Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Musick A, Kim A, Glass C. Acute cellular rejection. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/heartacutecellularrejection.html. Accessed May 14th, 2024.
Definition / general
- Lymphocyte predominant infiltration of the perivascular and interstitial myocardial compartments after orthotopic heart transplantation resulting in myocyte damage and necrosis, distorted myocardial architecture and allograft dysfunction
Essential features
- Early complication after heart transplantation (first 3 - 6 months)
- Endomyocardial biopsy is diagnostic
- Host T cell mediated inflammatory response to allograft differences in histocompatibility antigens, precipitating myocyte damage and myocardial dysfunction
Terminology
- Acute allograft rejection
ICD coding
Epidemiology
- Early complication after orthotopic heart transplant causing less than 10% of 1 year mortality and 9% of 3 year mortality (Transl Res 2012;159:238)
- Highest incidence within first 3 years after transplant, most frequently within first 3 - 6 months (Cagle: Atlas Of Transplant Pathology, 2015)
- Up to 60% experience at least one episode within the first 6 postoperative months
- Increased incidence / risk:
- Donor factors: female, < 18 years old, longer ischemic time (Circulation 1992;86:II236)
- Recipient factors: female, black, younger age, cytomegalovirus infection, higher levels of circulating donor specific antibodies to human leukocyte antigen before transplantation, greater number of previous rejection episodes (JAMA 1989;261:3561, Ann Thorac Surg 2007;84:1556)
- Greater number of donor recipient human leukocyte antigen mismatches or sex mismatched transplantation (Transpl Int 2014;27:482)
