Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Videos | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Ghani H, He J. Chronic gastritis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/stomachchronicgastritis.html. Accessed August 18th, 2025.
Definition / general
- Chronic gastritis is a chronic inflammatory condition of the gastric mucosa that can lead to structural change in the stomach lining (mucosal atrophy, epithelial metaplasia)
Essential features
- Persistent inflammatory infiltrate in the gastric mucosa (mainly lymphocytes and plasma cells)
- 3 main types of chronic gastritis
- Autoimmune gastritis - characteristic destruction of parietal cells
- Helicobacter pylori (H. pylori) induced gastritis
- Reactive (chemical) gastropathy - due to the presence of various chemicals or irritants (e.g., chemicals, medications, bile, alcohol)
- Most cases are nonautoimmune gastritis
- Atrophic changes, including thinning of the mucosal epithelium and loss of gastric glands
- Presence of intestinal metaplasia in severe cases
Terminology
- Atrophic gastritis
- H. pylori associated gastritis
- Autoimmune gastritis (type A gastritis)
- Reactive (chemical) gastropathy
- Gastritis chronica
ICD coding
Epidemiology
- Chronic gastritis is a common condition that affects up to 60% of people worldwide (Gut 2018;67:430)
- Can affect individuals of all ages, incidence increases with age (Gut 2018;67:430)
- H. pylori induced gastritis is prevalent in areas with poor sanitation
- Autoimmune gastritis is typically seen in patients with other autoimmune conditions and often affects older individuals
- Prevalence is higher in smokers, heavy alcohol users and those who use NSAIDs regularly
Sites
- Gastric mucosa, predominantly affecting the antrum and body of the stomach
- May affect the entire stomach in cases of severe atrophic gastritis or autoimmune gastritis
Pathophysiology
