early adulthood and is usually associated with malabsorption
- Secondary lymphangiectasia is often seen in adults and can be associated with various obstruction / constrictive conditions (described below), though exclusion of an underlying malignancy remains the main consideration
- Microscopy shows dilated lymphatic vessels in the mucosa and submucosa without significant villous atrophy or inflammation
Terminology
- Waldmann disease
ICD coding
- ICD-10: K63.89 - Other specified diseases of intestine
Epidemiology
- Primarily affects children (generally diagnosed before 3 years of age) and young adults but may be diagnosed later in adults (Orphanet J Rare Dis 2008;3:5)
- Very rare familial forms of Waldmann disease have been reported
Sites
- Small intestine
Pathophysiology
- To date, the etiology of primary intestinal lymphangiectasia is unknown
- Several genes, such as VEGFR3 (vascular endothelial growth factor receptor 3), prospero related homeobox transcriptional factor PROX1, forkhead transcriptional factor FOXC2 and SOX18 are implicated in the development of the lymphatic system (Orphanet J Rare Dis 2008;3:5)
- Mutations in the FOXC2 (MFH1) gene or deletion of the PIK3R1 gene may result in lymphangiectasia, arrested lymphatic sprouting and maturation defects (World J Gastrointest Endosc 2011;3:235)
Etiology
- Etiology is unknown for primary intestinal lymphangiectasia
- Syndromes associated with primary intestinal lymphangiectasia include von Recklinghausen, Turner or Noonan, Klippel-Trenaunay and Hennekam (Turk J Gastroenterol 2018;29:714)
- Some secondary causes of intestinal lymphangiectasia include constrictive pericarditis, intestinal lymphoma, lymphenteric fistula, Whipple disease, Crohn's disease, sarcoidosis, intestinal tuberculosis, systemic sclerosis, radiation or chemotherapy with retroperitoneal fibrosis and human immunodeficiency virus related enteropathy (Orphanet J Rare Dis 2008;3:5)