- Decreased risk if the transplant was received in the last 15 years
Sites
- Inflammatory infiltrate associated with interstitial and/or perivascular compartments of allograft myocardium
- Severe cases may involve transmural inflammation of distal coronary arteries (Cagle: Atlas Of Transplant Pathology, 2015)
Pathophysiology
- Host allorecognition of donor major and minor histocompatibility antigens on the allograft → T cell activation → myocardial infiltration of host T cells and macrophages → myocyte damage and necrosis (Transl Res 2012;159:238)
- More severe episodes associated with polymorphonuclear leukocyte infiltration, B cell presence and greater numbers of macrophages and dendritic cells (Cagle: Atlas Of Transplant Pathology, 2015)
- CD4 T cells more abundant in mild / early rejection and CD8 T cells in moderate rejection (Arch Pathol Lab Med 2007;131:1169)
- Ratio of memory (CD45RO+) to naive (CD45RA+) T cells is higher in moderate rejection than in mild rejection
- Rejection mediated by IL-2, TNF beta and IFN gamma (Ludhwani: StatPearls, 2019)
Etiology
- Interplay between immunologic (cellular mediated rejection and human leukocyte antigen matching) and nonimmunologic (e.g., recipient cytomegalovirus infection, pediatric donor) factors
Diagrams / tables
Clinical features
- Presents with dyspnea orthopnea, paroxysmal nocturnal dyspnea, syncope, palpitations and arrhythmias (notably atrial flutter), nausea and weight gain
- Gastrointestinal symptoms due to secondary hepatic congestion can confuse the clinical picture and lead to delays in diagnosis (UpToDate: Acute Cardiac Allograft Rejection - Diagnosis [Accessed 7 October 2019])
- If severe, may present with cardiogenic shock (Cagle: Atlas Of Transplant Pathology, 2015)