- Exact pathophysiology of chronic gastritis is not fully understood but it is thought to be caused by a combination of factors that damage the stomach lining; these factors can include (Scand J Gastroenterol Suppl 1994;201:7, J Evid Based Med 2021;14:161, Arch Pathol Lab Med 2019;143:1327)
- H. pylori infection: H. pylori is a bacterium that can live in the stomach lining; it can irritate the lining and cause inflammation
- Autoimmune conditions: autoimmune destruction of parietal cells and intrinsic factor, leading to gastric atrophy, vitamin B12 deficiency and pernicious anemia
- Long term NSAID use: NSAIDs (nonsteroidal anti-inflammatory drugs) can irritate the stomach lining and increase the risk of gastritis
- Bile reflux: if bile flows back up from the intestine into the stomach, it can irritate the stomach lining and cause inflammation
- Other factors: other factors that may contribute to chronic gastritis include smoking, alcohol abuse, stress and certain foods
- Chronic inflammation: infiltration of lymphocytes, plasma cells lead to mucosal damage
- Atrophy: progressive loss of gastric glands results in thinning of the mucosal layer
- Intestinal metaplasia: considered an adaptive response to chronic injury or inflammation; gastric epithelium may be replaced by intestinal type epithelium, which can increase the risk of gastric adenocarcinoma
Etiology
- Infectious causes: H. pylori infection is the leading cause of chronic gastritis, often resulting in antral gastritis; other infections are less common and include
- Viral infection (e.g., cytomegalovirus, herpes simplex virus in immunocompromised patients)
- Fungal infection (e.g., Candida species)
- Parasitic infection (e.g., strongyloidiasis, anisakis) (Am J Gastroenterol 1997;92:2116, Acta Parasitol 2022;67:94)
- Autoimmune causes: autoimmune destruction of gastric parietal cells
- Chemical causes
- Chronic use of nonsteroidal anti-inflammatory drugs (NSAIDs)
