Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Case reports | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Siegmund S, Acosta A. Cysts. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/testiscysts.html. Accessed August 24th, 2025.
Definition / general
- Benign, cystic lesions that may be confused with testicular tumors
- Does not include cystic neoplasms (e.g., epidermoid cyst, dermoid cyst [teratoma], papillary cystadenoma of the epididymis)
Essential features
- Mesothelial cysts and hydrocele constitute benign true cysts and fluid collections arising from the mesothelial lining of the visceral and parietal tunica vaginalis and are more common in children
- Cysts and cystic dilatations of the epididymis and rete testis (or more rarely, the seminiferous tubule) arise from the tubal epithelium, frequently secondary to obstruction and are more common in adults
- Frequently characterized by simple unilocular or multilocular cystic structures and an absence of complex growth / solid areas
Terminology
- Includes true cysts and fluid collections (celes) of the spermatic cord and paratesticular structures
- 2 main types
- Extratesticular (arises from the mesothelial lining [tunica vaginalis] and does not communicate with tubular system)
- Hydrocele
- Encysted presentation does not communicate with peritoneal cavity
- Funicular presentation does communicate with peritoneal cavity
- Mesothelial cyst (also termed spermatic cord cyst)
- Hydrocele
- Testicular (arises from the epithelial lining of the rete testis, efferent ducts and epididymis)
- Epididymal cysts and cystic dilatation (tubular ectasia) of epididymis and rete testis are associated and likely exist on a continuum
- Epididymal cysts > 2 cm within the vaginal cavity are termed spermatocele
- Cystic dysplasia of rete testis is distinctive congenital malformation
- Extratesticular (arises from the mesothelial lining [tunica vaginalis] and does not communicate with tubular system)
ICD coding
Epidemiology
- Hydrocele is one of the most common causes of painless scrotal swelling in infants (up to 10%); generally regresses spontaneously by 1 - 2 years old and rarely persists into adulthood
- Mesothelial cysts are most common in men > 40 years old
- Cysts and cystic dilatation of epididymis and rete testis constitute the most common paratesticular cystic lesions, frequently in men > 55 years old and seen in up to 30% of asymptomatic patients at ultrasound (AJR Am J Roentgenol 1984;143:161)
- Cystic dysplasia of rete testis is rare, generally unilateral and most often seen in children (mean presentation of 5 years old), in association with urinary tract malformations (Front Pediatr 2022;10:898038)
Sites
- Spermatic cord, testicular adnexa
Etiology
- Hydrocele
- Congenital form occurs due to patent processus vaginalis or abnormal closure of processus; most regress by adulthood