- Signs: jugular vein distention, extra heart sounds, peripheral edema, hypotension and oliguria (Ludhwani: StatPearls, 2019)
Diagnosis
- Surveillance endomyocardial biopsies (J Heart Lung Transplant 2005;24:1710)
- In biopsy negative rejection (20%), utilize troponin, Doppler echocardiography, cardiovascular MRI, antimyosin scintigraphy, annexin V imaging or gene expression profiling (Ludhwani: StatPearls, 2019)
- Can screen for but not diagnose rejection via noninvasive methodologies: Doppler echocardiography, cardiovascular MRI and gene expression profiling (Transl Res 2012;159:238)
- Cannot be used as a diagnostic tool due to insufficient sensitivity and specificity
- Gene expression profiling of peripheral blood mononuclear cells distinguished moderate severe rejection from quiescence (Am J Transplant 2006;6:150)
Radiology description
- Doppler echocardiography: decreased isovolumic relaxation time, decreased pressure half time and disturbed early diastolic wall motion velocity (J Am Coll Cardiol 1988;12:63, Circulation 2001;104:I184)
- Cardiovascular MRI: long T2 relaxation times due to myocardial edema (J Cardiovasc Magn Reson 2009;11:7, J Am Coll Cardiol 2001;37:825)
Radiology images
Prognostic factors
- Favorable:
- Use of tacrolimus based immunosuppression versus cyclosporine (Am J Transplant 2006;6:1377)
- Unfavorable:
- Sex mismatched transplantation (Clin Transplant 2017;31)
- Occurrence within the first postoperative year
- Greater numbers of rejection episodes or higher grades of rejection severity (Best Pract Res Clin Anaesthesiol 2017;31:201)
- Higher numbers of CD8 T cells on endomyocardial biopsy (J Heart Lung Transplant 1991;10:235)
- Quilty positive biopsies (Transpl Immunol 2008;19:209)