- Bile reflux (backflow of bile into the stomach from the duodenum)
- Excessive alcohol consumption
- Smoking or exposure to other toxins
- Other causes
- Dietary factors (e.g., high salt food or spicy foods)
- Prolonged physiological stress
- Granulomatous disease conditions, such as Crohn's disease
- Exposure to therapeutic radiation for abdominal malignancy
Clinical features
- Symptoms are often nonspecific and may include epigastric pain, bloating, nausea and dyspepsia (Dig Endosc 2022;34:700, Zhongguo Dang Dai Er Ke Za Zhi 2022;24:1340)
- H. pylori infection may present with more severe symptoms or complications, such as ulcers
- Autoimmune gastritis may manifest with signs of vitamin B12 deficiency, including fatigue and anemia
- May be asymptomatic in the early stages, especially in the case of H. pylori associated gastritis
- Histology does not correlate well with symptoms
Diagnosis
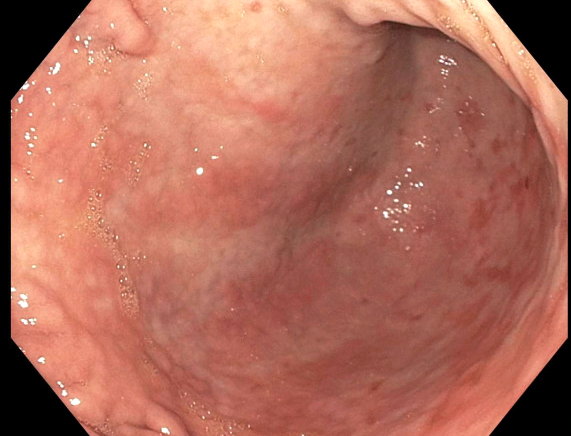
- Esophagogastroduodenoscopy (EGD): direct visualization of gastric lining to identify inflammation, erosions, erythema, atrophy, friability or ulcer (Gastroenterology 2021;161:1325, Dig Endosc 2022;34:700)
- Biopsy: gastric tissue samples taken during endoscopy are analyzed histologically to identify inflammatory infiltrates, glandular atrophy, intestinal metaplasia, dysplasia or malignancy
- H. pylori associated gastritis: biopsy samples can be tested for H. pylori using special stains, immunohistochemical stain, PCR or bacterial culture; noninvasive methods include the urea breath test, stool antigen test and serological testing
- Autoimmune gastritis: histological findings with correlated clinical and serological evidence are required
Laboratory
- Iron deficiency: microcytic anemia (Helicobacter 2003;8:573)
- H. pylori tests: invasive techniques include histological evaluation or urease test or culture on the gastric biopsy; noninvasive techniques include urea breath test, stool antigen test or serology (Am J Med 1996;100:35S)
