Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Castillo VF, Saleeb R. Papillary adenoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneytumorrenalcortadenoma.html. Accessed May 18th, 2024.
Definition / general
- Benign unencapsulated renal epithelial neoplasm characterized by papillary, tubular or tubulopapillary architecture with low grade nuclei and a diameter of ≤ 15 mm
Essential features
- Benign papillary or tubulopapillary, low nuclear grade lesions of the kidney, similar in morphology to classic papillary renal cell carcinoma (PRCC); however, they lack fibrous capsules and are ≤ 15 mm
- Prevalent in damaged and injured kidneys
- Could be related to a progenitor / stem cell-like renal tubular cell population that increases upon kidney damage
- Postulated to be precursor lesions to PRCC
- However, the prevalence of adenoma is much higher than of carcinoma, indicating that many of them do not progress
Terminology
- Tubulopapillary adenoma
- Renal adenoma (not recommended)
ICD coding
- ICD-O: 8260/0 - papillary adenoma, NOS
- ICD-11: 2F35 & XH09B0 - benign neoplasm of urinary organs & papillary adenoma, NOS
Epidemiology
- ~20% in autopsy kidneys; 7% in nephrectomy specimens (Am J Surg Pathol 2019;43:277, Hum Pathol 2007;38:239)
- Incidence increases with age
- 8% (20 - 40 years old) versus 25% (> 40 years old) versus 40% in 70 - 90 year olds (Am J Surg Pathol 2019;43:277, Semin Diagn Pathol 1998;15:41)
- M:F = 4.6 - 5:1 (Am J Surg Pathol 2019;43:277, Kidney Int 2002;61:2201)
- More frequent in resected kidneys with PRCC compared with other subtypes (Hum Pathol 2007;38:239)
- More common in those with end stage renal disease, acquired cystic disease, glomerulosclerosis, prolonged hemodialysis and a history of smoking (Am J Surg Pathol 2019;43:277, Kidney Int 2002;61:2201)
Sites
- Renal cortex
Pathophysiology
- Studies hypothesize that the origin is renal tubular progenitor / stem cells (Am J Pathol 2011;178:828)