Clinical features
- Classical symptoms are bilateral or unilateral lower limb edema and intermittent diarrhea (Am J Case Rep 2016;17:512)
- Some patients develop steatorrhea
- Accumulation of fluids in body cavities resulting in pleural effusion or ascites has been reported
- Lymphedema (Orphanet J Rare Dis 2008;3:5)
- In children, primary intestinal lymphangiectasia is generally diagnosed before 3 years of age and may be complicated by fatigue, abdominal pain, nausea, vomiting and weight loss, inability to gain weight and growth retardation; malabsorption may cause fat soluble vitamin deficiencies and hypocalcemia leading to convulsions (Orphanet J Rare Dis 2008;3:5)
- In secondary cases, the symptoms may be related to the underlying condition
Diagnosis
- Endoscopy or capsule endoscopy can show swollen mucosa and enlarged whitish villi (World J Gastrointest Endosc 2011;3:235)
- Biopsy
Laboratory
- Hypoproteinemia, hypoalbunimia and hypogammaglobunimea due to protein loss (Orphanet J Rare Dis 2008;3:5)
- Exudative enteropathy is confirmed by high 24-h stool alpha-1 antitrypsin clearance due to enteric protein loss
- Functional absorption tests such as D-xylose test results are normal in primary intestinal lymphangiectasia
Radiology description
- Ultrasonographic findings may show dilation of the intestinal loops, regular and diffuse thickening of the walls, plical hypertrophy and severe mesenteric edema and, in some cases, ascites (Orphanet J Rare Dis 2008;3:5)
- CT scan can show diffuse, nodular small bowel wall thickening and edema, which are a consequence of the dilated lymphatics within the villi along with some degree of small bowel dilation with (in few cases) a halo sign due to swelling and edema (Orphanet J Rare Dis 2008;3:5)