- Vitamin B12 deficiency: macrocytic anemia, elevated methylmalonic acid
- Gastrin levels: elevated in autoimmune gastritis due to loss of acid production by parietal cells
- Antibody detection: antiparietal cell antibodies or anti-intrinsic factor antibodies are commonly seen in autoimmune gastritis (JAMA Oncol 2022;8:268, Diagnostics (Basel) 2023;13:1599)
Radiology description
- Barium Xray fluoroscopy: mucosal irregularities, delayed gastric emptying, abnormal gastric folds and reduced elasticity seen in chronic gastritis with significant fibrosis or atrophy
- Endoscopic findings of chronic gastritis vary depending on the severity and underlying
cause of the inflammation (J Clin Med 2022;11:3523, Dig Endosc 2015;27:53)
- H. pylori associated gastritis
- Diffuse erythema
- Nodular or granular appearance of the antral mucosa
- Atrophy and intestinal metaplasia in advanced cases
- Autoimmune gastritis
- Pallor and thinning of the mucosa, primarily in the body and fundus of the stomach
- Loss of gastric rugae (folds) in severe atrophic cases
- Chemical (reactive) gastritis
- Erosions or superficial ulcerations
- Mucosal hemorrhages
- Bile stained gastric contents or signs of bile reflux
- Advanced endoscopic findings include intestinal metaplasia, dysplasia or malignancy
- Intestinal metaplasia: may appear as patchy or flat, pale areas
- Chronic gastritis may progress to dysplasia or cancer, which may appear as irregular, raised or ulcerated lesions
- H. pylori associated gastritis
Prognostic factors
- Favorable prognosis: early treatment of H. pylori infection often leads to full mucosal healing
- Unfavorable prognosis (Dig Endosc 2022;34:700, World J Gastroenterol 2014;20:5461)
- Longstanding or untreated gastritis increases the risk of developing gastric carcinoma, neuroendocrine tumors and MALT (mucosa associated lymphoid tissue) lymphoma