- Renal tubular progenitor / stem cells proliferate upon renal injury or damage (Int Urol Nephrol 2014;46:2127)
- These cells give rise to papillary adenoma, which in turn could be a precursor to PRCC (Hum Pathol 2007;38:239, Mod Pathol 2003;16:1053)
Etiology
- Unknown, possibly secondary to renal injury as chronic medical renal diseases, pyelonephritis or nearby mass tumor effect (Am J Pathol 2019;189:2046)
Clinical features
- Asymptomatic; incidentally found in nephrectomies removed for larger tumors or other causes
- Common in end stage kidneys (Virchows Arch 2008;453:313, Transplant Proc 2008;40:3354, Int Urol Nephrol 2014;46:2127)
Diagnosis
- Imaging: usually computed tomography (CT) scan, ≤ 15 mm, often not seen
- Biopsy or resection
- Diagnosis on needle biopsy should be made with caution as capsule and nuclear grade heterogeneity may not be visualized
Radiology description
- CT / magnetic resonance imaging (MRI): ≤ 15 mm in size
- No specific imaging findings; may be difficult to distinguish from other renal lesions
Prognostic factors
- Benign lesions thought to be precursors of PRCC (Hum Pathol 2007;38:239, Mod Pathol 2003;16:1053)
- However, the incidence of PRCC is much lower than papillary adenoma, indicating that not all cases have the potential to progress to PRCC (Am J Pathol 2019;189:2046)
- Size criterion has been changed from 5 mm to 15 mm based on data that these lesions have no capacity to metastasize (Eur Urol 2011;60:983)
- Change allows for increased acceptance of donor kidneys for transplantation, in which kidneys with papillary lesions ≤ 15 mm would not be rejected (Ann Transplant 2014:19:362)
Case reports
- 34 year old man with autosomal dominant polycystic kidney disease and renal papillary adenomas with unusual clinical presentation (Iran J Kidney Dis 2013;7:439)
- 47 year old man with incidentally detected renal adenomatosis in hydronephrotic kidney (Turk J Urol 2013;39:56)