- May be associated with trauma, testicular torsion, tumors, chronic inflammation (e.g., in setting of bacterial epidiymoorchitis, filarial disease) or congenital lymphatic malformations
- Mesothelial cyst
- Mesothelial rests trapped during embryonic development (J Urol 1975;114:730)
- Cysts (and cystic dilatation) of epididymis and rete testis
- Acquired condition frequently associated with or resulting from mechanical compression of epididymis or spermatic cord by surgical changes (e.g., vasectomy), trauma, neoplastic or infectious process, dialysis (rete testis cystic dilation) or hormonally induced atrophy of epididymis (e.g., secondary to cirrhosis) (Hum Pathol 1996;27:336, Am J Surg Pathol 1996;20:1231, J Ultrasound 2011;14:208)
- Rare intraparenchymal cystic dilatation of seminiferous tubules may result from focal malformation or inflammation
- Epididymal cysts associated with in utero exposure to diethylstilbestrol
- Cystic dysplasia of rete testis
- Congenital malformation of rete testis, frequently associated with ipsilateral urogenital malformations (e.g., renal agenesis, multicystic dysplasia of the kidney)
- Thought to arise due to disorders of communication between mesonephric duct and germinal epithelium during development (Front Pediatr 2022;10:898038)
Clinical features
- Painful or painless cystic swelling of the scrotum
- May be incidentally identified
Diagnosis
- Transillumination
- Ultrasonography (Doppler ultrasonography is important in a setting of painful swelling to rule out testicular torsion)
Radiology description
- Varies by entity
- Most frequently characterized by simple uninoculated or multiloculated fluid filled cystic structures
- Complex loculations or areas of solid growth should raise concern for alternative etiology
Radiology images
Images hosted on other servers:
Case reports
- 4 day old boy with bilateral scrotal masses (Asian J Surg 2023;46:2546)
- 18 month old boy with painless unilateral scrotal swelling and spontaneous regression (J Ultrasound 2021;24:81)
- 2 year old with persistent unilateral scrotal mass (Int J Surg Case Rep 2023;107:108374)
- 9 year old boy with multicystic unilateral testicular lesion and ipsilateral renal agenesis (Front Pediatr 2022;10:898038)
- 32 year old man with progressive bilateral painless scrotal swelling (Indian J Urol 2010;26:593)
- 64 year old man with unilateral painless testicular enlargement (Ann R Coll Surg Engl 2008;90:W1)
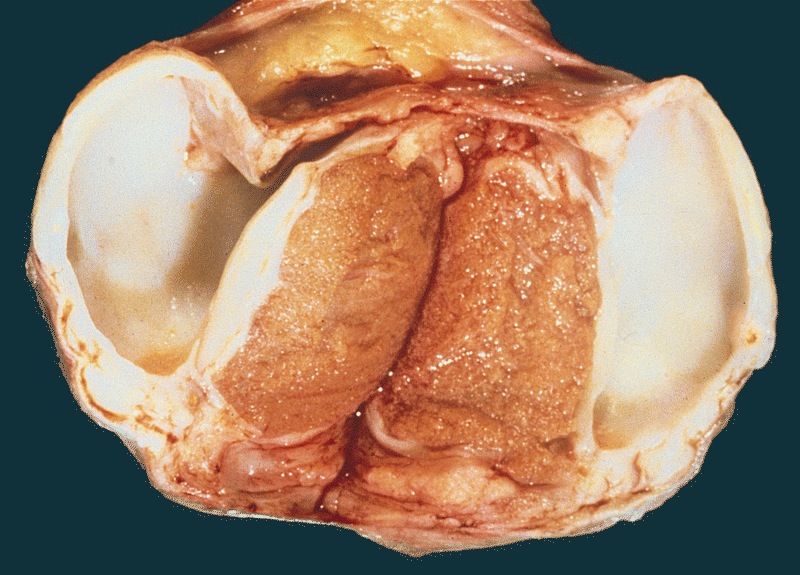
Gross description
- Hydrocele
- Fluid filled cyst caused by accumulation of clear serous fluid between the visceral and parietal tunica vaginalis
- Cyst fluid is generally clear but may be complicated by hemorrhage or infection
- May appear multiloculated in the setting of chronic inflammation and progressive fibrosis resulting in internal septa (J Ultrasound 2011;14:208)
- Mesothelial cyst
- Simple or multilocular cystic dilation within the tunica vaginalis or tunica albuginea