- Presence of intestinal metaplasia or dysplasia is a precancerous change and considered a poor prognostic factor
- Chronic inflammation increases the risk of ulcers, bleeding or perforation
- Potential recurrence with persistent H. pylori infection or continued NSAID use
Case reports
- 48 and 54 year old men were referred for medical checkups without any particular symptoms (Intern Med 2016;55:1865)
- 53 year old otherwise healthy woman admitted to the emergency department following 2 bouts of hematemesis and a single melanic stool (Drug Healthc Patient Saf 2015;7:31)
- 54 year old woman with heartburn and epigastric pain associated with bloating, gas and sometimes constipation (Cureus 2023;15:e42172)
Treatment
- Proton pump inhibitors: used to reduce gastric acid secretion and promote mucosal healing in all forms of chronic gastritis
- Protective agents: help to prevent further irritation and promote healing (e.g., bismuth)
- H. pylori associated gastritis
- Bismuth quadruple therapy (proton pump inhibitor [PPI], bismuth, tetracycline and nitroimidazole)
- Rifabutin triple therapy (PPI, rifabutin and amoxicillin)
- Dual therapy (potassium competitive acid blocker and amoxicillin) (Am J Gastroenterol 2024;119:1730)
- Autoimmune gastritis: PPI therapy; vitamin B12 supplementation if B12 deficient
- Chemical (reactive) gastritis: discontinue the causative agent
- Lifestyle changes, such as avoiding smoking and alcohol
Clinical images
Gross description
- Gastric mucosa may show erythema, mucosal nodularity or superficial erosions (Endoscopy 2003;35:946)
- In severe cases, areas of erosion or ulceration may be present
- In atrophic gastritis, the gastric mucosa may appear thin and pale, with flattening or loss of rugal folds, particularly in the body and fundus in autoimmune gastritis (Gastroenterology 2021;161:1325)
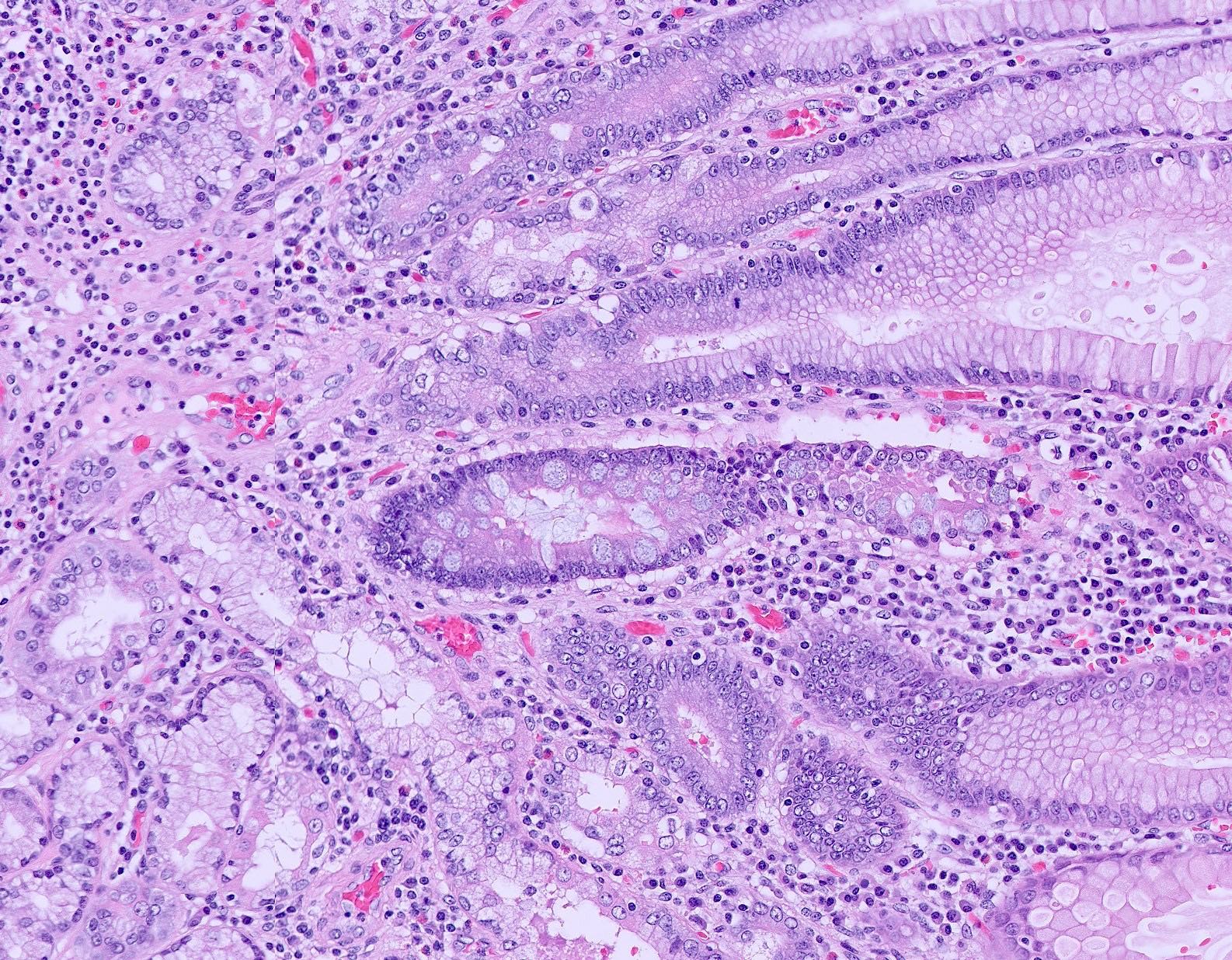
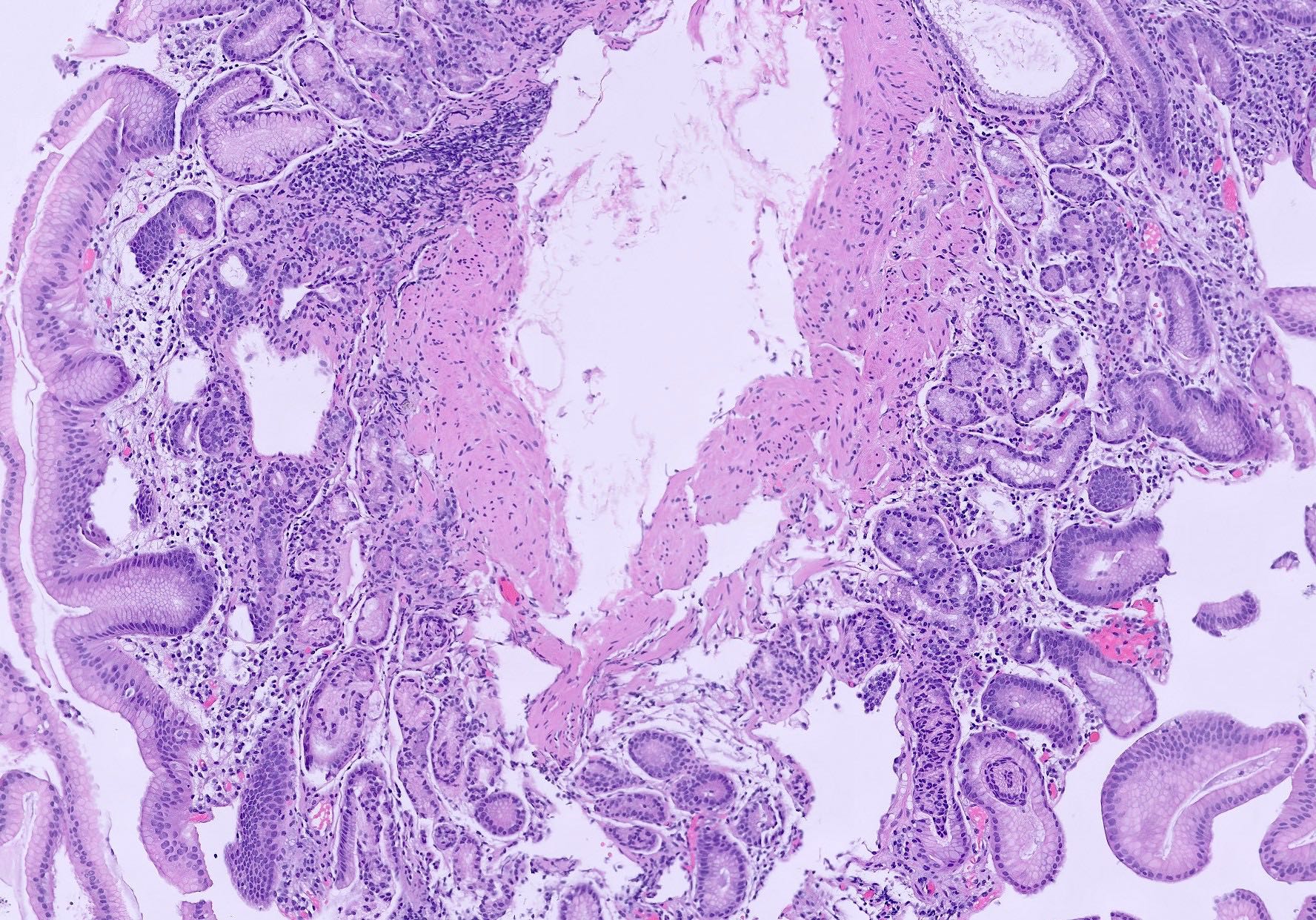