- 62 year old woman with renal adenomatosis with 10 year imaging follow up (J Med Case Rep 2022;16:168)
Treatment
- Treatment is based on the presenting tumor or condition
- Considered benign; does not on its own require treatment
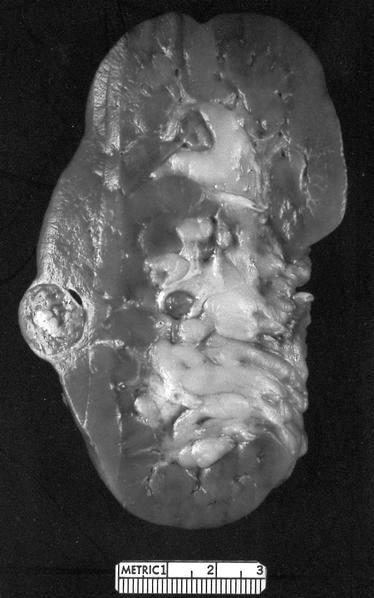
Gross description
- Usually subcapsular
- Spherical or wedge shaped, grayish white to yellow (Am J Surg Pathol 2019;43:277)
- Smaller lesions may not be visible
- May be multiple (renal adenomatosis)
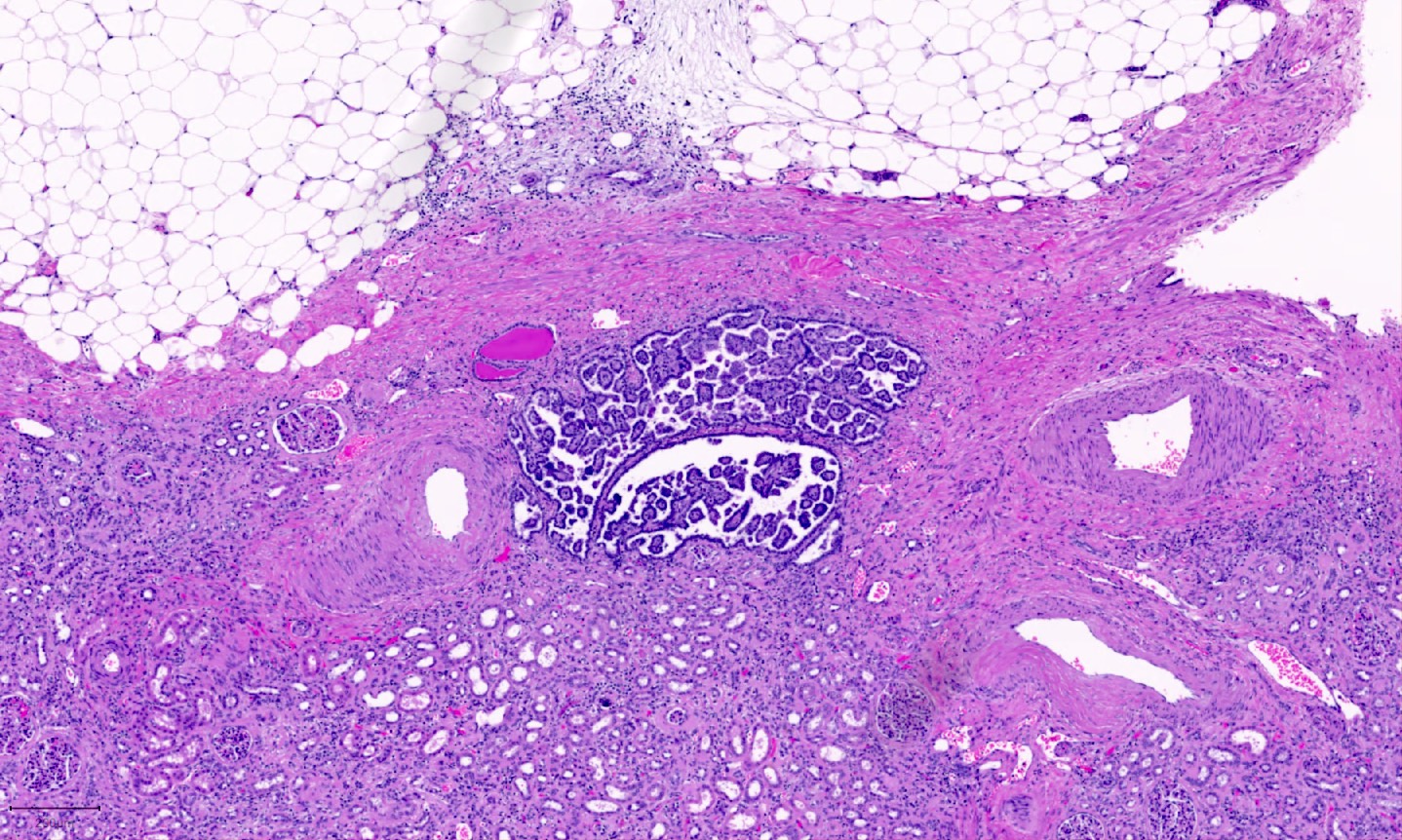
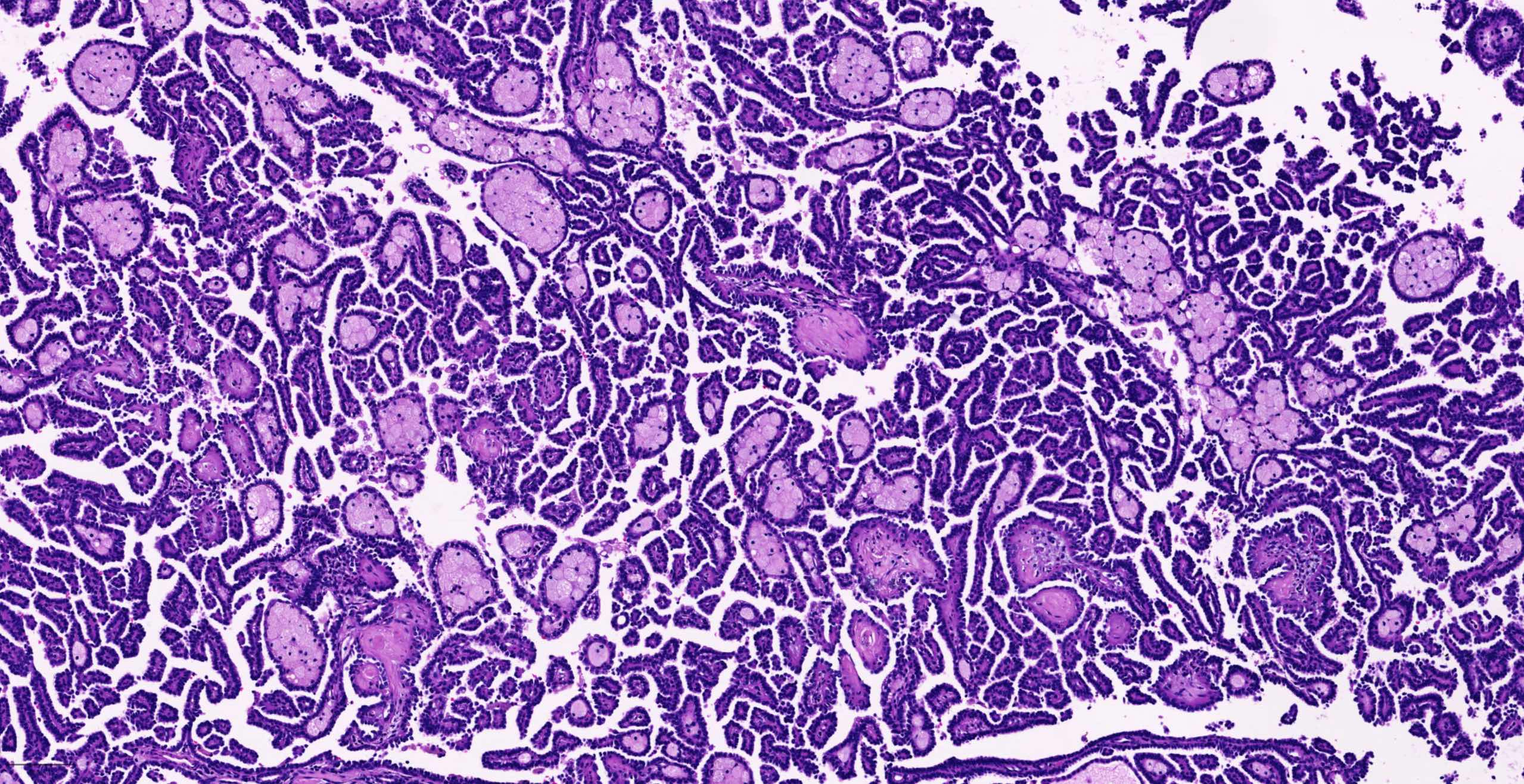
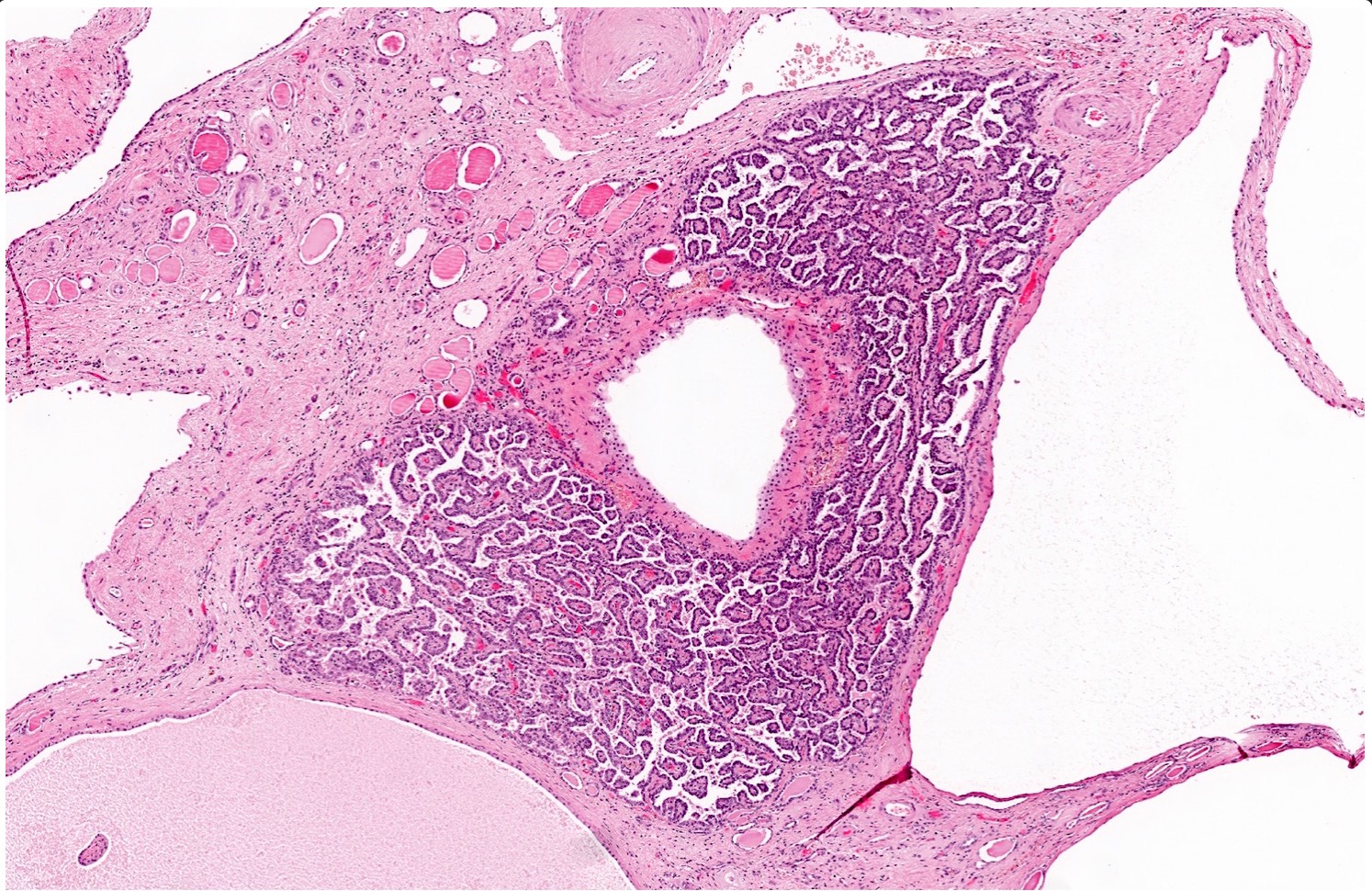
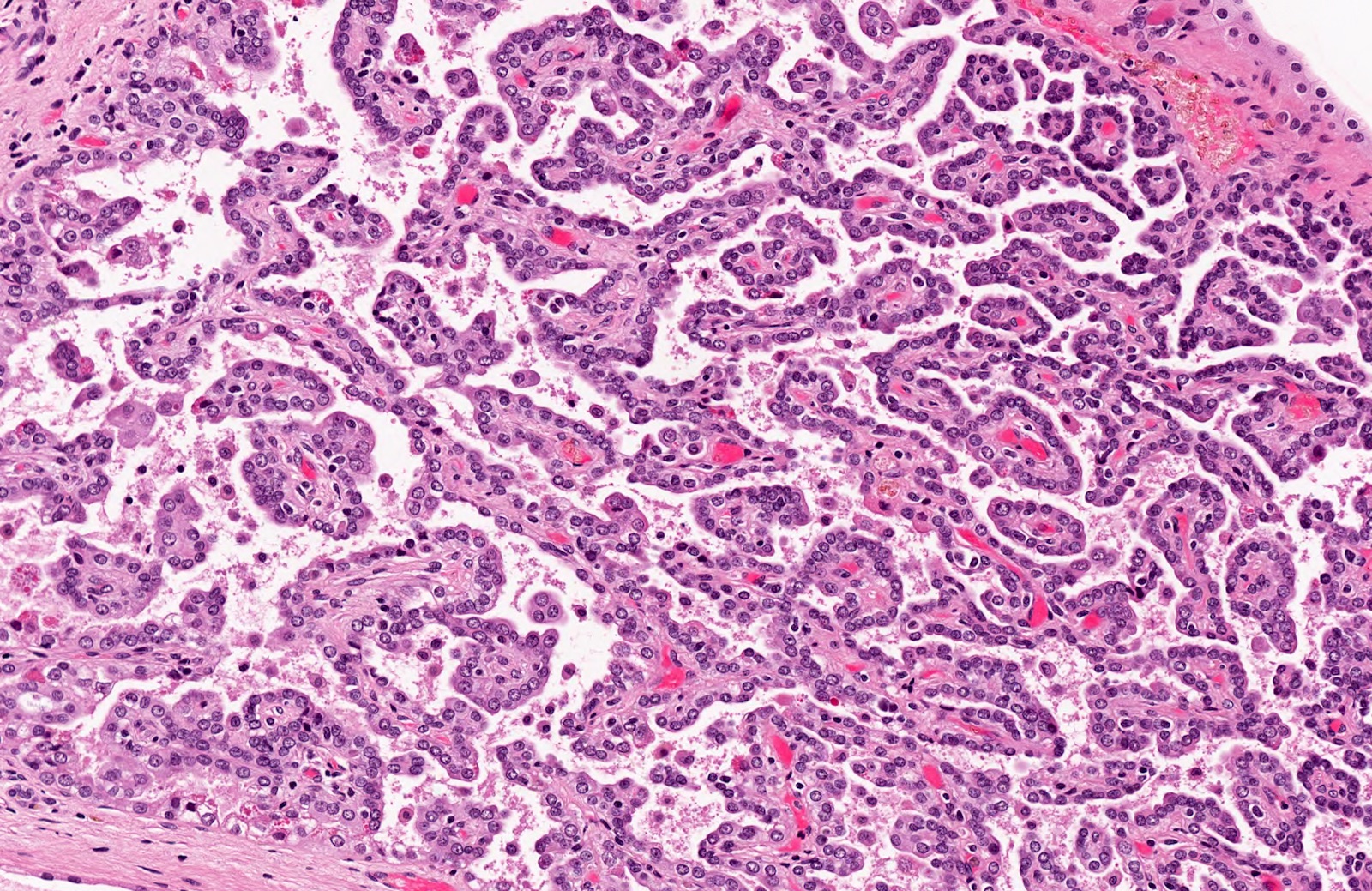
Microscopic (histologic) description
- Papillary, tubular or tubulopapillary architecture
- No fibrous capsule; in direct contact to adjacent renal parenchyma
- Lined by cuboidal cells with scant, pale cytoplasm with low nuclear grade (WHO / International Society of Urological Pathology [ISUP] grade 1 - 2) (similar to classic pattern of PRCC)
- Papillary adenomas are benign lesions and are not graded