- Use of extracorporeal membrane oxygenation support before transplantation (Ludhwani: StatPearls, 2019)
Case reports
- 24 year old woman with fatal mixed humoral and cellular rejection not detected on surveillance biopsies or circulating antibodies (J Transplant 2011;2011:351950)
- 43 year old man with asymptomatic acute cellular rejection demonstrated on cardiovascular MRI (Ann Transplant 2014;19:447)
- 53 year old woman with fulminant mixed humoral and cellular rejection presenting with coronary pan-ischemia (Int Heart J 2015;56:679)
- 60 year old woman with recurrent asymptomatic acute cellular rejection monitored with speckle tracing echocardiography (Pol Arch Med Wewn 2016;126:700)
- 74 year old man with mixed humoral and cellular rejection presenting with sinus tachycardia segment elevation in leads I and aVL (Circ Heart Fail 2015;8:836)
Treatment
- Preventative therapy: posttransplantation immunosuppressants
- Treat with oral / intravenous steroids, antithymocyte globulin and Murine monoclonal antibodies OKT3 based on patient hemodynamic status and histological severity of disease (Ludhwani: StatPearls, 2019)
- First line: high-dose IV corticosteroids (J Heart Lung Transplant 2010;29:914)
- Grades ≥ 2R are considered clinically relevant and are treated even if asymptomatic (Cagle: Atlas Of Transplant Pathology, 2015)
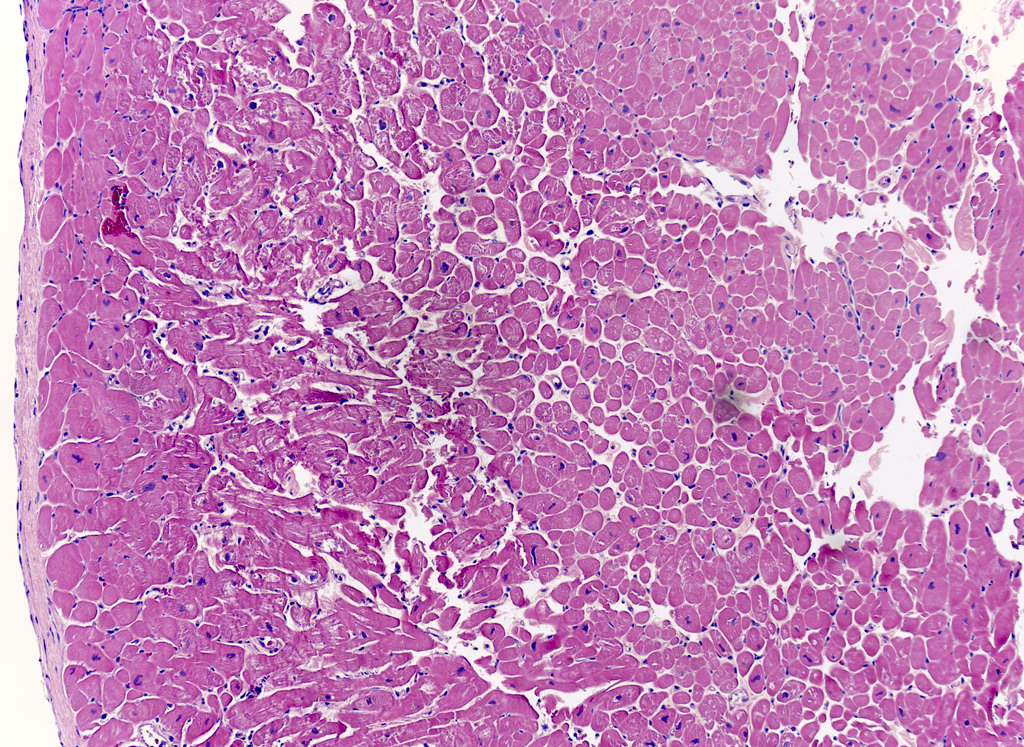
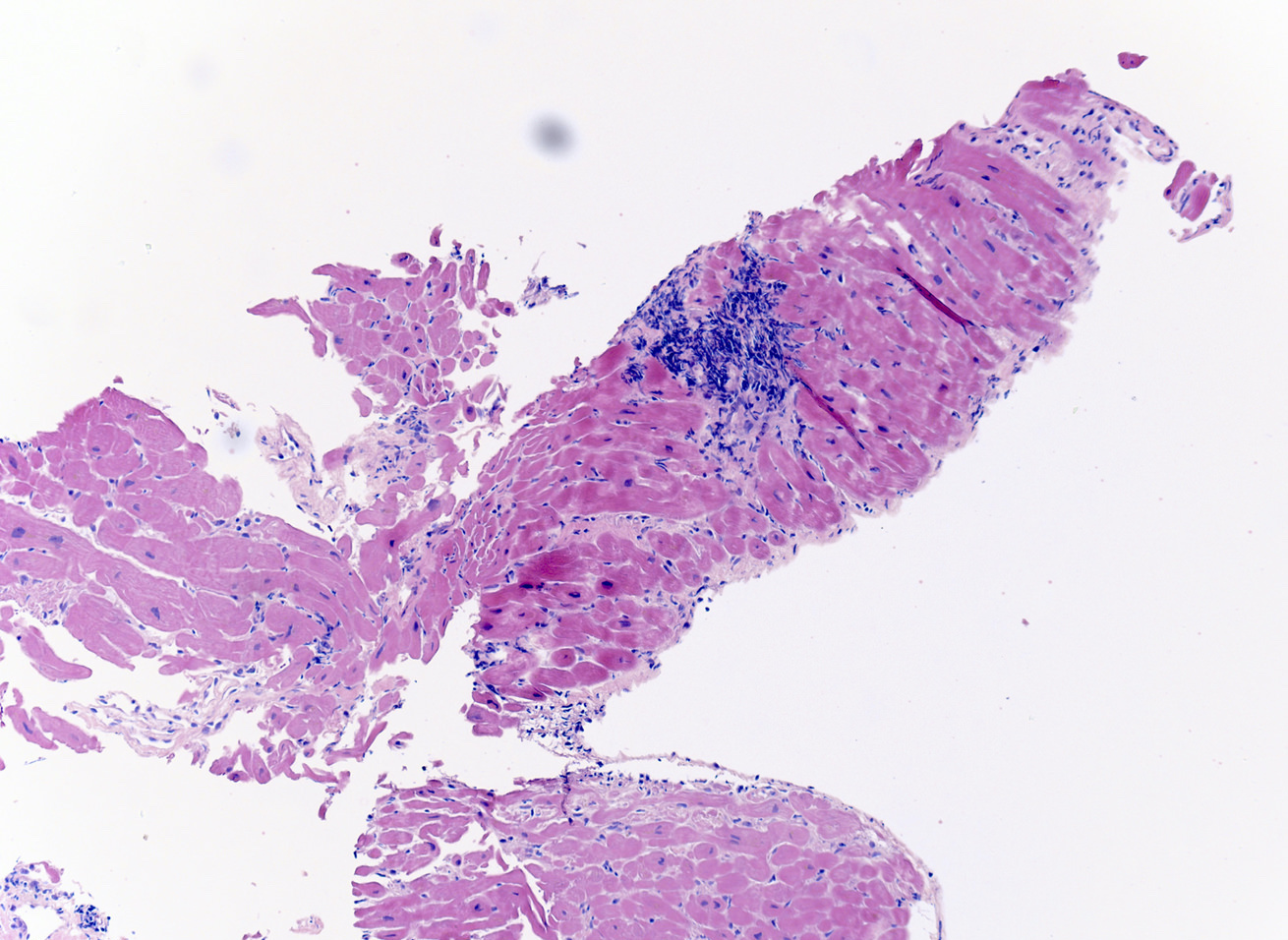
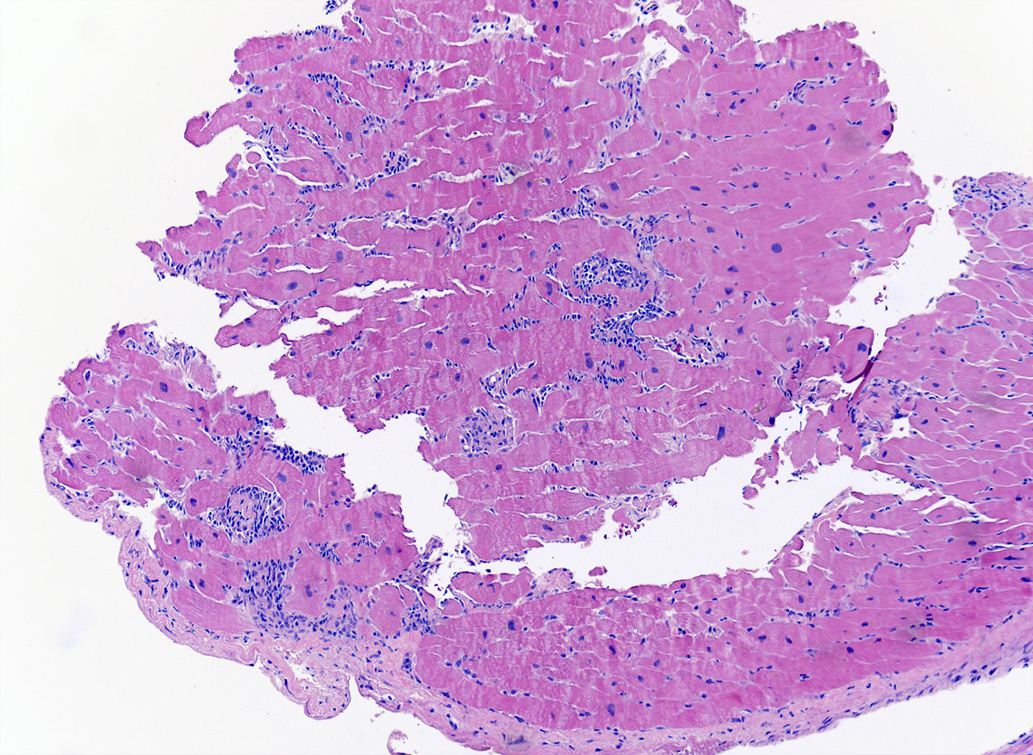
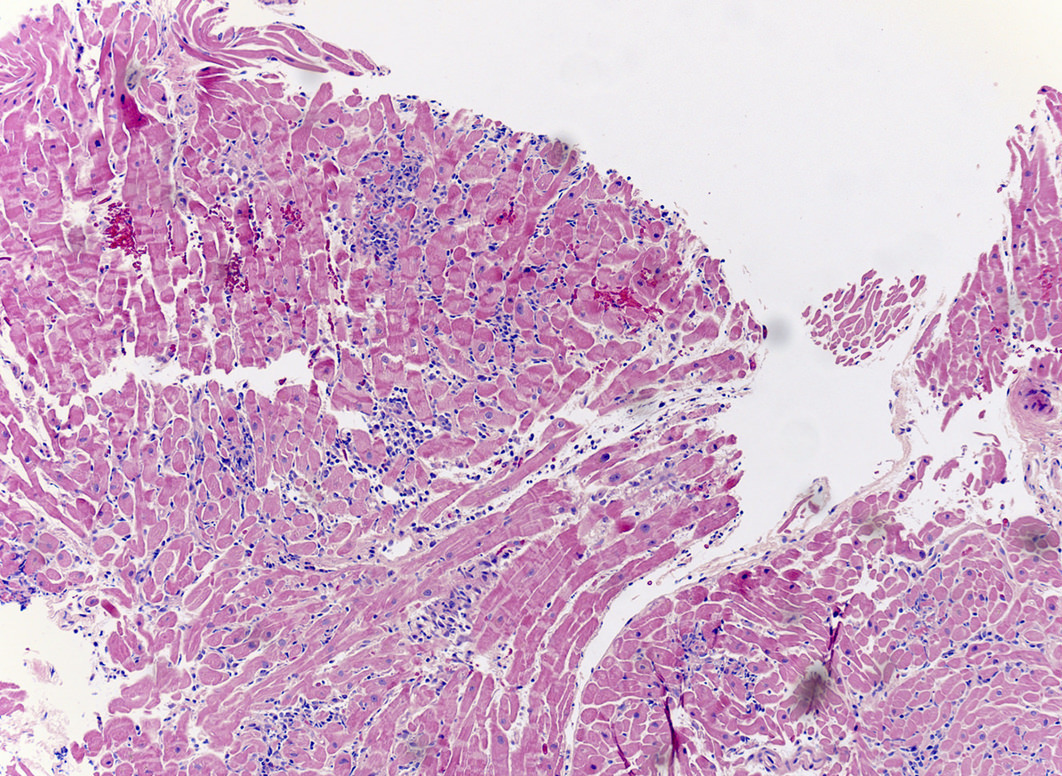
Microscopic (histologic) description
- International Society for Heart and Lung Transplantation (ISHLT) 2004 standardized endomyocardial biopsy grading (J Heart Lung Transplant 2005;24:1710):