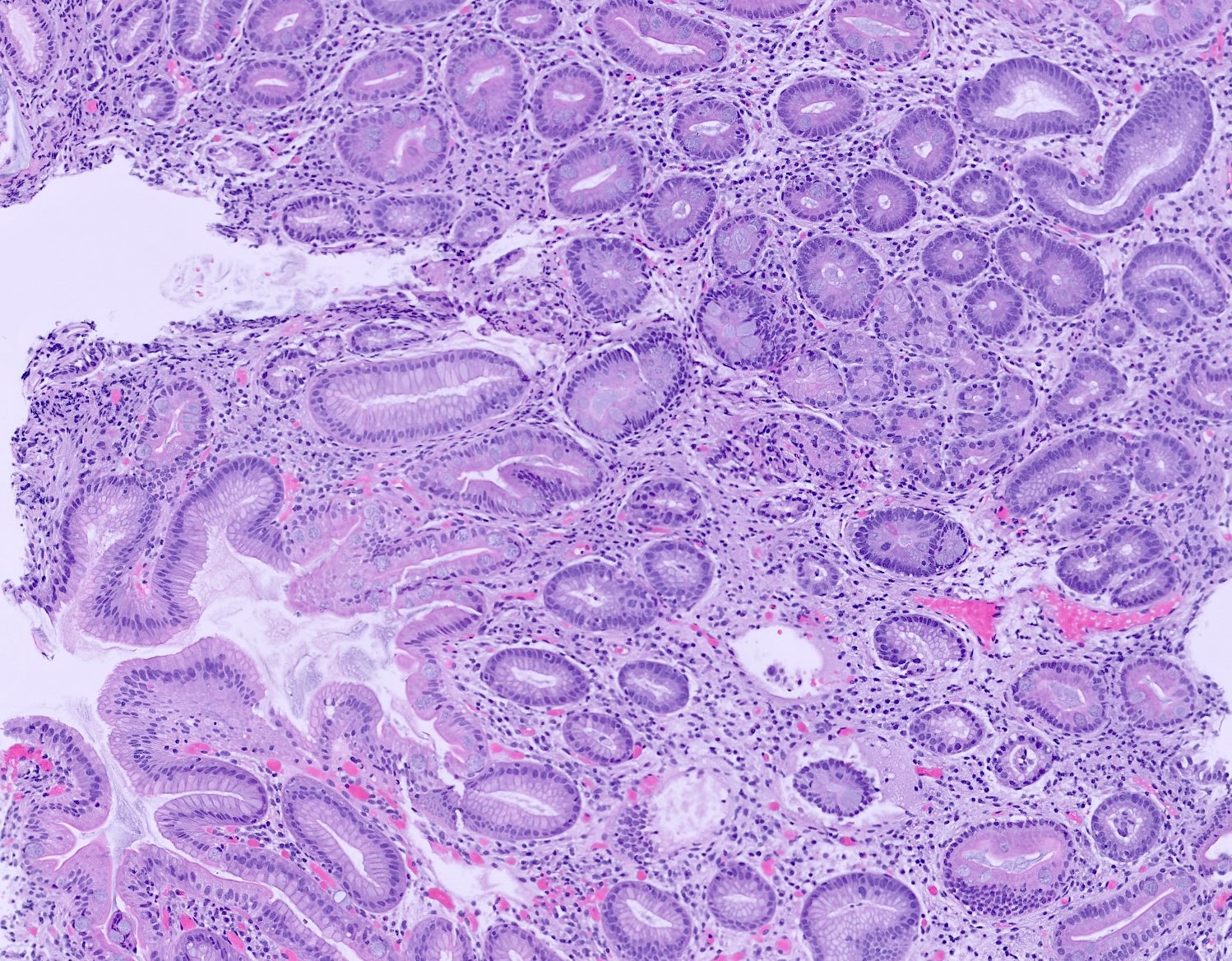
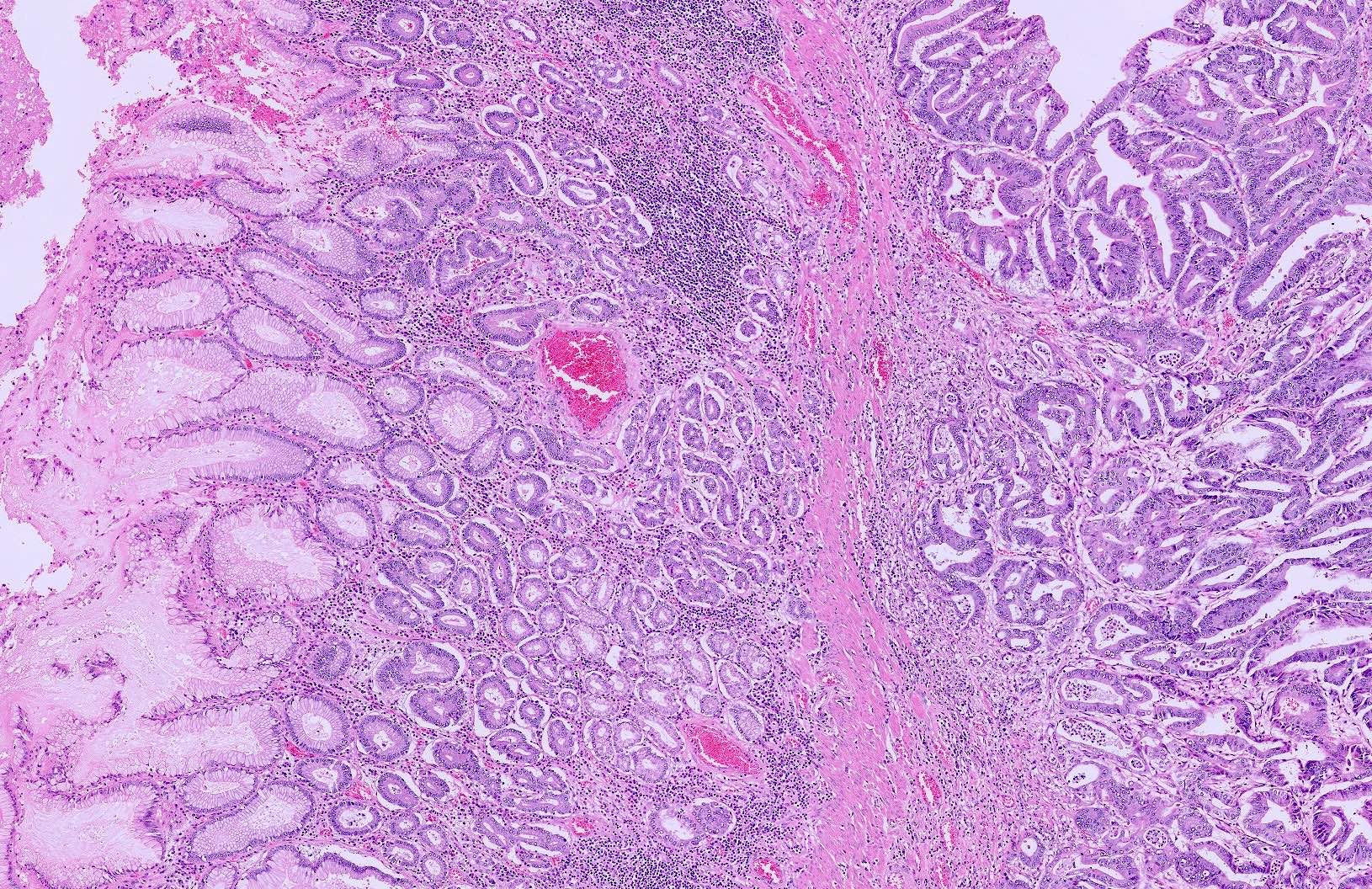
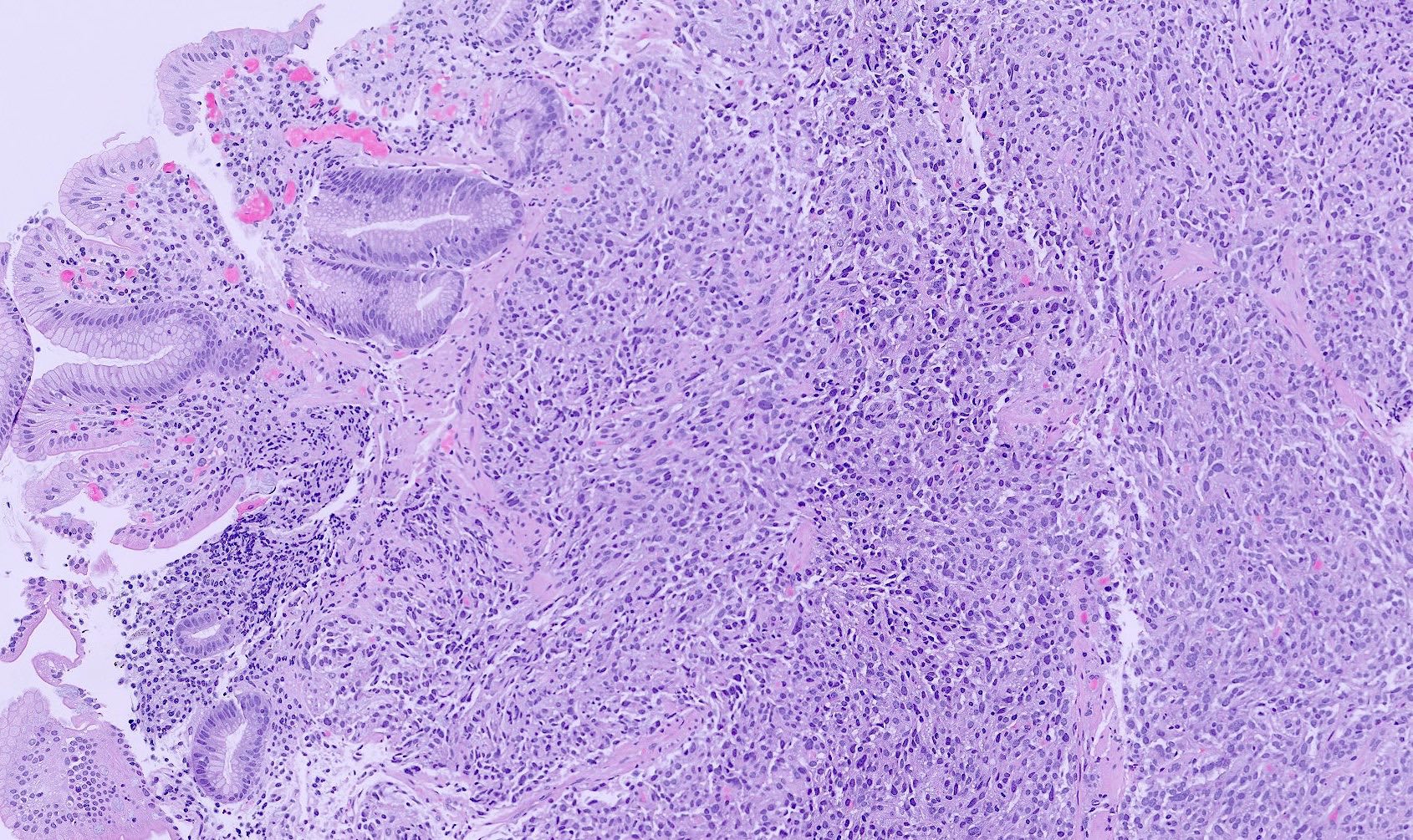
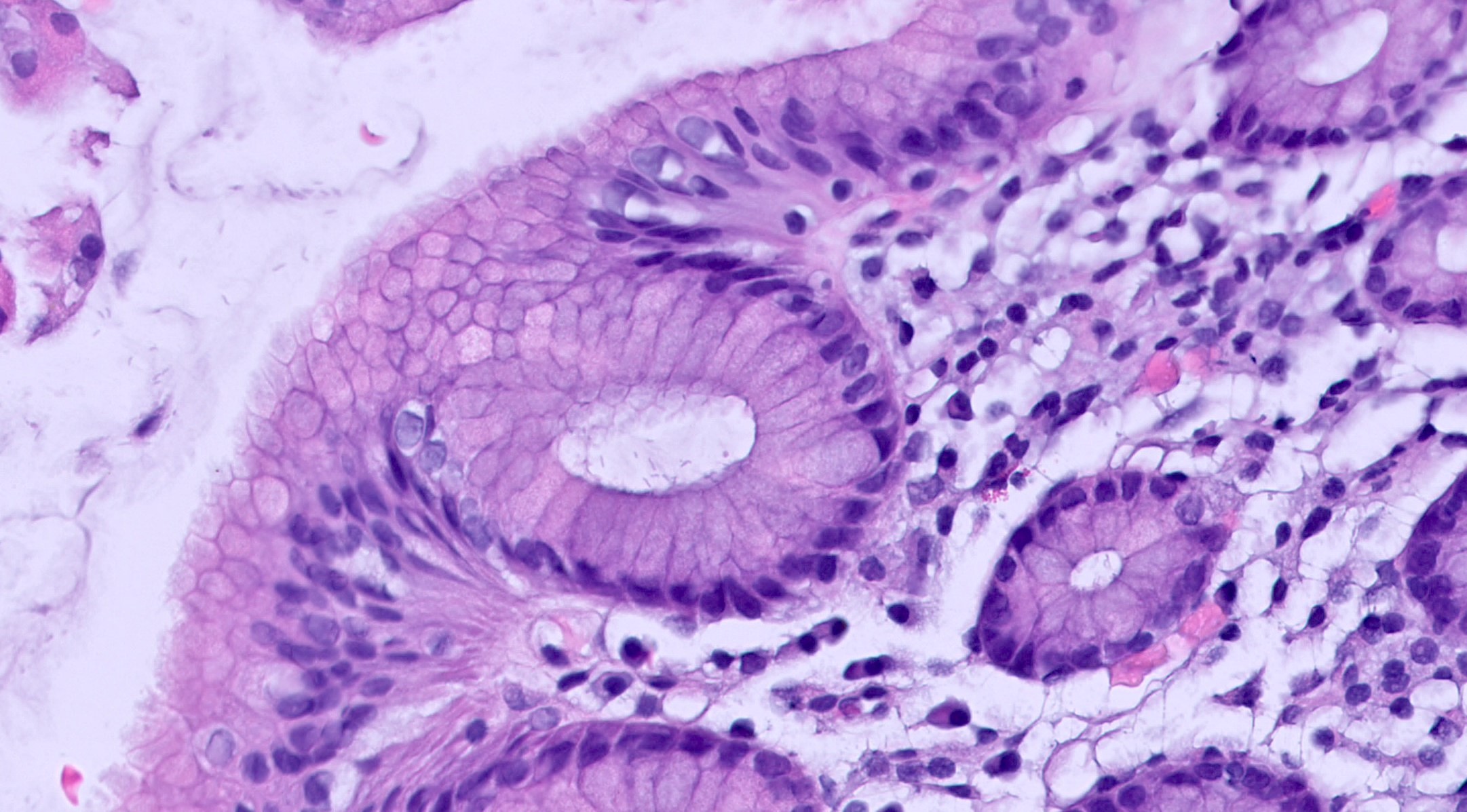
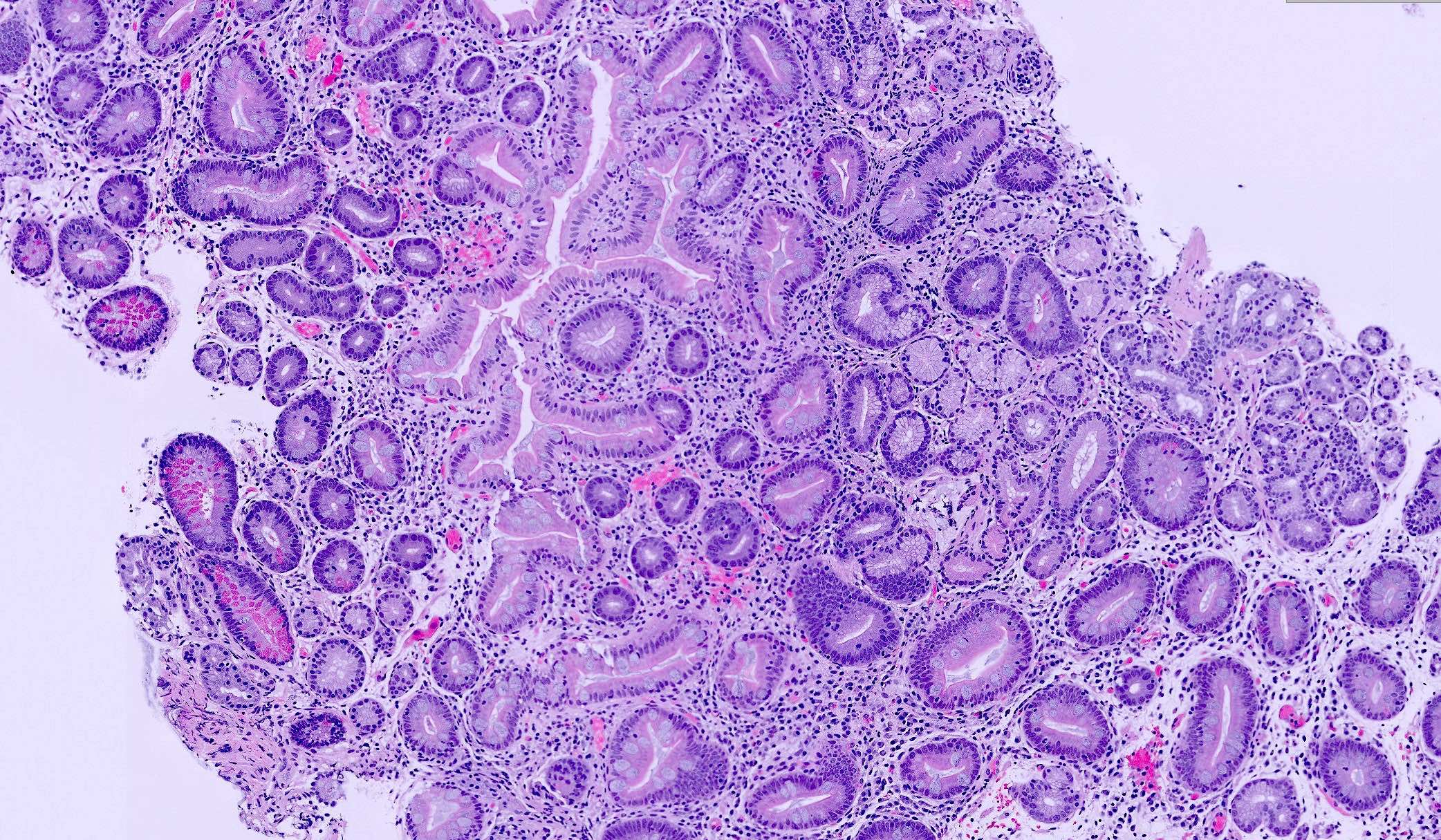
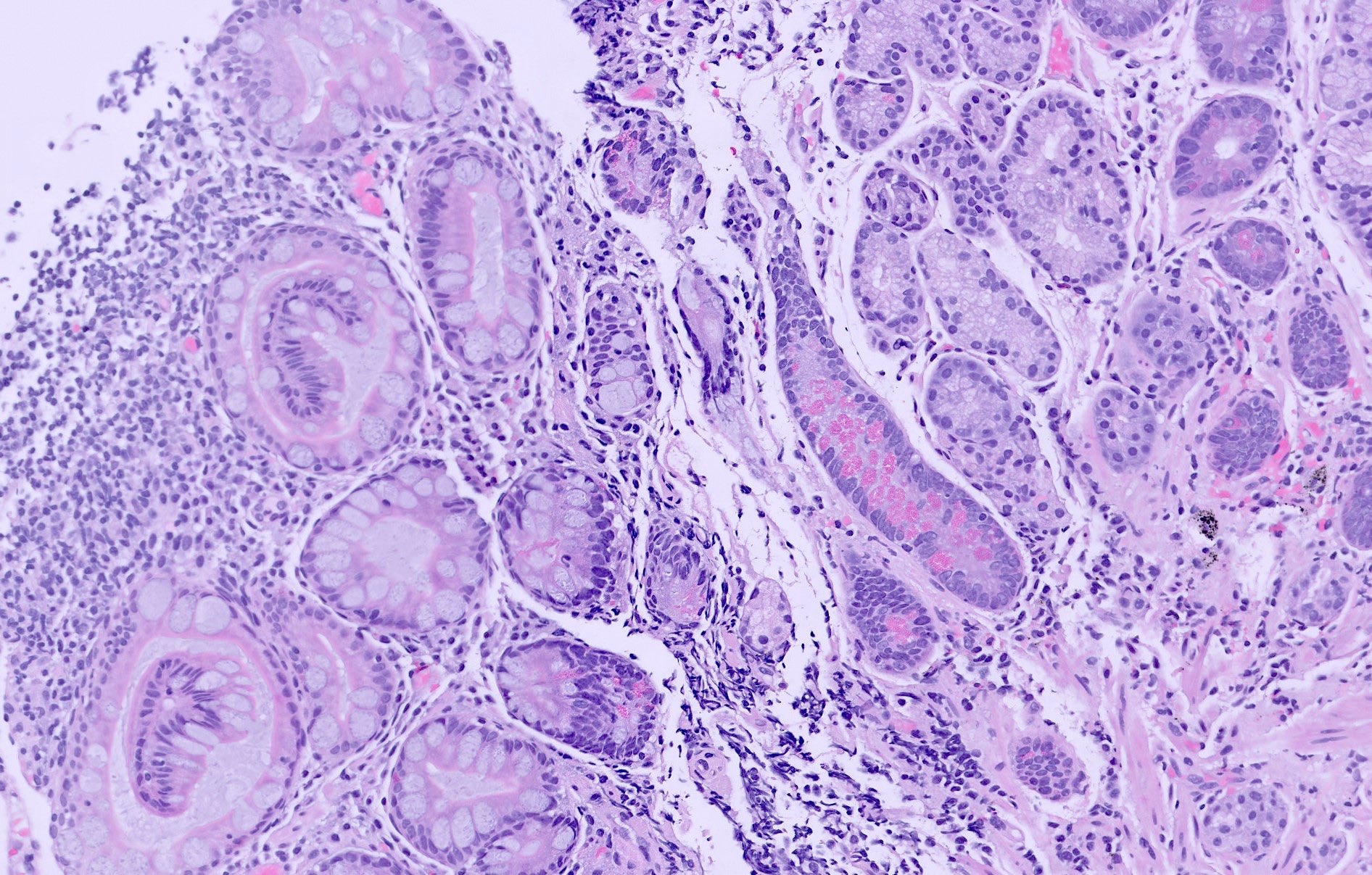
Microscopic (histologic) description
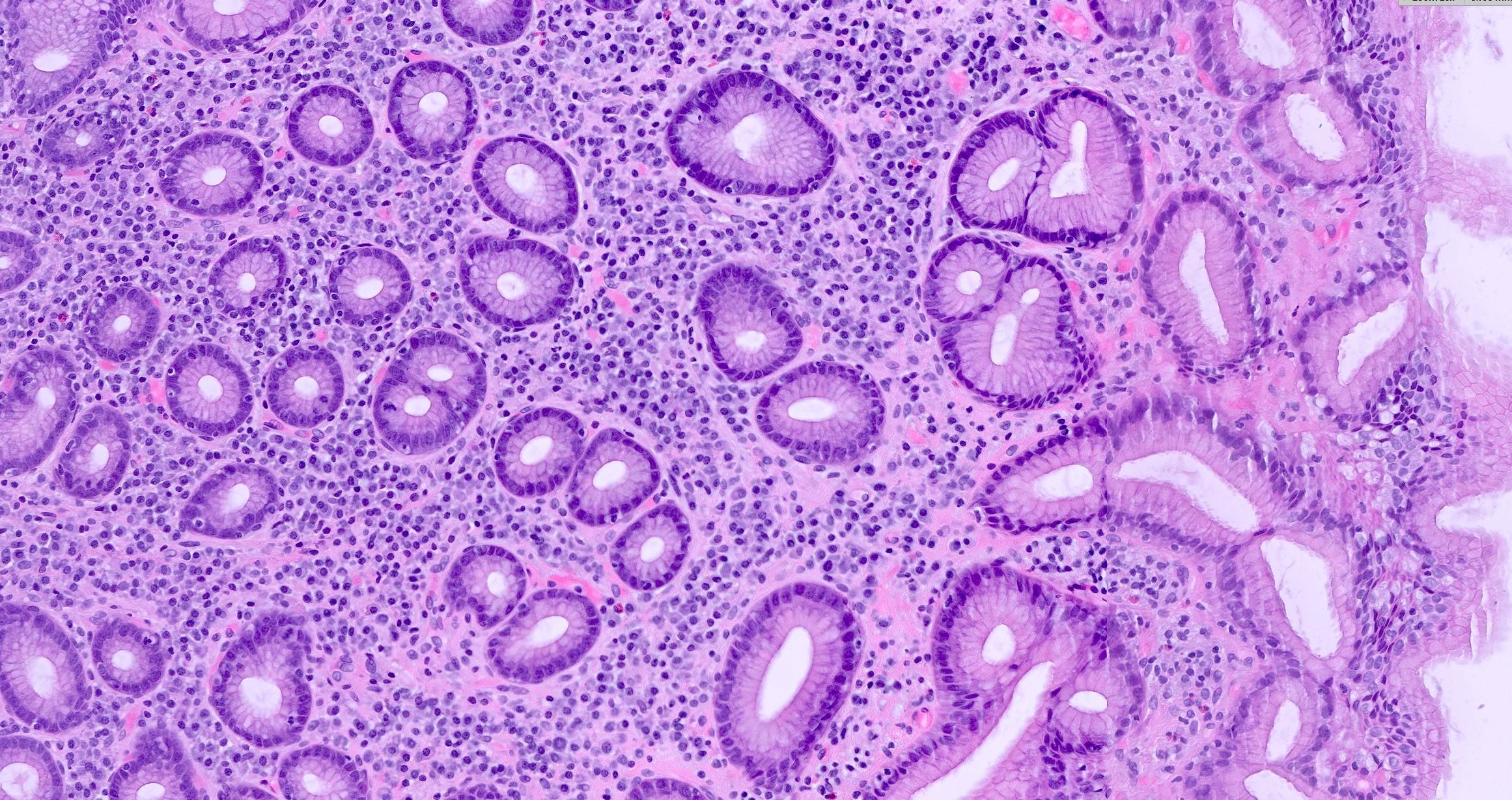
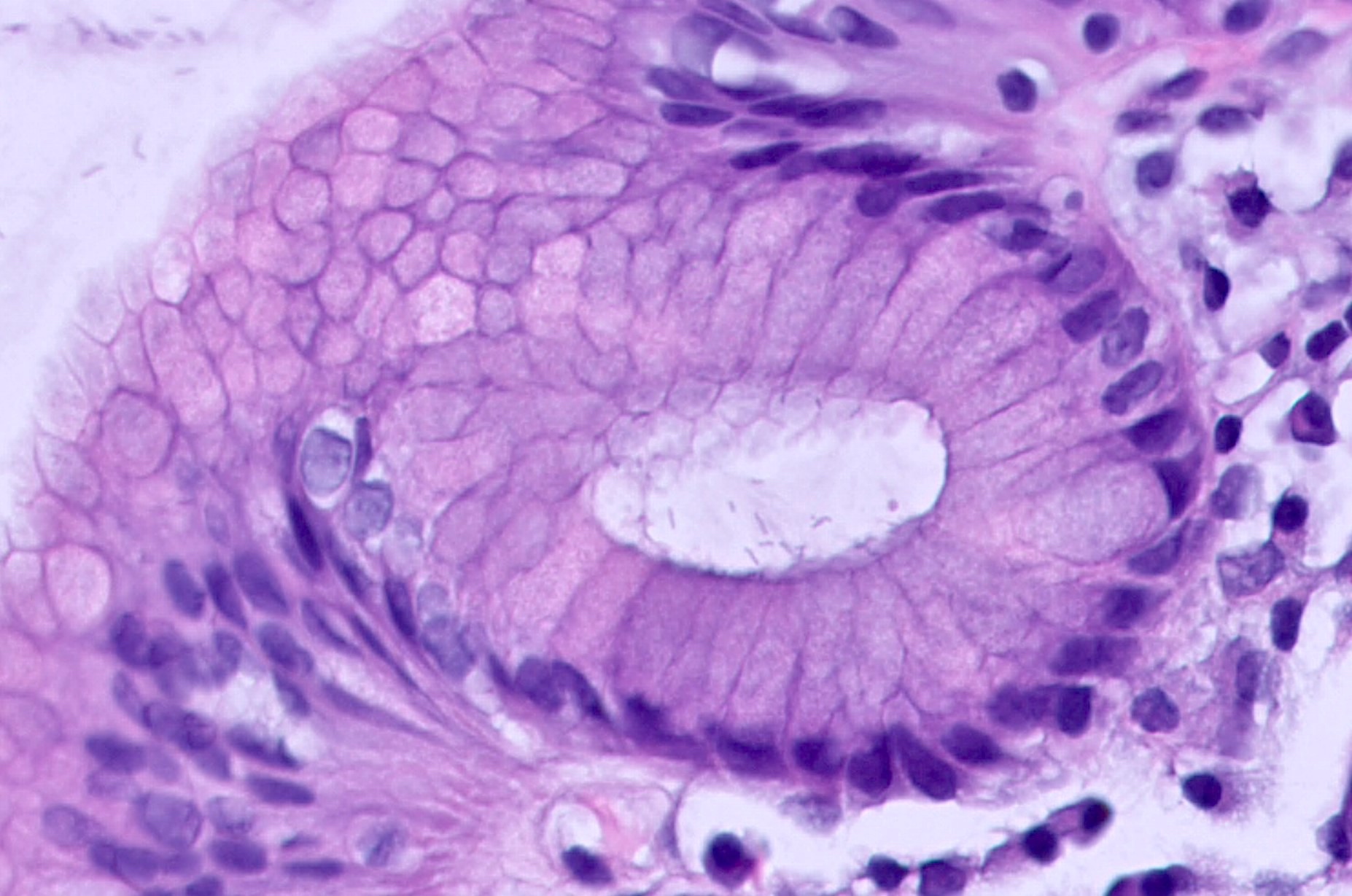
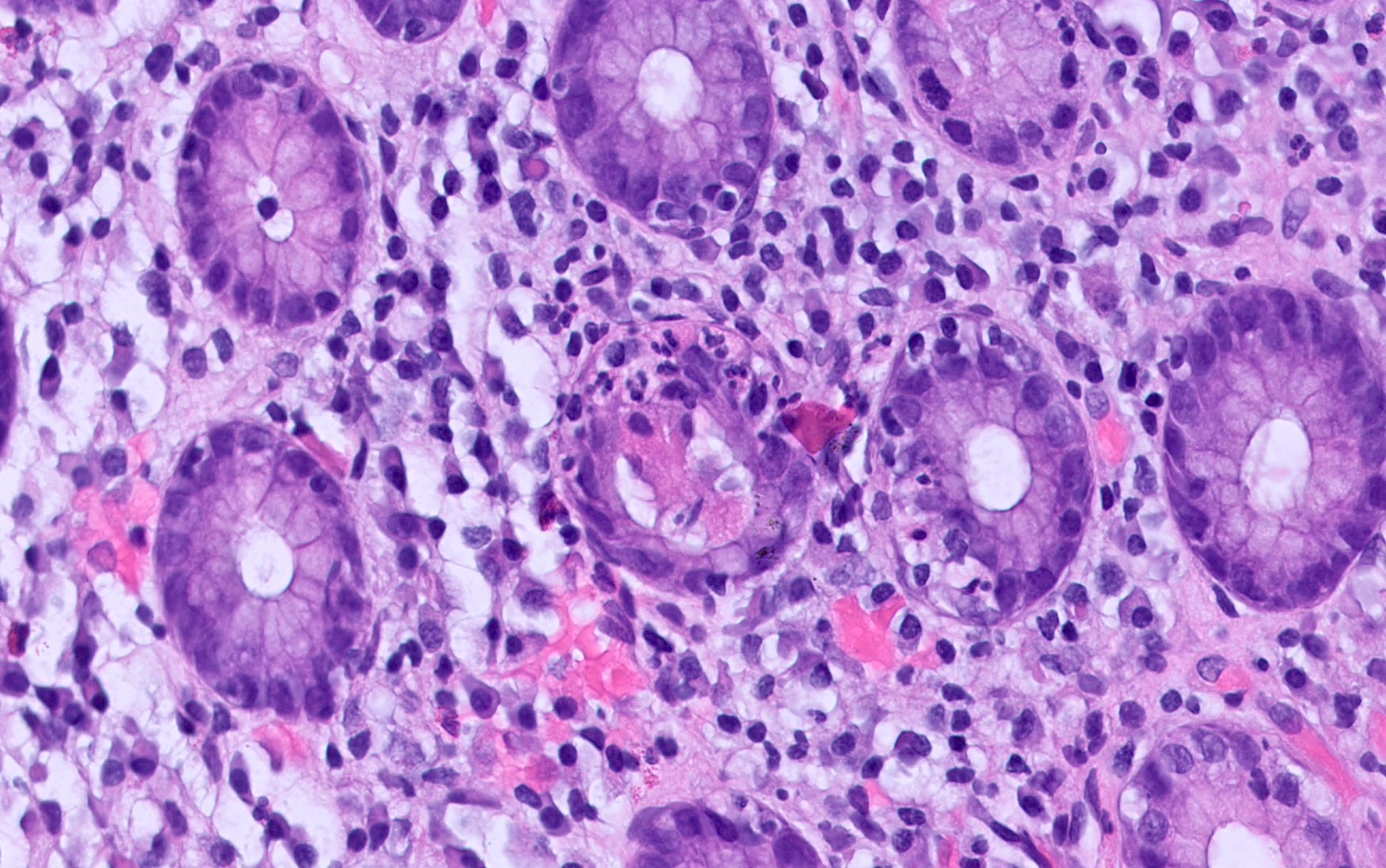
- Infiltrate of lymphocytes and plasma cells in the lamina propria of the gastric mucosa (Am J Surg Pathol 1996;20:1161)
- Prominent lymphoid aggregates, sometimes with germinal centers, may be seen, particularly in H. pylori associated gastritis
- Neutrophils may be present in active chronic gastritis; severe cases may show epithelial disruption, loss of the mucosal surface or ulceration
- Chronic inflammation and damage may result in fibrosis within the lamina propria
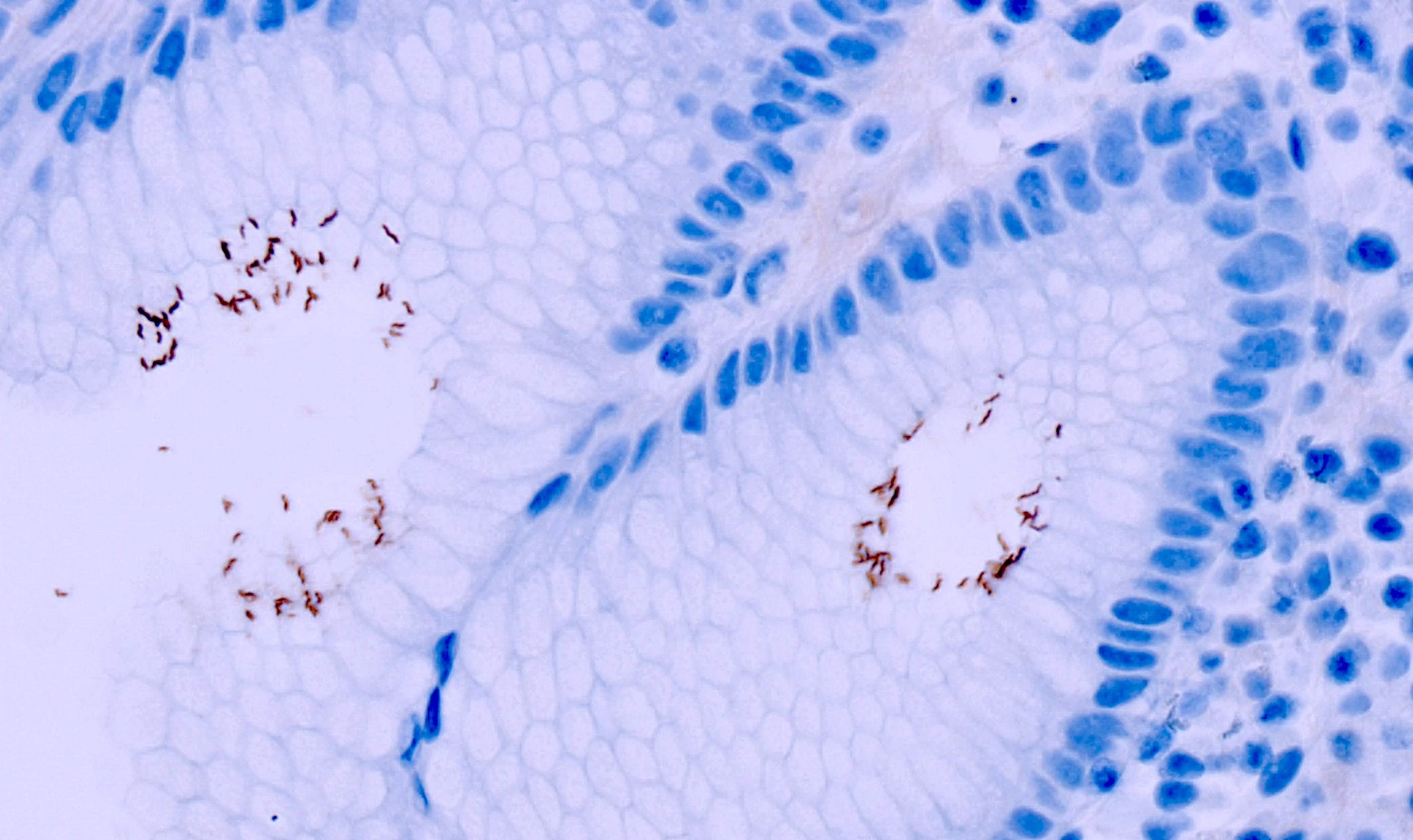
- H. pylori bacteria can be identified on the gastric epithelium, typically localized in the antrum
- Loss of gastric glands and thinning of the mucosal epithelium are features of chronic atrophic gastritis
- Loss of parietal and chief cells and endocrine cell hyperplasia are characteristic features of autoimmune gastritis (Arch Pathol Lab Med 2019;143:1327)
- Intestinal metaplasia: replacement of gastric glands with goblet cells and intestinal type columnar epithelium
- In response to chronic irritation, there may be elongation and tortuosity of foveolar glands, accompanied by mucus hypersecretion
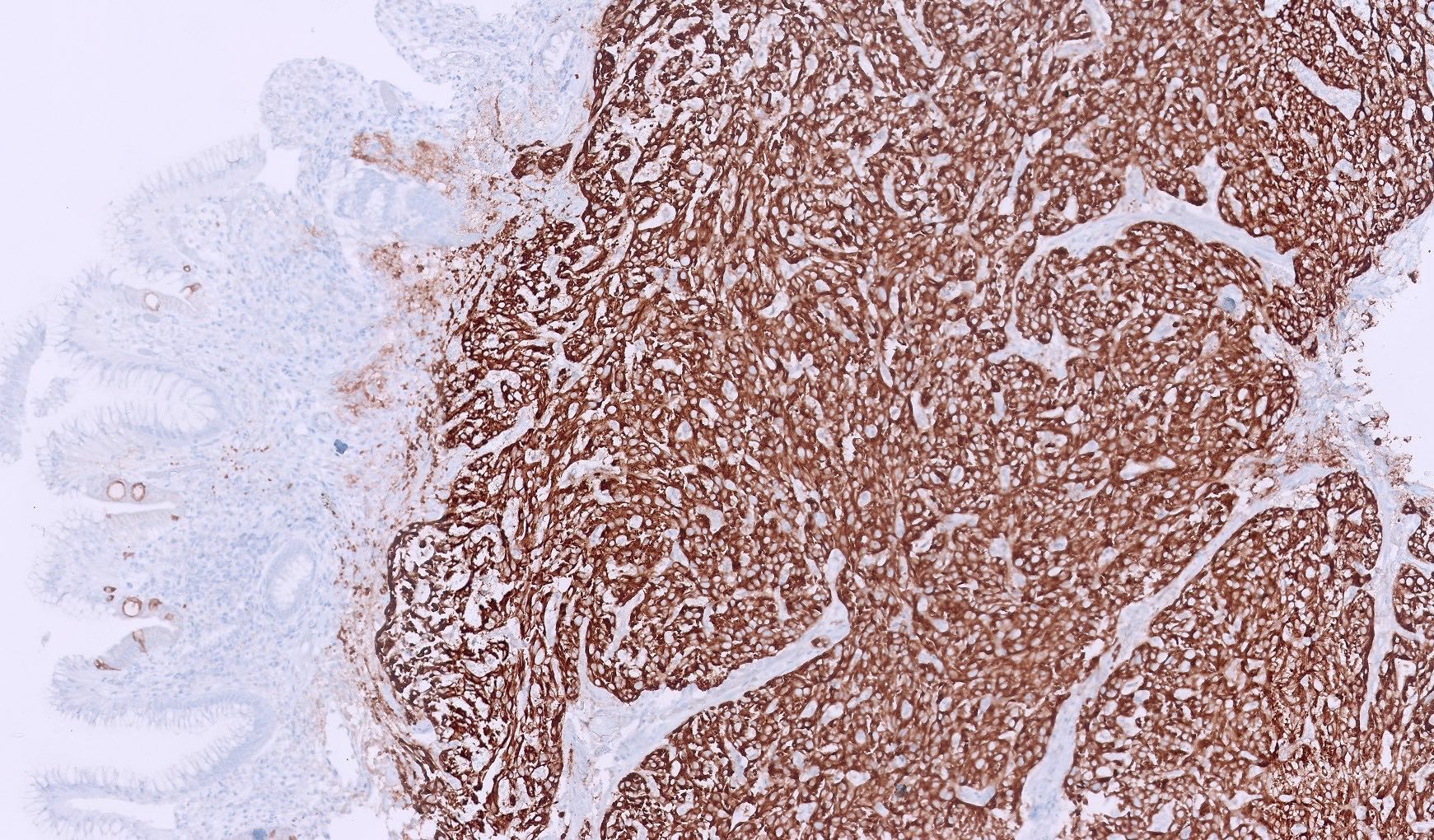
Microscopic (histologic) images
Contributed by Hafiz Ghani, M.D.
Virtual slides
Positive stains
- H. pylori can be highlighted by immunohistochemistry or special stain (e.g., Warthin-Starry) (Front Oncol 2023;13:1229871, Arch Pathol Lab Med 2008;132:1586)
- Intestinal metaplasia can be highlighted by Alcian blue (Am J Surg Pathol 2006;30:357)