- Tumors with high grade nuclei should not be diagnosed as papillary adenoma
- Some lesions show cytoplasmic clearing with fine granularity similar to what is occasionally seen in PRCC
- Lesions diagnostic of clear cell papillary renal cell tumor should not be considered as papillary adenoma
- Absent to rare mitosis
- Foamy macrophages and psammomatous calcifications may be present (Am J Surg Pathol 2019;43:277)
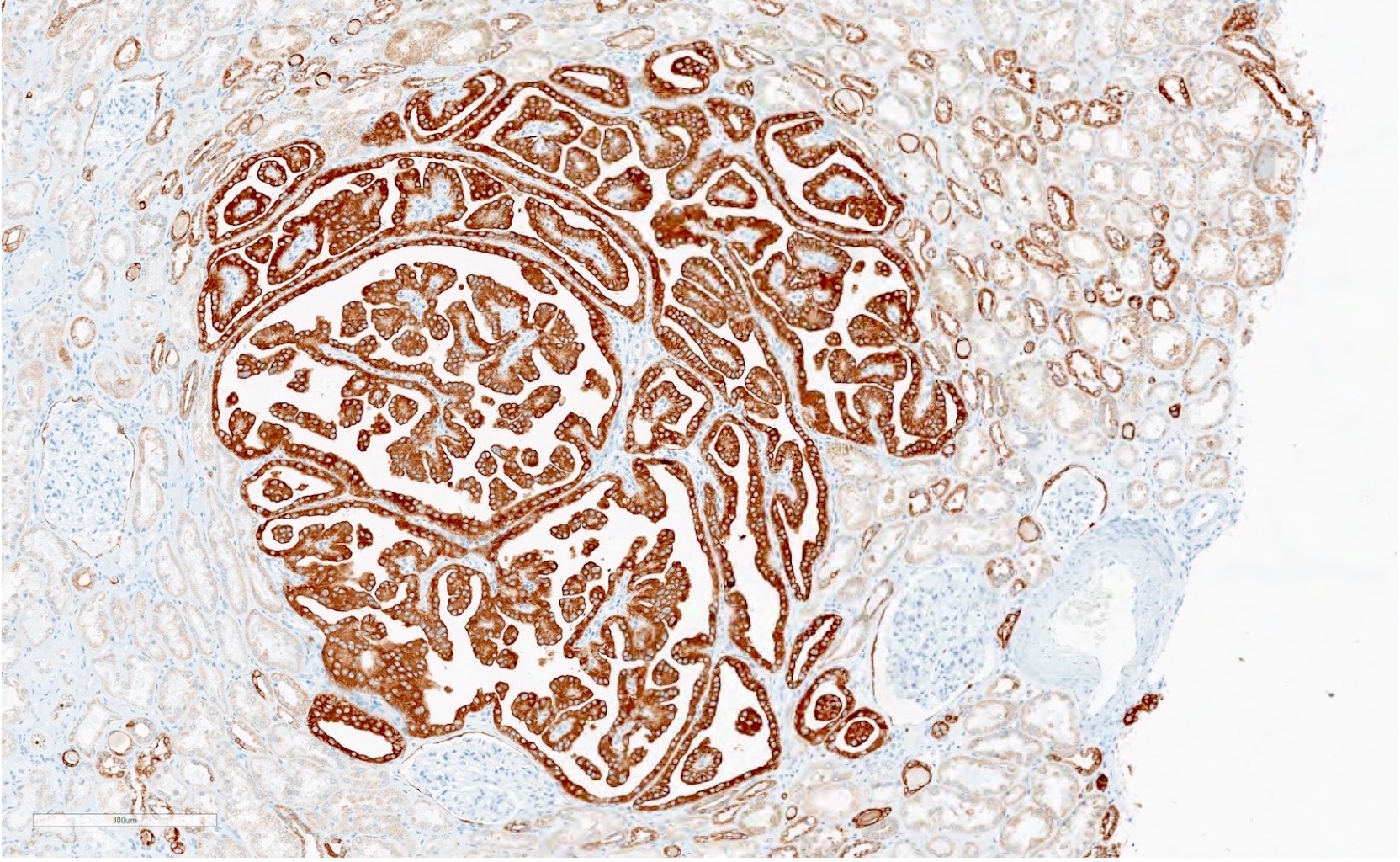
Microscopic (histologic) images
Cytology description
- Cellular, bland cells in tubules spherules and papillae, minimal cytologic atypia (identical to low grade PRCC) (Cancer Cytopathol 2022;130:927)
Positive stains
- CK7, AMACR, vimentin (similar to PRCC) (Hum Pathol 2007;38:239)
Negative stains
- CAIX (positive in CCPRCT)
- GATA3, L1-CAM (positive in papillary renal neoplasm with reversed polarity) (Am J Surg Pathol 2019;43:1099)
- WT1, CD57, BRAF V600E (positive in metanephric adenoma) (Mod Pathol 2015;28:1236)
Molecular / cytogenetics description
- Trisomy 7 and 17 and loss of Y chromosome; may have gains of chromosomes 12, 16 and 20
- Chromosomal profile is similar to classic PRCC and end stage kidney disease (Hum Pathol 2007;38:239, Mod Pathol 2003;16:1053, Virchows Arch 2008;453:313, Am J Pathol 2019;189:2046)
- KMT2C mutation
- Could be an early molecular event in papillary adenoma (Am J Pathol 2019;189:2046)
Sample pathology report
- Kidney, left, partial nephrectomy:
- Papillary adenoma, 1.2 cm
- Kidney, right, needle core biopsy:
- Low grade papillary renal lesion (see comment)
- Comment: The differential diagnosis includes papillary adenoma and papillary renal cell carcinoma. The clinical history is noted regarding the 0.6 cm size of the lesion. Clinical correlation is advised as to the size of the lesion by imaging. A lesion ≤ 1.5 cm would be consistent with a papillary adenoma, while a lesion > 1.5 cm would be classified as a papillary renal cell carcinoma.