Prognostic factors
- Primary intestinal lymphangiectasia is a chronic debilitating disorder requiring constraining long term dietary control based on a low fat regimen associated with supplementary medium chain triglycerides (Orphanet J Rare Dis 2008;3:5)
- Primary intestinal lymphangiectasia may be life threatening when malignant complications (lymphoma) or serous effusion(s) (pleural, pericardic) occur (Orphanet J Rare Dis 2008;3:5)
Case reports
- 10 year old boy with pediatric localized intestinal lymphangiectasia treated with resection (Int Med Case Rep J 2019;12:23)
- 30 year old woman with primary intestinal lymphangiectasia causing intussusception and small bowel obstruction (ACG Case Rep J 2019;6:e00233)
- 47 year old patient with marginal zone lymphoma complicated by protein losing enteropathy (Case Rep Hematol 2016;2016:9351408)
- 60 year old woman with Waldmann disease (Rev Esp Enferm Dig 2017;109:385)
Treatment
- Low fat diet associated with supplementary medium chain triglycerides is the cornerstone of primary intestinal lymphangiectasia medical management (Orphanet J Rare Dis 2008;3:5)
- Small bowel resection is useful in the rare cases in which intestinal lymphangiectasia is segmental and localized (duodenum)
- Steroids were prescribed to patients with intestinal lymphangiectasia secondary to inflammatory disease with variable efficacy and also to systemic lupus erythematosus patients with protein losing enteropathy
- Treatment of the underlying disease in secondary causes
Gross description
- White granular surface (Turk J Gastroenterol 2018;29:714)
- Mucosa can be swollen
- May form a polypoid lesion
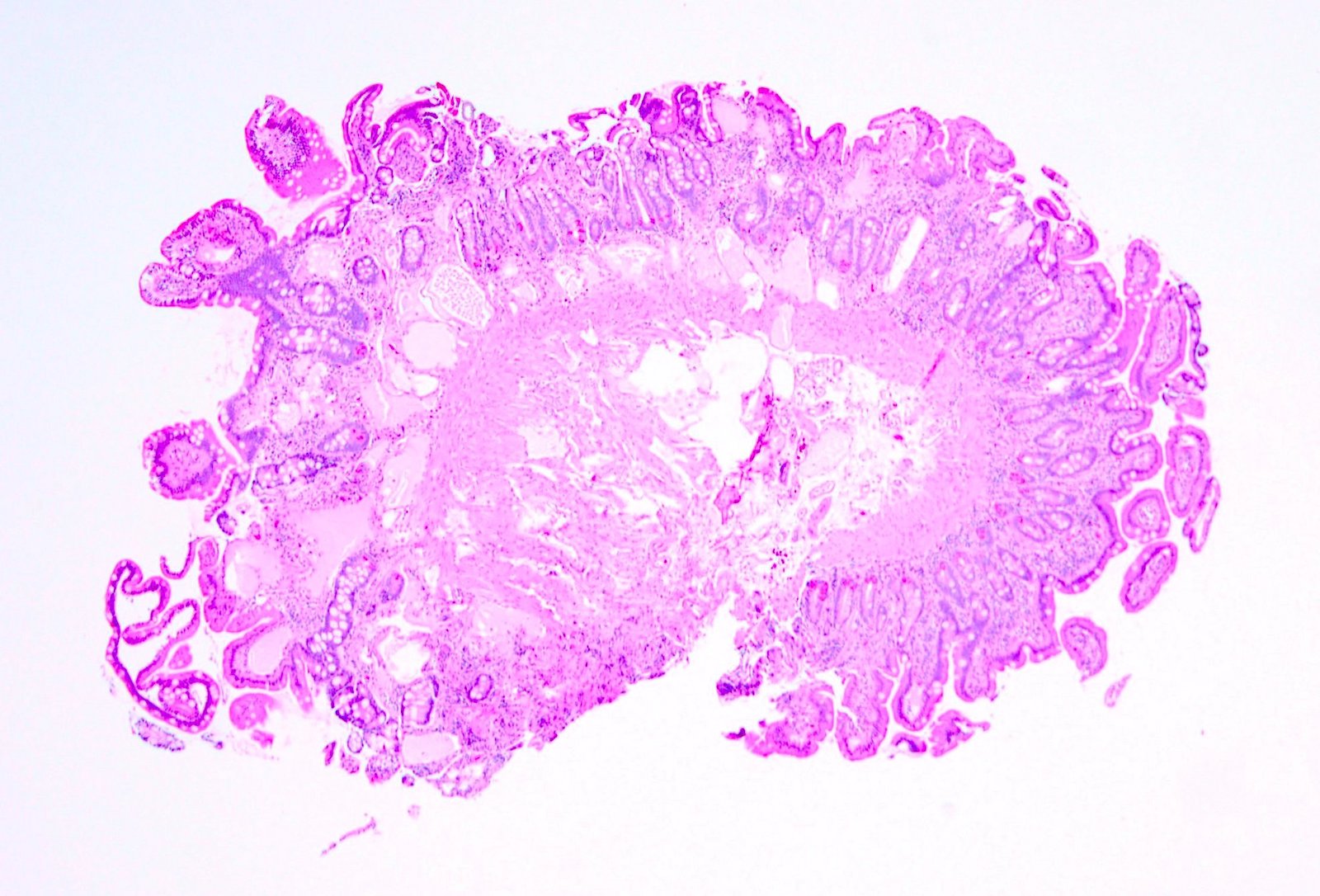
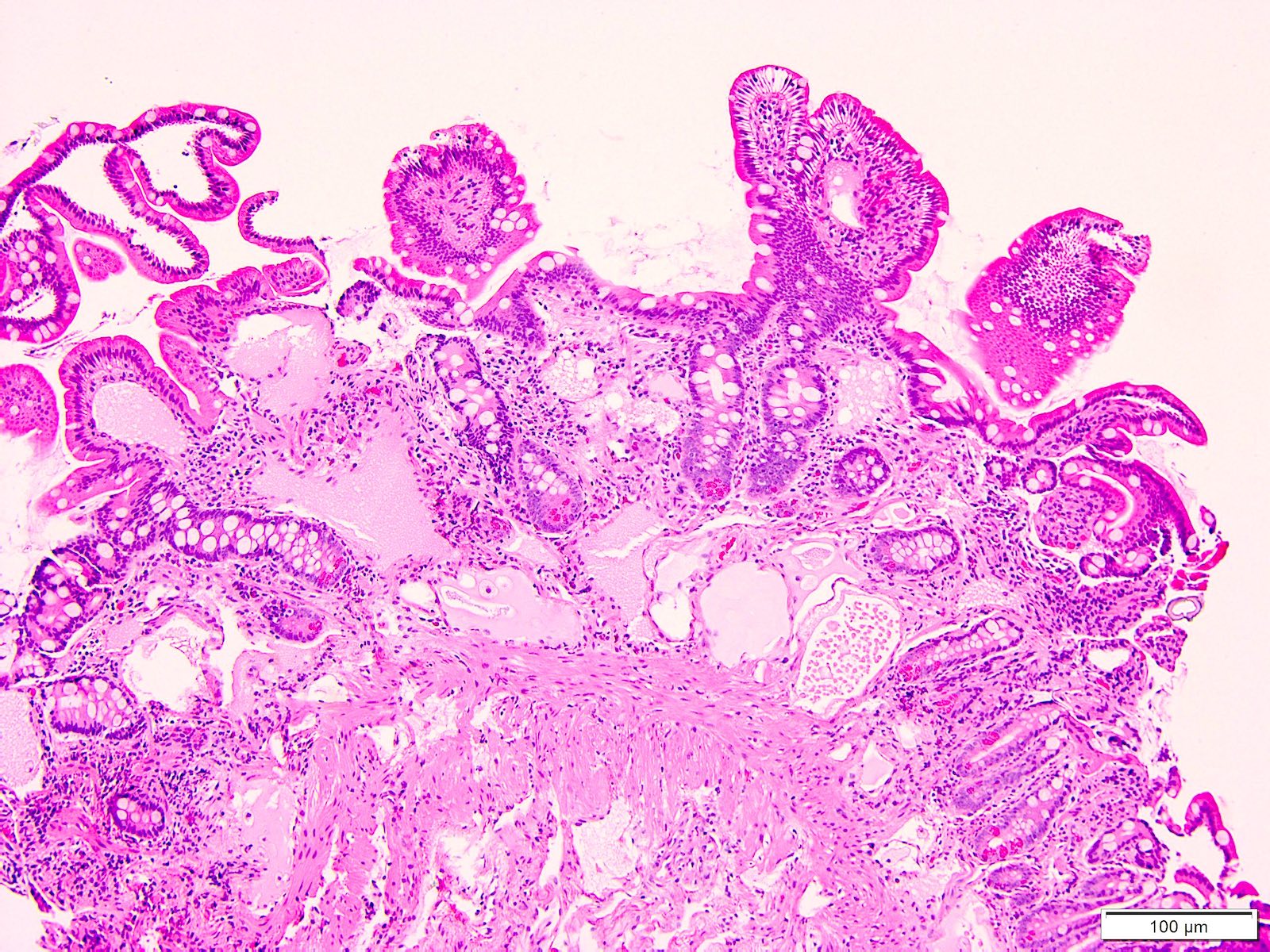
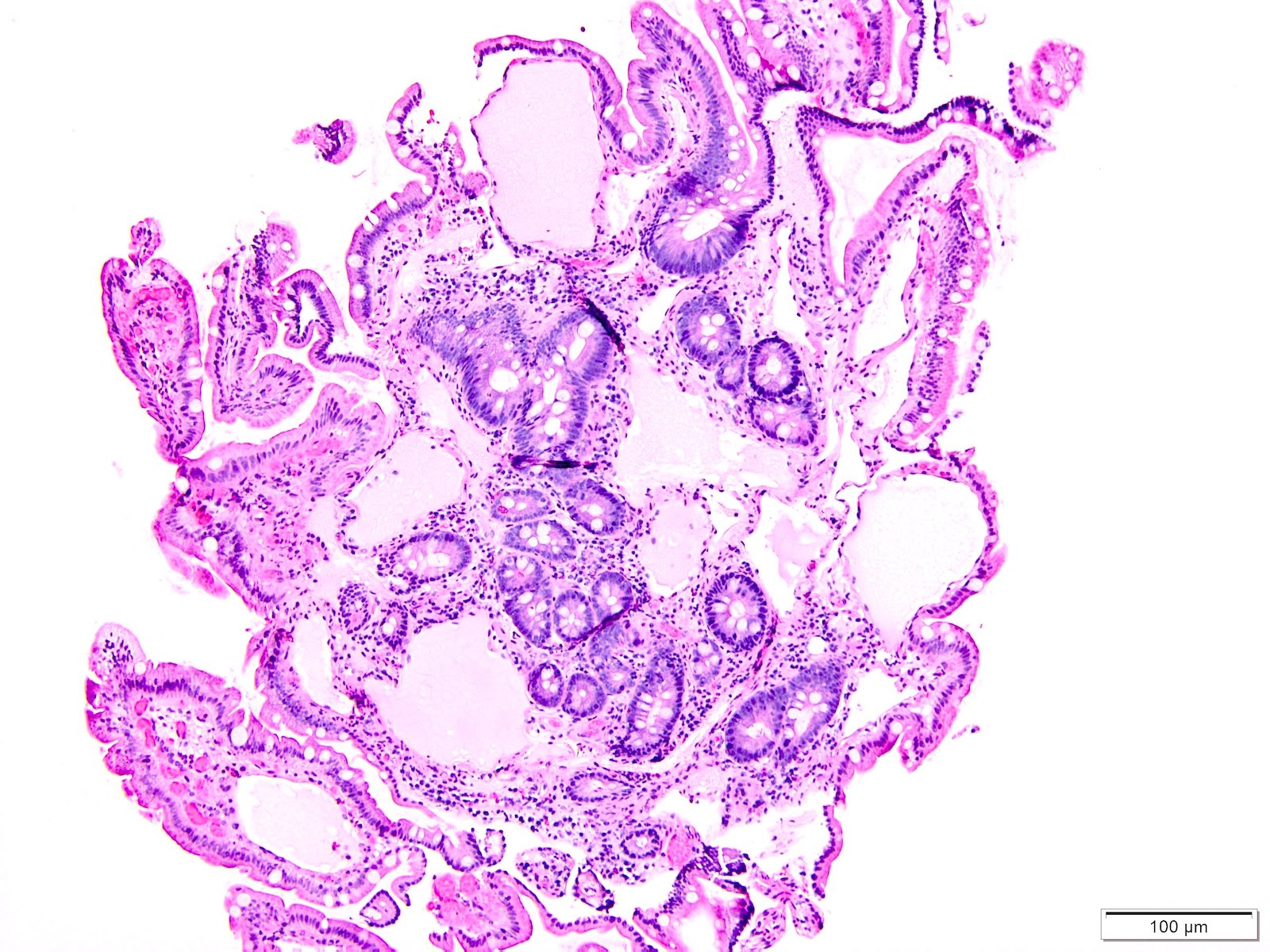
Microscopic (histologic) description