- Enterochromaffin-like cell (ECL) hyperplasia can be highlighted by synaptophysin and chromogranin (Adv Anat Pathol 2020;27:193)
Videos
Pathology of gastric disorders - chronic gastritis
Sample pathology report
- Stomach, antrum, biopsy:
- Gastric antral mucosa with active chronic gastritis
- Intestinal metaplasia identified
- No dysplasia identified
- No H. pylori organisms identified
Differential diagnosis
- Lymphocytic gastritis:
- > 20 - 25 intraepithelial lymphocytes/100 epithelial cells
- Gastric lymphoma:
- Mass lesion with sheets of neoplastic lymphocytes
- Infiltrative pattern with lymphoepithelial lesions and architectural distortion
Additional references
- Hum Pathol 2021;116:31, World J Clin Cases 2021;9:6686, Pediatr Rev 2020;41:585, Medicine (Baltimore) 2020;99:e21985, Aliment Pharmacol Ther 2012;35:1310, J Pediatr Gastroenterol Nutr 2012;55:728, Pediatr Dev Pathol 2012;15:101, Pediatr Dev Pathol 2005;8:420, J Gastroenterol 2004;39:734, Fetal Pediatr Pathol 2004;23:11, Am J Surg Pathol 2004;28:1347, Pediatr Dev Pathol 2003;6:209, Curr Opin Pediatr 2000;12:460, Arch Med Res 2000;31:431, Ann Diagn Pathol 2000;4:279, Gastrointest Endosc Clin N Am 2001;11:717
Practice question #1
Practice answer #1
A. Chronic Helicobacter associated gastritis. The image shows infiltration of inflammatory cells (lymphocytes and plasma cells) into the lamina propria and H. pylori organisms are observed in the gastric epithelium, which are characteristic features of H. pylori associated chronic gastritis. Answer C is incorrect because there is significant inflammation and H. pylori present in the image. Answer B is incorrect because there are no invasive neoplastic cells and the architectural distortion or glandular atypia typical of neoplastic processes is not observed. Answer D is incorrect because there are no surface neutrophils, necrotic debris or granulation tissue present, which are features indicative of peptic ulcer.