- Grade 0R (no rejection): no evidence of cellular infiltration or myocyte damage
- Grade 1R (mild): interstitial or perivascular infiltrate with or without 1 focus of myocyte damage
- Grade 2R (moderate): ≥ 2 foci of infiltrate with associated myocyte damage
- Grade 3R (severe): diffuse infiltrate with multifocal myocyte damage variable edema, vasculitis and interstitial hemorrhage
- Inflammatory infiltrate: lymphocytes variable macrophages and eosinophils
- Neutrophils generally absent except in severe cases
- Presence of plasma cells suggests an alternative etiology
- Inflammatory infiltrate is usually proportionally greater than the degree of myocyte damage
- Myocyte damage and encroachment of inflammatory cells (→ irregular myocyte borders and distorted myocardial architecture)
- Mild: myocytolysis (sarcoplasmic / nuclear clearing, nuclear enlargement, prominent nucleoli)
- Severe: contraction band or coagulation necrosis
Microscopic (histologic) images
Virtual slides
Positive stains
- CD3, CD4 and CD8 positive T lymphocytes within inflammatory infiltrate
- Increased intercellular adhesion molecules with high MHC class II expression on cardiac myocytes (Ludhwani: StatPearls, 2019)
Negative stains
- Lack of C4d deposition on capillary endothelium on stain or immunofluorescence (presence is typical of antibody mediated rejection)
- Can have mixed humoral and cellular acute rejection, so should assess endomyocardial biopsies for both (Arch Pathol Lab Med 2016;140:910)
Sample pathology report
- Heart, endomyocardial biopsy:
- Multifocal moderate acute cellular allograft rejection with associated multifocal myocyte necrosis (ISHLT Grade 2R; 1990 Grade 3A)
- pAMR 0: No significant evidence of antibody mediated rejection on immunohistology.