- Clear to bloody serous cyst fluid
- Epididymal cyst (spermatocele) and simple cyst of rete testis
- Epididymal cyst fluid contains abundant spermatozoa
- Epididymal cysts > 2 cm present clinically as spermatocele
- Rete testis cysts are typically unilocular and limited to hilum but may bulge into testis; a multilocular form is associated with epididymal cysts
Gross images
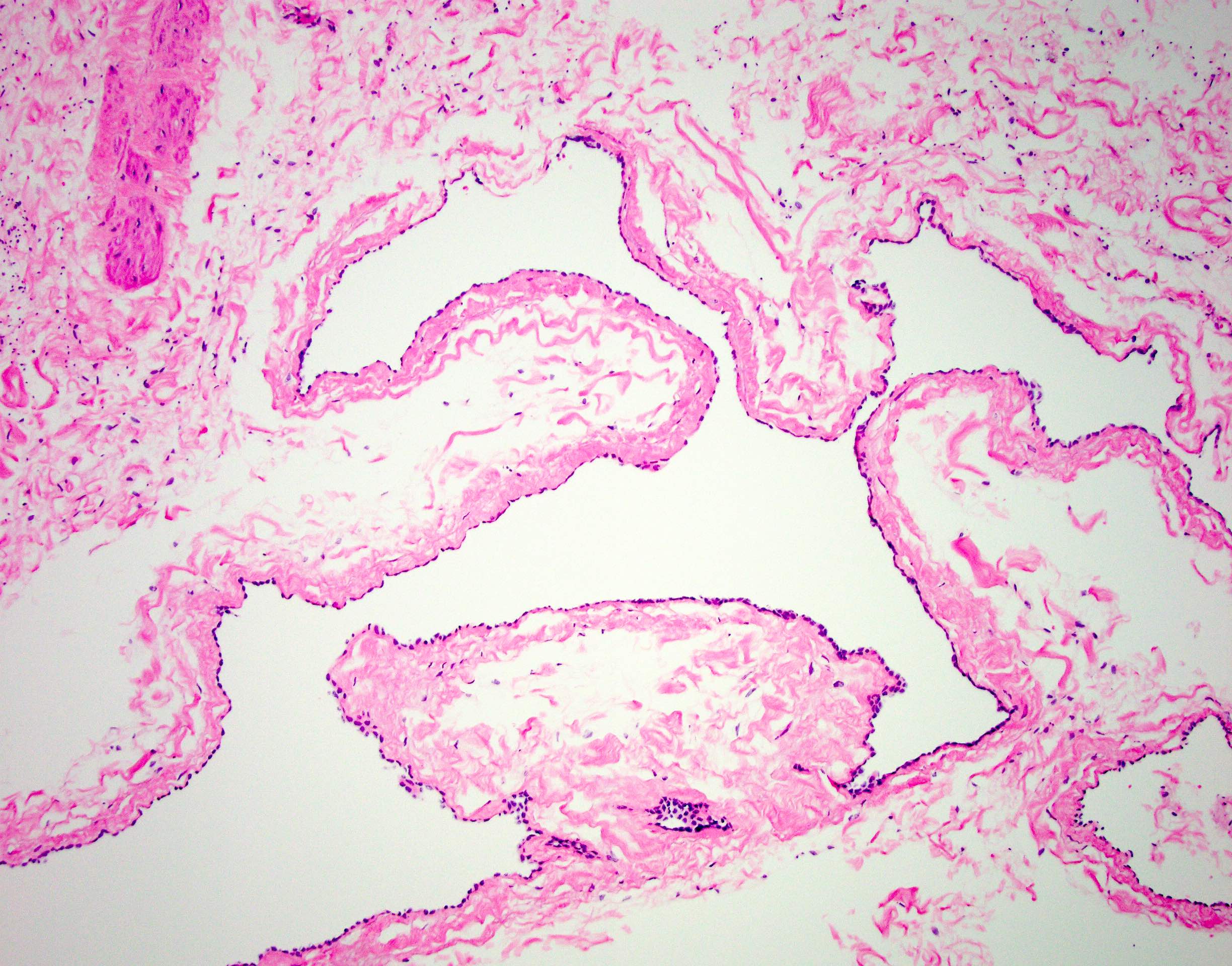
Microscopic (histologic) description
- Hydrocele and mesothelial cysts
- Single layer of cuboidal or flattened mesothelial cells
- Prominent atypia, squamous metaplasia or inflammation may be present (Mod Pathol 2005;18:S131)
- Cysts and cystic dilatation of epididymis and rete testis
- Simple cyst or multicystic distension of the rete testis or epididymis
- Single layer of normal tubal epithelium (cuboidal to flattened ciliated epithelial cells)
- Lumen filled with spermatozoa
- Chronic inflammation may be present
- May show columnar cell change, fibrosis, giant cell reaction
- Cystic dysplasia of rete testis
- Multicystic lesion located in the mediastinum testis
- Irregular cystic spaces lined by a single layer of cuboidal epithelium (Front Pediatr 2022;10:898038)
Microscopic (histologic) images
Sample pathology report
- Right testes:
- Mesothelium lined cyst (3.0 cm), consistent with hydrocele sac
- Spermatocele sac:
- Ciliated columnar / cuboidal cell lined cyst with aggregates of spermatozoa, consistent with spermatocele
Differential diagnosis
- Ovarian epithelial type tumors:
- Believed to arise from Müllerian duct remnants or secondary to Müllerian metaplasia of mesothelium
- Entire spectrum of serous or mucinous cystadenomas, borderline tumors and carcinomas can be seen, with serous borderline tumors most frequent (Diagn Pathol 2015;10:118)
- Histologically and immunophenotypically identical to ovarian counterparts
- Can be distinguished by their complex papillary structures and expression of PAX8, WT1, variable ER and PR, EMA and CA-125
- Cystadenoma of rete testis:
- Irregular proliferation of cystic structures lined by cytologically bland low cuboidal epithelium and separated by fibrous septa (AJR Am J Roentgenol 2007;189:W67)
- Can be distinguished grossly from rete testis cysts and cystic dilatation by admixed irregular cystic and solid areas and histologically by areas of complex growth (e.g., sertoliform cystadenoma), budding and tufting
- Papillary cystadenoma of epididymis:
- Associated with von Hippel-Lindau syndrome
- Dilated ducts lined by a single or double layer of cuboidal to low columnar epididymis epithelium, characterized by cilia and secretory droplets / variable cytoplasmic vacuolization; rarely, mucinous features may be present mimicking intestinal type goblet cells
- Can be distinguished from rete testis cysts and cystic dilatation by presence of papillae
- Teratoma, prepubertal type:
- Epidermoid cysts are unilocular and can be distinguished grossly and histologically by their simple stratified squamous epithelium lining (lacking skin appendages) and keratinaceous contents
- Dermoid cysts can be distinguished grossly and histologically by the complex structure frequently containing multiple somatic tissue elements (e.g., bone, hair)
- Cysts of appendix epididymis and appendix testis:
- These 2 embryonic remnants may become enlarged and cystically dilated by serous fluid, thus mimicking other testicular cysts (Surg Radiol Anat 2005;27:557)
Practice question #1
Practice answer #1
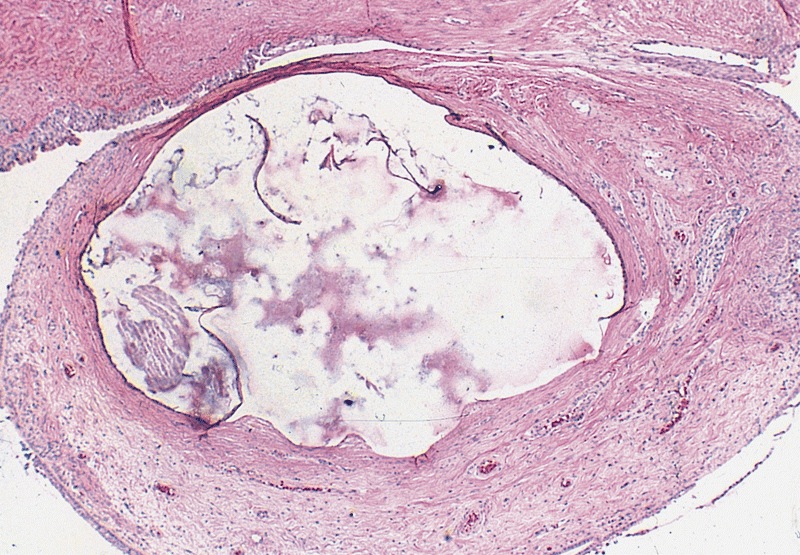
A. Cystic dilation of epididymis. The image shows a cystically dilated epididymis with proteinaceous luminal accumulation in a cystic space lined by tubal epithelium. Answer E is incorrect because the structure is consistent with normal histology in this location rather than teratomatous elements and teratoma would be less common in an elderly patient with a history of hormonal abnormality (i.e., cirrhosis). Answers C and B are incorrect because a mesothelial cyst or hydrocele would be lined by mesothelium. Answer D is incorrect because while spermatocele is also an epididymal structure lined by tubal epithelium, there is no evidence of spermatozoa in this image.
Comment Here
Reference: Cysts
Comment Here
Reference: Cysts
Practice question #2
Which of the following clinical scenarios is most likely to be associated with cystic dysplasia of the rete testis?
- 4 day old neonate with persistent bilateral scrotal swelling
- 5 year old boy with a complex solid and cystic scrotal mass
- 6 year old boy with right renal agenesis and unilateral scrotal swelling
- 34 year old man with 2 months of painful unilateral scrotal mass and recent diagnosis of tuberculosis
- 67 year old man with metastatic castration resistant prostatic adenocarcinoma
Practice answer #2
C. 6 year old boy with right renal agenesis and unilateral scrotal swelling. Cystic dysplasia of the rete testis is most commonly seen in children (median age is 5 years old) and is frequently associated with ipsilateral urogenital malformations, such as renal agenesis. Answer A is incorrect because by contrast, unilateral or bilateral neonatal scrotal swelling is most commonly due to persistent patency of the processus vaginalis with spontaneous resolution by 1 - 2 years of age. Answers E and D are incorrect because scrotal swelling in adults is more frequently due to cysts or cystic dilatation of the epididymis or rete testis secondary to obstruction in the setting of hormonal changes, neoplastic processes, surgery or infection. Answer B is incorrect because the presence of a complex scrotal mass rather than uniloculated or multiloculated fluid filled mass raises the possibility of prepubertal teratoma.
Comment Here
Reference: Cysts
Comment Here
Reference: Cysts