Differential diagnosis
- Papillary renal cell carcinoma (PRCC):
- Size > 15 mm
- Capsule is present or with high grade morphology
- See differential diagnosis of low grade PRCC
- Papillary renal neoplasm with reversed polarity (PRNRP):
- Papillary architecture lined by cells with abundant and eosinophilic cytoplasm and apically located linearly arranged nuclei (Am J Surg Pathol 2019;43:1099)
- WHO / ISUP grade 1 - 2 (key feature)
- Positive for GATA3 nuclear staining (key feature), weak / negative AMACR and vimentin (Am J Surg Pathol 2019;43:1099)
- GATA3 positive in papillary renal neoplasm with reversed polarity (Am J Surg Pathol 2019;43:1099)
- Commonly harbor KRAS mutations (Mod Pathol 2020;33:1157, Mod Pathol 2020;33:690)
- Older terminologies: oncocytic low grade PRCC or type 4 PRCC (Am J Surg Pathol 2017;41:1618)
- Often smaller in size than classic PRCCs (most cases reported were pT1a disease)
- Indolent entity, no cases with disease progression reported to date (Front Oncol 2023;13:1101268)
- Important to recognize from eosinophilic PRCC, which is often a high grade lesion (Lab Investig 2023;103:S697)
- Clear cell papillary renal cell tumor (CCPRCT) (Mod Pathol 2013;26:697):
- Metanephric adenoma (MA) (Mod Pathol 2015;28:1236):
- Primitive blue cells forming small, crowded acini; WT1 and CD57 positive in MA while negative in PRCC
- Positive for BRAF V600E mutation
Additional references
Board review style question #1
A 38 year old woman with recurrent pyelonephritis was found to have a 1 cm left renal mass on imaging. A biopsy of the lesion was performed and showed the morphology above. Which of the following is the correct diagnosis and WHO / ISUP grade?
- Papillary adenoma, not graded
- Papillary adenoma WHO / ISUP grade 2
- Papillary renal cell carcinoma WHO / ISUP grade 1
- Papillary renal cell carcinoma WHO / ISUP grade 2
Board review style answer #1
A. Papillary adenoma, not graded. Papillary adenomas are low grade lesions by morphology; however, they are considered benign and are not graded as per the current guidelines. Answer B is incorrect because grading is not recommended for papillary adenoma. Answers C and D are incorrect because to diagnose papillary renal cell carcinoma, the tumor size should be > 1.5 cm.
Comment Here
Reference: Papillary adenoma
Comment Here
Reference: Papillary adenoma
Board review style question #2
What are the chromosomal aberrations reported in papillary adenoma lesions?
- Multiple chromosomal gains and losses
- Trisomies of 7 and 17 only
- Trisomies of 7, 17 and loss of Y and less frequently gains in chromosomes 12, 16 and 20
- Trisomies of 7, 17 and loss of Y as well as deletions of the short arm of chromosome 3
Board review style answer #2
C. Trisomies of 7, 17 and loss of Y and less frequently gains in chromosomes 12, 16 and 20. Papillary adenomas show chromosomal aberrations similar to low grade papillary renal cell carcinoma (PRCC), which include trisomies of chromosomes 7 and 17, loss of Y and occasional gains in 12, 16 and 20. Answer B is incorrect because other chromosomal aberrations have also been reported in papillary adenoma. Answer D is incorrect because chromosome 3p deletions are common in clear cell RCC. Answer A is incorrect because multiple chromosomal alterations are typically seen in high grade PRCC.
Comment Here
Reference: Papillary adenoma
Comment Here
Reference: Papillary adenoma