- Quilty effect: Moderate focal endocardial inflammatory cell aggregate with myocardial encroachment.
Differential diagnosis
- Ischemic injury (e.g., perioperative ischemia or allograft coronary disease)
- Infiltrate is predominantly neutrophils and macrophages rather than lymphocytes (Arch Pathol Lab Med 2007;131:1169)
- If perioperative: proportionally greater myocyte damage than inflammatory infiltrate
- If allograft coronary disease: secondary myocardial changes (myocyte vacuolization or microinfarcts)
- Acute antibody mediated rejection: positive immunofluorescence for immunoglobulins, complement and CD68 staining for macrophages (J Heart Lung Transplant 2005;24:1710)
- Quilty lesions: extends to endocardium and may involve B lymphocytes (Ludhwani: StatPearls, 2019)
- Infection (e.g. cytomegalovirus, myocarditis, toxoplasmosis, disseminated aspergillosis): demonstration of infectious entity on endomyocardial biopsy
- Sarcoidosis: noncaseating granulomas (Chest 1986;90:528)
- Giant cell myocarditis: inflammatory cell infiltrate with multinucleated giant cells (CD68+), nonnecrotizing granulomas and eosinophils (Arch Pathol Lab Med 2016;140:1429)
- Prior biopsy site: biopsy will feature a lesion in several stages of healing, including thrombus, granulation tissue and perimyocytic fibrosis
- Cardiac allograft vasculopathy: presence of angiographic evidence supporting cardiac allograft vasculopathy (Croat Med J 2014;55:562)
- Posttransplant lymphoproliferative disease: EBV seroconversion or reactivation of anti-EBV IgM with constitutional symptoms (J Cardiovasc Pharmacol Ther 2006;11:77)
Board review style question #1
A 42 year old black man underwent an orthotopic heart transplantation 4 months ago following viral myocarditis induced dilated cardiomyopathy in which he received a heart from a 19 year old Hispanic male. A routine posttransplant surveillance endomyocardial biopsy demonstrated mild interstitial inflammatory cell infiltrate with one small focus of myocyte damage. There was no evidence of myocyte necrosis. At that time, the patient was completely asymptomatic and reported no history of complications from his heart transplant. Which of the following is a significant risk factor in the development of this patient's disease?
- Donor Hispanic race
- Donor young age
- Recipient black race
- Sex matched transplantation
Board review style answer #1
C. Recipient black race. This patient has acute cellular rejection following his orthotopic heart transplantation. Given the brief histological description of his endomyocardial biopsy, this patient has an International Society for Heart and Lung Transplantation acute cellular rejection grade of 1R. Acute cellular rejection has a peak incidence 3 - 6 months after transplantation, which aligns with this patient's current presentation. Recipient black race is associated with an increased risk / incidence of acute cellular rejection. A sex mismatched transplantation, recipient (or donor) female sex and a pediatric donor would also increase the risk / incidence of acute cellular rejection, not the inverse as presented in the answer choices for this case. Donor race has not been demonstrated to have an impact on the risk or incidence of acute cellular rejection.