Comment Here
Reference: Chronic gastritis
Comment Here
Reference: Chronic gastritis
Practice question #2
A 52 year old woman presents with fatigue, tingling in her hands and feet and abdominal discomfort. Neurological examination reveals decreased vibratory sensation in her lower extremities. Laboratory studies reveal macrocytic anemia, positive antiparietal cell antibody and anti-intrinsic factor antibody. Upper endoscopy shows thin gastric mucosa with loss of rugal folds in the body and fundus. A biopsy was taken from the gastric body and the images are shown above. Which of the following is a common complication of the condition shown in the images?
- Gastric hyperacidity
- Gastric lymphoma
- Peptic ulcer disease
- Vitamin B12 deficiency
Practice answer #2
D. Vitamin B12 deficiency. The image shows gastric body mucosa with loss of parietal cells and replacement of gastric glands by intestinal type epithelium. The clinical presentation and biopsy findings suggest autoimmune gastritis as the most likely diagnosis. In autoimmune gastritis, the destruction of parietal cells leads to a loss of intrinsic factor production, impairing vitamin B12 absorption. Vitamin B12 deficiency can cause macrocytic anemia and neurological symptoms. Answer B is incorrect because gastric lymphoma is more commonly associated H. pylori related gastritis, not autoimmune gastritis and is not a direct complication of the latter. Answer C is incorrect because peptic ulcer disease is more commonly associated with H. pylori related chronic gastritis or NSAIDs. Answer A is incorrect because autoimmune gastritis is associated with reduced gastric acid secretion due to the loss of parietal cells, which often results in conditions like achlorhydria (absence of hydrochloric acid) or hypochlorhydria (low acid), rather than gastric hyperacidity.
Comment Here
Reference: Chronic gastritis
Comment Here
Reference: Chronic gastritis