- Moderately to severely dilated mucosal and submucosal lymphatic vessels with polyclonal normal plasma cells (Orphanet J Rare Dis 2008;3:5)
- Intestinal lymphatics may be dilated in few or many villi
- No histologic difference between primary and secondary lymphangiectasia
Microscopic (histologic) images
Positive stains
- Lymphatic vessels are D2-40 positive
Negative stains
Sample pathology report
- Small intestine, biopsy:
- Small bowel lymphangiectasia (see comment)
- Comment: Small bowel lymphangiectasia can be primary or secondary to other conditions such as constrictive pericarditis, intestinal lymphoma, lymphenteric fistula, Whipple disease, Crohn's disease, sarcoidosis, intestinal tuberculosis, systemic sclerosis, radiation or chemotherapy with retroperitoneal fibrosis and human immunodeficiency virus related enteropathy.
Differential diagnosis
- Lymphangioma (Am J Clin Pathol 2015;144:563):
- Presents as a discrete lesion
- Most reliable histologic features distinguishing lymphangioma from lymphangiectasia are the presence of smooth muscle surrounding the lymphatic spaces and complete circumferential lining of spaces by endothelial type cells present in lymphangioma
- Lymphoid aggregates may often be seen in lymphangiomas
Board review style question #1
A 10 year old presented with bilateral edema of the legs and diarrhea. Laboratory evaluation showed hypoalbuminemia and hypogammaglobinemia. No other abnormality was identified. Capsule endoscopy performed showed white granular surface in the small intestine. A biopsy was performed which showed dilated spaces in the mucosa and submucosa. PAS stain performed is negative. What is the most likely cause of the patient's underlying condition?
- Crohn's disease
- Primary lymphangiectasia
- Ulcerative colitis
- Whipple disease
Board review style answer #1