Comment Here
Reference: Acute cellular rejection
Comment Here
Reference: Acute cellular rejection
Board review style question #2
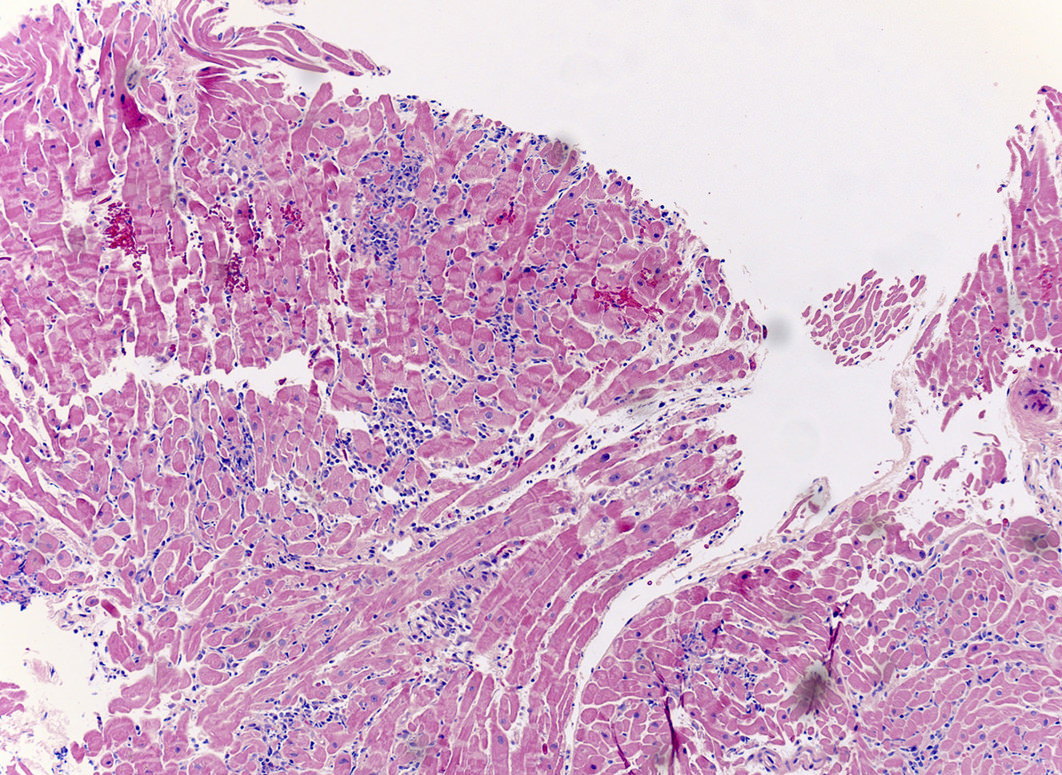
A 20 year old man received an orthotopic heart transplant 3 months ago for restrictive cardiomyopathy. He attended his first followup visit but was unable to return to clinic for any subsequent appointments. He presented urgently today with concerns that, for the last few weeks, he has been experiencing progressive exertional dyspnea and intermittent palpitations. He also reports that he needed to use 4 to 5 pillows last night to sleep, as he felt as if he couldn't breathe well while lying flat. These symptoms have never happened before. His physician obtained an endomyocardial biopsy and a representative section (H&E) is shown above. Which of the following statements about this disease is true?
- Condition is mediated by B cells, which extend into the endocardium
- High dose IV corticosteroids are the first line therapy for this condition
- Invasive coronary angiography with assessment of cardiac allograft function is required to make the diagnosis
- Myocardial inflammatory infiltrate is predominantly composed of neutrophils
- Positive immunofluorescence for endothelial C4d is characteristic of the disease
Board review style answer #2
B. High dose IV corticosteroids are the first line therapy for this condition. This patient has an International Society for Heart and Lung Transplantation grade 3R acute cellular rejection following his orthotopic heart transplantation. The endomyocardial biopsy demonstrates a diffuse inflammatory infiltrate with multifocal myocyte damage, myocardial edema and interstitial hemorrhage, consistent with an International Society for Heart and Lung Transplantation grade of 3R. In acute cellular rejection, the first line therapy is high-dose IV corticosteroids. Positive immunofluorescence for C4d is characteristic of acute humoral rejection, not acute cellular rejection. Coronary angiography is used to diagnose cardiac allograft vasculopathy; in acute cellular rejection, endomyocardial biopsy is the gold standard for diagnosis. The inflammatory infiltrate in acute cellular rejection is T lymphocyte predominant and occurs primarily within the myocardium. A neutrophilic infiltrate is associated with ischemic injury while a B lymphocyte mediated process in the endocardium is consistent with a quilty lesion.
Comment Here
Reference: Acute cellular rejection
Comment Here
Reference: Acute cellular rejection